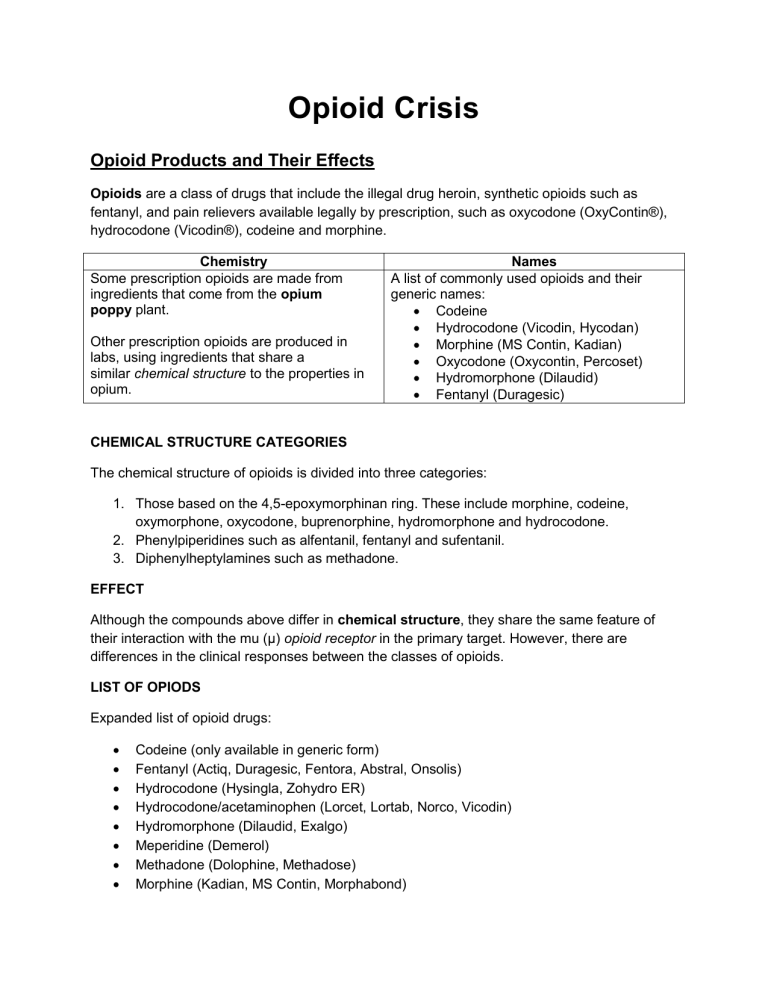
Opioid Crisis Opioid Products and Their Effects Opioids are a class of drugs that include the illegal drug heroin, synthetic opioids such as fentanyl, and pain relievers available legally by prescription, such as oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine and morphine. Chemistry Some prescription opioids are made from ingredients that come from the opium poppy plant. Other prescription opioids are produced in labs, using ingredients that share a similar chemical structure to the properties in opium. Names A list of commonly used opioids and their generic names: Codeine Hydrocodone (Vicodin, Hycodan) Morphine (MS Contin, Kadian) Oxycodone (Oxycontin, Percoset) Hydromorphone (Dilaudid) Fentanyl (Duragesic) CHEMICAL STRUCTURE CATEGORIES The chemical structure of opioids is divided into three categories: 1. Those based on the 4,5-epoxymorphinan ring. These include morphine, codeine, oxymorphone, oxycodone, buprenorphine, hydromorphone and hydrocodone. 2. Phenylpiperidines such as alfentanil, fentanyl and sufentanil. 3. Diphenylheptylamines such as methadone. EFFECT Although the compounds above differ in chemical structure, they share the same feature of their interaction with the mu (μ) opioid receptor in the primary target. However, there are differences in the clinical responses between the classes of opioids. LIST OF OPIODS Expanded list of opioid drugs: Codeine (only available in generic form) Fentanyl (Actiq, Duragesic, Fentora, Abstral, Onsolis) Hydrocodone (Hysingla, Zohydro ER) Hydrocodone/acetaminophen (Lorcet, Lortab, Norco, Vicodin) Hydromorphone (Dilaudid, Exalgo) Meperidine (Demerol) Methadone (Dolophine, Methadose) Morphine (Kadian, MS Contin, Morphabond) Oxycodone (OxyContin, Oxaydo) Oxycodone and acetaminophen (Percocet, Roxicet) Oxycodone and naloxone USE OF OPIOIDS Opioids are often used as medicines because they contain chemicals that relax the body and can relieve pain. Prescription opioids are used mostly to treat moderate to severe pain, though some opioids can be used to treat coughing and diarrhea. Misuse Prescription opioids used for pain relief are generally safe when taken for a short time and when prescribed by a doctor. However, they can be misused. When misusing a prescription opioid, people sometimes crush pills, open capsules, dissolve the powder in water, and inject the liquid into a vein. Some also snort the powder. Addiction Opioids can also make people feel very relaxed and "high" - which is why they are sometimes used for non-medical reasons. This can be dangerous, because opioids can be highly addictive, and overdoses and death are common. Heroin is one of the world's most dangerous opioids. However, it is rarely used as a prescription medicine. PATTERNS OF USE Pattern Medical prescriptions for opioids started to increase sharply in the mid-to late 1990s. Shortly thereafter, nonmedical opioid use also started to increase markedly, reaching a peak of 2.7 million new users in 2002. Increase The annual number of new nonmedical users slowly declined to about 1.8 million in 2012, but the overall pool of people continuing to use nonmedically is very large. From 1999 to 2011, hydrocodone use increased more than two-fold, oxycodone use more than five-fold. REASONS FOR USE Abuse Prescription opioid abuse can occur for multiple reasons, including: Rise Self-medication Recreational highs Compulsory habits, due to dependence or addiction There are numerous factors underlying the rise of prescription opioid problems. A lot of it has to do with how the drugs are viewed in wider society. Non-medical prescription drug users are more likely to have positive expectations about the effects of their using. However, many young users do not recognize the extent of the risks associated with the use of opioids. Examples Young people may gain their understanding of prescription opioid use, by observing older people taking pills. In addition, social media has expanded the scope of community connections, allowing for substance-using teens to develop a network of like-minded peers. Preferences College students are reported to prefer prescription medications for the following reasons: For recreational highs, because they are easy to hide They produce effects that last longer than other substances It enhances the feeling of drunkenness There are potentially less severe consequences if caught using them CRISIS AND BURDEN Crisis Every day, more than 130 people in the United States die from overdosing on opioid drugs. The misuse of and addiction to opioids is considered to be a national crisis in the US, that affects public health and social and economic welfare. Burden The Centers for Disease Control and Prevention estimates that the total "economic burden" of prescription opioid misuse is $78.5 billion per year. This includes costs associated with healthcare, lost productivity, addiction treatment and the criminal justice system. OPIOD MISUSE FACTS Roughly 21 to 29 percent of patients who are prescribed opioids for pain, end up misusing them. Between 8 and 12 percent of opioid users end up developing an opioid use "disorder". An estimated 4 to 6 percent of people who misuse prescription opioids, go on to use the illegal drug heroin. About 80 percent of people who use heroin, began by misusing prescription opioids. Opioid overdoses increased by 30 percent from July 2016 to September 2017 in 45 US states. EPIDEMIC WAVES First Wave The so-called "opioid epidemic" appears to have occurred in three waves. The first wave began in 1991, when deaths involving opioids began to rise following a sharp increase in the prescribing of opioid drugs. Communities where opioids were readily available and prescribed liberally, were the first places to experience increased opioid abuse and "diversion". Diversion: Diversion is the practice where a medicine legally prescribed to an individual, end up in the hands of another person illegally. Second Wave The second wave of the opioid epidemic began in 2010, when there was a rapid increase in deaths from heroin use. Because there were efforts to decrease the prescribing of opioids after the first wave of problems, people then turned to heroin. Deaths due to heroin overdose increased by 286% from 2002 to 2013. Approximately 80% of heroin users admitted to misusing prescription opioids before they started using heroin. Third Wave The third wave of the opioid epidemic began in 2013 with an increase in deaths related to the use of synthetic opioids, such as fentanyl. The sharpest rise in drug-related deaths occurred in 2016 when there were over 20,000 deaths from the use of fentanyl and related drugs. This increase in fentanyl-related deaths has been linked to illegally manufactured fentanyl. MARKET AND PRODUCTS The global opioids market was valued at USD 22.96 billion in 2016 and is projected to expand (see chart below). The increasing occurrence of diseases that cause chronic pain, such as cancer, lower back pain, postsurgical pain, arthritis and fibromyalgia, is driving growth. The opioids market is categorized into immediate-release and extended-release products (see next page for a list of products). Extended-release was the largest segment in 2016 and is expected to be the fastest growing segment in the future. This is owing to the development of innovative dose dispensers, such as transdermal patches. OPIOD PRODUCTS Immediate-Release/Short-Acting Opioids Codeine Oxycodone Hydrocodone Fentanyl Morphine Hydroxymorphone Oxymorphone Propoxyphene Extended-Release/Long-Acting Opioids Oxycodone Hydrocodone Methadone Fentanyl Morphine Oxymorphone Tapentadol Buprenorphine Hydromorphone GROWTH AND SEGMENTS Growth Increasing usage of opioids for non-cancer conditions and in palliative care is promoting market growth. Along with analgesic use, they are widely used as an antidiarrheal medicine and as a cough suppressant. Their use in anesthetics is also increasing their market value. GLOBAL MARKETS North America Segments The global market for opioids is segmented into pain relief, anesthesia, cough suppression, diarrhea suppression and deaddiction (see chart below). In 2016, the pain relief segment dominated the market, mainly due to the high usage of opioids in pain-management therapies. North America is leading the market in opioids, with a share of over 56.0%. One of the major reasons for its dominance, is the rising geriatric population, with terminal conditions such as rheumatoid arthritis. The market is strictly regulated by the FDA, due to the substantial number of deaths from drug abuse. The FDA has released guidelines for the manufacturing, marketing, storage and sales of opioid products. Asia-Pacific Asia Pacific is expected to witness fast growth in opioid sales in the coming years, owing to their rising geriatric population and an increasing focus on palliative care. In addition, the need for improved infrastructure and the rise in healthcare expenditure, is expected to drive the market further. KEY MARKET PLAYERS Some of the key players and manufacturers in the market are listed below. Key players are focusing on expanding their business globally, to increase market share. For example, Purdue Pharma is making inroads in Asia, Latin America, the Middle East and Africa. Purdue Pharma L.P. West-Ward Pharmaceuticals Corporation Allergan Pfizer Inc. Janssen Pharmaceuticals Inc. Egalet Corporation Sun Pharmaceutical Industries Limited. MARKETING STUDY A recent study by the Boston Medical Center's Grayken Center for Addiction, claims that aggressive marketing by pharmaceutical companies to doctors, is a direct cause of the ongoing opioid abuse epidemic in the US. Analysis from the study showed that opioid use increased in places where drug makers focused their marketing efforts. In addition, drug companies did not need to spend lavishly in order to have an effect on opioid prescribing. According to the findings, they gained as much influence after buying meals for doctors, as by paying big cash for speaking and consultation fees. DEATHS AND PAYMENTS Correlations The Grayken Center study found that opioid overdose deaths grew by 18 percent with every three marketing payments that were made to physicians. In addition, sales reps downplayed the risks of addiction and overdose from opioids. The director of policy analysis and research at the Center, Linda Richter, said policymakers and health regulators should prohibit licensed health professionals from accepting payments and incentives from the industry. Comparisons The U.S. opioid addiction crisis continues. Abuse of the drugs led to approximately 50,000 overdose deaths in 2017, according to the Centers for Disease Control (CDC). And according to the National Safety Council, Americans are more likely to die from opioid overdose than from the following causes: Car/motorcycle crash Falls Drowning Choking on food FIGURES AND FINDINGS Figures Pharma companies spent $39.7 million marketing opioid medications to 67,507 doctors across 2,208 counties in the United States, between August 2013 and December 2015, according to the Grayken study. There were 434,754 payments in total. One in twelve U.S. physicians received marketing. The proportion was higher for family physicians, where one in five received marketing for opioid products. Findings The findings of the study suggest that directto-physician opioid marketing runs counter to national efforts to reduce overdose deaths and that policymakers should consider limits on marketing, as part of a serious response to the opioid crisis. It also found that heroin and non-prescribed fentanyl are more commonly involved in U.S. overdose deaths than prescription opioids. However, prescription opioids are involved in about one-third of opioid overdose deaths. Effects, Treatment, and Recovery RECOVERY STRATEGIES Policy Policymakers, the criminal justice system and public health officials have begun to recognize that a holistic, multi-faceted approach is required in order to help people to recover from Substance Abuse Disorders (SUDs) and prevent people from MLPs Legal services can be delivered, as part of a medical-legal partnership (MLP), where lawyers are present in clinical settings and can address patients’ legal problems. becoming addicted in the future. LEGAL SERVICES AND RECOVERY Components of Recovery The Substance Abuse and Mental Health Services Administration (SAMHSA) in the United States, has identified four evidence-based areas that are crucial to managing life in recovery: HEALTH HOME PURPOSE COMMUNITY This involves a full range of medical, social and legal services. Legal Services Legal services help individuals to address issues and barriers to the components necessary for their recovery. Legal services address the unmet social needs of patients, that would otherwise not be addressed in clinical settings and that have a direct impact on health outcomes. PRACTICAL BENEFITS Legal Issues Legal issues involved in substance abuse recovery include: Providing/increasing recovery capital Organizing care and custody issues for children Ensuring people are legally able to work Enforcing workplace rights Preventing housing evictions Example The Helping Opiate-addicted Pregnant women Evolve (HOPE) program, in Cincinnati, Ohio connects with more than 500 pregnant women with opioidrelated SUDs annually. Many of these women have legal needs related to custody, homelessness, domestic violence, sex trafficking, enslavement and access to public benefits. "These women have two main goals...", says Dr. Michael Marcotte, Medical Director for the program "...sobriety and parenting and these goals are intertwined." Their legal needs can directly and indirectly interfere with Benefit Individuals with SUDs have a high correlation of involvement with the criminal justice system, that has made many of them distrust lawyers and the legal system generally. Being referred for legal services through a health care provider can help clients trust these services, because they already have a trusting relationship with their health care provider. Additionally, many people do not know their legal rights or understand that a problem they are facing may have a legal solution. Solving legal issues for clients can be the stability and support needed to pursue these goals. an important step in the process of their recovery from opioid misuse and addiction. LAWSUITS AND ARGUMENTS Lawsuits Summer 2018 saw over 600 lawsuits confronting the U.S. opioid epidemic. Plaintiffs alleged that for over two decades, drug makers have widely advertised their opioid products as virtually non-addictive. Arguments Plaintiffs in the aforementioned lawsuits also claimed that drug makers exaggerated the advantages of opioids and glossed over the chances of addiction that these drugs can cause. Companies named in the suits included: Johnson & Johnson, Purdue Pharma and Ohio’s Cardinal Health. The drug manufacturers on the other hand, contended that medications such as Oxycontin®, have been cleared by the U.S. Food and Drug Administration (FDA) and have genuine medicinal value. CASES AND JUDGEMENTS Settlements Two pharmaceutical companies reached settlements in August 2019 totaling $15 million. Dublin, Ireland-based Endo Pharmaceuticals said it has agreed to pay the Ohio counties of Cuyahoga and Summit, home to Cleveland and Akron, a total of $10 million to settle their lawsuits, which are scheduled to go to trial against other drug makers and distributors in Oct. 21. Allergan, also based in Dublin, agreed to pay $5 million to settle claims related to its branded opioid. Ruling In August 2019, U.S. District Judge Dan Polster, of the Northern District of Ohio, who is overseeing most of the opioid lawsuits, ruled that drug manufacturers and distributors had a legal obligation not to ship opioid orders that were considered suspicious. The companies had argued there was a legal requirement to report suspicious orders, but not to stop from shipping them. Polster denied an additional request from the Ohio counties to rule before trial that defendants did not comply with the requirement, saying there were factual disputes about that. His ruling could be a major win for plaintiffs, particularly in their cases against distribution companies and the big generic drug makers. Oklahoma An Oklahoma judge has found Johnson & Johnson and its subsidiaries helped fuel the state's opioid drug crisis and ordered the consumer products giant to pay $572 million to help address the problem. This marks the first time an opioid manufacturer has been deemed responsible in court and made to pay damages. It could have implications for the slew of lawsuits filed against opioid manufacturers and distributors throughout the country. The financial implications of the $572 million judgment against Johnson & Johnson could extend beyond Oklahoma, according to Tom Claps, a legal analyst with Susquehanna Financial Group. Claps wrote that the Oklahoma settlement suggests future damages could total $37 billion to abate the opioid crisis across the entire country. PAIN MANAGEMENT Opioids are a powerful class of drugs used for the treatment of pain. They are used by healthcare providers to relieve pain that cannot be treated with other types of drugs. Opioids are a type of analgesic drug that contain natural or synthetic chemicals based on morphine, the active component of opium. Opioids include illicit drugs, such as heroin. However, these are not generally used to treat pain. USES AND SIDE EFFECTS Varieties Common opioids include heroin and synthetic (narcotic) medications such as oxycodone, buprenorphine, morphine, codeine, methadone and fentanyl. Opioids are the most commonly prescribed pain-relievers, because of their effectiveness. Uses Morphine is frequently prescribed to alleviate severe pain after surgery. Fentanyl is also prescribed for this purpose. Diphenoxylate or Lomotil is used to relieve severe diarrhea. Codeine is used to ease severe coughs. Side Effects Common side effects of opioids include constipation, sleepiness, nausea, vomiting, clouded thinking, respiratory problems and sexual dysfunction. Some side effects can be minimized by adjusting the time doses are taken, for example after a meal or at bedtime. Constipation can be lessened by drinking fluids, eating foods that are high in fibre, or by taking a laxative. PHYSIOLOGY Receptors Opioids contain chemicals that bind to receptors in the brain and body that mimic pain-relieving chemicals that the body produces naturally. Endorphins, also called endogenous or "natural opioids", are responsible for eliminating minor pain. Strength Opioids, such as morphine and oxycodone, are typically prescribed to people recovering from major surgery or those who have been seriously injured. In these situations, the natural endorphins in the body are not strong enough to combat the pain. For example, when a person hits their elbow on a doorframe it may hurt briefly, but the brain immediately signals the release of endorphins to counteract the pain. Once the chemicals from the opioid attach to the body's receptors, the pain signals are blocked. Methods Opioids can be taken orally by pill. They can also be taken through patches on the skin or intravenously through the bloodstream. BIOLOGICAL PROCESSES Biology When opioids are taken, a series of events take place: The opioid molecules bind to receptors, which are located at the end of nerves throughout the body, including the brain and the spinal cord. The receptors are activated and either suppress or prompt a reaction. In most cases, opioids will suppress pain signals from being transmitted. Effects on receptors are also responsible for side effects, such as respiratory depression and constipation. Processes Certain neurological processes will occur in the brain for everyone taking an opioid, regardless of genetic, environmental and social factors: There is an increase in dopamine production in the limbic reward system. The brain "remembers" rewarding experiences, making them easier to repeat. This mechanism results in the formation of habits and reinforces the connection between taking an opioid and the pleasurable feeling associated with it. Euphoria Dopamine is often responsible for the euphoric feeling many people receive from the recreational use of opioids. Dopamine is also responsible for encouraging the brain to repeat "rewarding behavior". However, the misuse of opioids can lead to abuse and addiction. ADDICTON AND DISEASE Numbers In 2014: - 4.3 million Americans were reportedly using prescription opioids for non-medical reasons. - 435,000 Americans aged 12 and older were reportedly using heroin. Chronic Disease Addiction is a chronic disease. Like diabetes and heart disease, there is no cure. However, addiction can be managed and people with addictions can and do recover. BEGINNING RECOVERY Effects & Assessment Besides harming a person’s health, addiction changes how someone thinks and feels. This may last a long time, leading to harmful actions and difficult relationships. Without treatment and recovery, addiction will keep getting worse. Seeking help is the first step to recovery. The next step is to meet with a qualified clinician. The clinician will review or assess how someone is doing. This first meeting is called an assessment. Treatment Plan The goal of assessment is to gain a thorough understanding of the patient, which will help the clinician and the patient to develop a suitable treatment plan. The clinician will ask questions to understand almost every part of the patient’s life. Common assessment questions include: How long has the person been using drugs? What other medications are being taken, if any? Are there additional social or financial needs? Is there a family history of addiction? Are there other mental or chronic health problems? Clinician: A clinician is a health professional, such as a physician, psychiatrist, psychologist, or nurse. EXAM AND TREATMENT OPTIONS Physical Exam The next step in the treatment plan process, is to complete a thorough physical examination to check the patient’s overall health. This includes finding any conditions (physical or mental) which may change how the Treatment Options After the assessment, the clinician will discuss treatment options with the patient. Every patient's situation is different, so choosing the best option is a shared decision between the patient and the Setting Treatment can occur in different settings, depending on the medication being used and the patient’s particular situation. Four broad treatment settings can be considered: patient is treated and identifying any traces of drugs already in the patient's system. clinician. There are three main choices for medication to treat opioid addiction (details page #8): 1. Methadone 2. Buprenorphine 3. Naltrexone 1. Outpatient 2. Intensive outpatient or partial hospitalization 3. Residential addiction treatment 4. Hospital setting These medications are used alongside counseling and other supports. Drug Testing The most commonly used drug test to test for the presence of drugs in the patient's system, uses the patient’s urine and is called a 'Urine Analysis'. AGREEMENT AND EXPECTATIONS Agreement After discussing the assessment and treatment choices, it is common for the patient and clinician to sign an agreement about what to expect during treatment. This can include: Treatment goals Which medications are used Treatment schedule Counseling plan Expectations Patient commitment to cooperate with the treatment is essential. Risks of relapse and other safety concerns must be discussed. Treatment will be ongoing, as addiction is a chronic disease. TRANSPARENCY AND RESPONSIBILITY Transparency A patient should expect to be treated with respect and dignity and have their concerns listened to when starting or changing a treatment plan. To avoid health problems, patients must share with clinicians any medications they are taking in addition to those in the treatment plan and/or if they drink alcohol regularly. This is important, as taking certain medications and alcohol at the same time, can cause problems. Responsibility Common patient responsibilities include: Keeping appointments Agreeing to drug testing on a regular basis Taking the medications as prescribed Using only drugs that are prescribed Allowing and encouraging involvement of family and friends Avoiding persons, places and situations that may cause a person to use a substance again COUNSELING Counseling is an important part of treatment and is usually a requirement in formal programmes. Counseling helps patients to address personal, social and other issues that may contribute to their substance abuse/addiction. Examples of issues explored in counseling: Improving feelings of self-worth Addressing difficult situations at work or at home The problem of spending time with people who are using drugs or alcohol OPIOD WITHDRAWAL Opioid withdrawal refers to a wide range of symptoms that can occur after stopping the use of opioid drugs. Withdrawal can last up to 10 days, but most often occurs between 3-5 days. Although it can cause very troubling symptoms such as vomiting, cramps and sweating, withdrawal is rarely life-threatening. Using medications to control withdrawal (withdrawal management) is almost always recommended, rather than trying to quit “cold turkey.” When patients try to quit “cold turkey,” it can lead to stronger cravings and continued use. MEDICATIONS Methadone Methadone is an opioid, used to reduce the desire to use other problem drugs. The patient taking methadone feels normal not "high", and withdrawal symptoms do not occur. Methadone can also reduce cravings. Methadone comes in pill, liquid or wafer Buprenorphine Buprenorphine acts to reduce the desire to use problem drugs. It also helps the patient to avoid withdrawal symptoms and reduces cravings. Buprenorphine comes in tablet form. Patients should wait until they are experiencing mild to moderate opioid Naltrexone Naltrexone works by blocking opioids from acting on the brain. It takes away the ability to get "high" from using opioids. This makes naltrexone a good option for preventing relapse. However, it may not stop all drug cravings. A person cannot have any opioids in their body when starting Naloxone Naloxone is used to treat opioid overdose. It can be injected or sprayed in the nose. Naloxone only works for opioids. It may need to be given more than once for an opioid overdose, since its effects may wear off before the opioid does. form. It is usually taken once per day, but over time dosage may change. People who are in stable recovery may be provided a supply of the medication to take at home. withdrawal, before taking the first dose of buprenorphine. This medication is usually taken once per day. naltrexone. If a person does, withdrawal may be very strong. Before a clinician starts a patient on naltrexone, the patient must go through withdrawal under supervision, which lasts between 7-10 days. Naltrexone comes in pill form and in extended release form, by injection in the buttocks. OVERDOSE INCREASE The National Center for Health Statistics, at the Centers for Disease Control and Prevention in the United States, collects information on fatalities as a result of commonly used drugs. The CDC also has a searchable database, called CDC Wonder. More than 70,200 Americans died from drug overdoses in 2017, including illicit drugs and prescription opioids. This represents a twofold increase in a decade. Among the more than 70,200 drug overdose deaths estimated in 2017, the sharpest increase occurred among deaths related to fentanyl and other synthetic narcotics, where there were more than 28,400 overdose deaths (Source: CDC WONDER). FATALITIES – ALL OPIODS The chart below shows the total number of U.S. overdose deaths involving all opioids from 1999 to 2017. This includes heroin, methadone and other synthetic narcotics (mainly fentanyl). Drug overdose deaths rose from 8,048 in 1999 to 47,600 in 2017. Overall, there were a higher number of drug overdose deaths among males. FATALITIES – PRESCRIBED OPIOIDS The chart below shows the total number of U.S. overdose deaths involving prescription opioids, from 1999 to 2017. Drug overdose deaths involving prescription opioids rose from 3,442 in 1999 to 17,029 in 2017. FATALITIES – HEROIN RELATED FATALITIES – PSYCHOSTIMULANTS RELATED The chart below shows the total number of U.S. overdose deaths involving psychostimulants, from 1999 to 2017. Drug overdose deaths rose from 547 in 1999 to 10,333 in 2017. The number of deaths involving the combination of psychostimulants with any opioid, has been increasing steadily since 2014. FATALITIES – COCAINE RELATED SUMMARY AND CONCLUSION All Opioids Drug overdose deaths involving any opioid, including synthetic prescription opioids rose from 18,515 deaths in 2007 to 47,600 deaths in 2017. 68% of deaths occurred among males. From 2016 to 2017, the number of deaths involving prescription opioids remained unchanged. Combination Overdose deaths involving heroin, psychostimulants or cocaine rose in 2017. Deaths involving heroin and cocaine were driven by deaths involving the combination of these drugs with synthetic opioids. Conclusion Clearly the use of illegal and prescription opioids, in combination with other substances, has resulted in a sharp increase in the number of drug overdose fatalities in the United States over the past 20 years. PROJECTIONS AND CAMPAIGN Study A study from investigators at the Massachusetts General Hospital (MGH) Institute for Technology Assessment, projects that the opioid overdose epidemic in the U.S. is likely to increase in the coming years. Illicit Drugs The report published in JAMA Network Open, notes that the nature of the opioid epidemic is changing. It is now driven by the use of illicit opioids such as heroin and fentanyl. Thus, the potential impact of programs targeting prescription opioids is reduced. Measures based on restricting access to prescription opioids will have a minimal impact in reducing overdose deaths, it is claimed. FENTANYL AND PROJECTIONS Fentanyl Jagpreet Chhatwal, PhD, of the MGH Institute for Technology Assessment (MGH-ITA) and author in the aforementioned report said: "In the past five years, deaths have accelerated with the introduction of the powerful synthetic opioid fentanyl into the opioid supply, leading to a continuing increase in overdose deaths at a time when the supply of prescription opioids is decreasing." Projections Chhatwal's team used data from sources such as the National Survey on Drug Use and Health and the Centers for Disease Control and Prevention, to develop an Opioid Policy Model. They then used that model to make projections for probable outcomes up to 2025. TREND AND INITIATIVES Fatalities Under a status quo scenario, the opioid policy model projects that the annual number of opioid overdose deaths will increase from 33,100 in 2015 (when the data began) to 81,700 in 2025. This represents a 147 percent increase. The model also predicts that approximately 700,000 people will die from opioid overdose, with 80 percent of these from illicit drugs such as heroin and fentanyl. Illicit Drugs Researchers estimate that by 2025, half of all new opioid users will begin with illicit drugs, rather than prescription drugs. In the scenarios tested, interventions directed towards reducing the misuse of prescription opioids, would only decrease overall overdose deaths by 3 to 5 percent. Initiatives Co-author of the study, Marc Larochelle, MD, MPH, of the Grayken Center for Addiction at Boston Medical Center said: "This study demonstrates that initiatives focused on the prescription opioid supply are insufficient to bend the curve of opioid overdose deaths in the short and medium term. We need policy, public health and health care delivery efforts to amplify harm reduction efforts and access to evidence-based treatment." INITIATIVE AAOA Allied Against Opioid Abuse (AAOA) is a national education and awareness initiative in the United States, that helps to prevent the abuse and misuse of prescription opioids. Collaborative The AAOA initiative is a collaborative effort. It includes diverse partners from across the pharmaceutical supply chain as well as organizations that are experts in healthcare and public health. Their goal is to contribute to solving the opioid crisis in a meaningful way, by educating patients about the rights, risks and responsibilities associated with prescription opioids. RESOURCES AND SUBSCRIPTION Resources AAOA provides facts, information and resources concerning the Opioid Abuse Epidemic, including references to organizations such as the Centers for Disease Control and Prevention and the National Survey on Drug Use and Health (SAMHSA). In the video on the NEXT slide, healthcare professionals and patients discuss alternatives to opioids for pain management. Subscription You can subscribe to the Allied Against Opioid Abuse (AAOA) mailing list, to learn more about the campaign and to receive regular updates. Their website features surveys and reports on issues such as the need for better consumer education, alternative pain treatments and managing prescriptions safely. For more information and to get involved, visit: https://againstopioidabuse.org/ LESSON SUMMARY Policymakers, the criminal justice system and public health officials have begun to recognize that a holistic, multi-facited approach is required in order to help people to recover from Substance Abuse Disorders (SUDs) and prevent people from becoming addicted in the future. The Substance Abuse and Mental Health Services Administration (SAMHSA) in the United States, has identified four evidence-based areas that are crucial to managing life in recovery: Health, Home, Purpose and Community. Legal services help individuals to address issues and barriers to the components necessary for recovery. Individuals with SUDs have a high correlation of involvement with the criminal justice system. Summer 2018 saw over 600 lawsuits confronting the U.S. opioid epidemic, namely drug makers and suppliers. Federal court cases are being likened to a 1998 ruling against tobacco companies, that gave a total of $206 billion to forty-eight states. Opioids are a type of analgesic drug that contain natural or synthetic chemicals based on morphine, the active component of opium. They are used by healthcare providers to relieve pain that cannot be treated with other types of drugs. Opioids include illicit drugs, such as heroin. Common side effects of opioids include constipation, sleepiness, nausea, vomiting and respiratory problems. Opioids contain chemicals that bind to receptors in the brain and body, that mimic painrelieving chemicals that the body produces naturally. Opioids can be taken orally in tablet form, through patches on the skin or intravenously. Dopamine is responsible for the euphoric feeling many people receive from the recreational use of opioids. In 2014, 4.3 million people reportedly used prescription opioids for non-medical reasons. Addiction is a chronic disease, but recovery is possible through appropriate treatment. More than 70,200 Americans died from drug overdoses in 2017, including illicit drugs and prescription opioids. Among the more than 70,200 drug overdose deaths estimated in 2017, the sharpest increase occurred among deaths related to fentanyl and other synthetic narcotics. A study from investigators at the Massachusetts General Hospital (MGH) Institute for Technology Assessment, projects that the opioid overdose epidemic in the U.S. is likely to increase in the coming years. Initiatives focused on the prescription opioid supply are insufficient to bend the curve of opioid overdose deaths, as they do not sufficiently address the proportional use of illicit opioid use. Allied Against Opioid Abuse (AAOA) is a national education and awareness initiative in the United States, that helps to prevent the abuse and misuse of opioids.