Pediatric Cardiovascular Disorders: Nursing Management
advertisement

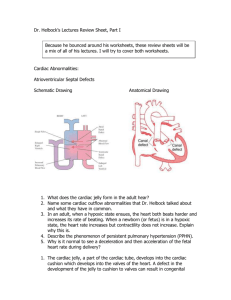
NCM 107 WEEK 14 CHILD WITH CARDIOVASCULAR DISORDERS _______________________________________ Prepared by Giovanni Clyde E. Rebadulla INTRODUCTION _________________________________ This lesson module will serve as the basis for the students understanding on the Cardiovascular disorders of Pediatric clients. This will focus on assessment , common laboratory tests, new classification of cardiac pathologic conditions , the specific disorders and the medical and Nursing managements. CHILD WITH CARDIOVASCULAR DISORDER DEFINITION OF TERMS • Systole – Contraction of the chambers of the heart. • Diastole – Relaxation of the chambers of the heart. DEFINITION OF TERMS • CARDIAC OUTPUT (CO) – The volume of blood pumped by the ventricles per minute. – Calculated by multiplying stroke volume (the volume of blood a ventricle ejects during systole) by the heart rate (beats per minute). – CO = SV x HR DEFINITION OF TERMS • CARDIAC OUTPUT (CO) – Affected by 3 main factors: • PRELOAD – Volume of blood in the ventricles at the end of diastole. • AFTERLOAD – Resistance against which the ventricles must pump. • CONTRACTILITY – Ability of the ventricles to stretch. – Refers to the force of contraction generated by the myocardial muscle. ASSESMENT OF HEART DISORDERS IN CHILDREN HISTORY TAKING HISTORY • Should include: – Thorough pregnancy history. – Ask about the frequency of infections. – Ask the ff: • “ How much activity does it take before the child becomes tired?” “An hour of strenuous play?” “ A short walk?” – Ask about the child’s usual position when resting. ( Some infants with CHD often prefer the knee-chest position, whereas older children often voluntarily squat. PHYSICAL ASSESSMENT PHYSICAL ASSESSMENT • General Appearance – Inspect the toes & fingers. Check for cyanosis & capillary refill time. – Inspect mucous membranes. – Cyanosis can be best recognized in the tongue & mucous membrane of the newborn. – Cyanosis persisting for over 20 minutes after birth suggests serious cardiopulmonary dysfunction. PHYSICAL ASSESSMENT • General Appearance – If the cyanosis increases with crying, cardiac dysfunction is suggested because the child is unable to meet increased circulatory demands. PHYSICAL ASSESSMENT • Pulse, Blood Pressure, & Respirations – Tachycardia • Pulse rate of more than 160 bpm in an infant. • More than 100 bpm at 3 years of age. – Tachycardia is particularly significant if present during sleep. PHYSICAL ASSESSMENT • Pulse, Blood Pressure, & Respirations – Murmurs • Innocent heart murmur – Murmurs of no significance. • Organic heart murmur – As a result of a congenital heart disease or defect. DIAGNOSTIC TESTS • ELECTROCARDIOGRAM DIAGNOSTIC TESTS • ELECTROCARDIOGRAM – Rate – Rhythm – Hypertrophy – Ischemia – Infarction DIAGNOSTIC TESTS • RADIOGRAPHY – Determines heart size. – Can reveal fluid collecting in the lungs (pleural effusion) in cardiac failure. DIAGNOSTIC TESTS • ECHOCARDIOGRAPHY – Assesses movement & dimension of cardiac chambers, thickness of walls & motion of valves. DIAGNOSTIC TESTS • Complete blood count DIAGNOSTIC TESTS • Arterial Blood Gas DIAGNOSTIC TESTS • Cardiac catheterization DIAGNOSTIC TESTS • Cardiac catheterization –Helps evaluate cardiac function. • Diagnostic –Helps diagnose heart defects. • Interventional –Corrects an abnormality by dilating a narrowed valve with the use of a ballon catheter. MONITORING • Central Venous Pressure (CVP) monitoring. CARDIOVASCULAR DISORDERS CONGENITAL HEART DISEASES Common in girls – PDA, ASD Common in boys – TOGA ( transportation of great arteries) TA – truncus arteriosus TOF – tetralogy of Fallot Causes: genetic predisposition teratogens: exposure to rubella – 1st month CONGENITAL HEART DISEASE • The usual cause is failure of heart structure to progress beyond an early stage of embryonic development. CONGENITAL HEART DISEASE • CLASSIFICATION (Old) – Acyanotic heart defects • Involves either a stricture to the flow of blood or a shunt that moves blood from arterial to the venous system (oxygenated to unoxygenated blood, or left-to-right shunt). – Cyanotic heart defects • Blood is shunted from the venous to the arterial system as a result of abnormal communication between the two (deoxygenated blood to oxygenated blood; right-to-left shunt) . CONGENITAL HEART DISEASE I. DEFECTS WITH INCREASED PULMONARY BLOOD FLOW 1. 2. 3. 4. Ventricular Septal Defect (VSD) Atrial Septal Defect (ASD) Atrioventricular Canal Defect (AVC) Patent Ductus Arteriosus (PDA) II. OBSTRUCTIVE DEFECTS 1. Pulmonic Stenosis 2. Aortic Stenosis 3. Coarctation of the Aorta III. MIXED DEFECTS 1. Transposition of the Great Arteries 2. Total Anomalous Pulmonary Venous Return 3. Truncus Arteriosus 4. Hypoplastic Left Heart Syndrome IV. DEFECTS WITH DECREASED PULMONARY BLOOD FLOW 1. 2. Tricuspid Atresia Tetralogy of Fallot CONGENITAL HEART DISEASE • CLASSIFICATION (New) – Include defects with: I. Increased pulmonary blood flow. II. Obstruction to blood flow (out of the heart). III. Mixed blood flow (oxygenated & deoxygenated blood mixing in the heart or great vessels). IV. Decreased pulmonary blood flow. DEFECTS w/ INCREASED PULMONARY BLOOD FLOW Acyanotic Heart defects • • • Increased pressure in the left side of the heart Left to Right shunting of blood CONGENITAL HEART DISEASE I. DEFECTS WITH INCREASED PULMONARY BLOOD FLOW 1. Ventricular Septal Defect (VSD) 2. Atrial Septal Defect (ASD) 3. Atrioventricular Canal Defect (AVC) 4. Patent Ductus Arteriosus (PDA) CONGENITAL HEART DISEASE • VENTRICULAR SEPTAL DEFECT (VSD) CONGENITAL HEART DISEASE • VENTRICULAR SEPTAL DEFECT (VSD) – The most common of all congenital cardiac defects. – Assessment: • At 4-8 wks: Loud, harsh systolic murmur, 3rd-4th ICS, Left sternal border. – Therapeutic management: • About 60 % of small VSDs close spontaneously. A number may be closed by interventional cardiac catheterization. The remainder may require open heart surgery. I. VSD or Ventricular Septal Defect : opening between 2 ventricles Most common isolated congenital heart defect Sx: systolic murmurs at lower border of sternum; 3-4th LICS cardiac catheterization : increased O2 saturation ECG : hypertrophy of R side of heart Nsg Care: Cardiac catheterization: site Right femoral vein 1.NPO 6 hrs before procedure. 2.Assess for complications – infection, thrombus formation 3.Check pedal pulses (dorsalis pedis) Mgt.1. long term antibiotic – to prevent subacute bacterial endocarditis (SBE) 2. open heart surgery- if > 2 mm defect CONGENITAL HEART DISEASE • ATRIAL SEPTAL DEFECT (ASD) CONGENITAL HEART DISEASE • ATRIAL SEPTAL DEFECT (ASD) – Abnormal communication between the two atria. – More frequent in girls. – Blood flow is from left to right (oxygenated ot unoxygenated). – Assessment: • Harsh Systolic murmur at the 2nd -3rd ICS, pulmonic area. – Therapeutic Management: • Without surgery, the child is at risk for infectious endocarditis & eventual heart failure. II. ASD or Atrial Septal Defect : failure of foramen ovale to close Ostium ASD Primum 1 opening is at the lower end of the septum ASD Ostium Opening is near the 2 secundum center of the septum ASD Sinus 3 venosus Opening is near the junction of SVC and right Sx :systolic murmur @ upper border of sternum; 2-3th LICS result of cardiac catheterization & ECG same with VSD Mgt: open heart surgery ; Increase in Pressure in the left ventricle + Back flow + Pulmonary congestion and edema RESULT : Dsypnea Cracles Frothy secretions Blood tinge sputum ( pink) **** Failure of the Foramen Ovale to close CONGENITAL HEART DISEASE • ATRIOVENTRICULAR CANAL DEFECT (AVC) CONGENITAL HEART DISEASE • ATRIOVENTRICULAR CANAL DEFECT (AVC) – Also known as an endocardial cushion defect. – Results from the incomplete fusion of the endocardial cushion or in the septum of the heart at the junction of the atria & ventricles. – 1 in 9 children with trisomy 21 (Down Syndrome) has this type of congenital heart defect. CONGENITAL HEART DISEASE • PATENT DUCTUS ARTERIOSUS (PDA) CONGENITAL HEART DISEASE • PATENT DUCTUS ARTERIOSUS (PDA) – The ductus arteriosus is an accessory fetal structure that connects the pulmonary artery to the aorta. If it fails to close at birth, blood will be shunted from the aorta (oxygenated blood) to the pulmonary artery (deoxygenated blood). – Assesment: • Wide pulse pressure • Typical continuous “machinery” murmur, upper left sternal border. CONGENITAL HEART DISEASE • PATENT DUCTUS ARTERIOSUS (PDA) – Therapeutic management: • Prostaglandins particularly PGE1 stimulates the ductus arteriosus to remain open during fetal life. • Indomethacin, a prostaglandin inhibitor may be used for ductus closure. • If medical management fails, surgical ligation of the ductus arteriosus is done. I.PDA=Pulsus Ductus Arteriosus failure of the ductus arteriosus to close - should close within 24 h-complete month close – 1 = + Persistent connection = + congestion as more blood goes to lungs Sx : machinery-like murmur wide pulse pressure (>40 mmHg) prominent radial pulse ECG : hypertrophy Left ventricle Drug: Indomethacin –Pg inhibitor facilitate closure of PDA ligation of PDA by 3-4 yo thoracotomy procedure CONGENITAL HEART DISEASE II. OBSTRUCTIVE DEFECTS 1. Pulmonic Stenosis 2. Aortic Stenosis 3. Coarctation of the Aorta CONGENITAL HEART DISEASE • PULMONIC STENOSIS CONGENITAL HEART DISEASE • PULMONIC STENOSIS – Narrowing of the pulmonary valve or the pulmonary artery just distal to the valve. – Assessment: • asymptomatic or have signs of heart failure. • Cyanosis may be present if narrowing is severe. – Therapeutic Management: • Depends OBSTRUCTIVE LESIONS 1.PULMONIC Stenosis:narrowing of pulmonic valve Sx: typical systolic ejection murmur : upper left border of sternum S2 sound widely split ECG : RIGHT ventricular hypertrophy Mgt.: Balloon angioplasty CONGENITAL HEART DISEASE • AORTIC STENOSIS CONGENITAL HEART DISEASE • AORTIC STENOSIS – Stenosis or stricture of the aortic valve preventing blood from passing freely from the LV to the aorta. – Assessment: • The child may be free of symptoms if severe, there is decreased cardiac output as evidenced by faint pulses, hypotension, tachycardia. – Therapeutic Management • Balloon angioplasty or surgical repair. 2. Aortic Stenosis=:narrowing of the Aortic valve Sx: angina typical murmur rough systolic sound and thrill ECG: Left ventricular hypertrophy Mgt: Balloon valvuloplasty Open heart surgery : if >2 mm defect CONGENITAL HEART DISEASE • COARCTATION OF THE AORTA CONGENITAL HEART DISEASE • COARCTATION OF THE AORTA – Narrowing of the lumen of the aorta due to a constricting band. – Results in increased blood pressure in the upper portions of the body therefore producing headache & vertigo. – Epistaxis may occur. CONGENITAL HEART DISEASE • COARCTATION OF THE AORTA – Assessment: • Absence of femoral pulses • Enlarged collateral vessels seen as nodules on the ribs. • (+) leg pain due to diminished blood supply to the lower extremities. • Blood pressure on the arms will be at least 20 mmHg higher than the legs. – Therapeutic Management: • Balloon catheter, surgery. • Surgical repair is usually scheduled by 2 years of age. 3. Coarctation of Aorta : narrowing of the segment in aortic arch Sx: absent femoral pulse -increased BP in upper extremities; -decreased in lower extremities - PR in upper extremities; higher than he PR in lower extremities ECG: left ventricle hypertrophy Mgt: close heart surgery;Balloon angioplasty again:::Different BP in lower and upper Extremities • • • • • A young child has Coarctation of the Aorta. When taking the child’s vital signs, the nurse can expect to observe: a. Nothing of the clavicle b. Bounding femoral pulses c. Weak, thread and radial pulses d. High BP in upper extremities • • • A child undergoes heart surgery to repair the defects associated with COA Postoperatively it is essential that the nurse prevent: a. Crying c. Constipation b. Coughing d.Unnecessary movement CONGENITAL HEART DISEASE III. MIXED DEFECTS 1. Transposition of the Great Arteries 2. Total Anomalous Pulmonary Venous Return 3. Truncus Arteriosus 4. Hypoplastic Left Heart Syndrome CONGENITAL HEART DISEASE • TRANSPOSITION OF THE GREAT ARTERIES CONGENITAL HEART DISEASE • TRANSPOSITION OF THE GREAT ARTERIES – Incompatible with life. – Assessment: • Cyanotic at birth. – Therapeutic Management: • PGE1 Administration to keep Ductus Arteriosus open. • Surgical repair. Transposition of Great Arteries (TOGA) - aorta originates from Right ventricle (normally from Left ventricle) - pulmonary artery arising form Leftt ventricle (normally – Right ventricle) Sx: cyanosis or signs of CHF polycythemia: compensatory due to chronic hypoxia ECG : cardiomegaly Cardiac cath Mgt :Pg E1 : decreased O2 saturation Palliative repair – Rashkind procedure Complete repair – Mustard repair CONGENITAL HEART DISEASE • TOTAL ANOMALOUS PULMONARY VENOUS RETURN – The pulmonary veins return to the right atrium or the superior vena cava instead of to the left atrium. – Infants are mildly cyanotic & tire easily. • right side of the heart hypertrophies& the left side remain small • - CHF & cyanosis may occur • Mgt : Corrective repair in early infancy CONGENITAL HEART DISEASE • TRUNCUS ARTERIOSUS – One major artery or “trunk” arises from the left & right ventricles in place of a separate aorta & pulmonary artery. – The child is cyanotic & may have a typical VSD murmur. 3. TRUNCUS ARTERIOSUS: aorta & pulmonary artery arise from 1 single vessel or common trunk that originates from both ventricles Sx: cyanosis, polycythemia, poor growth ,CHF signs murmur Mgt: Corrective repair in early infancy CONGENITAL HEART DISEASE • HYPOPLASTIC LEFT HEART SYNDROME CONGENITAL HEART DISEASE • HYPOPLASTIC LEFT HEART SYNDROME – The LV is non-functional & is unable to effectively pump blood into the systemic circulation. – Attempts at surgery are of limited success. – Infants rarely live longer than 1 month. CONGENITAL HEART DISEASE IV. DEFECTS WITH DECREASED PULMONARY BLOOD FLOW 1. Tricuspid Atresia 2. Tetralogy of Fallot DEFECTS w/ DECREASED PULMONARY BLOOD FLOW Cyanotic Heart Defects: Right to Left heart shunting of blood : increased pressure in the right side of the heart. Common sign is Cyanosis CONGENITAL HEART DISEASE • TRICUSPID ATRESIA – An extremely serious disorder since the tricuspid valve is completely closed allowing no blood to flow from the right atrium to the right ventricle. – Instead, blood crosses through the patent foramen ovale into the left atrium. 4. Tricuspid atresia: failure of tricuspid valve to open Sx: cyanosis, tachycardia, dyspnea polycythemia, clubbing of fingers Mgt: Pg E1: to keep patency of ductus arteriosus Fontan procedure: to open valve tricuspid • • • A 2-year old has a congenital right to left shunt defect of the heart, the nurse would expect to observe: a. Orthopnea c. Absense of pedal pulses b. An elevated hematocrit d. Edema in the extremities CONGENITAL HEART DISEASE • TETRALOGY OF FALLOT CONGENITAL HEART DISEASE • TETRALOGY OF FALLOT – Four anomalies are present: 1. 2. 3. 4. Pulmonic stenosis VSD Overriding aorta Hypertophy of the right ventricle CONGENITAL HEART DISEASE • TETRALOGY OF FALLOT – Assessment: • • • • • Newborns may not exhibit a high degree of cyanosis but as they become more active, they will begin to appear cyanotic. Polycythemia will occur. Sever dyspnea, growth retardation & clubbing of fingers. Tend to assume a squatting or knee chest position. May develop syncope or fainting episodes (“tet” spells) caused by decreased blood supply to the brain. CONGENITAL HEART DISEASE • TETRALOGY OF FALLOT – Therapeutic management • Surgery done at 1 – 2 years of age. – Temporary repair: – Full repair: • Blalock –Taussig procedure. Brock procedure. If a baby begins to have a hypoxic episode, placing the baby in a knee-chest position & administering morphine effective. sulfate is generally 5. Tetralogy of Fallot = Persistent cyanosis with vigorous crying = Hypoxia inspite of O2 therapy P – pulmonary stenosis R – right ventricular Hypertrophy O – overriding or dextroposition of aorta V – ventricular septal defect 1. 2. 3. 4. 5. 6. Sx: ECG : right ventricular hypertrophy Cyanosis; polycythemia; syncope severe dyspnea –> squatting position : to decrease venous Return growth retardation: d/t decreased tissue perfusion Exertional Dyspnea with cyanosis 6. tet spell or cyanotic spell : short episodes of hypoxia, relieved by squatting Knee chest position 7. clubbing of fingers: compensatory enlargement of due to chronic hypoxia 8. mental retardation:bd/t oxygenation in the brain 9. CXR: boot-shaped heart 10. Stunted growth capillaries decreased Mgt: 1.O2 and decrease o2 demand 2.Avoid Valsalva maneuver/ administer laxative/ increase roughage 3.Beta-blockers : Propranolol 4. Palliative repair – Blalocktaussig procedure 5. Brock procedure – complete repair of associated defects 6.Prophylactic antibiotics 7. Monitor hemoglobin hct,consciousness 8. POSITION during attacks : SQUAT or Knee Chest Position • • • • • A common finding in most children with cardiac anomalies is: a. Mental retardation. b. Delayed physical growth. c. Cyanosis and clubbing of fingertips. d. A family history of cardiac anomalies. ACQUIRED HEART DISEASE • • • • • • • Heart Failure Rheumatic Fever Kawasaki Disease Endocarditis Hypertension Hyperlipidemia Cardiomyopathy ACQUIRED HEART DISEASE • HEART FAILURE – Results when the myocardium of the heart cannot circulate & pump enough blood to supply oxygen & nutrients to body cells. – Blood pools in the heart or in the pulmonary or venous system. ACQUIRED HEART DISEASE • HEART FAILURE – Assessment: • First sign is tachycardia then followed by tachypnea. • Infants are usually breathless, tire easily & have feeding difficulties. • Right sided HF: – Increased venous pressure. – Hepatomegaly. – Edema (late sign). • Left Sided HF: – Pulmonary congestion (blood accumulates in the lungs). – Dyspnea. ACQUIRED HEART DISEASE • HEART FAILURE – Therapeutic Management: • Evacuation of excess fluid: – Diuretics: Furosemide (Lasix) • Improve contractility of the heart: – Inotropics: Digoxin (Lanoxin) • Signs of Digoxin toxicity: Anorexia, nausea & vomiting, dizziness, diarrhea & headache. • Reduce afterload: – Vasodilators: Hydralazine • • • Among the last signs of heart failure in the infant and child is: a. Orthopnea c. Tachycardia b. Tachypnea d. Peripheral edema ACQUIRED HEART DISEASE • RHEUMATIC FEVER • - inflammatory ,Autoimmune dise.ase due to an infection w/ Group A Beta Hemolytic streptococcus (GABHS) • -pharyngitis, tonsillitis, scarlet fever, “strep throat” or impetigo. – Occurs most often in children 6 – 25 years old. ACQUIRED HEART DISEASE • RHEUMATIC FEVER – Therapeutic Management: • Penicillin (IM) therapy to be maintained for 10 – 14 days then the child is maintained on prophylactic penicillin therapy for at least 5 years after the initial attack or until they are 18 years of age. Rheumatic Heart Disease -complication of untreated Rheumatic fever; -presence of Aschoff’s bodies that affect the mitral valve ; MVP or mitral regurgitation Jones Criteria Major 1. polyarthritis – multi joint pain; asymmetrical, migratory 2. chorea – st. vitus dance purposeless involuntary hand and shoulder with grimace 3. pancarditis – tachycardia erythema marginatum - macular rashes 4. SQ nodules 5. erythema marginatum – reddish macular lesions on extensor surfaces (elbow, knee) Minor 1. arthralgia – joint pain 2. low grade fever 3. Inc. C reactive protein 4. Inc. ESR 5. Inc. ASO titer 6. ECG : prolonged PR interval Criteria: 2 major manifestations 1 major + 2 minor signs OR Nsg Care: CBR throat swab – culture and sensitivity DOC – penicillin G NSAIDS for arthritis A/E of aspirin w/ viral infection : Reye’s syndrome– form of encephalopathy - fatty infiltration of organs such as liver and brain Penadur ; IM once amonth .3-5 years ACYANOTIC Heart Disease Ventricular Septal Defect Atrial Septal Defect Coartation of the Aorta Atrial Septal Defect Aortic stenosis Pulmonary stenosis Cyanotic Heart Disease (3 T’s) TOGV Tetralogy of Fallot Truncus Arteriosus • • • The pathology of rheumatic fever chiefly involves changes in which basic type of tissue? a. Muscular c. Connective b. Endocrine d. Epithelial • • In obtaining health history the nurse should be alert to the mention of which of the following as evidence of previous episodes of rheumatic fever? 1. Watery diarrhea 3. Frequent • • • epistaxis 2. Growing pains 4. Episodic vertigo a. 1 and 2 c. 3 and 4 b. 2 and 3 d. All of the above ACQUIRED HEART DISEASE • KAWASAKI DISEASE ACQUIRED HEART DISEASE • KAWASAKI DISEASE – A febrile, multi-systemic disorder that occurs almost exclusively in children before the age of puberty. – Vasculitis is the principle (& life threatening) finding. – Therapeutic management: • Salicyclic acid (Aspirin): decreases inflammation & platelet aggregation. ACQUIRED HEART DISEASE • ENDOCARDITIS ACQUIRED HEART DISEASE • ENDOCARDITIS – Inflammation & infection of the endocardium or heart valves of the heart. – Vegetation is composed of bacteria, fibrin & blood. – Commonly occurs as a complication of congenital heart disease such as VSD, TOF, COA. – Streptococcal infection tends to invade the body during dental surgery. – Over a period of time the invading process destroys the valves & endocardium. ACQUIRED HEART DISEASE • HYPERTENSION – Primary Hypertension • Occurs as a secondary manifestation of another disease such as kidney disease, COA. – Essential Hypertension • No identifiable cause • HYPERLIPEDEMIA – Increased fatty acid in the blood. • CARDIOMYOPATHY – Refers to a structural or functional abnormality of the ventricular myocardium. – Impairs systolic function & may lead to heart failure. CARDIOPULMONARY ARREST • Assessment: – Respiratory failure is the most frequent cause of cardiac arrest because anoxia in the heart muscle quickly leads to cardiac arrest. CARDIOPULMONARY ARREST • STEPS FOR RESUSCITATION (ABC’s) – AIRWAY – BREATHING – CIRCULATION CARDIOPULMONARY RESUSCITATION • AIRWAY – Assess the patient’s airway for patency and look for signs of airway obstruction. – Open the airway using head tilt/chin lift if no spinal trauma is suspected, or modified jaw thrust if spinal trauma is suspected CARDIOPULMONARY RESUSCITATION • BREATHING CARDIOPULMONARY RESUSCITATION • CIRCULATION – Feel for the carotid pulse (in an infant, the brachial pulse). CARDIOPULMONARY RESUSCITATION • CIRCULATION – If you feel no pulse, proceed with chest compressions.