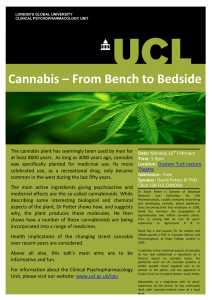
CP10CH28-vanWinkel ARI ANNUAL REVIEWS 12 February 2014 14:36 Further Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Click here for quick links to Annual Reviews content online, including: • Other articles in this volume • Top cited articles • Top downloaded articles • Our comprehensive search Epidemiological, Neurobiological, and Genetic Clues to the Mechanisms Linking Cannabis Use to Risk for Nonaffective Psychosis Ruud van Winkel1,2 and Rebecca Kuepper1 1 Department of Psychiatry and Psychology, School of Mental Health and Neuroscience, European Graduate School of Neuroscience (EURON), South Limburg Mental Health Research and Teaching Network (SEARCH), Maastricht University Medical Center, Maastricht, The Netherlands; email: ruud.vanwinkel@maastrichtuniversity.nl 2 University Psychiatric Center, Catholic University Leuven, 3070 Kortenberg, Belgium Annu. Rev. Clin. Psychol. 2014. 10:767–91 Keywords First published online as a Review in Advance on January 20, 2014 THC, cannabidiol, psychosis, schizophrenia, gene-environment interaction The Annual Review of Clinical Psychology is online at clinpsy.annualreviews.org Abstract This article’s doi: 10.1146/annurev-clinpsy-032813-153631 c 2014 by Annual Reviews. Copyright All rights reserved Epidemiological studies have shown that the association between cannabis and psychosis is robust and consistent across different samples, with compelling evidence for a dose-response relationship. Because longitudinal work indicates that cannabis use precedes psychotic symptoms, it seems reasonable to assume a causal relationship. However, more work is needed to address the possibility of gene-environment correlation (for example, genetic risk for psychosis causing onset of cannabis use). Moreover, knowledge about underlying biological mechanisms linking cannabis use and psychosis is still relatively limited. In order to understand how cannabis use may lead to an increased risk for psychosis, in the present article we (a) review the epidemiological, neurobiological, and genetic evidence linking cannabinoids and psychosis, (b) assess the quality of the evidence, and finally (c) try to integrate the most robust findings into a neurodevelopmental model of cannabis-induced psychosis and identify the gaps in knowledge that are in need of further investigation. 767 CP10CH28-vanWinkel ARI 12 February 2014 14:36 Contents Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. THE ASSOCIATION BETWEEN CANNABIS AND PSYCHOSIS . . . . . . . . . . . . . . . Self-Medication or Reverse Causality . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Gene-Environment Correlation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . INSIGHTS FROM EPIDEMIOLOGY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Age of Onset of Cannabis Use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . The Amount of THC and CBD in the Cannabis Consumed . . . . . . . . . . . . . . . . . . . . . . Interaction with Other Environmental Risk Factors . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . INSIGHTS FROM NEUROBIOLOGICAL STUDIES . . . . . . . . . . . . . . . . . . . . . . . . . . . . Neurobiology of the Endocannabinoid System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Effects of THC on the Brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Effects of CBD on the Human Brain in Interaction with THC . . . . . . . . . . . . . . . . . . . . Cannabis Use and the Dopamine System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . INSIGHTS FROM GENETIC STUDIES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Evidence for G×E: Omnibus Approach Using Familial Risk . . . . . . . . . . . . . . . . . . . . . . Candidate Gene Studies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . FACTS, CONTROVERSIES, AND MYTHS IN THE CANNABIS-PSYCHOSIS RELATIONSHIP . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Compiling the Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Recommendations for Future Research . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 768 768 769 771 771 772 773 773 773 774 776 776 777 778 778 781 781 784 THE ASSOCIATION BETWEEN CANNABIS AND PSYCHOSIS Since the initial reports linking cannabis use to risk of schizophrenia were published in the late 1960s, a large body of epidemiological studies and meta-analytic work has demonstrated an association between psychotic disorder and cannabis use, with a twofold increased risk for psychotic disorder associated with the use of relevant amounts of cannabis (Henquet et al. 2005b, Moore et al. 2007). The association has now been clearly established and quantified, and the issue that deserves further scrutiny is the nature of this association. Most investigators assume that cannabis is a “component cause” of schizophrenia, that is, its influence on the risk of schizophrenia is causal, but cannabis in itself is neither necessary nor sufficient to induce the illness (Murray et al. 2007). However, alternative explanations need to be considered before claims of causality can be substantiated and possible underlying causal mechanisms can be discussed. Self-Medication or Reverse Causality A first alternative explanation for the association between cannabis and psychosis is that emerging psychotic symptoms may lead to cannabis use as a way of dealing with these symptoms; this explanation is also referred to as the “self-medication hypothesis.” A number of studies have addressed this hypothesis using longitudinal designs. Henquet and colleagues (2005a) found no evidence for self-medication but did find a significant association between cannabis use at baseline and psychotic symptoms at four-year follow-up in 2,437 individuals from the general population between ages 14 and 24 years, and similar findings were reported by Fergusson and coworkers from a seven-year follow-up (from ages 18 to 25) of a New Zealand birth cohort (N = 1,055) (Fergusson et al. 2003). Ferdinand and coworkers (2005), however, found a bidirectional association between 768 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 cannabis use and psychotic symptoms in a 14-year follow-up of a general population sample of 1,580 individuals (ages 4 to 16 at baseline), as did McGrath and colleagues (2010) in a birth cohort study of 3,801 individuals assessed at ages 14 and 21 years. Importantly, the latter study also included a sibling-pair analysis (228 pairs), confirming the association between duration since first cannabis use (as proxy for age at first cannabis exposure) and incident delusionallike experiences in nonaffected sibling pairs. The inclusion of a sibling-pair analysis reduces the likelihood that the reported association could be explained by unmeasured residual confounding because many of the unmeasured potential confounders can be assumed to be similar for both siblings. The most methodologically rigorous study so far reported that over a ten-year follow-up period, in individuals without psychotic symptoms and without cannabis use at baseline, the onset of cannabis use at the four-year follow-up measurement increased the risk of incident psychotic symptoms at the nine-year follow-up assessment, and there was no evidence for self-medication (Kuepper et al. 2011c). Thus, although some studies found evidence for self-medication with cannabis, this finding was inconsistent across different studies; in contrast, evidence for a temporal relationship between onset of cannabis use and later psychotic symptoms was strong, significant, and consistent across different studies (Decoster et al. 2012). Gene-Environment Correlation An alternative explanation for the association between cannabis and psychosis is genetic confounding, or gene-environment correlation (for schematic overview, see Figure 1), which would indicate that genetic risk for schizophrenia also results in higher risk of cannabis use. This could take the form of genetic confounding (cannabis use does not cause psychosis but is merely an epiphenomenon of genetic risk for schizophrenia) or environmental mediation of genetic risk (genetic risk leads to cannabis use, which subsequently leads to even higher risk for psychosis compared to genetic risk alone). Unfortunately, very few studies have examined the possibility of gene-environment correlation. Veling and colleagues (2008) studied patterns of cannabis use in 100 patients with psychotic disorder, their unaffected siblings (N = 63), and 100 healthy controls (matched for age, gender, and ethnicity). In this sample, the healthy siblings displayed rates of cannabis use similar to those of the healthy controls, a finding that argues against the possibility that a genetic predisposition for schizophrenia also leads to a genetic predisposition for cannabis use. Similarly, the Genetic Risk and Outcome in Psychosis (GROUP) investigators did not find evidence for genetic confounding in a study using a cross-sibling, cross-trait design to investigate sensitivity to the psychotomimetic effect of cannabis in a sample of 1,120 patients with psychotic disorder, 1,057 unaffected siblings, and 590 controls [Genetic Risk Outcome Psychos. (GROUP) Investig. 2011]. By contrast, Smith and colleagues did report that rates of cannabis use were higher in 53 nonpsychotic siblings of patients with psychotic disorder than in 75 siblings of community controls (Smith et al. 2008). These reports have all used family membership as a proxy of genetic risk, which has both advantages and disadvantages. The largest advantage of such an approach is that it takes into account the net genetic risk, including the risk brought about by epistatic interactions between genes (van Os et al. 2008). The major disadvantage is that it is unable to take into account underlying genetic heterogeneity and assumes genetic risk to be equal across different families (which is unlikely to be the case). Moreover, familial clustering of cannabis use in families with psychosis does not necessarily indicate a relationship to genetic risk for psychosis, as this may also merely indicate that cannabis use per se tends to cluster in families. Recent advances in molecular genetics have resulted in the possibility to quantify genetic risk using polygenic risk scores derived from www.annualreviews.org • Cannabis Use and Psychosis 769 CP10CH28-vanWinkel ARI 12 February 2014 14:36 Causal association Psychosis Reverse causality Psychosis Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Genetic confounding Genetic risk Psychosis Genetic risk Psychosis Gene-environment interaction Genetic risk Psychosis Figure 1 Representation of the different possible relationships among cannabis use, genetic risk, and expression of psychosis. genome-wide association studies (Purcell et al. 2009). Studies using these polygenic risk scores may therefore provide a novel means to examine the possibility of gene-environment correlation in a more methodologically rigorous way. At present, given the relative scarcity of data on the relationship between genetic risk for psychosis and onset of cannabis use, gene-environment correlation cannot be ruled out as (at least a partial) explanation of the association between cannabis and psychosis. Interestingly, studies using polygenic risk scores have convincingly shown that polygenic risk for schizophrenia is not only associated with risk for schizophrenia in independent samples, but also 770 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 for depression and bipolar disorder and, to a lesser extent, autism and attention-deficit hyperactivity disorder (ADHD) (Cross-Disord. Group Psychiatr. Genomics Consort. et al. 2013). This raises the question of whether the association between cannabis use and mental disorders is specific to psychosis. This question was addressed in a meta-analysis conducted by Moore and colleagues, who reported that, although several studies found an association with affective outcomes, effect sizes were much smaller than for psychotic outcomes, and fewer attempts were made to address noncausal explanations such as confounding or reverse causality (Moore et al. 2007). Given that (a) the association between cannabis and psychosis is robust, (b) the association is consistent across different samples, (c) compelling evidence exists for a dose-response relationship (Moore et al. 2007), (d ) the temporal relationship indicates that cannabis use precedes psychotic symptoms (Kuepper et al. 2011c), and (e) alternative explanations are unlikely to explain the link between cannabis and psychosis, it seems reasonable to assume a causal relationship. In order to understand how cannabis use may lead to an increased risk for psychosis, we (a) review the epidemiological, neurobiological, and genetic evidence linking cannabinoids and psychosis, (b) assess the quality of the evidence, and (c) integrate the most robust findings and identify the gaps in knowledge that are in need of further investigation. INSIGHTS FROM EPIDEMIOLOGY A number of findings from epidemiological studies may help to elucidate the underlying mechanisms linking cannabis use to risk for psychosis. These include (a) the influence of age of onset of first use, (b) the importance of the ratio of tetrahydrocannabinol (THC) to CBD (cannabidiol, a further cannabis constituent) in the type of cannabis consumed, and (c) evidence for interaction with other epidemiological risk factors for psychosis. Age of Onset of Cannabis Use There is good epidemiological evidence that the link between cannabis use and later psychotic illness may be modulated by age of first exposure. In the prospective Dunedin Multidisciplinary Health and Development Study, a general population birth cohort study, 1,037 individuals were assessed and follow-ups were conducted with regard to substance use and psychiatric outcomes, including psychotic and depressive symptoms as well as disorders, at ages 11, 15, 18, and 26 (Arseneault et al. 2002). When self-reported psychotic symptoms at age 11 were accounted for, cannabis use at age 15 and 18 was associated with a higher risk of psychotic symptoms at age 26, and this effect was stronger for earlier cannabis use. Similarly, the association between cannabis use and a later diagnosis of psychotic disorder was stronger, yet no longer significant, for early cannabis use (Arseneault et al. 2002). Stefanis and colleagues (2004) investigated the association between adolescent cannabis use and subclinical positive and negative psychotic symptoms using cross-sectional data for 3,500 individuals from a Greek birth cohort. Information on psychotic symptoms was gathered using the Community Assessment of Psychic Experiences questionnaire (Konings et al. 2006), and cannabis use was assessed by means of self-report. Results showed that age of onset of use moderated the association between cannabis use and subclinical psychotic symptoms: Independent of lifetime frequency of use, the association between cannabis use and psychotic experiences in both the positive and the negative symptom dimension was much stronger for individuals who had started to use cannabis before the age of 16 compared to those who started to use cannabis thereafter (Stefanis et al. 2004). A similar interaction between cannabis use and age of onset of use was revealed in a non-Western sample of 472 individuals randomly drawn from the general population in Trinidad (Konings et al. 2008). Participants provided information on www.annualreviews.org • Cannabis Use and Psychosis 771 ARI 12 February 2014 14:36 past and current cannabis use and completed the Community Assessment of Psychic Experiences. After adjustment for age, gender, school type, current use of cannabis, and use of other drugs, lifetime use of cannabis was associated with psychotic experiences only in individuals who started using cannabis before the age of 14; no such association was revealed for individuals with later onset of cannabis use (Konings et al. 2008). More recently, Schubart and colleagues (2011a) reported that cannabis use before the age of 12 was associated with a fourfold risk for psychiatric hospitalizations compared to individuals with later initial use in a sample of about 17,000 individuals from the general population. Similarly, Stowkowy and colleagues (2013) reported on predictors of clinical high-risk symptoms for psychotic disorder and revealed that lower age of onset of cannabis use was significantly associated with clinical high-risk status. Average age of onset of use was 15.56 ( ±2.19) and 15.67 ( ±1.67) for healthy controls and individuals with a family history of psychosis who did not present clinical high-risk symptoms, respectively, whereas the average age of onset of cannabis use was 13.94 ( ±1.83) in individuals who presented with both a familial liability and clinical high-risk symptoms of psychosis (Stowkowy & Addington 2013). In addition, several studies demonstrate worse cognitive performance as well as morphological brain changes in adults who started to use cannabis before the age of 17 compared to individuals who started at a later age (Ehrenreich et al. 1999, Pope et al. 2003, Wilson et al. 2000). This is supported by animal studies demonstrating that exposure to THC during puberty but not adulthood may lead to long-lasting changes in adult brain function and morphology that are associated with deficits in cognitive functioning as well as neurobehavioral alterations implicated in addictive behavior such as increased sensitivity to other drugs of abuse (Klugmann et al. 2011, Pistis et al. 2004, Realini et al. 2009, Rubino et al. 2009, Schneider et al. 2005, 2008; Schneider & Koch 2003, 2007; Wegener & Koch 2009). Thus, evidence from both animal and human studies suggests that puberty represents a period of particular vulnerability for cannabis exposure, which is not surprising given the neurodevelopmental changes and maturational processes that happen in the pubertal brain (Bossong & Niesink 2010). Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel The Amount of THC and CBD in the Cannabis Consumed Another important aspect may be the ratio between THC and CBD, which differs considerably between the various cannabis preparations. In contrast to THC, which has been shown to induce psychotomimetic effects and anxiety, to worsen cognitive performance, and to have a neurotoxic effect, CBD has been shown to have neuroprotective, antioxidative, and anti-inflammatory properties and may antagonize the negative effects of THC (Arnold et al. 2012, Zuardi et al. 2012). In a series of naturalistic studies, Morgan and colleagues analyzed hair samples from regular and recreational cannabis users and measured the amount of THC and CBD. Cannabis users with only traces of THC in hair had significantly higher levels of schizophrenia-like symptoms compared to cannabis users with THC + CBD or no cannabinoid in hair (Morgan & Curran 2008). Individuals who smoked cannabis low in CBD further showed impaired recall on a verbal learning task while intoxicated with their own cannabis, whereas no such memory impairment was detected in individuals smoking cannabis high in CBD (Morgan et al. 2010). Notably, the amount of CBD had no effect on acute psychotomimetic effects, which were elevated in all individuals during intoxication. Finally, it was demonstrated that the memory-impairing effects of cannabis containing high levels of THC persisted beyond the period of intoxication and that higher THC levels in hair were associated with greater depression and anxiety, yet irrespective of CBD levels (Morgan et al. 2012). In line with the above, Schubart and colleagues (2011b) found lower levels of self-reported subclinical positive psychotic but not negative or depressive symptoms in individuals from the general population (N = 1,877) who smoked cannabis containing high levels of CBD. 772 van Winkel · Kuepper CP10CH28-vanWinkel ARI 12 February 2014 14:36 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Interaction with Other Environmental Risk Factors Finally, evidence has emerged recently that environmental risk factors such as early trauma, urbanicity, and cannabis use might interact with each other in increasing psychosis risk (Cougnard et al. 2007). Subclinical psychotic symptoms constitute a common but transitory developmental phenomenon in the general population (van Os et al. 2009). However, common, nonclinical developmental expression of psychosis may become abnormally persistent and eventually translate into psychotic illness when synergistically combined with environmental exposures such as early trauma, growing up in an urban environment, and cannabis use (Cougnard et al. 2007, Dominguez et al. 2011, van Os et al. 2009). In line with this, two cross-sectional studies reported that individuals who were exposed to trauma early in life had a much higher risk to develop psychotic outcomes following adolescent cannabis use compared to those without trauma (Harley et al. 2010, Houston et al. 2008). The interaction between cannabis use and childhood trauma has since been replicated in two independent population-based cohorts making use of longitudinal data (Konings et al. 2012) as well as in two further cross-sectional data sets including 7,403 and 2,355 individuals from the general population, respectively (Houston et al. 2011, Murphy et al. 2013). In contrast, the prospective German Early Developmental Stages of Psychopathology study did not find evidence for an interaction between cannabis use and childhood trauma (Kuepper et al. 2011a). One longitudinal cohort study provided evidence that cannabis use also interacts with urbanicity in increasing psychosis risk by showing that the association between baseline cannabis use and psychotic symptoms at follow-up was much stronger in individuals who grew up in an urban environment than in individuals from rural areas. This effect was independent of baseline cannabis use, age, gender, socioeconomic status, use of other drugs, and childhood trauma (Kuepper et al. 2011b). INSIGHTS FROM NEUROBIOLOGICAL STUDIES In addition to epidemiological studies examining the link between cannabis use and psychosis and the biology of the endocannabinoid system, additional studies examining the effects of cannabinoids on brain development and function may be helpful to explicate why cannabis use would lead to acute psychotic symptoms and even nonaffective psychotic disorders such as schizophrenia. Neurobiology of the Endocannabinoid System Extensive research throughout the past decade has contributed greatly to the understanding of the complex molecular basis and function of the endocannabinoid system (Castillo et al. 2012, Ohno-Shosaku et al. 2012). Two main types of cannabinoid receptors have been identified so far: CB1 receptors, which are predominantly distributed in the brain, and CB2 receptors, which are mainly expressed in peripheral tissues, particularly in the immune system (Pertwee 1997, 2008). Recently, the existence of additional cannabinoid receptors has been suggested (Pertwee 2010); the most thoroughly characterized so far is the GPR55, a G-protein coupled receptor with 13–14% homology with the CB1 receptor and a similar brain distribution (Anavi-Goffer et al. 2012, Ryberg et al. 2007). Expression of CB1 receptors is high in cortical regions, particularly the frontal regions, basal ganglia, cerebellum, hippocampus, amygdala, and substantia nigra pars reticulata (Mackie 2005). CB1 receptors are activated by their endogenous ligands, the endocannabinoids, of which the best characterized are anandamide (N-arachidonoylethanolamine) and 2-arachidonoylglycerol (Devane et al. 1992, Mechoulam et al. 1995). Endocannabinoid signaling has been found to primarily occur in a retrograde fashion, i.e., endocannabinoids are stored and www.annualreviews.org • Cannabis Use and Psychosis 773 ARI 12 February 2014 14:36 released on demand by postsynaptic neurons to activate presynaptic CB1 receptors. Activation of CB1 receptors leads to the presynaptic inhibition of both inhibitory [gamma-aminobutyric acid (GABA)] and excitatory (glutamate) neurotransmitter release (Chevaleyre et al. 2006) as well as manipulation of neuromodulators such as dopamine, noradrenalin, serotonin, and acetylcholine (Lopez-Moreno et al. 2008). It is thought that principal output neurons such as cerebellar Purkinje cells, cortical pyramidal cells, striatal medium spiny neurons, and mesencephalic dopamine neurons fine-tune their excitatory and inhibitory inputs via retrograde endocannabinoid signaling (Chevaleyre et al. 2006). Moreover, by controlling both inhibitory and excitatory neurotransmitter release in regions such as the hippocampus, endocannabinoid-mediated retrograde signaling has been implicated in numerous forms of short- and long-term synaptic plasticity including phenomena such as depolarization-induced suppression of inhibition or excitation and presynaptic forms of long-term depression (LTD). Recently, other, nonretrograde forms of endocannabinoid signaling have also been observed. In nucleus accumbens and hippocampus, N-arachidonoylethanolamine acting at transient receptor potential vanilloid receptor type 1 receptors have been found to modulate postsynaptic forms of LTD (Chavez et al. 2010, Grueter et al. 2010). And in somatosensory cortex, autocrine signaling in the form of slow self-inhibition has been demonstrated at GABAergic interneurons, where 2-arachidonoylglycerol activation of postsynaptic CB1 receptors led to a decrease in its excitability via signaling to a G-protein-coupled inwardly rectifying K+ channel (Bacci et al. 2004, Howlett et al. 2011, Marinelli et al. 2009). Because of its powerful role in fine-tuning synaptic neurotransmission, the endocannabinoid system thus appears to be involved in a wide range of neural functions, including neural development, motor control, cognition, and emotional processing. Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel Effects of THC on the Brain Acute effects. In most individuals, the acute, psychological effects of cannabis include relaxation, sociability, and euphoria, but anxiety, panic attacks, and paranoia also have been reported (Hall & Solowij 1998, Murray et al. 2007). Furthermore, cannabis use has been shown to affect cognitive functioning, in particular mnemonic and executive functioning, as well as psychomotor speed, both acutely and beyond the period of intoxication (Lundqvist 2005, Ranganathan & D’Souza 2006, Solowij & Battisti 2008). Behaviorally, the administration of cannabis and THC has been particularly associated with the induction of psychotomimetic effects, characterized by delusional thinking and hallucinations, closely resembling the symptoms observed in psychosis and schizophrenia. In a double-blind placebo-controlled randomized laboratory study on the acute psychotomimetic effects of THC in 22 healthy cannabis users with average age of 29 years, D’Souza and colleagues (2004) demonstrated that 2.5 mg and 5 mg of intravenously administered THC dose-dependently induced positive and negative psychotic symptoms as well as perceptual alterations, as measured with the Positive and Negative Syndrome Scale (PANSS) and the Clinician-Administered Dissociative Symptom Scale, respectively. THC further impaired neuropsychological functioning, which was most pronounced in the domains of learning and memory (D’Souza et al. 2004). Similar results were obtained by Morrison and colleagues (Morrison & Stone 2011, Morrison et al. 2009), who studied the acute effects of 2.5 mg intravenous THC in 22 healthy males with an average age of 28 years. THC significantly increased scores on the PANSS, including both the positive and negative symptom domain, and worsened performance in the domains of verbal learning, attention, working memory, and reasoning but not verbal fluency. THC-induced cognitive impairment was unrelated to increased scores on the PANSS (Morrison & Stone 2011, Morrison et al. 2009). 774 van Winkel · Kuepper CP10CH28-vanWinkel ARI 12 February 2014 14:36 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Functional neuroimaging studies on the acute effects of THC have demonstrated increased resting activity in several brain areas, including frontal and temporal regions, and increased activation of frontal and anterior cingulate cortex during cognitive processing (Martin-Santos et al. 2010). Animal studies have furthermore demonstrated that acute administration of THC disrupts retrograde signaling underlying endocannabinoid-mediated synaptic plasticity in areas involved in learning and memory, such as nucleus accumbens, amygdala, and hippocampus (Azad et al. 2008, Mato et al. 2004). Chronic effects. Beyond the period of acute intoxication, cannabis use has been shown to affect not only psychotic symptoms but also neurocognitive function. Solowij and colleagues (2002) showed in a multisite study including a total of 102 heavy cannabis users and 33 controls that cannabis users performed significantly worse than nonusers on a number of tests measuring attention and memory. Furthermore, there was a significant association with duration of use, with long-term users performing worse than shorter-term users (Solowij et al. 2002). More recently, deficits in sensory gating (Broyd et al. 2013) and directed attention and cognitive flexibility (Battisti et al. 2010) were demonstrated in chronic cannabis users. Again, the effects were more pronounced with longer duration of cannabis use and earlier onset of use, supporting the notion that longterm cannabis use leads to impairments in cognitive functioning that endure beyond the period of intoxication and worsen with increasing years of use. A study in rats demonstrated that hippocampal synaptic plasticity is disrupted for up to 14 days after THC administration (Hoffman et al. 2007). Furthermore, it has been shown that rats that were chronically treated with THC during postnatal days 35 to 45 showed alterations in hippocampal neuroplasticity, including lower total dendritic length and number and reduced spine density, in adulthood compared to vehicletreated animals (Rubino et al. 2009). Thus, THC seems to affect brain processes by disrupting endocannabinoid-mediated synaptic plasticity in brain regions that are critical for learning and memory. Whether the neurocognitive effects of chronic long-term use are reversible is unclear; some level of neuropsychological impairment has been detected in abstinent users (Meier et al. 2012, Solowij 1995). In patients with psychosis, however, recent meta-analyses reported better cognition in cannabis-using patients (Rabin et al. 2011, Yücel et al. 2012). It has been hypothesized that persons who develop a psychotic disorder in the absence of cannabis use have greater neurodevelopmental vulnerability compared to their cannabis-using counterparts who, under the influence of cannabis may have developed psychosis that they would not have developed in the absence of use (Yücel et al. 2012). A systematic review of imaging studies published before January 2009 concluded that the evidence for structural brain abnormalities in cannabis users was minimal, as only three out of eight included studies found significant differences between users and controls (Martin-Santos et al. 2010). Yet more recent evidence does suggest cannabis-related changes in the brain morphology of chronic users, including reduced hippocampal volume and cerebellar white matter (Demirakca et al. 2011; Solowij et al. 2011, 2013). Some studies further suggest that these changes happen dose dependently and are related to early age of onset of use (Arnone et al. 2008, Wilson et al. 2000, Yücel et al. 2008). A study of patients with psychosis, their unaffected siblings, and healthy controls furthermore revealed decreases in cortical thickness associated with cannabis use in the patients and the unaffected siblings but not the healthy controls (Habets et al. 2011). This result is in agreement with the widespread idea that familial risk and cannabis use act synergistically to increase risk for psychosis, and it suggests that increased risk may be mediated by brain structural alterations. Interestingly, evidence from early animal studies also suggests that contextual factors such as environmental stress alter the brain’s response to THC (Littleton et al. 1976, MacLean & Littleton 1977, Mokler et al. 1987). www.annualreviews.org • Cannabis Use and Psychosis 775 CP10CH28-vanWinkel ARI 12 February 2014 14:36 Effects of CBD on the Human Brain in Interaction with THC Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. As mentioned previously in this review, THC and CBD differ in their effects on brain function and mental health. In line with this, functional neuroimaging studies have demonstrated distinctive and in part opposing effects of THC and CBD on brain activation during cognitive and emotional processing in various regions of the brain including the hippocampus, amygdala, temporal and occipital cortex, and anterior cingulate (Bhattacharyya et al. 2010, 2012; Borgwardt et al. 2008; Fusar-Poli et al. 2009, 2010; Winton-Brown et al. 2011). Furthermore, pretreatment with CBD was shown to prevent the behaviorally observed psychotomimetic and anxiogenic effects of THC (Bhattacharyya et al. 2010, Fusar-Poli et al. 2010), the latter possibly by disrupting the neural connectivity between amygdala and anterior cingulate cortex (Fusar-Poli et al. 2010). In line with these findings are the results of a recent laboratory study showing that pretreatment with CBD inhibited acute THC-induced psychotic symptoms as well as THC-induced cognitive impairment (Englund et al. 2013). Interestingly, CBD has recently been suggested to also protect against the long-term effects of THC on brain structure: Compared to nonusing controls, users of highCBD/low-THC strains of cannabis showed a lesser reduction in hippocampal volume than users of high-THC/low-CBD cannabis preparations (Demirakca et al. 2011). Cannabis Use and the Dopamine System Based on animal research showing that THC increases dopamine levels in several regions of the brain including striatal and prefrontal areas (El Khoury et al. 2012), neurochemical interactions between cannabinoids and dopamine have been hypothesized to constitute a neurobiological link between cannabis and psychosis (Kuepper et al. 2010, Morrison & Murray 2009). An early single-photon emission computed tomography study on dopaminergic alterations in schizophrenia by chance found evidence for increased dopamine release in the striatum following cannabis exposure in a single patient who violated the study protocol by smoking marijuana in-between two scans (Voruganti et al. 2001). This acute effect of cannabis on striatal dopamine release was later replicated by Bossong and colleagues (2009), who administered 8 mg of pulmonary THC to seven healthy males with recreational cannabis use. Using positron emission tomography (PET) and [11 C]raclopride, the researchers observed an up to 4.1% decrease in nondisplaceable binding potential (BPND ) in the THC condition compared to placebo condition. The effect was most pronounced in ventral striatum, dorsal putamen, and caudate nucleus. In contrast, Stokes and colleagues (2009) as well as Barkus and colleagues (2011), who investigated acute effects of THC on striatal dopamine neurotransmission using PET in combination with [11 C]raclopride and singlephoton emission tomography with [123 I]IBZM, respectively, did not observe significant dopamine release after the experimental THC challenge. Yet significant decreases in BPND measured with PET and [11 C]raclopride were observed in cortical brain regions, in particular in right middle frontal gyrus, left superior frontal gyrus, and left superior temporal gyrus (Stokes et al. 2010). Recently, acute THC-induced dopamine response was measured for the first time in patients with psychotic disorder, unaffected first-degree relatives, and healthy controls, who were all frequent cannabis users (Kuepper et al. 2013). In line with most previous findings, no dopamine release associated with the administration of THC was detected in healthy controls. Yet in patients and relatives, THC did induce significant amounts of dopamine release, most pronounced in the caudate nucleus. Although the sample size was small (seven patients, eight relatives, and nine healthy controls), this study provides further preliminary evidence for an interaction between THC and familial liability for psychosis from the neurobiological perspective. 776 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 Other studies have investigated the involvement of the dopamine system in the effects of cannabis use by examining different parameters of dopamine neurotransmission in chronic cannabis users. Stokes and colleagues (2012) measured the availability of striatal dopamine D2-like receptors in 10 cannabis users and 10 controls. They did not find any difference in BPND between cannabis users and nonusers. Neither did BPND correlate with lifetime frequency of cannabis use (Stokes et al. 2012). Bloomfield and colleagues (2013) investigated presynaptic dopamine synthesis capacity—a parameter that has been found to be increased in schizophrenia and prodromal states (Egerton et al. 2013, Howes et al. 2012)—in 19 regular cannabis users. However, cannabis use was not associated with elevated striatal dopamine synthesis capacity. In fact, the opposite was found. Dopamine synthesis capacity was negatively correlated with cannabis use, and cannabis users showed reduced dopamine synthesis capacity in associative and limbic striatum (Bloomfield et al. 2013). Two other studies examined dopamine release in response to a psychosocial stress challenge and a pharmacological amphetamine challenge, respectively, in chronic cannabis users and nonusing controls (Mizrahi et al. 2013, Urban et al. 2012). Both studies reported negative results; that is, a history of cannabis use was not associated with increased dopamine release in response to either amphetamine (Urban et al. 2012) or psychosocial stress (Mizrahi et al. 2013). INSIGHTS FROM GENETIC STUDIES A final source of information on the link between psychosis and cannabis is genetic studies, which may be particularly helpful in explaining why some individuals develop psychosis following cannabis use while most do not. Genetic factors are assumed to play a pivotal role in determining sensitivity to the psychosis-inducing effects of cannabis. When the effect of an environmental factor is influenced by genetic factors, this is usually referred to as gene-environment interaction (van Winkel et al. 2010) (Figure 1). Most commonly, this takes the form of increased risk after exposure to an environmental risk factor in those with genetic predisposition, versus a small to absent increase in risk after environmental exposure in those without a genetic predisposition (a quantitative or fan-shaped interaction). It is also possible, however, that the environmental factor has opposite effects dependent on the underlying genotype, which is referred to as a qualitative or cross-over interaction. Gene-environment interaction can be examined at the omnibus level using an overall measure of genetic risk, such as familial loading, psychometric risk, or polygenic risk scores derived from genome-wide association studies (Purcell et al. 2009), or at the level of specific genes or single-nucleotide polymorphisms (SNPs). Usually, the possibility of gene-environment interaction is examined at the omnibus level before hypotheses relating to specific genetic markers are tested (Decoster et al. 2012). The use of familial risk as a proxy of psychosis liability is based on the observation that the risk to develop a psychotic disorder increases as the degree of genetic affinity with an affected family member increases. In addition to familial risk, some researchers have used psychometric psychosis liability as a proxy for the underlying genetic vulnerability. Psychometric psychosis liability refers to the level of subtle psychotic experiences, which are seen as the behavioral expression of genetic vulnerability in unaffected individuals. Earlier research argues that psychometric psychosis liability in the general population reflects a genetic liability that is consistent with the genetic vulnerability in patients (Decoster et al. 2012). However, this approach assumes early, subtle psychotic experiences to be the result of only genetic predisposition, which is unlikely. Furthermore, it cannot take into account underlying genetic heterogeneity and assumes genetic risk to be equal across different individuals with these experiences. Therefore, we focus on studies using familial risk as the measure of genetic loading; for an overview of studies using psychometric risk as the measure of genetic loading, see Decoster et al. (2012). www.annualreviews.org • Cannabis Use and Psychosis 777 CP10CH28-vanWinkel ARI 12 February 2014 14:36 Evidence for G×E: Omnibus Approach Using Familial Risk Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. A number of studies have investigated whether unaffected individuals who have a family member with psychosis are more sensitive to the effects of cannabis use than are healthy controls. Hollis and colleagues (2008) compared mental health functioning in relation to cannabis use in three groups of young people: 36 nonpsychotic siblings of patients with schizophrenia, 25 patients with ADHD, and 72 healthy controls. In this study, an association between cannabis use and schizotypal symptoms was specific for the group at familial risk for psychosis, suggesting that this subgroup was particularly vulnerable to the detrimental effects of cannabis use (Hollis et al. 2008). In addition, the Genetic Risk and Outcome in Psychosis (GROUP) Investigation (2011) demonstrated an increased sensitivity to the psychosis-inducing effects of cannabis associated with familial risk for psychosis, using a sibling-control and cross-sibling design (participants included 1,120 patients with psychotic disorder, 1,057 siblings of these patients, and 590 community controls) [Genetic Risk Outcome Psychos. (GROUP) Investig. 2011]. These results were recently supported by novel patient-sibling (978 pairs; 1,723 observations) and parent-sibling (669 pairs; 1,222 observations) analyses of the same sample, using data from the baseline assessment as well as the three-year follow-up assessment, which showed that the familial correlation in psychosis-related experiences was significantly stronger in siblings exposed to cannabis use [van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. 2013]. Candidate Gene Studies Caspi and colleagues were the first to report an interaction between cannabis use and a specific genetic marker in its effect on the risk for psychotic disorder (Caspi et al. 2005). Their study focused on a functional polymorphism (Val158Met or rs4680) in the catechol-O-methyltransferase (COMT ) gene. COMT is an enzymatic inactivator of dopamine and other monoamines and is essential for dopamine signaling in the prefrontal cortex. The Val allele is associated with a 40% higher enzyme activity (Chen et al. 2004). The authors reported that the COMT polymorphism moderated the risk of developing schizophreniform disorder at age 26 following adolescent-onset cannabis use in a birth cohort of 1,037 individuals, with Val carriers displaying a more than 10 times higher risk (Caspi et al. 2005). Since its original publication, this study has been cited more than 500 times (Web of Science; accessed July 1, 2013), and researchers from different groups worldwide have attempted to replicate this finding, with mixed results (Decoster et al. 2012). To put these observations into perspective, a recent critical review by Duncan & Keller (2011) of observational studies in the field of candidate gene-environment interactions (cG×E) in psychiatry should be considered. Duncan and Keller compared the rate of positive (i.e., significant) results among studies reporting novel findings to the rate among replication attempts, following the reasoning that replication attempts should have a higher rate of significant findings because both positive and negative findings should be of interest to the general public, whereas for novel reports, significant results will be most publishable (Duncan & Keller 2011). However, the observed pattern was opposite of the one expected: 96% of novel cG×E reports were significant in comparison with 27% of replication attempts, which is strongly suggestive of publication bias. Second, the authors considered the sample sizes of replication efforts: In the absence of publication bias, larger sample sizes should provide more statistical power than smaller ones and thus should be more likely to produce significant findings (assuming the same effect size). Again, the observed pattern was the exact opposite: the median sample size of the 10 positive replication attempts was 154 in comparison with 377 for the negative replication attempts, which suggests that larger replication attempts were published irrespective of the results (significant or not), whereas smaller studies 778 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 were preferentially published when they yielded significant results. A third consideration is the definition of what constitutes replication: In a series of simulations of genetic associations, Sullivan (2007) showed that the rate of false-positive findings can be very high (up to 96%) when using broad definitions of replication, whereas when using precise definitions, false discovery rates were much lower, especially in combination with more stringent levels of statistical significance. Therefore, in considering the evidence base for a particular cG×E, Duncan & Keller (2011) conclude that it is important that only direct replications are considered; only when a cG×E is supported by a number of direct replications can indirect replications help to gauge the generalizability of the original finding. Given this conclusion, we distinguish between studies that attempt to directly replicate the original finding of Caspi and colleagues (replication studies) and studies examining COMT×cannabis interaction in other phenotypes relevant to psychosis (validation studies). The results are sobering: Whereas almost all of the validation studies report significant interaction, there is not a single attempt at replication showing significant replication in the expected direction (Table 1). Recently, groups from Spain and the Netherlands have independently reported a three-way interaction between cannabis use, childhood adversity, and the COMT Val158Met genotype using epidemiological designs (Alemany et al. 2014, Vinkers et al. 2013). The Dutch group also reported results from an attempt at replication; although this attempt failed in terms of statistical significance, the effect was in the same direction (Vinkers et al. 2013). A few papers have examined possible interactions with candidate markers other than COMT Val158Met. Given the recommendations of Duncan & Keller (2011), we consider only genetic markers for which human observational studies assessing possible effects on the clinical disorder phenotype are available. Zammit and colleagues (2007) used a case-only design to examine a possible interaction between cannabis use and two other SNPs in COMT (rs737865 and rs165599) as well as an interaction between cannabis and rs1049353 in the CNR1 gene. There was no evidence for gene-environment interaction for any of these SNPs (Zammit et al. 2007), nor was evidence found that COMT Val158Met interacts with cannabis use, as reported in Table 1. van Winkel and the GROUP investigators examined a broader selection of a priori defined candidate genes including 152 SNPs selected from 42 candidate genes (including COMT Val158Met) [van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. 2011]. They first examined interactions between these markers and recent cannabis use in 740 unaffected siblings of patients with schizophrenia, following the reasoning that a number of disease-related confounding mechanisms may be reduced by studying the effects of recent use in individuals at risk, such as stress associated with emerging psychotic symptoms, changes in patterns of use, or treatment with antipsychotics, whereas the clinical relevance of identified interactions may be subsequently confirmed by selective follow-up in the patients [van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. 2011]. Three SNPs showed evidence for interaction with cannabis at the Bonferroni threshold of statistical significance in the unaffected siblings, situated in AKT1 (two SNPs) and LRRTM1 (one SNP). Follow-up of these SNPs in the patients confirmed the presence of gene-environment interaction between rs2494732 in AKT1 and cannabis using case-only (801 patients with psychotic disorder), case-sibling, and case-control (419 unrelated controls) designs. Compared to those with the T/T genotype, individuals with a C/C genotype displayed a twofold-increased risk of being diagnosed with a psychotic disorder after having used cannabis [van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. 2011]. A recent case-control study of an independent sample of 489 patients and 278 controls from the United Kingdom supported an interaction between rs2494732 in AKT1 and cannabis (Di Forti et al. 2012); indirect evidence supporting this interaction was also found at the level of AKT1-dependent prefrontal functioning under the influence of cannabis, as measured by the Continuous Performance Test (van Winkel et al. 2011). www.annualreviews.org • Cannabis Use and Psychosis 779 CP10CH28-vanWinkel ARI 12 February 2014 14:36 Table 1 Studies following up the finding of COMT Val158Met interaction with cannabis on phenotypes relevant to psychosis, distinguishing between direct replication studies and indirect validation studies Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Replication studies Indirect validation in humans Outcome Indirect validation in animal models Outcome Outcome Zammit et al. (2007) case-only study Negative Henquet (2006) Acute effects of experimental cannabis exposure on psychotic symptoms and cognition Positiveb O’Thuathaigh (2010) COMT KO mice exposed to THC: impact on behavioral phenotypes Negatived Kantrowitz (2009) case-only study Negative Henquet (2009) Psychotic symptoms after cannabis use in daily life Positiveb O’Thuathaigh (2012) COMT KO mice exposed to cannabinoid WIN55212: impact on behavioral phenotypes and prepulse inhibition Negatived Gutiérrez (2009) case-control study Negative Pelayo-Teran (2010) Age at onset of psychosis and duration of untreated psychosis Positivec Behan (2012) COMT KO mice exposed to THC: impact on dopamine cell size in VTA, CB1R expression in hippocampus, and parvalbumin cell size in prefrontal cortex Negatived Costas (2011) case-only study Negativea Estrada (2011) Age at onset of psychosis Positive – – Zammit (2011) birth cohort study Negative van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. (2011) Subclinical symptoms in unaffected siblings following recent cannabis use Negative – – – – Verdejo-Garcia (2013) Executive functioning in cannabis users versus healthy controls Positive – – – – Batalla (2013) Structural magnetic resonance imaging study in cannabis users and controls Positive – – a The authors found a significant association but with opposite directionality (association with the Met rather than the Val allele). Conditional on psychometric psychosis liability. c Genotype differences were significantly different in nonusers but not in users of cannabis. d COMT KO mice were consistently (and significantly) more vulnerable to the adverse effects of cannabinoids than wild-type mice, in contrast to expectations (the Val allele in humans is associated with higher enzymatic function, whereas COMT KO leads to loss of enzymatic function). Abbreviations: CB1R, cannabinoid receptor 1; COMT, catechol-O-methyltransferase; KO, knockout; THC, tetrahydrocannabinol; VTA, ventral tegmental area. b 780 van Winkel · Kuepper CP10CH28-vanWinkel ARI 12 February 2014 14:36 Table 2 Studies following up the finding of AKT1 rs2494732 interaction with cannabis on phenotypes relevant to psychosis, distinguishing between direct replication studies and indirect validation studies Replication studies Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Di Forti et al. (2012) case-control study Outcome Positive Indirect validation in humans Outcome Indirect validation in animal models Outcome van Winkel & Genetic Risk Outcome Psychos. (GROUP) Investig. (2011) Subclinical symptoms in unaffected siblings following recent cannabis use Positive – – van Winkel et al. (2011) Cognition (assessed with Cognitive Performance Test) in patients with psychotic disorder Positive – – Nevertheless, further efforts at replication and indirect validation are necessary because the currently available evidence base is still relatively small (Table 2). FACTS, CONTROVERSIES, AND MYTHS IN THE CANNABIS-PSYCHOSIS RELATIONSHIP A large body of work relevant to the cannabis-psychosis relationship has been published; the present review focuses on studies in the field of epidemiology, neurobiology, and genetics. What are the most important and reliable findings from this literature that may help to gain further insight in the underlying mechanisms relating cannabis to psychosis? In order to answer this question, we graded the available evidence using the number of studies published and the consistency of the reported results as well as the degree to which different research fields (i.e., epidemiological, neurobiological, and genetics) converge on similar findings (Table 3). This categorization could then be used as different pieces of the puzzle, which can be combined into a developmental model relating cannabis use to risk of psychosis (Figure 2). Compiling the Evidence Cannabis use is associated with psychosis, but most people do not develop psychosis following (prolonged periods of ) cannabis use. A first factor that needs to be considered is the type of cannabis that is consumed, in particular the balance between THC and CBD in the different available varieties, as there is good evidence that the THC/CBD ratio is an important factor in determining the psychotogenic properties of cannabis (evidence grade A). Furthermore, a number of robust findings indicate the existence of vulnerable subpopulations and/or time windows. Observational studies, as well as experimental animal studies, have shown that adolescence is a particularly vulnerable period in terms of the psychosis-inducing effects of cannabis (evidence grade A+). Although on average the duration of cannabis use is longer in people who start using at a younger age, there is good evidence from long-term observational studies, as well as studies in adult animals, that duration of use per se is not responsible for the particularly strong association with cannabis use in adolescence. In addition, observational and animal studies have shown that subgroups exposed to early life stress, such as growing up in an urban environment or exposure to childhood trauma, or, in rats, experiencing isolation and food deprivation, increases vulnerability to the effects of cannabis (evidence grade B). Finally, familial www.annualreviews.org • Cannabis Use and Psychosis 781 782 van Winkel · Kuepper NB NB NB G, NB G, NB G − − − ++ +/− + Cannabis use impacts dopamine D2 receptor availability Cannabis use is associated with increased dopamine synthesis capacity Cannabis use is associated with increased striatal dopamine response to a challenge with amphetamine or stress Individuals at familial risk are more sensitive to the psychosis-inducing effects of cannabis COMT Val158Met is an important genetic risk factor for cannabis-induced psychosis AKT1 rs2494732 is an important genetic risk factor for cannabis-induced psychosis B C A D D D C C C C C C C A+ A B a Statements were rated independently by the authors of the present review for their consistency of evidence, evidence from multiple fields of investigation, and grade of evidence. In the case of disagreements, categorizations were discussed until consensus was reached. b Definitions applied: +++, considerable number of studies with consistent results; ++, considerable number of studies with largely consistent results or a reasonable number of studies (more than three) with consistent results; +, a small number of studies (at least two) with consistent results or a reasonable number of studies (more than three) with largely consistent results; +/−, several studies available but with mixed results or only one study reporting a given finding; −, no positive evidence available. c Definitions applied: A+, consistent evidence from several studies and multiple fields; A, consistent evidence from multiple studies from one field of investigation and absence of conflicting evidence from other fields; B, consistent evidence from some studies in one or more fields of investigation; C, conflicting evidence within one field of investigation or between different fields of investigation, or only one study available reporting a significant finding; D, most studies reporting negative results in one or more fields of investigation. Abbreviations: CBD, cannabidiol; COMT, catechol-O-methyltransferase; KO, knockout; THC, tetrahydrocannabinol. NB NB +/− +/− Cannabis use induces striatal dopamine release in individuals at familial risk for psychosis Cannabis use is associated with specific brain tissue loss in cerebellum Cannabis use induces striatal dopamine release NB NB +/− +/− Cannabis use is associated with specific brain tissue loss in hippocampus NB NB +/− +/− Cannabis use is associated with brain tissue loss, especially in individuals at familial risk for psychosis E, NB +/− Cannabis has enduring negative effects on cognition, even in the absence of current use A+ A 12 February 2014 Cannabis use is associated with generalized brain tissue loss NB E, NB +++ + There is a synergistic interaction between early life stress and cannabis use to increase psychosis risk +++ E, NB ++ The balance between THC and CBD is a critical factor Cannabis affects cognitive ability in the short term E, NB E, NB +++ The younger the age at onset of use, the higher the risk Evidence gradec ARI THC interferes with processes regulating synaptic plasticity Evidence from multiple fields of investigation: epidemiology (E), neurobiology (NB), genetics (G) Consistency of evidenceb Statement Table 3 Facts, controversies, and myths relevant to the association between cannabis use and psychosisa Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel 14:36 CP10CH28-vanWinkel ARI 12 February 2014 14:36 a Synaptic plasticity Minimal or no structural or functional changes Critical neurodevelopment Cannabis use 15 20 25 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Age b Environmental risk Familial risk ? Synaptic plasticity Increased striatal dopamine release? Structural brain changes? Psychosis Critical neurodevelopment Cannabis use 15 20 25 Age Figure 2 (a) Typical timeline of a person for whom cannabis use is relatively benign. Cannabis use (indicated by the green bar) is initiated after the most critical time window in adolescence, where important neurodevelopmental processes take place (indicated by the blue bar). Tetrahydrocannabinol (THC) exposure is moderate in terms of relatively low TCH/cannabidiol (CBD) ratio and/or frequency and duration of exposure. In the absence of high genetic risk and in the absence of environmental risk factors such as childhood trauma, this type of exposure to cannabis in most cases does not lead to psychotic outcomes, and long-term alterations of brain structure and cognition are probably minimal or absent. (b) Typical timeline of a person for whom cannabis use may be a causal factor in the development of psychotic disorder. Cannabis use (indicated by the green bar) is initiated before or during the most critical time window in adolescence, where important neurodevelopmental processes take place (indicated by the blue bar). THC exposure is severe (as indicated by the more intense color of the green bar) in terms of a relatively high THC/CBD ratio and/or greater frequency and duration of exposure. This type of exposure in itself may already lead to onset of psychotic symptoms, and this effect may be even more pronounced in the presence of familial/genetic or environmental risk. There is preliminary evidence that in such vulnerable subgroups, neurodevelopment brain processes may go awry, leading to brain alterations associated with psychosis, such as sensitization of striatal dopamine release and selective (e.g., hippocampal) or generalized structural alterations. It is not known whether familial and environmental risk exert their hypothesized effects via inducing more intense alterations in synaptic plasticity following cannabis use (dashed red arrows) or via an increased sensitivity to structural or functional alterations associated with cannabis-induced changes in synaptic plasticity (solid red arrows). www.annualreviews.org • Cannabis Use and Psychosis 783 ARI 12 February 2014 14:36 and genetic factors (evidence grade A), possibly including the AKT1 rs2494732 polymorphism (evidence grade B), are contributing factors in determining sensitivity to the psychosis-inducing effects of cannabis. Although these findings identify vulnerable subgroups, which may give indirect hints about the underlying biology of cannabis-induced psychosis, studies trying to tie cannabis use to specific biological mechanisms have been largely unsuccessful. Currently no robust evidence indicates that cannabis use leads to abnormalities in dopaminergic neurotransmission or to generalized or specific brain tissue loss. What has been established is that administration of THC interferes with processes regulating synaptic plasticity (evidence grade A). Authors have hypothesized how disruption of synaptic plasticity by THC may induce developmental brain alterations that ultimately may lead to psychosis (Bossong & Niesink 2010, Morrison & Murray 2009). Bossong & Niesink (2010) propose that exposure to THC in adolescence disrupts the normal process of fine-tuning of glutamate and GABA release by the endocannabinoid system, thereby adversely impacting brain maturational processes occurring in adolescence, especially with regard to prefrontal neural circuitries. Another theory is based on the observation that dopamine, adenosine, and the endocannabinoid system work together to gate input from the cortex to the striatum, thus regulating implicit learning. Given the essential role of striatal endocannabinoid signaling in habit formation and implicit learning, excessive stimulation of the endocannabinoid system by THC might favor connections between logically unrelated ideas, ultimately resulting in delusion formation (Morrison & Murray 2009). These theories link disruption of the long-term potentiation/LTD balance caused by excessive stimulation of the endocannabinoid system to processes of adolescent brain maturation and dopamine-dependent striatal learning. Although these theories are appealing, human studies have failed to consistently show a disruption of dopamine neurotransmission or developmental brain alterations associated with the use of cannabis (Table 3). It is important to note, however, that these studies have typically been conducted in healthy adult volunteers with limited previous exposure to cannabis, or in long-term cannabis users without frank psychotic symptoms, whereas the epidemiological evidence suggests that such processes mainly occur in certain vulnerable subpopulations (Figure 2). The few studies that have been conducted in such populations are suggestive of (a) significant dopamine release following administration of THC in persons at familial risk for schizophrenia (patients as well as their first-degree relatives) but not in healthy controls (Kuepper et al. 2013) and (b) significantly reduced cortical thickness associated with a history of cannabis use in persons at familial risk but not in healthy controls (Habets et al. 2011). Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel Recommendations for Future Research The above findings indicate a number of gaps in knowledge that are in need of further scientific investigation. A first important aspect is the possible correlation between genetic risk for psychosis and exposure to cannabis. Although it seems unlikely that gene-environment correlation entirely explains the association between cannabis and psychosis, examination of this issue is necessary before causality can be more confidently assumed. In addition, a better understanding of the exact mechanisms through which THC and CBD act on the endocannabinoid system, and how this in turn affects adolescent brain development and brain function, is necessary. The actions of CBD in particular remain insufficiently understood. Although having only low affinity for the CB1 and CB2 receptor, CBD seems be a powerful antagonist of CB1 and CB2 receptor agonists (Pertwee 2008). Preliminary data further suggest that CBD may exert its effects by inhibiting reuptake of the endogenous cannabinoid anandamide (Mechoulam et al. 2002, Pertwee 2008). 784 van Winkel · Kuepper CP10CH28-vanWinkel ARI 12 February 2014 14:36 The results also suggest that specific examination of vulnerable subgroups—be it based on genetic risk or on environmental risk—may yield valuable information on differential vulnerability to long-term brain alterations relevant for psychosis. Central to possible long-term brain alterations may be THC-induced changes of synaptic plasticity; how these processes are influenced by genetic risk or early childhood exposure to relevant stressors is likely to be very important (Figure 2). Likewise, further delineation of the time window in which these changes take place is likely to provide valuable information. DISCLOSURE STATEMENT Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review. LITERATURE CITED Alemany S, Arias B, Fatjo-Vilas M, Villa H, Moya J, et al. 2014. Psychosis-inducing effects of cannabis are related to both childhood abuse and COMT genotypes. Acta Psychiatr. Scand. 129:54–62 Anavi-Goffer S, Baillie G, Irving AJ, Gertsch J, Greig IR, et al. 2012. Modulation of L-alphalysophosphatidylinositol/GPR55 mitogen-activated protein kinase (MAPK) signaling by cannabinoids. J. Biol. Chem. 287:91–104 Arnold JC, Boucher AA, Karl T. 2012. The yin and yang of cannabis-induced psychosis: the actions of (9)tetrahydrocannabinol and cannabidiol in rodent models of schizophrenia. Curr. Pharm. Des. 18:5113–30 Arnone D, Barrick TR, Chengappa S, Mackay CE, Clark CA, Abou-Saleh MT. 2008. Corpus callosum damage in heavy marijuana use: preliminary evidence from diffusion tensor tractography and tract-based spatial statistics. NeuroImage 41:1067–74 Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE. 2002. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 325:1212–13 Azad SC, Kurz J, Marsicano G, Lutz B, Zieglgansberger W, Rammes G. 2008. Activation of CB1 specifically located on GABAergic interneurons inhibits LTD in the lateral amygdala. Learn. Mem. 15:143–52 Bacci A, Huguenard JR, Prince DA. 2004. Long-lasting self-inhibition of neocortical interneurons mediated by endocannabinoids. Nature 431:312–16 Barkus E, Morrison PD, Vuletic D, Dickson JC, Ell PJ, et al. 2011. Does intravenous 9-tetrahydrocannabinol increase dopamine release? A SPET study. J. Psychopharmacol. 25:1462–68 Batalla A, Soriano-Mas C, Lopez-Sola M, Torrens M, Crippa JA, et al. 2013. Modulation of brain structure by catechol-o-methyltransferase Val(158)Met polymorphism in chronic cannabis users. Addict. Biol. In press. doi:10.1111/adb.12027 Battisti RA, Roodenrys S, Johnstone SJ, Pesa N, Hermens DF, Solowij N. 2010. Chronic cannabis users show altered neurophysiological functioning on Stroop task conflict resolution. Psychopharmacology 212:613–24 Behan A, Hryniewiecka M, O’Tuathaigh CM, Kinsella A, Cannon M, et al. 2012. Chronic adolescent exposure to delta-9-tetrahydrocannabinol in COMT mutant mice: impact on indices of dopaminergic, endocannabinoid and GABAergic pathways. Neuropsychopharmacology 37:1773–83 Bhattacharyya S, Crippa JA, Allen P, Martin-Santos R, Borgwardt S, et al. 2012. Induction of psychosis by 9tetrahydrocannabinol reflects modulation of prefrontal and striatal function during attentional salience processing. Arch. Gen. Psychiatry 69:27–36 Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, et al. 2010. Opposite effects of -9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 35:764–74 Bloomfield MA, Morgan CJ, Egerton A, Kapur S, Curran HV, Howes OD. 2013. Dopaminergic function in cannabis users and its relationship to cannabis-induced psychotic symptoms. Biol. Psychiatry. In press Borgwardt SJ, Allen P, Bhattacharyya S, Fusar-Poli P, Crippa JA, et al. 2008. Neural basis of -9tetrahydrocannabinol and cannabidiol: effects during response inhibition. Biol. Psychiatry 64:966–73 www.annualreviews.org • Cannabis Use and Psychosis 785 ARI 12 February 2014 14:36 Bossong MG, Niesink RJ. 2010. Adolescent brain maturation, the endogenous cannabinoid system and the neurobiology of cannabis-induced schizophrenia. Prog. Neurobiol. 92:370–85 Bossong MG, van Berckel BN, Boellaard R, Zuurman L, Schuit RC, et al. 2009. Delta 9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology 34:759–66 Broyd SJ, Greenwood LM, Croft RJ, Dalecki A, Todd J, et al. 2013. Chronic effects of cannabis on sensory gating. Int. J. Psychophysiol. 89:381–89 Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, et al. 2005. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol. Psychiatry 57:1117–27 Castillo PE, Younts TJ, Chavez AE, Hashimotodani Y. 2012. Endocannabinoid signaling and synaptic function. Neuron 76:70–81 Chavez AE, Chiu CQ, Castillo PE. 2010. TRPV1 activation by endogenous anandamide triggers postsynaptic long-term depression in dentate gyrus. Nat. Neurosci. 13:1511–18 Chen J, Lipska BK, Halim N, Ma QD, Matsumoto M, et al. 2004. Functional analysis of genetic variation in catechol-O-methyltransferase (COMT): effects on mRNA, protein, and enzyme activity in postmortem human brain. Am. J. Hum. Genet. 75:807–21 Chevaleyre V, Takahashi KA, Castillo PE. 2006. Endocannabinoid-mediated synaptic plasticity in the CNS. Annu. Rev. Neurosci. 29:37–76 Costas J, Sanjuan J, Ramos-Rios R, Paz E, Agra S, et al. 2011. Interaction between COMT haplotypes and cannabis in schizophrenia: a case-only study in two samples from Spain. Schizophr. Res. 127:22–27 Cougnard A, Marcelis M, Myin-Germeys I, De Graaf R, Vollebergh W, et al. 2007. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness-persistence model. Psychol. Med. 37:513–27 Cross-Disord. Group Psychiatr. Genomics Consort., Smoller JW, Craddock N, Kendler KS, Lee PH, et al. 2013. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381:1371–79 D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, et al. 2004. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29:1558–72 Decoster J, Van Os J, Myin-Germeys I, De Hert M, van Winkel R. 2012. Genetic variation underlying psychosis-inducing effects of cannabis: critical review and future directions. Curr. Pharm. Des. 18:5015– 23 Demirakca T, Sartorius A, Ende G, Meyer N, Welzel H, et al. 2011. Diminished gray matter in the hippocampus of cannabis users: possible protective effects of cannabidiol. Drug Alcohol Depend. 114:242–45 Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, et al. 1992. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258:1946–49 Di Forti M, Iyegbe C, Sallis H, Kolliakou A, Falcone A, et al. 2012. Confirmation that the AKT1 (rs2494732) genotype influences the risk of psychosis in cannabis users. Biol. Psychiatry 72:811–16 Dominguez MD, Wichers M, Lieb R, Wittchen HU, van Os J. 2011. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr. Bull. 37:84–93 Duncan LE, Keller MC. 2011. A critical review of the first 10 years of candidate gene-by-environment interaction research in psychiatry. Am. J. Psychiatry 168:1041–49 Egerton A, Chaddock CA, Winton-Brown TT, Bloomfield MA, Bhattacharyya S, et al. 2013. Presynaptic striatal dopamine dysfunction in people at ultra-high risk for psychosis: findings in a second cohort. Biol. Psychiatry 74:106–12 Ehrenreich H, Rinn T, Kunert HJ, Moeller MR, Poser W, et al. 1999. Specific attentional dysfunction in adults following early start of cannabis use. Psychopharmacology 142:295–301 El Khoury MA, Gorgievski V, Moutsimilli L, Giros B, Tzavara ET. 2012. Interactions between the cannabinoid and dopaminergic systems: evidence from animal studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 38:36–50 Englund A, Morrison PD, Nottage J, Hague D, Kane F, et al. 2013. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J. Psychopharmacol. 27:19–27 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel 786 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 Estrada G, Fatjó-Vilas M, Muñoz MJ, Pulido G, Miñano MJ, et al. 2011. Cannabis use and age at onset of psychosis: further evidence of interaction with COMT Val158Met polymorphism. Acta Psychiatr. Scand. 123:485–92 Ferdinand RF, Sondeijker F, van der Ende J, Selten JP, Huizink A, Verhulst FC. 2005. Cannabis use predicts future psychotic symptoms, and vice versa. Addiction 100:612–18 Fergusson DM, Horwood LJ, Swain-Campbell NR. 2003. Cannabis dependence and psychotic symptoms in young people. Psychol. Med. 33:15–21 Fusar-Poli P, Allen P, Bhattacharyya S, Crippa JA, Mechelli A, et al. 2010. Modulation of effective connectivity during emotional processing by 9-tetrahydrocannabinol and cannabidiol. Int. J. Neuropsychopharmacol. 13:421–32 Fusar-Poli P, Crippa JA, Bhattacharyya S, Borgwardt SJ, Allen P, et al. 2009. Distinct effects of 9tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch. Gen. Psychiatry 66:95–105 Genetic Risk Outcome Psychos. (GROUP) Investig. 2011. Evidence that familial liability for psychosis is expressed as differential sensitivity to cannabis: an analysis of patient-sibling and sibling-control pairs. Arch. Gen. Psychiatry 68:138–47 Grueter BA, Brasnjo G, Malenka RC. 2010. Postsynaptic TRPV1 triggers cell type–specific long-term depression in the nucleus accumbens. Nat. Neurosci. 13:1519–25 Gutiérrez B, Rivera M, Obel L, McKenney K, Martı́nez-Leal R, et al. 2009. Variability in the COMT gene and modification of the risk of schizophrenia conferred by cannabis consumption. Rev. Psiquiatr. Salud Ment. 2:89–94 Habets P, Marcelis M, Gronenschild E, Drukker M, van Os J. 2011. Reduced cortical thickness as an outcome of differential sensitivity to environmental risks in schizophrenia. Biol. Psychiatry 69:487–94 Hall W, Solowij N. 1998. Adverse effects of cannabis. Lancet 352:1611–16 Harley M, Kelleher I, Clarke M, Lynch F, Arseneault L, et al. 2010. Cannabis use and childhood trauma interact additively to increase the risk of psychotic symptoms in adolescence. Psychol. Med. 40:1627–34 Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, et al. 2005a. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330:11–14 Henquet C, Murray R, Linszen D, van Os J. 2005b. The environment and schizophrenia: the role of cannabis use. Schizophr. Bull. 31:608–12 Henquet C, Rosa A, Delespaul P, Papiol S, Fananas L, et al. 2009. COMT ValMet moderation of cannabisinduced psychosis: a momentary assessment study of “switching on” hallucinations in the flow of daily life. Acta Psychiatr. Scand. 119:156–60 Henquet C, Rosa A, Krabbendam L, Papiol S, Fananas L, et al. 2006. An experimental study of catechol-omethyltransferase Val158Met moderation of delta-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacology 31:2748–57 Hoffman AF, Oz M, Yang R, Lichtman AH, Lupica CR. 2007. Opposing actions of chronic 9 tetrahydrocannabinol and cannabinoid antagonists on hippocampal long-term potentiation. Learn. Mem. 14:63–74 Hollis C, Groom MJ, Das D, Calton T, Bates AT, et al. 2008. Different psychological effects of cannabis use in adolescents at genetic high risk for schizophrenia and with attention deficit/hyperactivity disorder (ADHD). Schizophr. Res. 105:216–23 Houston JE, Murphy J, Adamson G, Stringer M, Shevlin M. 2008. Childhood sexual abuse, early cannabis use, and psychosis: testing an interaction model based on the National Comorbidity Survey. Schizophr. Bull. 34:580–85 Houston JE, Murphy J, Shevlin M, Adamson G. 2011. Cannabis use and psychosis: re-visiting the role of childhood trauma. Psychol. Med. 41:2339–48 Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, et al. 2012. The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch. Gen. Psychiatry 69:776–86 Howlett AC, Reggio PH, Childers SR, Hampson RE, Ulloa NM, Deutsch DG. 2011. Endocannabinoid tone versus constitutive activity of cannabinoid receptors. Br. J. Pharmacol. 163:1329–43 Kantrowitz JT, Nolan KA, Sen S, Simen A, Lachman HM, Bowers M. 2009. Adolescent cannabis use, psychosis and catechol-O-methyltransferase genotype in African Americans and Caucasians. Psychiatr. Q. 80:213–18 www.annualreviews.org • Cannabis Use and Psychosis 787 ARI 12 February 2014 14:36 Klugmann M, Klippenstein V, Leweke FM, Spanagel R, Schneider M. 2011. Cannabinoid exposure in pubertal rats increases spontaneous ethanol consumption and NMDA receptor associated protein levels. Int. J. Neuropsychopharmacol. 14:505–17 Konings M, Bak M, Hanssen M, van Os J, Krabbendam L. 2006. Validity and reliability of the CAPE: a selfreport instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr. Scand. 114:55–61 Konings M, Henquet C, Maharajh HD, Hutchinson G, Van Os J. 2008. Early exposure to cannabis and risk for psychosis in young adolescents in Trinidad. Acta Psychiatr. Scand. 118:209–13 Konings M, Stefanis N, Kuepper R, de Graaf R, ten Have M, et al. 2012. Replication in two independent population-based samples that childhood maltreatment and cannabis use synergistically impact on psychosis risk. Psychol. Med. 42:149–59 Kuepper R, Ceccarini J, Lataster J, Van Os J, Van Kroonenburgh M, et al. 2013. Delta-9tetrahydrocannabinol-induced dopamine release as a function of psychosis risk:18 F-fallypride positron emission tomography study. PLoS ONE 8:e70378 Kuepper R, Henquet C, Lieb R, Wittchen HU, van Os J. 2011a. Non-replication of interaction between cannabis use and trauma in predicting psychosis. Schizophr. Res. 131:262–63 Kuepper R, Morrison PD, van Os J, Murray RM, Kenis G, Henquet C. 2010. Does dopamine mediate the psychosis-inducing effects of cannabis? A review and integration of findings across disciplines. Schizophr. Res. 121:107–17 Kuepper R, van Os J, Lieb R, Wittchen HU, Henquet C. 2011b. Do cannabis and urbanicity co-participate in causing psychosis? Evidence from a 10-year follow-up cohort study. Psychol. Med. 41:2121–9 Kuepper R, van Os J, Lieb R, Wittchen HU, Hofler M, Henquet C. 2011c. Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study. BMJ 342:d738 Littleton JM, MacLean KI, Brownlee G. 1976. Proceedings: alterations in dopamine uptake in rat corpus striatum induced by combinations of stress and delta8-tetrahydrocannabinol (delta8-THC). Br. J. Pharmacol. 56:370P Lopez-Moreno JA, Gonzalez-Cuevas G, Moreno G, Navarro M. 2008. The pharmacology of the endocannabinoid system: functional and structural interactions with other neurotransmitter systems and their repercussions in behavioral addiction. Addict. Biol. 13:160–87 Lundqvist T. 2005. Cognitive consequences of cannabis use: comparison with abuse of stimulants and heroin with regard to attention, memory and executive functions. Pharmacol. Biochem. Behav. 81:319–30 Mackie K. 2005. Distribution of cannabinoid receptors in the central and peripheral nervous system. Handb. Exp. Pharmacol. 168:299–325 MacLean KI, Littleton JM. 1977. Environmental stress as a factor in the response of rat brain catecholamine metabolism to delta8-tetrahydrocannabinol. Eur. J. Pharmacol. 41:171–82 Marinelli S, Pacioni S, Cannich A, Marsicano G, Bacci A. 2009. Self-modulation of neocortical pyramidal neurons by endocannabinoids. Nat. Neurosci. 12:1488–90 Martin-Santos R, Fagundo AB, Crippa JA, Atakan Z, Bhattacharyya S, et al. 2010. Neuroimaging in cannabis use: a systematic review of the literature. Psychol. Med. 40:383–98 Mato S, Chevaleyre V, Robbe D, Pazos A, Castillo PE, Manzoni OJ. 2004. A single in-vivo exposure to delta 9 THC blocks endocannabinoid-mediated synaptic plasticity. Nat. Neurosci. 7:585–86 McGrath J, Welham J, Scott J, Varghese D, Degenhardt L, et al. 2010. Association between cannabis use and psychosis-related outcomes using sibling pair analysis in a cohort of young adults. Arch. Gen. Psychiatry 67:440–47 Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, et al. 1995. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharmacol. 50:83–90 Mechoulam R, Parker LA, Gallily R. 2002. Cannabidiol: an overview of some pharmacological aspects. J. Clin. Pharmacol. 42:11–19S Meier MH, Caspi A, Ambler A, Harrington H, Houts R, et al. 2012. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc. Natl. Acad. Sci. USA 109:E2657–64 Mizrahi R, Suridjan I, Kenk M, George TP, Wilson A, et al. 2013. Dopamine response to psychosocial stress in chronic cannabis users: a PET study with [(11)C]-(+)-PHNO. Neuropsychopharmacology 38:673–82 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel 788 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 Mokler DJ, Robinson SE, Johnson JH, Hong JS, Rosecrans JA. 1987. Neonatal administration of delta-9tetrahydrocannabinol (THC) alters the neurochemical response to stress in the adult Fischer-344 rat. Neurotoxicol. Teratol. 9:321–27 Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, et al. 2007. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 370:319–28 Morgan CJ, Curran HV. 2008. Effects of cannabidiol on schizophrenia-like symptoms in people who use cannabis. Br. J. Psychiatry 192:306–7 Morgan CJ, Gardener C, Schafer G, Swan S, Demarchi C, et al. 2012. Sub-chronic impact of cannabinoids in street cannabis on cognition, psychotic-like symptoms and psychological well-being. Psychol. Med. 42:391–400 Morgan CJ, Schafer G, Freeman TP, Curran HV. 2010. Impact of cannabidiol on the acute memory and psychotomimetic effects of smoked cannabis: naturalistic study [corrected]. Br. J. Psychiatry 197:285–90 Morrison PD, Murray RM. 2009. From real-world events to psychosis: the emerging neuropharmacology of delusions. Schizophr. Bull. 35:668–74 Morrison PD, Stone JM. 2011. Synthetic delta-9-tetrahydrocannabinol elicits schizophrenia-like negative symptoms which are distinct from sedation. Hum. Psychopharmacol. 26:77–80 Morrison PD, Zois V, McKeown DA, Lee TD, Holt DW, et al. 2009. The acute effects of synthetic intravenous Delta9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol. Med. 39:1607–16 Murphy J, Houston JE, Shevlin M, Adamson G. 2013. Childhood sexual trauma, cannabis use and psychosis: statistically controlling for pre-trauma psychosis and psychopathology. Soc. Psychiatry Psychiatr. Epidemiol. 48:853–61 Murray RM, Morrison PD, Henquet C, Di Forti M. 2007. Cannabis, the mind and society: the hash realities. Nat. Rev. 8:885–95 Ohno-Shosaku T, Tanimura A, Hashimotodani Y, Kano M. 2012. Endocannabinoids and retrograde modulation of synaptic transmission. Neuroscientist 18:119–32 O’Tuathaigh CM, Clarke G, Walsh JJ, Desbonnet L, Petit E, et al. 2012. Genetic vs. pharmacological inactivation of COMT influences cannabinoid-induced expression of schizophrenia-related phenotypes. Int. J. Neuropsychopharmacol. 15:1331–42 O’Tuathaigh CM, Hryniewiecka M, Behan A, Tighe O, Coughlan C, et al. 2010. Chronic adolescent exposure to delta-9-tetrahydrocannabinol in COMT mutant mice: impact on psychosis-related and other phenotypes. Neuropsychopharmacology 35:2262–73 Pelayo-Teran JM, Perez-Iglesias R, Mata I, Carrasco-Marin E, Vazquez-Barquero JL, Crespo-Facorro B. 2010. Catechol-O-methyltransferase (COMT) Val158Met variations and cannabis use in first-episode non-affective psychosis: clinical-onset implications. Psychiatr. Res. 179:291–96 Pertwee RG. 1997. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol. Ther. 74:129–80 Pertwee RG. 2008. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br. J. Pharmacol. 153:199–215 Pertwee RG. 2010. Receptors and channels targeted by synthetic cannabinoid receptor agonists and antagonists. Curr. Med. Chem. 17:1360–81 Pistis M, Perra S, Pillolla G, Melis M, Muntoni AL, Gessa GL. 2004. Adolescent exposure to cannabinoids induces long-lasting changes in the response to drugs of abuse of rat midbrain dopamine neurons. Biol. Psychiatry 56:86–94 Pope HG Jr, Gruber AJ, Hudson JI, Cohane G, Huestis MA, Yurgelun-Todd D. 2003. Early-onset cannabis use and cognitive deficits: What is the nature of the association? Drug Alcohol Depend. 69:303–10 Purcell SM, Wray NR, Stone JL, Visscher PM, O’Donovan MC, et al. 2009. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460:748–52 Rabin RA, Zakzanis KK, George TP. 2011. The effects of cannabis use on neurocognition in schizophrenia: a meta-analysis. Schizophr. Res. 128:111–16 Ranganathan M, D’Souza DC. 2006. The acute effects of cannabinoids on memory in humans: a review. Psychopharmacology 188:425–44 Realini N, Rubino T, Parolaro D. 2009. Neurobiological alterations at adult age triggered by adolescent exposure to cannabinoids. Pharmacol. Res. 60:132–38 www.annualreviews.org • Cannabis Use and Psychosis 789 ARI 12 February 2014 14:36 Rubino T, Realini N, Braida D, Guidi S, Capurro V, et al. 2009. Changes in hippocampal morphology and neuroplasticity induced by adolescent THC treatment are associated with cognitive impairment in adulthood. Hippocampus 19:763–72 Ryberg E, Larsson N, Sjogren S, Hjorth S, Hermansson NO, et al. 2007. The orphan receptor GPR55 is a novel cannabinoid receptor. Br. J. Pharmacol. 152:1092–101 Schneider M, Drews E, Koch M. 2005. Behavioral effects in adult rats of chronic prepubertal treatment with the cannabinoid receptor agonist WIN 55,212–2. Behav. Pharmacol. 16:447–54 Schneider M, Koch M. 2003. Chronic pubertal, but not adult chronic cannabinoid treatment impairs sensorimotor gating, recognition memory, and the performance in a progressive ratio task in adult rats. Neuropsychopharmacology 28:1760–69 Schneider M, Koch M. 2007. The effect of chronic peripubertal cannabinoid treatment on deficient object recognition memory in rats after neonatal mPFC lesion. Eur. Neuropsychopharmacol. 17:180–86 Schneider M, Schomig E, Leweke FM. 2008. Acute and chronic cannabinoid treatment differentially affects recognition memory and social behavior in pubertal and adult rats. Addict. Biol. 13:345–57 Schubart CD, Boks MP, Breetvelt EJ, van Gastel WA, Groenwold RH, et al. 2011a. Association between cannabis and psychiatric hospitalization. Acta Psychiatr. Scand. 123:368–75 Schubart CD, Sommer IE, van Gastel WA, Goetgebuer RL, Kahn RS, Boks MP. 2011b. Cannabis with high cannabidiol content is associated with fewer psychotic experiences. Schizophr. Res. 130:216–21 Smith MJ, Barch DM, Wolf T, Mamah D, Csernansky JG. 2008. Elevated rates of substance use disorders in non-psychotic siblings of individuals with schizophrenia. Schizophr. Res. 106:294–99 Solowij N. 1995. Do cognitive impairments recover following cessation of cannabis use? Life Sci. 56:2119–26 Solowij N, Battisti R. 2008. The chronic effects of cannabis on memory in humans: a review. Curr. Drug Abuse Rev. 1:81–98 Solowij N, Stephens RS, Roffman RA, Babor T, Kadden R, et al. 2002. Cognitive functioning of long-term heavy cannabis users seeking treatment. JAMA 287:1123–31 Solowij N, Walterfang M, Lubman DI, Whittle S, Lorenzetti V, et al. 2013. Alteration to hippocampal shape in cannabis users with and without schizophrenia. Schizophr. Res. 143:179–84 Solowij N, Yücel M, Respondek C, Whittle S, Lindsay E, et al. 2011. Cerebellar white-matter changes in cannabis users with and without schizophrenia. Psychol. Med. 41:2349–59 Stefanis NC, Delespaul P, Henquet C, Bakoula C, Stefanis CN, Van Os J. 2004. Early adolescent cannabis exposure and positive and negative dimensions of psychosis. Addiction 99:1333–41 Stokes PR, Egerton A, Watson B, Reid A, Breen G, et al. 2010. Significant decreases in frontal and temporal [11C]-raclopride binding after THC challenge. NeuroImage 52:1521–27 Stokes PR, Egerton A, Watson B, Reid A, Lappin J, et al. 2012. History of cannabis use is not associated with alterations in striatal dopamine D2/D3 receptor availability. J. Psychopharmacol. 26:144–49 Stokes PR, Mehta MA, Curran HV, Breen G, Grasby PM. 2009. Can recreational doses of THC produce significant dopamine release in the human striatum? NeuroImage 48:186–90 Stowkowy J, Addington J. 2013. Predictors of a clinical high risk status among individuals with a family history of psychosis. Schizophr. Res. 147:281–86 Sullivan PF. 2007. Spurious genetic associations. Biol. Psychiatry 61:1121–26 Urban NB, Slifstein M, Thompson JL, Xu X, Girgis RR, et al. 2012. Dopamine release in chronic cannabis users: a [11c]raclopride positron emission tomography study. Biol. Psychiatry 71:677–83 van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. 2009. A systematic review and metaanalysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med. 39:179–95 van Os J, Rutten BP, Poulton R. 2008. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr. Bull. 34:1066–82 van Winkel R, Esquivel G, Kenis G, Wichers M, Collip D, et al. 2010. Genome-wide findings in schizophrenia and the role of gene-environment interplay. CNS Neurosci. Ther. 16:e185–92 van Winkel R, Genetic Risk Outcome Psychos. (GROUP) Investig. 2011. Family-based analysis of genetic variation underlying psychosis-inducing effects of cannabis: sibling analysis and proband follow-up. Arch. Gen. Psychiatry 68:148–57 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel 790 van Winkel · Kuepper Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. CP10CH28-vanWinkel ARI 12 February 2014 14:36 van Winkel R, Genetic Risk Outcome Psychos. (GROUP) Investig. 2013. Family-based study examining moderation of familial correlation in psychosis-related experiences by the environment. Manuscr. submitted van Winkel R, van Beveren JM, Genetic Risk Outcome Psychos. (GROUP) Investig. 2011. AKT1 moderation of cannabis-induced cognitive alterations in psychotic disorder. Neuropsychopharmacology 36:2529–37 Veling W, Mackenbach JP, van Os J, Hoek HW. 2008. Cannabis use and genetic predisposition for schizophrenia: a case-control study. Psychol. Med. 38:1251–56 Verdejo-Garcia A, Beatriz Fagundo A, Cuenca A, Rodriguez J, Cuyas E, et al. 2013. COMT Val158Met and 5-HTTLPR genetic polymorphisms moderate executive control in cannabis users. Neuropsychopharmacology 38:1598–606 Vinkers C, Van Gastel WA, Schubart CD, Van Eijk K, Luykx J, et al. 2013. The effect of childhood maltreatment and cannabis use on adult psychotic symptoms is modified by the COMT Val158Met polymorphism. Schizophr. Res. 150:303–11 Voruganti LN, Slomka P, Zabel P, Mattar A, Awad AG. 2001. Cannabis induced dopamine release: an in-vivo SPECT study. Psychiatry Res. 107:173–77 Wegener N, Koch M. 2009. Behavioural disturbances and altered Fos protein expression in adult rats after chronic pubertal cannabinoid treatment. Brain Res. 1253:81–91 Wilson W, Mathew R, Turkington T, Hawk T, Coleman RE, Provenzale J. 2000. Brain morphological changes and early marijuana use: a magnetic resonance and positron emission tomography study. J. Addict. Dis. 19:1–22 Winton-Brown TT, Allen P, Bhattacharyya S, Borgwardt SJ, Fusar-Poli P, et al. 2011. Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an FMRI study. Neuropsychopharmacology 36:1340–48 Yücel M, Bora E, Lubman DI, Solowij N, Brewer WJ, et al. 2012. The impact of cannabis use on cognitive functioning in patients with schizophrenia: a meta-analysis of existing findings and new data in a firstepisode sample. Schizophr. Bull. 38:316–30 Yücel M, Solowij N, Respondek C, Whittle S, Fornito A, et al. 2008. Regional brain abnormalities associated with long-term heavy cannabis use. Arch. Gen. Psychiatry 65:694–701 Zammit S, Owen M, Evans J, Heron J, Lewis G. 2011. Cannabis, COMT and psychotic experiences. Br. J. Psychiatry 199:380–85 Zammit S, Spurlock G, Williams H, Norton N, Williams N, et al. 2007. Genotype effects of CHRNA7, CNR1 and COMT in schizophrenia: interactions with tobacco and cannabis use. Br. J. Psychiatry 191:402–7 Zuardi AW, Crippa JA, Hallak JE, Bhattacharyya S, Atakan Z, et al. 2012. A critical review of the antipsychotic effects of cannabidiol: 30 years of a translational investigation. Curr. Pharm. Des. 18:5131–40 www.annualreviews.org • Cannabis Use and Psychosis 791 CP10-FrontMatter ARI 6 March 2014 22:5 Annual Review of Clinical Psychology Contents Volume 10, 2014 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Advances in Cognitive Theory and Therapy: The Generic Cognitive Model Aaron T. Beck and Emily A.P. Haigh p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 1 The Cycle of Classification: DSM-I Through DSM-5 Roger K. Blashfield, Jared W. Keeley, Elizabeth H. Flanagan, and Shannon R. Miles p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p25 The Internship Imbalance in Professional Psychology: Current Status and Future Prospects Robert L. Hatcher p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p53 Exploratory Structural Equation Modeling: An Integration of the Best Features of Exploratory and Confirmatory Factor Analysis Herbert W. Marsh, Alexandre J.S. Morin, Philip D. Parker, and Gurvinder Kaur p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p85 The Reliability of Clinical Diagnoses: State of the Art Helena Chmura Kraemer p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 111 Thin-Slice Judgments in the Clinical Context Michael L. Slepian, Kathleen R. Bogart, and Nalini Ambady p p p p p p p p p p p p p p p p p p p p p p p p p p p p 131 Attenuated Psychosis Syndrome: Ready for DSM-5.1? P. Fusar-Poli, W.T. Carpenter, S.W. Woods, and T.H. McGlashan p p p p p p p p p p p p p p p p p p p 155 From Kanner to DSM-5: Autism as an Evolving Diagnostic Concept Fred R. Volkmar and James C. McPartland p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 193 Development of Clinical Practice Guidelines Steven D. Hollon, Patricia A. Areán, Michelle G. Craske, Kermit A. Crawford, Daniel R. Kivlahan, Jeffrey J. Magnavita, Thomas H. Ollendick, Thomas L. Sexton, Bonnie Spring, Lynn F. Bufka, Daniel I. Galper, and Howard Kurtzman p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 213 Overview of Meta-Analyses of the Prevention of Mental Health, Substance Use, and Conduct Problems Irwin Sandler, Sharlene A. Wolchik, Gracelyn Cruden, Nicole E. Mahrer, Soyeon Ahn, Ahnalee Brincks, and C. Hendricks Brown p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 243 vii CP10-FrontMatter ARI 6 March 2014 22:5 Improving Care for Depression and Suicide Risk in Adolescents: Innovative Strategies for Bringing Treatments to Community Settings Joan Rosenbaum Asarnow and Jeanne Miranda p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 275 The Contribution of Cultural Competence to Evidence-Based Care for Ethnically Diverse Populations Stanley J. Huey Jr., Jacqueline Lee Tilley, Eduardo O. Jones, and Caitlin A. Smith p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 305 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. How to Use the New DSM-5 Somatic Symptom Disorder Diagnosis in Research and Practice: A Critical Evaluation and a Proposal for Modifications Winfried Rief and Alexandra Martin p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 339 Antidepressant Use in Pregnant and Postpartum Women Kimberly A. Yonkers, Katherine A. Blackwell, Janis Glover, and Ariadna Forray p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 369 Depression, Stress, and Anhedonia: Toward a Synthesis and Integrated Model Diego A. Pizzagalli p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 393 Excess Early Mortality in Schizophrenia Thomas Munk Laursen, Merete Nordentoft, and Preben Bo Mortensen p p p p p p p p p p p p p p p p 425 Antecedents of Personality Disorder in Childhood and Adolescence: Toward an Integrative Developmental Model Filip De Fruyt and Barbara De Clercq p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 449 The Role of the DSM-5 Personality Trait Model in Moving Toward a Quantitative and Empirically Based Approach to Classifying Personality and Psychopathology Robert F. Krueger and Kristian E. Markon p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 477 Early-Starting Conduct Problems: Intersection of Conduct Problems and Poverty Daniel S. Shaw and Elizabeth C. Shelleby p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 503 How to Understand Divergent Views on Bipolar Disorder in Youth Gabrielle A. Carlson and Daniel N. Klein p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 529 Impulsive and Compulsive Behaviors in Parkinson’s Disease B.B. Averbeck, S.S. O’Sullivan, and A. Djamshidian p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 553 Emotional and Behavioral Symptoms in Neurodegenerative Disease: A Model for Studying the Neural Bases of Psychopathology Robert W. Levenson, Virginia E. Sturm, and Claudia M. Haase p p p p p p p p p p p p p p p p p p p p p p p 581 viii Contents CP10-FrontMatter ARI 6 March 2014 22:5 Attention-Deficit/Hyperactivity Disorder and Risk of Substance Use Disorder: Developmental Considerations, Potential Pathways, and Opportunities for Research Brooke S.G. Molina and William E. Pelham Jr. p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 607 The Behavioral Economics of Substance Abuse Disorders: Reinforcement Pathologies and Their Repair Warren K. Bickel, Matthew W. Johnson, Mikhail N. Koffarnus, James MacKillop, and James G. Murphy p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 641 Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. The Role of Sleep in Emotional Brain Function Andrea N. Goldstein and Matthew P. Walker p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 679 Justice Policy Reform for High-Risk Juveniles: Using Science to Achieve Large-Scale Crime Reduction Jennifer L. Skeem, Elizabeth Scott, and Edward P. Mulvey p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 709 Drug Approval and Drug Effectiveness Glen I. Spielmans and Irving Kirsch p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 741 Epidemiological, Neurobiological, and Genetic Clues to the Mechanisms Linking Cannabis Use to Risk for Nonaffective Psychosis Ruud van Winkel and Rebecca Kuepper p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 767 Indexes Cumulative Index of Contributing Authors, Volumes 1–10 p p p p p p p p p p p p p p p p p p p p p p p p p p p p 793 Cumulative Index of Articles Titles, Volumes 1–10 p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 797 Errata An online log of corrections to Annual Review of Clinical Psychology articles may be found at http://www.annualreviews.org/errata/clinpsy Contents ix Annual Reviews It’s about time. Your time. It’s time well spent. New From Annual Reviews: Annual Review of Organizational Psychology and Organizational Behavior Volume 1 • March 2014 • Online & In Print • http://orgpsych.annualreviews.org Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Editor: Frederick P. Morgeson, The Eli Broad College of Business, Michigan State University The Annual Review of Organizational Psychology and Organizational Behavior is devoted to publishing reviews of the industrial and organizational psychology, human resource management, and organizational behavior literature. Topics for review include motivation, selection, teams, training and development, leadership, job performance, strategic HR, cross-cultural issues, work attitudes, entrepreneurship, affect and emotion, organizational change and development, gender and diversity, statistics and research methodologies, and other emerging topics. Complimentary online access to the first volume will be available until March 2015. Table of Contents: • An Ounce of Prevention Is Worth a Pound of Cure: Improving Research Quality Before Data Collection, Herman Aguinis, Robert J. Vandenberg • Burnout and Work Engagement: The JD-R Approach, Arnold B. Bakker, Evangelia Demerouti, Ana Isabel Sanz-Vergel • Compassion at Work, Jane E. Dutton, Kristina M. Workman, Ashley E. Hardin • Constructively Managing Conflict in Organizations, Dean Tjosvold, Alfred S.H. Wong, Nancy Yi Feng Chen • Coworkers Behaving Badly: The Impact of Coworker Deviant Behavior upon Individual Employees, Sandra L. Robinson, Wei Wang, Christian Kiewitz • Delineating and Reviewing the Role of Newcomer Capital in Organizational Socialization, Talya N. Bauer, Berrin Erdogan • Emotional Intelligence in Organizations, Stéphane Côté • Employee Voice and Silence, Elizabeth W. Morrison • Intercultural Competence, Kwok Leung, Soon Ang, Mei Ling Tan • Learning in the Twenty-First-Century Workplace, Raymond A. Noe, Alena D.M. Clarke, Howard J. Klein • Pay Dispersion, Jason D. Shaw • Personality and Cognitive Ability as Predictors of Effective Performance at Work, Neal Schmitt • Perspectives on Power in Organizations, Cameron Anderson, Sebastien Brion • Psychological Safety: The History, Renaissance, and Future of an Interpersonal Construct, Amy C. Edmondson, Zhike Lei • Research on Workplace Creativity: A Review and Redirection, Jing Zhou, Inga J. Hoever • Talent Management: Conceptual Approaches and Practical Challenges, Peter Cappelli, JR Keller • The Contemporary Career: A Work–Home Perspective, Jeffrey H. Greenhaus, Ellen Ernst Kossek • The Fascinating Psychological Microfoundations of Strategy and Competitive Advantage, Robert E. Ployhart, Donald Hale, Jr. • The Psychology of Entrepreneurship, Michael Frese, Michael M. Gielnik • The Story of Why We Stay: A Review of Job Embeddedness, Thomas William Lee, Tyler C. Burch, Terence R. Mitchell • What Was, What Is, and What May Be in OP/OB, Lyman W. Porter, Benjamin Schneider • Where Global and Virtual Meet: The Value of Examining the Intersection of These Elements in Twenty-First-Century Teams, Cristina B. Gibson, Laura Huang, Bradley L. Kirkman, Debra L. Shapiro • Work–Family Boundary Dynamics, Tammy D. Allen, Eunae Cho, Laurenz L. Meier Access this and all other Annual Reviews journals via your institution at www.annualreviews.org. Annual Reviews | Connect With Our Experts Tel: 800.523.8635 (us/can) | Tel: 650.493.4400 | Fax: 650.424.0910 | Email: service@annualreviews.org Annual Reviews It’s about time. Your time. It’s time well spent. New From Annual Reviews: Annual Review of Statistics and Its Application Volume 1 • Online January 2014 • http://statistics.annualreviews.org Annu. Rev. Clin. Psychol. 2014.10:767-791. Downloaded from www.annualreviews.org by University of Dayton on 08/12/14. For personal use only. Editor: Stephen E. Fienberg, Carnegie Mellon University Associate Editors: Nancy Reid, University of Toronto Stephen M. Stigler, University of Chicago The Annual Review of Statistics and Its Application aims to inform statisticians and quantitative methodologists, as well as all scientists and users of statistics about major methodological advances and the computational tools that allow for their implementation. It will include developments in the field of statistics, including theoretical statistical underpinnings of new methodology, as well as developments in specific application domains such as biostatistics and bioinformatics, economics, machine learning, psychology, sociology, and aspects of the physical sciences. Complimentary online access to the first volume will be available until January 2015. table of contents: • What Is Statistics? Stephen E. Fienberg • A Systematic Statistical Approach to Evaluating Evidence from Observational Studies, David Madigan, Paul E. Stang, Jesse A. Berlin, Martijn Schuemie, J. Marc Overhage, Marc A. Suchard, Bill Dumouchel, Abraham G. Hartzema, Patrick B. Ryan • High-Dimensional Statistics with a View Toward Applications in Biology, Peter Bühlmann, Markus Kalisch, Lukas Meier • Next-Generation Statistical Genetics: Modeling, Penalization, and Optimization in High-Dimensional Data, Kenneth Lange, Jeanette C. Papp, Janet S. Sinsheimer, Eric M. Sobel • The Role of Statistics in the Discovery of a Higgs Boson, David A. van Dyk • Breaking Bad: Two Decades of Life-Course Data Analysis in Criminology, Developmental Psychology, and Beyond, Elena A. Erosheva, Ross L. Matsueda, Donatello Telesca • Brain Imaging Analysis, F. DuBois Bowman • Event History Analysis, Niels Keiding • Statistics and Climate, Peter Guttorp • Statistical Evaluation of Forensic DNA Profile Evidence, Christopher D. Steele, David J. Balding • Climate Simulators and Climate Projections, Jonathan Rougier, Michael Goldstein • Probabilistic Forecasting, Tilmann Gneiting, Matthias Katzfuss • Bayesian Computational Tools, Christian P. Robert • Bayesian Computation Via Markov Chain Monte Carlo, Radu V. Craiu, Jeffrey S. Rosenthal • Build, Compute, Critique, Repeat: Data Analysis with Latent Variable Models, David M. Blei • Structured Regularizers for High-Dimensional Problems: Statistical and Computational Issues, Martin J. Wainwright • Using League Table Rankings in Public Policy Formation: Statistical Issues, Harvey Goldstein • Statistical Ecology, Ruth King • Estimating the Number of Species in Microbial Diversity Studies, John Bunge, Amy Willis, Fiona Walsh • Dynamic Treatment Regimes, Bibhas Chakraborty, Susan A. Murphy • Statistics and Related Topics in Single-Molecule Biophysics, Hong Qian, S.C. Kou • Statistics and Quantitative Risk Management for Banking and Insurance, Paul Embrechts, Marius Hofert Access this and all other Annual Reviews journals via your institution at www.annualreviews.org. Annual Reviews | Connect With Our Experts Tel: 800.523.8635 (us/can) | Tel: 650.493.4400 | Fax: 650.424.0910 | Email: service@annualreviews.org