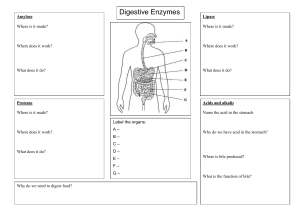
1 DIGESTIVE TRACT DISORDERS The GI tract begins in the mouth and extends through the pharynx, esophagus, stomach, small intestine, large intestine to the anus. Accessory organs include the salivary glands, liver, gall bladder and pancreas. Nursing Assessment of the GI Tract Assessment of the GI tract follows the 4 basic assessment skills and techniques Inspection Auscultation Palpation Percussion Diagnostic Test History and physical exams Chemistries Coagulating factors Radiological studies X-ray (abdominal) CT scan MRI Endoscopy Gastric analysis Fecal fat study Occult blood test Occult blood Test Is done when bleeding is suspected, samples can be tested for occult blood. Specimens most often tested for occult blood are vomitus, gastric secretions and stool Stool samples can be tested for occult blood. A series of three tests are usually collected to increase the chances of detecting blood in the stool and also helps presents false – positive results. False positive results usually occur: following dental procedures Ingestion of meat (iron-liver meats) Ingestion of beats Medications (ASA, colchicines (gout medication), NSAIDS, steroids) 2 Upper GI series/study Also called a Barium Swallow This is an X-Ray examination of the mouth, esophagus, stomach and small intestines (duodenum, jejunum) using an oral liquid radiopaque contrast medium Preoperative Nursing Explain the procedure to the pt-inform the patient that during the procedure he/she will be asked to drink a thick chalky white substance called barium while standing in front of a fluoroscopy tube. X-Rays will be taken at specific intervals to visualize the outline of the organs and note the passage of the barium through the GI tract Pt needs to be NPO for 6-8 hours before the procedure- should eat a light meal the night before the test Pt is discouraged from smoking the evening before the procedure or the day of the procedure (because smoking increase gastric motility or stimulates gastric motility) Assess for allergies to barium – not to iodine because iodine is not used Pt does not require informed consent for barium swallow Postoperative Nursing Patient is instructed to increase fluid intake to 3-3 ½ L unless contraindicated Encourage the pt to ambulate as soon as possible after procedure to help excrete barium from barium A laxative Assess abdominal girth, abdominal tenderness, abdominal distention, abdominal firmness/board like abdomen and nausea and vomiting-the presence of the following may indicate barium impaction Assess the stool to determine if the barium is completely eliminated from the body stool would be white or clay –If the pt is ordered a barium swallow, gallbladder sonogram, barium enema the tests should be done in this order: gallbladder sonogram barium enema barium swallow Barium enema (lower GI series) Barium enema is done to visualize the position, movement and filling of the colon. Preoperative Nursing pt does not need an informed consent pt placed on a low residue diet, or clear liquid diet at least 2 days before the procedure and then NPO after midnight laxative or bowel cleansing agents or solution (golytely) and enemas may be given the evening before the procedure 3 no barium enema is done when a pt has an obstruction or suspected obstruction, perforation, active GI bleeding, diarrhea, inflammation of the colon Assess for electrolyte imbalances increase fluid intake apply lubricant to the rectal area because loose stools may cause irritation Endoscopy Uses a rigid or flexible tube to observe a hollow organ or cavity o Upper GI Endoscopy o Lower GI endoscopy Upper GI Endoscopy EGD – Esophagogastroduodenoscopy This procedure visualizes the esophagus, stomach and the duodenum Usually done to diagnose inflammation, cancer, trauma, bleeding or obstruction Preoperative Nursing Explain procedure to the patient Informed consent NPO after midnight to prevent aspiration of stomach contents in the lungs if vomiting occurs Local anesthesia is usually used to depress the gag or cough reflex Baseline vital signs Mild sedative is usually given before the procedure to calm the pt Postoperative Nursing maintain patent airway-place patient on the side to prevent aspiration until gag reflex return assess respiratory pattern, rate and effort after the procedure check vital signs and level of consciousness Keep patient NPO until gag reflex returns Nurse should assess for bleeding- small bright red bleeding or blood streak is expected after the procedure Nurse should assess for S/S of bowel perforation o Fever 101-103oF o Abdominal cramps o Abdominal distention o Board like abdomen o Absent or diminished bowel signs o Abdominal pain o Malaise o Change in VS o Referred pain – shoulder and back/flank pain 4 Signs and symptoms of esophageal perforation o Dysphagia o Hematoma o Cyanosis o Epigastric pain o Sore throat for few days o Dyspnea o Chest pain Lower GI endoscopy (colonoscopy and proctosigmoidoscopy) Colonoscopy-Visualization of the colon Proctosigmoidoscopy-visualization of the distal sigmoid colon, the rectum and the anal wall using a rigid or flexible endoscope. Preoperative Nursing Informed consent pt needs to be NPO after midnight prepare the bowel by ensuring that the bowel cleansing agent (golytely) is completely taken by the pt a mild laxative or enema can also be given with the bowel cleansing agent a mild sedative is usually given to calm the pt VS taken before and during the procedure-Especially the pulse –because vagal stimulation increase which has the potential of causing bradycardia Coagulation studies –PT,PTT,INR are done before the test Postoperative Nursing Vital signs are checked frequently after the test Asses for bleeding-small bleeding is expected excessive bleeding should be reported to MD Explain to the pt that cramping or flatulence are common after the procedure pt should not drive immediately after the procedure Pt should also not make any important or major decisions 24hours after the procedure Keep pt NPO until bowel sounds return or able to pass gas Gastric Analysis Measure the amount of hydrochloric acid in gastric fluid Diagnose pyloric or duodenal obstruction or pernicious anemia (B12 deficiency) Gastric analysis is done in two ways: o basal cell secretion test o gastric acid stimulations test Basal Cell Secretion Test The pt is advised to avoid drugs that could interfere with gastric acid secretion o antacids 5 o cholinergic pt is asked to be NPO after midnight No smoking on the day of the test stimulate reduction of gastric acid A nasal gastric tube is inserted and the contents of the stomach is aspirated through the tube using a syringe gastric contents is withdrawn or aspirated every 15minutes for 1 hour If too much HCL acid is found on the gastric content the pt is said to have peptic ulcer disease (PUD) If there is too little or no HCL – pernicious anemia is diagnosed Gastric Acid Stimulation Test Measures the amount of gastric acid for one hour after subcutaneous injection of histamine drugs A stimulus in the form of carbohydrate like a dry toast or caffeinated product or medication like histamine is given to produce more secretion. Common Therapeutic Measures Gastrointestinal intubation This refers to an insertion of a tube into the stomach or small intestines. Purpose of GI intubation diagnostic purposes Gastric Decompression - Remove gas or fluid from the stomach or intestine relieve or treat obstruction or bleeding within the GI tract means of nutrition, hydration or administering medications when PO is not possible To promote healing after esophageal, gastric or intestinal surgery by preventing distention of the GI tract and strain on the suture line. GI intubation can be temporary or permanent Tube Feeding Tube feeding is initiated when the patient is unable to eat or swallow. Tube feeding requires an MD order Tube feeding can be administered through a Nasogastric Tube Orogastric Tube Jejunostomy Tube Gastrostomy Tube Tube feeding administered either via gravity or by a pump 6 Nasogastric Tubes Types Levin-Single lumen stomach tube used to remove stomach contents or provide tube feeding Salem-Sump-Double lumen stomach tube;most frequently used tube for decompression with suction Measurement of NG Tube The nurse should measure from the tip of the nose to the tip of the auricle and to the xiphoid process Add 5 cm to the above measurement if the tube has to enter into the intestine Placement of NGT Before the nurse administers anything into a tube he/she needs to check for placement Check for placement: Abdominal X-ray Aspiration of gastric content and checking the pH Tube feedings are delivered intermittently, continuously or by a bolus Care of the patient with enteral feeding– Assist pt to semi-fowler’s position when receiving tube feeding at all times Good mouth care Lubricate tube around nares with water-soluble jelly Check for placement before administering tube feeding Check bowel sounds every 4 hours and before each feeding Check the stoma site for redness, exudates, irritation and granuloma etc. Check for residual – nurse should check the residual anytime the feeding is administered to the pt and if the patient is receiving continuous feeding residual is checked every 4 hours– Check for patency of the tube before administering anything into a tube Nurse needs 5cc of water to check for patency When administration medication into a tube request liquid form if possible, if not the tablets should be crushed thoroughly Check with the pharmacy to determine which medications are not to be crushed The nurse should not crush –enteric coated, sustained release or capsules TPN (Total Parenteral Nutrition) Also referred to as intravenous hyper alimentation TPN contains protein, fat, CHO, vitamins, minerals, water and trace element TPN is used when the pts nutritional needs can not be met satisfactory by the GI Tract Hyperemesis gravidarium Extensive burns Trauma Cancer Pancreatitis 7 Inflammatory bowel disease Following extensive bowel surgery Acute renal failure Nursing care of a patient on TPN Follow doctor’s order A registered nurse is responsible for administering TPN TPN should be started slowly to allow the pancreas to adjust to the high glucose content The nurse should check the patency of the central catheter before resuming the feeding TPN should only be administered via sterile technique TPN orders should be renewed everyday Nurse should monitor the following when the pt is on TPN Weight Intake and output Check fluid and electrolyte status Check albumin levels Nurse should check blood glucose every 4 hours and continuously while receiving TPN Nurse should monitor for complications of TPN Infection Septicemia Hyperglycemia Depression Fluid overload Gastrointestinal Surgery A laparotomy is the surgical opening of the abdomen Surgery can be done for bleeding ulcers, cancers, hernia’s (abdominal or umbilical), appendicitis or for obstruction. Gastrectomy is the surgical excision of the stomach Billroth I-Pyloric portion is removed and the remaining stomach is joined to the duodenum Billroth II- The pylorus is removed, the proximal end of the duodenum is sutured and the remaining portion of the stomach is joined to the jejunum DIET Clear Liquid Apple juice Full Liquid All clear liquid Soft Diet All full liquids Water Milk Pureed foods Cranberry juice Ice cream Poached eggs 8 Broth (soup) Creamed soup Mashed potatoes Jello (gelatin) Cooked cereal Meat (tender puree) Ginger ale Fruit juices Popsicle Custard Tea with lemon Bland diet- A diet without spices GI Medications HISTAMINE 2 ANTAGONISTS These drugs are used in the treatment of GERD and gastric ulcers. They inhibit histamine release in the gastric parietal cells, therefore gastric acids. H2 blocks – reduce the acidity of gastric juices by blocking the ability of histamine to stimulate gastric acid secretion tidine Cimetidine (Tagamet) Famotidine ( Pepcid) Ranitidine (Zantac) Nizatidine (Axid) Nursing consideration for H2 Antagonists Monitor kidney function-BUN, creatinine Administer with meals Take antacids one hour before or after taking these drugs Monitor gastric Ph- should be checked periodically Cimetidine may be prescribed in one large dose at bedtime Sucralfate decreases the effects of histamine 2 receptor blockers Avoid smoking because it interferes or impairs the effect of H2 blockers H2 blockers should be used cautiously in the elderly PROTON PUMP INHIBITORS Suppress gastric secretions- inhibiting the hydrogen/potassium ATPase enzyme system. prazole Lansoprazole (Prevacid) Pantoprazole (Protonix) Rabeprazole (Aciphex) Esomeprazole (Nexium) Nursing considerations Monitor liver function Take medications before meals Inform the patient not to crush pantoprazole (protonix) 9 ANTACIDS Act by elevating the pH of the gastric contents, thereby deactivating pepsin. They are inadequate for the control of symptoms because their duration of action is too short and their nighttime effectiveness is minimal. Aluminum or magnesium salts (Mylanta, Maalox) Aluminum hydroxide (Amphogel) Magnesium carbonate (Gaviscon) Calcium carbonates (Tums) Nursing consideration for antacids Give after meals and at bedtime Observe the client for constipation or diarrhea Absorption of tetracyclines, phenothiazides, Isoniazid and ferrous sulfate reduced when given with antacids Effectives of oral contraceptives and salicylates may decrease when giving with antacids Do not administer antacids with ferrous sulfate, histamine 2 blockers and other medications. Use medication with sodium content cautiously for clients with cardiac and renal disease Disorders of the GI tract Oral Cancers Oral cancer comprises of any cancer in the mouth or the throat. It also affects the tongue, lips, roof of mouth etc. It is life threatening because of the possibility of obstructing the airway Highest incidence of oral cancer is found in the pharynx (throat) Risk Factor Diagnosis Hiatal Hernia In hiatal hernia there is a protrusion of part of the stomach into the thoracic cavity through the opening in the diaphragm where the esophagus passes. Common in women than in men Two types of Hiatal Hernia Sliding hiatal hernia Rolling hiatal hernia Sliding Hiatal Hernia 90% of hiatel hernias are sliding 10 In sliding hiatal hernia the top of the stomach enters the thoracic cavity when the pt is in a supine position – but slides back in the abdomen when a pt assumes a vertical (reclining) position (associated with GERD) Rolling Hiatal Hernia In a rolling hiatal hernia also referred to as a Paraesophageal hernia – the gastroesophageal junction remains in place but a portion of the stomach protrudes or herniates into the thoracic cavity through a secondary opening. Risk Factors Weakness of the muscles of the diaphragm in the lower esophageal sphincter (LES) Aging Obesity Surgery Genetics/hereditary Stress Trauma Straining or lifting heavy objects Pregnancy Increased intraabdominal or thoracic pressure-from bending, coughing or vomiting Prolonged bed rest in a reclining position Signs and Symptoms most pts are asymptomatic heartburn belching gas (flatulence) abdominal distention abdominal fullness bloating SOB Chest pain Increase pulse Difficulty swallowing (dysphagia) Diagnosis Nursing Intervention Nurse should instruct the pt to avoid alcohol – because alcohol increase the pressure in the LES (lower esophageal sphincter) Patient should also avoid activities or conditions that increase intraabdominal pressure. These activities or conditions include: bending 11 straining lifting carrying heavy objects coughing vomiting pregnancy sneezing obesity eating a large meal wearing constrictive clothing Inform the patient that prolong bed-rest can also cause hiatal hernia –because it decrease LES pressure Avoid smoking (increase gastric acid secretion) If obese – counsel the patient to decrease weight Serve the pt small –frequent meals instead of 3 large meals Eat slowly and chew food well Inform pt to avoid foods that are known to decrease LES pressure Caffeinated products tea chocolate carbonated drinks Instruct pt to avoid spicy or acid foods Give antacids- should be given after meals Encourage pt to sit up at least (30-45 degrees) for at least 2-3 hours after meals HOB should always be elevated when sleeping Instruct the client to keep a diary of the foods that seem to increase the signs and symptoms and avoid these foods Reduce stress and encourage relaxation techniques Assess patient general nutritional needs and identify dietary changes Surgery may be done-fundoplication Gastroesophageal Reflux Disease (GERD) Backflow of gastric content from the stomach into the esophagus GERD also referred to as heartburn or esophagitis Normally the LES remains closed except during swallowing When a pt has GERD the LES remains open even after the pt has swallowed When a pt has GERD – gastric content are regurgitated into the esophagus, these gastric contents contains gastric acid, pepsin, bile and corrosive substances which may irritate the lining of the esophagus causing ulcerations. Causes High fat diet Hiatal hernia Duodenal or gastric ulcers Obesity 12 Pregnancy Conditions that reduce LES pressure-excessive caffeine intake, smoking and alcohol Congenital defects GI intubation Gastroparesis Signs and Symptoms of GERD Heartburn Pain 1-2 hours after eating –or when lying down Bloating Frequent belching with a sour taste Abdominal distention Sore throat Hoarseness Symptoms occur after activity that increase intra-abdominal pressure such as lifting, straining and lying supine position Diagnosis Treatment Nursing Intervention Peptic Ulcer Disease Loss of tissue or break in the mucous lining of the GI tract hydrochloric acid (HCL), pepsin, bile and other corrosive substances may cause injury to unprotected tissue Ulcers may occur in different areas Lower end of the esophagus Stomach Duodenum Most ulcers occur in the stomach or the duodenum Gastric Ulcers Often occur often in men and in the elderly. Gastric ulcers are usually small and located in the lesser curvature of the stomach Causes include: Ingestion of medications-aspirin, NSAIDS, steroids Coffee or caffeinated products Smoking Alcohol Stress Helicobacter pylori 13 Duodenal Ulcers Occur in the beginning area of the duodenum close to the pyloric sphincter Usually caused by secondary factors or problems: COPD Cirrhosis of the liver Hyperthyroidism Alcoholism Chronic pancreatitis Smoking H. pylori Stress Ulcer (Curling’s) Usually result from prolong illness or after surgery Usually related to inadequate blood flow to the lining of the GI tract Signs and Symptoms of Gastric Ulcers Severe epigastric pain or heartburn that occurs immediately or 1-2 hours after or during meals or at bedtime Pain may radiate to the lower back or flank area Weight loss N/V Anorexia Feeling fullness after eating Abdominal distention Bloating Hematemesis Melena Signs and Symptoms Duodenal Ulcers Patient may have no pain-if pain is present it is normally relieved by food Abdominal distention N/V Melena Hematemesis Weight gain Feeling of fullness Bloating Complication of Ulcers Major complication of an ulcer is Hemorrhage Perforation of the stomach or small intestine –Peritonitis Pyloric obstruction 14 Treatment Find cause and treat the underlying cause Relieve signs and symptoms Promote healing Prevent recurrence Drug therapy antacids H2 blockers Protein Pump Inhibitors (PPI’s) Mucosal barrier (Sulcrafate) Antibiotic therapy Flagyl Tetracycline Pepto-bismuth – is given with antibiotic to kill the H. pylori- Pepto-bismuth makes stool to be tarry (black) Nursing Interventions for Ulcers Inform pt to avoid alcohol and smoking Inform the pt to eat small frequent meals rather than 3 large ones The pt needs to be weigh periodically ( increase or decrease of more that 5 lbs in 1 month -report to MD) Inform pt to avoid meds know to exacerbate ulcers Give meds on time and as prescribed to relieve pain from local irritation of the intestinal mucosa Have patient rest because physical activity stimulates gastric secretions Increase fluid intake 2-3 liters unless contraindicated Nurse should closely monitor pt for complications of an ulcer Signs and Symptoms of Hemorrhagic Shock _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ Signs and Symptoms of Perforation Sudden severe sharp pain in the upper abdomen- pain may radiate to the mid epigastric area or to the shoulders or lower back N/V Increase temperature __________________ __________________ Malaise ___________________ 15 Surgery Gastrectomy (partial or total) Complications of gastrectomy Hemorrhage Pneumonia/atelectasis Pernicious anemia – lack of intrinsic factor –Vitamin B12 Dumping syndrome Nutritional imbalance Dumping Syndrome Rapid passage of large amounts of food and fluids through the remaining portion of the stomach into the intestines Rapid emptying of food and fluids from the stomach into the jejunum. When a pt has dumping syndrome-there is inabsorption of nutrients in the body Signs and Symptoms of Dumping Syndrome Nausea and Vomiting Abdominal pain/tenderness Diarrhea Decrease blood sugar Diaphoresis Feeling of dizziness/fainting Palpitations Hyperactive bowel sounds Weakness Pallor Decrease blood pressure Increase pulse Nursing Interventions for Dumping Syndrome Lie down flat for 30 minutes to 1 hour after a meal Make sure pt eats small frequent meals Avoid drinking fluids in between meals Diet : low in CHO, high fiber, moderate in fat and high in protein Stress the need for reducing stress Check blood sugar every 4 hours-if pt has decrease blood sugar- encourage pt to eat a candy or drink fluids that contain glucose Absorption of vitamins and minerals-iron, folic acid, calcium, vitamin D may be impaired so encourage the intake of these nutrients Give medications on time Antispasmodic – Probanthine - Bentyl Sedatives are usually given as well 16 Appendicitis Inflammation of the appendix Any obstruction of the appendix makes it more susceptible to an infection Appendix can be obstructed by the following: Feces (stool) Helminths (worm) Bacteria Dead particles Undissolved substances (seeds, nuts) Rupturing of the appendix allows the digestive juices or contents to enter the abdominal cavity causing peritonitis or hemorrhage Signs and Symptoms of appendicitis Pain in the epigastric region around the umbilicus which shifts to the Right lower Quadrant (RLQ) Pain at the Mcburney’s point located midway between the umbilicus and the iliac crest Increased temperature 100o-103o Increase WBC Increase ESR Nausea and Vomiting Normal bowel sounds Guarding position or assume a position of hip flexion Pain in the RLQ when LLQ is palpated – this is referred to as the Rovsing sign Rebound tenderness –severe pain over the tender area when pressure is applied quickly and released Nursing Intervention for appendicitis Monitor VS Place patient in a semi-fowlers’ s position Keep pt NPO until diagnosis is made Assess the pt for pain-onset, location, severity, frequency and type Avoid giving narcotics – Avoid laxatives No enemas No heat-apply cold packs if needed No palpation of the stomach because this may cause a perforation of appendix If appendix has ruptured it is a medical emergency, however, surgery will be delayed for 6-8 hours after the ruptures because high doses of antibiotic are needed to diffuse the infection. Give IV fluids 17 The nurse should obtain a consent – because surgery is imminent Postoperative Nursing care for Appendectomy Abdominal Hernia Hernias are caused be a weakness in the wall of the cavity Hernias are classified into two Reducible Irreducible Reducible Hernia A reducible hernia means the protruding organ can be retuned to its proper place when the pt lies supine or when there is a gentle pressure placed on the protruding organ Irreducible Hernia (Strangulated) Means that the protruding part of the organ cannot be returned back to its proper place when pt lies supine or when gentle pressure is applied because the protruding organ is tightly wedged outside the cavity and cannot be pushed back through the opening Risk Factors Stress Obesity Straining Bending Carrying heavy objects Pregnancy Trauma Aging Wearing constrictive clothing Medical Treatment Surgery is warranted even for reducible hernia Herniorrhaphy Hernioplasty Hernias can also be treated without surgery. The patient is asked to wear a binder or a truss A Truss is an external restraining device that is held in place with a belt. Inguinal Hernia Scrotal support and elevate the scrotum with a towel/wash cloth Ice pack can greatly reduce the painful swelling Inflammatory Bowel Syndrome (IBD) Refers to any inflammation or infection of the intestine IBD refers to both ulcerative colitis and crohn’s disease 18 Ulcerative Colitis Eroded areas of the mucous membrane and tissues beneath it Inflammation of the superficial mucosa of the colon causing the bowel to eventually narrow, thicken and shortens due to the muscular hypertrophy Ulcerative colitis usually affects the large bowel-colon and the rectum Crohn’s Disease Crohn’s disease can affect any part of the intestines. It is a sub acute, chronic inflammation extending throughout the entire intestinal mucosa. Crohn’s disease can involve any part of the intestine but most commonly occur in the terminal portion of the ileum. The inflammation extends through the intestinal mucosa which leads to the formation of abscesses, fistulas and fissures. Causes of IBD Exact cause is unknown but there is a strong familiar tendency Autoimmune process Environmental Immunologic process Infectious agents-Bacteria, virus, mycobacterium Chemicals (pesticides) Stress Dietary - especially in people who eat decrease fiber diet IBD is characterized by a period of remission and exacerbation. Assessment Usual age of onset Fatty stool Rectal bleeding Abdominal pain Diarrhea Nutritional deficit, weight loss, anemia, dehydration Anal abscess Fever Crohns’s disease versus Ulcerative Colitis Crohn’s Disease Ulcerative Colitis 20-30 and 50-80 years Young adult to middle age (30-50) Frequent Absent Occasional: mucus, pus, fat Common: blood, pus, mucus in in stool stool After meals Predefecation Less severe 10-20 liquid stools per day common common common Present common Present 19 Complications for IBD Hemorrhage Fissures or fistula Malnutrition and nutritional deficiency Perforation or obstruction of the colon Enlargement of the colon-megacolon Fissures Fistulas Diagnosis of IBD Biopsy of colon Sigmoidoscopy or colonoscopy Occult stool test Serum albumin Antibody test (IGg) autoimmune Treatment of IBS Give anti inflammatory drugs : Sulfasalazine (Azulfidine) and oral steroids like budesonide (entocort EC) Give antibiotics Immunosuppressive meds Surgery if obstruction, stricture of fistula or abscess Surgical procedures include resection of the affected area with anastomosis. Nursing Intervention for IBS Promote rest Relieve rest Weigh pt periodically Monitor Intake and output Assess for pain and give pain meds If patient complain of pain in the rectal area sitz baths may be used Apply skin Protectants to the rectal area after cleaning gently and pat dry Increase fluid intake 2-3L unless contraindicated Monitor electrolytes periodically Assess signs and symptoms of dehydration The nurse should encourage the pt foods that are low in bulk- decrease fiber Offer nutritional supplement Offer psychological and emotional support Diet High calorie Low fat Low fiber May require TPN to rest bowel 20 Diverticular Disease Manifested in 2 clinical ways (forms) o diverticulitis o diverticulosis Diverticulitis Inflammation or infection of the diverticulum within the intestinal tract Diverticulosis outpouching of the walls of the colon Diverticular disease usually occurs due to a weakness in the wall of the intestine Most diverticulosis are found in the sigmoid colon More common in individuals above 60 years old with a long history of low residue diet Causes Constipation Associated with deficiency in dietary fiber diet Obesity Lack of blood supply to the intestine Mega colon (enlarged colon) Signs and Symptoms of Diverticular Disease Constipation alternating with diarrhea N/V Cramping pain in left lower quadrant of abdomen relieved by passage of stool or flatus Rectal bleeding Anorexia Abdominal distention/cramps Low grade fever Increased flatulence Increase white blood cell count Diagnostic Test History and physical exam Colonoscopy Sigmoidoscopy guaiac stool test (occult test) Medical Treatment Antispasmodics-Belladonna Tincture (Donnatal) is used for spastic colon. It is the drug of choice for diverticulosis Stool softeners Laxatives-bulk forming Antidiarrheal Analgesics Antipyretics 21 Nursing Intervention for Diverticular Disease Provide a well balanced diet- A diet high in fiber is recommended unless inflammation is present at which time client is NPO followed by a residue or bland diet. Increase fluids In the acute phase patient is usually on Bedrest NPO IV fluids NG tube Antibiotics Surgery Encourage fluid intake 2-3 liters per day unless contraindicated Avoid small poorly digested foods or foods that contain seeds, nuts etc. Popcorn Peanuts Cucumbers Watermelon Strawberries Grapes Guava Disorders of the Liver, Gallbladder and Pancreas Functions of the Liver a major role in digestion, absorption, metabolism and storage of nutrients converts excess glucose to glycogen and glycogen to glucose stores glycogen, fat soluble vitamins, iron and copper break down of fats, CHO and proteins the blood by removing foreign particles or substances from the blood produces and secretes bile needed for fat digestion helps detoxify drugs, toxins and other substances helps produces coagulating factors synthesize Vitamin K helps produce and store cholesterol Nursing Assessment of Liver Disease The liver performs many functions in the body so any alterations or dysfunction of the liver may lead to systemic effects Diagnostic Tests CBC Electrolytes Albumin level 22 Bilirubin levels ammonia will be high check Liver enzymes CT Scan MRI Liver biopsy is done to diagnose cirrhosis, hepatitis or other related diseases like cancer open biopsy or needle biopsy Open Biopsy- incision made into the abdominal cavity under general anesthesia Needle Biopsy- needle inserted through the abdominal wall to obtain the specimen Liver biopsy - high risk for bleeding because the liver is very vascular and because many patients with liver disease also have faulty clotting ability this also increases the chances of bleeding. Preoperative Nursing Care Explain procedure to pt Inform consent needed Keep pt NPO for 6-8 hours Obtain base line V/S Check CBC Check coagulating factors before the procedure Give preoperative sedative to calm and relax pt Ask the pt to empty the bladder Place the pt in a proper position with the right arm behind the head and ask the pt to remain still Patient is usually placed on the left side during the procedure Instruct pt to take a deep breath and hold it while the needle is being inserted to prevent accidental puncturing of the lung Post Operative Nursing care pt should remain on bed rest for 24 hours Assess V/S place pt on Right side for the first 2 hours after procedure (this prevent the possibility of bleeding)-a small pillow or small towel may be rolled under the biopsy site nurse should apply a pressure dressing over the puncture site and check the dressing frequently pt is advised to avoid coughing, straining or sneezing for the first couple of hours after procedure assess for pain and give pain medications assess for signs and symptoms of infection at the puncture site monitor for complications after liver biopsy o hemorrhage 23 o pneumothorax o puncturing of the bladder Cholecystogram X-ray visualization of the gallbladder Can visualize gallstones ingest a radio opaque dye that collects in the gallbladder. The patient is also asked to eat a high fat diet 2 days before the procedure and then a low or no fat diet on the day before the procedure and then the pt is asked to be NPO after midnight Before the pt is NPO the pt should take 6 radio opaque tablets called telepaque 5 minutes apart with water. These tablets contain iodine-so ask the pt if he or she has any allergies to iodine or seafood Side Effects of telepaque o N/V o Abdominal pain/cramps o Dysuria o Diarrhea ERCP (Endoscopic Retrograde Choliangiopancreatography) Endoscopic study of the gallbladder, liver and pancreas Dye is injected into the gallbladder, liver and pancreas and a scope is inserted through the esophagus in to the duodenum to help visualize the bile duct, pancreatic duct and common bile duct. Common therapeutic measures Paracentesis Usually done in pt with liver disease who has ascites. Abdominal paracentesis may be indicated if dietary restrictions and drug administration fail to control ascites and dyspnea is present. The procedure is performed at the bedside Preoperative Nursing Care ___________________________ Informed consent _____________________________ ask pt to void before procedure Pt is asked to be in an up right position in a chair or the side of the bed or can be lying down with feet and back supported Strict aseptic technique Fluid needs to be removed slowly to prevent shock or to prevent circulatory failure Postoperative Nursing Care Monitor V/S 24 Position the client in bed with the head of the bed elevated Maintain bed rest Weigh the client after the paracentesis Apply a pressure dressing at puncture site Monitor the amount, color and consistency of fluid being removed Disorders of the Liver Hepatitis Inflammation of the cells of the liver usually caused by a virus. When a pt has hepatitis there are local or systemic effects that occurs in the liver Local Liver becomes swollen due to the inflammatory response. If the swelling is profound 2 things happen The bile channels are compressed-damaging the cells of the liver that produces the bile Impaired blood flow to the liver causing the pressure to rise in the portal circulation Systemic Effects Are related to altered metabolic functions normally performed by the liver TYPES OF HEPATITIS Hepatitis A, B, C, D, and E, Hepatitis A Also called infectious hepatitis and epidemic hepatitis. Hepatitis A is primarily transmitted by the oral-fecal route. Signs and Symptoms of Hepatitis A Chills temperature malaise muscle weakness Abdominal pain in the RUQ Abdominal cramps Diarrhea Anorexia Jaundice High bilirubin levels Clay colored stools Bleeding Liver enlarged and tender Nursing Intervention for hepatitis A Identify individuals that are at high risk of hepatitis A Individuals living in poor sanitation conditions 25 Individuals in the military Food handlers Day care centers Individuals that are institutionalized Prisons Schools Nursing homes Wash hands thoroughly after eating and toileting Use clean water and food supplies Follow standard precautions when handling pt’s stool and urine Pt should receive immunoglobulin A before or within 48 hours after exposure All individuals with close contact with the pt must also receive the vaccine Hepatitis B Hepatitis B is also called serum hepatitis caused by HBV. Transmitted by parenteral routes and is present in all body fluids and stools Saliva Tears Semen Blood Urine Sweat Stool Breast milk Hepatitis B mostly transmitted by contaminated needles, sexual contact and contaminated equipments Incubation period for Hepatitis B is 2-5 months Signs and Symptoms No early signs and symptoms or only flu-like signs and symptoms Fatigue anorexia Malaise Low grade fever Nausea and vomiting Headaches Muscle aches Abdominal pain and cramps Chills If not treated jaundice like symptoms may result 26 Nursing Intervention for Hepatitis B Nurse should identify individuals that are high risk for Hepatitis B I V drug users Health care workers Homosexuals Prostitutes Hemodialysis blood donors blood transfusion pts who receive transplant Give Hepatitis B vaccine to high risk groups – immunoglobulin B vaccine Screen blood donors Dispose contaminated sharps appropriately Follow standard precautions Inform individuals to practice safe sex Hepatitis D Caused by the Delta Agent-the Delta agent is a defective RNA virus that survives only in the company of the HBV Coinfection with HBV Signs and Symptoms-same as Hepatitis B Hepatitis E Similar to Hepatitis A-very rare in the U.S. Mostly found in travelers in endemic areas. Poor sanitation No vaccine Cirrhosis of the Liver Is scarring or fibrosis of the liver resulting in the distortion of the liver structure and vessels or scarring of liver tissue which interferes with normal liver function and results in structural changes. Four types of cirrhosis of the liver Laenecc (alcoholic) cirrhosis Post necrotic cirrhosis resulting from previous acute viral hepatitis that produces scar tissue Biliary cirrhosis – chronic biliary obstruction and infection-scar tissue around the bile duct Cardiac cirrhosis – right heart failure (hepatomegaly) CAUSES There are many causes for cirrhosis- the major course is unknown. Other possible causes include: Chronic alcoholic use Viral hepatitis 27 Exposure to hepatotoxins Infection-autoimmune disease Chronic biliary tree obstruction Chronic severe right heart failure Signs and Symptoms of cirrhosis In the early stages signs and symptoms are subtle Weakness bruising Fatigue insomnia Fever pain in the RUQ Weight loss enlarged spleen Change in LOC spider angiomas Nausea and vomiting palmer erythema Diarrhea thrombocytopenia Constipation leucopenia Dark colored urine Fetor hepaticus Increased ammonia levels Sodium and water retention Peripheral neuropathy Lack of vitamin B12, thiamine and folic acid Decreased blood volume hematoma heartburn Loss of libido muscle wasting Edema Ascites Gynecomastia Anorexia Pruritis Complications of Liver Disease There are many complications that may result from liver disease. The student should familiarize themselves with the acronym CHEAP Coagulations disorder Hepatorenal syndrome Encephalopathy Ascitis Portal HTN Coagulation Disorders Thrombocytopenia Disseminated Intravascular Coagulation (DIC) Portal Hypertension A persistent increase in blood pressure within the portal vein. The portal vein delivers blood from the intestine to the liver. The liver damage causes a blockage of blood flow in the portal vein which allows the back up of in the portal system. The blood meets resistance to flow and seeks collateral venous channels around the high pressure area. 28 This obstruction causes the back up of blood into the spleen, the veins in the esophagus, stomach, intestines, abdomen and the rectum. These veins become engorged and dilated causing varices. Bleeding Esophageal varices Esophageal varices represent a life threatening medical emergency because of the potential of rupture causing massive hemorrhage. Esophageal bleeding can occur spontaneously with no precipitating factors; however any activity that increases intraabdominal pressure may increase the likelihood of bleeding. Esophageal varices can also be caused by coughing forcefully, straining or lifting heavy object, or by spicy food or acidic GI content. Ascites Is the accumulation of fluid within the peritoneal cavity. Ascites may be caused by the following: Increased hydrostatic pressure from portal hypertension Accumulation of plasma protein primarily albumin Inability of the liver to synthesize albumin Treatment of ascites Low sodium diet as an initial means of controlling fluid accumulation in the abdominal cavity Advise the client to read sodium content labels and to adhere to the sodium restrictions Limit fluid intake Give vitamin supplements such as thiamine, folate, zinc Administer diuretic to reduce fluid accumulation and to prevent cardiac and respiratory impairment Monitor intake and output Weigh daily Measure abdominal girth every 4 hours Prepare the patient for paracentesis Plasma expanders to help push fluid back into the circulation Hepatic Encephalopathy Also referred to as portal-systemic encephalopathy Caused by the accumulation of ammonia or other chemical or noxious substances in the brain or in the systemic circulation. The failing liver is unable to metabolize or detoxify ammonia, a waste product of protein metabolism. Signs and Symptoms of Hepatic Encephalopathy Neurologic symptoms and is characterized by an altered level of consciousness, impaired thinking processes and neuromuscular disturbances 29 Early signs and symptoms Restlessness Changes in LOC or diminished responsiveness Confusion Lethargy Irritability Apprehension Drowsiness Inability to concentrate Forgetfulness Late signs and symptoms Muscle twitching (facial twitching and fasciculation) Asterixis –flapping tremors of the hands when extending the arms Stuporous Hyperreflexia Marked mental confusion Positive babinski sign seizures Somnolence Fetor hepaticus-Fruity and musty breath Coma Seizures Treatment of hepatic Encephalopathy Assess level of consciousness frequently Identify factors that may precipitate hepatic encephalopathy: High protein diet Infections Hypovolemia Constipation Drugs-opoids, hypnotics, sedatives, analgesics and diuretics GI bleeding Administer lactulose to promote the excretion of ammonia in the stool give antibiotic – Neomycin is usually ordered to decrease colonic bacteria that breaks down protein and prevents the formation of ammonia reduce protein and fat intake and give simple carbohydrates restrict foods high in ammonia levels chicken egg yolk ham bacon butter milk cheddar cheese peanut butter onions 30 Nursing Intervention for Cirrhosis Goal of treatment is to prevent complications of liver disease The nurse should identify the cause and eliminate the cause In the acute phase of the cirrhosis the pt should be on bed rest Nurse should space nursing care because this allows the liver to regenerate Assess the pts neurological status every hour Give IV fluid to hydrate patient and correct electrolyte imbalances except if pt has ascites If ascites is present the pts fluid intake should be restricted to 1-1 ½ L Monitor I & O daily Weigh daily Measure abdominal girth every 4 hours Assess pt for peripheral edema or sacral area Give vitamin high in thiamine, pyridoxine and B12,folic acid, iron and zinc Avoid foods that produce high ammonia levels (chicken, ground beef, ham, bacon, peanut butter, egg yolk, cheese) offer small frequent meals give neomycin an antibiotic to reduce the bacterial count in the intestines To lower ammonia levels give lactulose a laxative that binds to ammonia and help excrete ammonia though the stool Inspect the skin daily Apply lotion on the skin to prevent dryness of the skin-if the skin is too dry this may cause pruritis If pt has pruritis advice the pt not to scratch the area this may cause bleeding. The Pt may apply pressure on the area or use a hair dryer set on low Make sure pt wears gloves/ mittens to avoid scratching the area Avoid cold/hot water – use warm water while bathing. Institute bleeding precautions Give vitamin K (to promote coagulation) Inform pt to avoid alcohol or medications that are known to be hepatotoxic– Tylenol, INH, oral contraceptive, antipsychotics, sedatives, opoids The Biliary Tract Includes the gall bladder and the bile duct The gall bladder stores bile which emulsifies fat, stimulates pancreatic secretion and activates pancreatic lipase. Nursing Assessment of the Biliary System Assess past medical history Assess for indigestion Assess for weight loss/ weight gain Assess patient stool (color, amount and consistency Assess vital signs Assess drug history 31 Disorders of the Biliary Tract Gallbladder disease is the most common health problem in the U.S. The two most common disorders of the gallbladder are Cholecystitis Cholelithiasis Risk Factor for Gallbladder Disease obesity familiar predisposition sedentary lifestyle use of estrogen (or oral contraception) More common in women than in men -think about 5Fs Female Fat Fair Forty Fertile Cholecystitis and Cholelithiasis Cholecystitis is an acute inflammation of the gallbladder or the cystic duct caused by the lodging of a gallstone in the duct. Cholecystitis can also be caused by bacteria or toxic chemicals, anesthesia, starvation, trauma, medications (opiods), surgery, TPN (hyperalimentation) (no fat) Signs and Symptoms Pt may be asymptomatic In the early phase of the disease the signs and symptoms include: Intolerance to fatty or spicy foods N/V Abdominal cramps Severe abdominal pain in the RUQ that radiates to the right shoulder and back Abdominal tenderness Abdominal guarding Fever Heartburn Diaphoresis As the condition progresses patient may start to have jaundice like symptoms Jaundice high bilirubin level high ammonia levels Dark colored urine fat in the stool (steatorrhea) White or clay colored stool 32 Biliary colic pain-spasmodic pain due to the obstruction of the duct and occurs when due to an attempt to move the stone Petechiae or ecchymosis Medical Treatment The goal of treatment depends on the condition, if the patient has cholecystitis supportive treatment is done Rest Keep pt NPO Give IV fluids Medications –antibiotics and analgesic Reduce fever Promote nutrition Dissolution therapy-administration of bile salts Lithotripsy Surgery-cholecystectomy Lithotripsy-EXTRACORPORAL SHOCKWAVE LITHOTRIPSY Nursing Intervention (Lithotripsy) Coagulation study-PT, PTT, platelet, fibrinogen Empty bladder before the procedure Relieve anxiety After the procedure monitor for complications Increase the pt’s fluid intake 3-3 ½ L unless contraindicated-fluid intake helps to push the crushed stone out of the body Assess for pain and medicate appropriately Inform the patient that small bright red tinged blood is normal after the procedure; excessive amount of blood in the urine should be reported to MD Give prophylactic antibiotic after the procedure to prevent infection Cholecystectomy Open cholecystectomy. To prevent this obstruction a T-tube is inserted. The T-tube is placed to maintain the flow of bile from the liver to the small intestine. Postoperative Nursing Intervention for Cholecystectomy Avoid fried, spicy or fatty foods Encourage low fat, high carbohydrate, high protein diet Low fat diet-Inform the patient to consume skim milk, cooked fruits, rice, lean meats, mashed potatoes, non gas forming vegetables, bread Patients should avoid eggs, cream, pork, fried foods, cheese and rich dressings Reduce weight Assess for pruritis due to the blockage of bile ducts. This blockage would cause the accumulation of bile salts under the skin-give cool baths and apply lanolin lotion, reduce room temperature, trim nails, have the patient wear mittens or gloves and administer cholestyramine (Questran) 33 Notify physician if patient has clay colored stools, dark urine, jaundice and pruritis because this mean bile is obstructed Check liver function Inform patient on oral contraceptives to seek alternative birth control measures if taking bile salts Reduce patient anxiety and encourage patient to verbalize fears and concerns Monitor T-Tube if present for amount, color and odor of drainage T-Tube inserted to ensure drainage of bile from common bile duct until edema subsides Place the pt in a semi fowlers position Follow MD orders when to clamp the T-tube-The T-tube may be clamped 12hrs before meals this allow bile to flow in the duodenum Observe for jaundice-yellow sclera, stool that does not slowly progress from light to dark color after removal of tube THE PANCREASE Fat – lipase Protein – trypsin Carbohydrate – amylase Pancreatitis Is an inflammation of the pancreas, it can be acute or chronic Acute Pancreatitis Caused by autodigestion, it occurs when there is digestion of the pancreas by its own enzymes primarily trypsin. Other causes include Alcohol abuse-excessive use of alcohol Diuretics (thiazide) Steroids Oral contraceptives Tylenol Cholecystitis Increase calcium High cholesterol diet High triglyceride levels Infection Gallstones Chronic Pancreatitis Prolong alcohol use Cholelithiasis (Gall Stones)-stone lodge in the pancreatic duct Surgery on or near the pancreas Signs and Symptoms of Pancreatitis 34 Severe mid epigastric or left upper quadrant pain-this pain may radiate to the back of shoulders The pain is aggravated by alcohol or eating a fatty meal The intensity of the pain when the patient assumes a lying position Abdominal distention Firm board like or rigid abdomen Bowel sounds are absent Nausea and Vomiting Flushing of the skin Increase temperature Decrease BP Increase Pulse Cool/clammy skin Dyspnea Grey Turner sign-bluish discoloration of the flank area Cullen sign-bluish discoloration of the periumbilical area Weight loss Dark concentrated urine High bilirubin levels Increase blood sugar in the urine and blood steatorrhea Diagnostic (Pancreatitis) Pancreatic enzymes Amylase 60-160 (normal) with pancreatitis Lipase 0-160 Trypsin Increase blood sugar Liver function test bilirubin levels Ammonia Check kidney function ERCP X-Ray 24 hour urine test Treatment for Pancreatitis Keep pt NPO-prevent visualization of food since gastric secretions are stimulated by the sight or smell of food Insert NG tube Maintain bed rest Assess for pain and give pain meds – No morphine Assess for the location, radiation, character, intensity and duration Instruct the patient to sit up and lean forward to reduce the pain knees bent Control the pts fever by giving antipyretics 35 Monitor I&O Weight pt daily Stress the importance of stopping alcohol Avoid caffeinated, spicy or fatty foods-these foods stimulate gastric and pancreatic secretions and may precipitate pain Place pt in a semi fowler position or side lying position with knees flexed Give pancreatic enzymes with meals or snacks. They should be swallow whole or sprinkle on food Encourage small frequent meals Check pt albumin levels Monitor the amount, color and consistency of the stool Individuals that have pancreatitis- color of stool is white or clay colored and contains fat Check bowel sounds q4hrs – if bowel sounds are present the NG tube may be removed Check blood sugar q4hrs if high – insulin may be administered Give antianxiety medications because anxiety increase pancreatic secretion by stimulating the autonomic nervous system Administer antiemetic if patient has nausea and vomiting Administer antispasmodic-Bentyl to relieve spasms Assess for signs and symptoms of infection