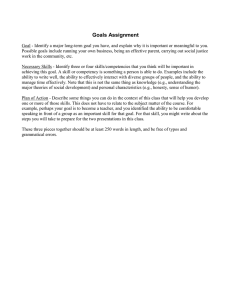
CONTINUING EDUCATION Ongoing Professional Performance Evaluation: Advanced Practice Registered Nurse Practice Competency Assessment Sharon L. Holley, DNP, CNM ABSTRACT The Ongoing Professional Performance Evaluation and the Focused Professional Practice Evaluation have been required by The Joint Commission for providers, including advanced practice registered nurses, who are credentialed and privileged in an accredited hospital. There are 6 required domains for these evaluations. The objective of these evaluations is to monitor for competence in the credentialing and privileging process for hospitals. The 6 domains come from medical education competencies. Nursing must develop a set of competencies to measure the performance of advanced practice registered nurses or continue to be measured by physician metrics. Keywords: APRN, competency, evaluation, FPPE, OPPE Ó 2016 Elsevier, Inc. All rights reserved. Sharon L. Holley, DNP, CNM, is an assistant professor teaching midwifery at the Vanderbilt University School of Nursing in Nashville, TN. She also currently serves as director for the Vanderbilt School of Nursing Faculty Nurse-Midwife Practice. She can be reached at sharon.holley@vanderbilt.edu. In compliance with national ethical guidelines, the author reports no relationships with business or industry that would pose a conflict of interest. INTRODUCTION I n 2014, the American Association of Nurse Practitioners estimated there were > 205,000 nurse practitioners (NPs) in the United States. Of that number, 44.8% hold hospital privileges.1 Although many NPs work full time in the hospital setting, most see patients in the ambulatory setting and are credentialed to see their patients who are hospitalized. NPs are 1 of the 4 types of advanced practice registered nurses (APRNs). The American This CE learning activity is designed to augment the knowledge, skills, and attitudes of nurse practitioners and assist in understanding performance evaluations of APRNs. At the conclusion of this activity, the participant will be able to: A. Describe the purpose of the Ongoing Professional Performance Evaluation (OPPE)/Focused Professional Practice Evaluation (FPPE) B. List 6 domains used for competency evaluation in OPPE/FPPE and medical education C. Compare/contrast competency requirements for PAs with APNs The authors, reviewers, editors, and nurse planners all report no financial relationships that would pose a conflict of interest. The authors do not present any off-label or non-FDA-approved recommendations for treatment. This activity has been awarded 1.0 Contact Hours of which 0 credits are in the area of Pharmacology. The activity is valid for CE credit until March 1, 2018. Readers may receive the 1.0 CE credit for $5 by reading the article and answering each question online at www.npjournal.org, or they may mail the test answers and evaluation, along with a processing fee check for $10 made out to Elsevier, to PO Box 1461, American Fork, UT 84003. Required minimum passing score is 70%. This educational activity is provided by Nurse Practitioner AlternativesÔ. NPAÔ is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. Accreditation does not imply endorsement by the provider, Elsevier, or ANCC of recommendations or any commercial products displayed or discussed in conjunction with the educational activity. www.npjournal.org The Journal for Nurse Practitioners - JNP 67 College of Nurse-Midwives found that, as of 2015, there are 11,018 certified nurse-midwives (CNMs) and 88 certified midwives (CMs). Although there are no specific numbers for hospital-credentialed CNM/ CMs, 95% of births attended by CNM/CMs occur in the hospital setting.2 Certified registered nurses (CRNAs) number around 48,000, with approximately 37% of them employed by hospitals and another 34% employed by an anesthesia group, with most credentialed to provide patient services in the hospital setting.3,4 Although not all 50 states recognize the clinical nurse specialist (CNS) as an APRN role, the list is growing. It is difficult to find exact numbers for how many hold hospital privileges, but this too is known to be increasing. To simplify terminology, for the remainder of this report, the term APRN is used to represent NP, CNM/CM, CRNA, and the CNS designations. Herein I focus on those who hold credentialing and privileging in hospitals that are accredited by The Joint Commission and the requirement for the Ongoing Professional Performance Evaluation (OPPE) and the Focused Professional Practice Evaluation (FPPE). APRNs, and other nonphysician providers, are now required to be evaluated based on criteria that come from physician competencies, rather than nursing competencies, for credentialing and privileging decisions. The OPPE and FPPE have been required since 2008 for all medical staff and providers who are granted privileges in hospitals accredited by The Joint Commission.5,6 These providers include not only physicians but also physician assistants (PAs), APRNs, including CNM/CMs, and CRNAs.6 The OPPE is a screening tool used on an ongoing basis to assess the competency of medical staff and providers. The OPPE/FPPE is used to evaluate the care provided to determine whether it meets accepted standards for provision of quality care.5 The OPPE is also used identify those who may benefit by learning from the results of the OPPE measures and implement performance improvement. If there is a new provider to the system, or an identified area that needs evaluation focus, then the FPPE is implemented to examine specific measures. Collecting meaningful data in a consistent and ongoing approach provides feedback opportunities for each provider so they may implement changes 68 The Journal for Nurse Practitioners - JNP immediately to their practice when needed.7 The ongoing evaluation process also affords the opportunity for analysis and can be used for faster response for quality improvement at the level of the individual provider as well as a given set of providers in a specific practice. This is now part of the decision-making process when providers are reviewed for a new request for credentialing or privileging or for renewal of credentialing. The OPPE/FPPE is meant to be more objective and continuous in its approach as compared with older methods that were more subjective, such as letters of reference. The Joint Commission has left the specific methods for data collection up to the individual hospitals and departments.8 This newer type of evaluation process has created some unique challenges for APRNs to have informative OPPE/ FPPE collection methods that can show competency for their particular specialty and practice setting. BACKGROUND The Institute of Medicine defines quality health care as, “The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”9 Since 1996, the Institute of Medicine has initiated a succession of reports focused on improving the quality of health care in the United States. All these reports have demonstrated how wide the gap is in relation to what is known to be quality care versus what is delivered in practice.10,11 The most recent report identifies 15 core metrics that stipulate benchmarks that will be used to improve health care in the nation as a whole as well as health care system performance. Two of these areas are patient safety and provision of evidenced-based care. Patient safety is a culture in which the priority is on prevention of errors and adverse effects through system performance throughout the organization. Evidenced-based care stresses the importance of using scientific evidence appropriately in the delivery of health care.12 The Agency for Healthcare Research and Quality, devoted to improving patient outcomes, has noted that quality measurement is a type of evaluation used in many industries and is now used increasingly in health care. When developing a quality measure the collection tool must be reliable, Volume 12, Issue 2, February 2016 valid, and standardized.13 The OPPE and FPPE both meet the goals set by these organizations by standardizing the format in which data should be collected and reported, as well as utilization of that data to evaluate the provision of quality patient care. Prior to the last half of the 20th century, individual provider competency was evaluated through education and board certification. Physicians functioned as contractors to a hospital where they treated patients. However, after a landmark case in 1965, a hospital could be held liable for the actions of a physician as an employee of that hospital. After this, hospitals began to implement verification of individual competency. This was accomplished by setting up processes that utilized references, educational training, and certification.6 However, what was not included in this process for competency assessment was a quality and safety component. Realizing this need, The Joint Commission began requiring the OPPE and FPPE to help determine that the care provided by credentialed and privileged providers meets acceptable performance, quality, and safety standards.5,14 DEFINITIONS OPPE The OPPE is a document summary of ongoing data collected for the purpose of assessing a practitioner’s clinical competence and professional behavior. The information collected during this process is factored into decisions to maintain, revise, or revoke newly requested or existing privilege(s) before or at the end of the 2-year license and privilege-renewal cycle. The intent for the OPPE is that the organization examine data on performance for all practitioners with privileges on an ongoing basis, rather than at the 2-year reappointment process. Performing the additional OPPE/FPPE verification of data allows a hospital to take timely action, if needed, to improve performance.15 The OPPE also allows verification that a provider is delivering competent quality patient care with professional behavior. FPPE The FPPE is a time-limited evaluation of practitioner competence in performing newly requested specific privileges. The intent is for the organization to have a focused review for all new privileges of new www.npjournal.org applicants as well as all new privileges for existing practitioners. There is no exemption for board certification, documented experience, or reputation.14 There are 3 distinct reasons for the FPPE: 1. Newly hired providers are evaluated using the FPPE template after the first 6 months of employment so that their competence is assured after adequate time for orientation. 2. Currently credentialed providers who are requesting a new privilege, such as an advanced skill not typically covered with board certification, yet still within the scope of practice of that specialty. 3. Whenever a question arises regarding a practitioner’s ability to provide safe, high-quality patient care or identification of unprofessional behavior. Privileging Privileging is the process whereby health care organizations, including hospitals, authorize providers to offer specific services to their patients.16 The specific scope and content of patient care services, or clinical privileges, are authorized for a health care practitioner to perform within a hospital. Privileging is based on evaluation of the individual’s credentials and performance.15 Credentialing Credentialing is the process of obtaining, verifying, and assessing the qualifications of a provider performing patient care or services within, or for, a health care organization. Credentials include documented evidence of licensure, education, training, experience, or other qualifications. Examples of credentials are a certificate, letter, or experience that qualifies an individual to do something. A credential may be a letter, badge, or other official identification that confirms a person’s position or status. A hospital, or health care organization, obtains primary source verification of the licensed independent practitioner’s education, training, certificates, and licensure from the primary source, and maintains the file of information.17 Credentialing is typically renewed every 2 years. REQUIRED DOMAINS FOR EVALUATION The Accreditation Council for Medical Education (ACGME) is the accrediting body for graduate The Journal for Nurse Practitioners - JNP 69 Table. Comparison of ACGME With The Joint Commission’s 6 Domainsa Medical Knowledge Practice-based Learning and Improvement Interpersonal and Communication Skills Provide care that is compassionate, appropriate, and effective treatment for health problems and to promote health Demonstrate knowledge about established and evolving biomedical, clinical, and cognate sciences and their application in patient care Show an ability to investigate and evaluate patient care practices, appraise and assimilate scientific evidence, and improve the practice of medicine Demonstrate skills that result in effective information exchange and teaming with patients, their families and professional associates (eg, fostering a therapeutic relationship that is ethically sound and uses effective listening skills with nonverbal and verbal communication; work as both a team member and, at times, as a leader) Demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to diverse patient populations Demonstrate awareness of and responsibility to the larger context and systems of health care; be able to call on system resources to provide optimal care (eg, coordinating care across sites or serving as the primary case manager when care involves multiple specialties, professions, or sites) Joint Practitioners Commission are expected to provide patient care that is compassionate, appropriate, and effective for the promotion of health, prevention of illness, treatment of disease, and care at the end of life Practitioners are expected to demonstrate knowledge of established and evolving biomedical, clinical and social sciences, and the application of their knowledge to patient care and the education of others Practitioners are expected to be able to use scientific evidence and methods to investigate, evaluate and improve patient care practices Practitioners are expected to demonstrate interpersonal and communication skills that enable them to establish and maintain professional relationships with patients, families, and other members of health care teams Practitioners are expected to demonstrate behaviors that reflect a commitment to continuous professional development, ethical practice, an understanding and sensitivity to diversityb and a responsible attitude toward their patients, their profession and society Practitioners are expected to demonstrate both an understanding of the contexts and systems in which health care is provided, and the ability to apply this knowledge to improve and optimize health care Patient Care ACGME Professionalism Systems-based Practice ABMS ¼ American Board of Medical Specialties; ACGME ¼ Accreditation Council for Medical Education; FPPE ¼ Focused Professional Practice Evaluation; OPPE ¼ Ongoing Professional Performance Evaluation. a Six Core Competencies for medical education identified by ACGME and American Board of Medical Specialties (AMBS).14 b Six Core Competencies for The Joint Commission.15 medical education. ACGME determines and enforces standards for residency and fellowship training programs. The American Board of Medical Specialties is an organization of approved medical specialties responsible for board certification of physicians in those specialties. ACGME first described 6 domains for clinical competency for physicians and began 70 The Journal for Nurse Practitioners - JNP using them in 1999.18 These domains are: (1) patient care; (2) medical and clinical knowledge; (3) practicebased learning and improvement; (4) interpersonal and communication skills; (5) professionalism; and (6) systems-based practice.14 The American Board of Medical Specialties then began using these same 6 domains as a framework for initial board certification Volume 12, Issue 2, February 2016 and maintenance. The next step in this evolving process is ongoing work by ACGME with the newer Next Accreditation System that will begin to link improved performance in clinical practice by physicians, as well as practice outcomes over their career in practice.19 In this effort, The Joint Commission incorporated those same 6 domains for evaluation of competency into the OPPE and FPPE (see Table). Originally, the OPPE and FPPE were interpreted for physicians, but in 2011 The Joint Commission made it clear these evaluations are required for all providers credentialed and privileged. The OPPE/FPPE are now required for APRNs, CNM/CMs, and PAs as well.5,7,8,15 ADVANCED PRACTICE PROVIDERS Nonphysician Provider Competencies PAs, CNMs/CMs, CRNAs, and other APRNs are all required by The Joint Commission to be evaluated more often than once per year using the OPPE formula of 6 domains that were originally created as an assessment for medical education of physicians. Each of these nonphysician advanced practice specialties has their own certifying body and board certification process, only one of which are based on these 6 domains. This creates a challenge to try to find methods that adequately assess individual performance and scope of practice competency of nonphysician providers. PAs. The Physician Assistant Education Association, National Commission on Certification of Physician Assistants, Accreditation Review Commission on Education for Physician Assistant, and the American Academy of Physician Assistants described the importance of maintaining professional competence through continuous professional development. These organizations define competence as application of specialized knowledge. The PA profession adopted the same 6 domains in 2005 for competency that was originally developed by the ACGME.20,21 Although position papers by the American Academy of Physician Assistants indicate agreement with other medical organizations on the terminology and definitions of what these 6 domains are, they note the caveat that PAs are not physicians and therefore this model of competency assessment “should be carefully applied to the PA profession.”20(p5) These same 4 www.npjournal.org organizations worked together to answer this dilemma by developing a self-assessment titled the “Physician Assistant Competencies: A Self-evaluation Tool.” This tool is focused on their own professional competency within each of the 6 domains while also used to self-identify areas they need to strengthen through some type of continuing educational opportunity. This self-evaluation is part of a larger demonstration of continuing competency that includes maintaining board certification, continuing education, as well as quality improvement projects meant to improve patient care.20 CNMs/CMs. CNM/CMs are certified by the American Midwifery Certification Board (AMCB), which is a national board that certifies graduates from nurse-midwifery and midwifery programs accredited by the Accreditation Commission for Midwifery Education (ACME). The American College of Nurse-Midwives (ACNM) is the professional organization that represents CNM/CMs. The AMCB, ACME, and ACNM utilize the Core Competencies for Midwifery Practice as the basis for what comprises competent midwifery practice. The competencies include: 1. The Hallmarks of Midwifery. 2. Components of Midwifery Care: Professional Responsibilities of CNMs and CMs. 3. Components of Midwifery Care: Midwifery Management Process. 4. Components of Midwifery Care: Fundamentals. 5. Components of Midwifery Care of Women. 6. Components of Midwifery Care of the Newborn.22 These competencies can be expanded to advanced skills, but the core competencies are seen as the basic knowledge, skills, and behaviors expected for any new CNM/CM. The core competencies were initially adopted by the ACNM in 2002.23 In 1986, the ACNM developed the Continuing Competency Assessment program as a voluntary way to demonstrate continuing competency. The Continuing Competency Assessment program was discontinued in 2010 and continuing competence is now maintained through the AMCB’s Certification Maintenance Program.20 Competency is now determined by maintenance of board certification, The Journal for Nurse Practitioners - JNP 71 20 hours of continuing education, and the option to complete 3 modules or take a reexamination of the certification exam within a 5-year cycle.24 CRNAs. CRNAs are initially certified by the National Board of Certification and Recertification for Nurse Anesthetists. In 1978, a recertification process was established for verification of continued competency. In 2011, the Board began work with the American Association of Nurse Anesthetists to redevelop the Continuing Professional Certification program. This work has been ongoing with the anticipated start date for the new changes taking affect August 1, 2016. The Continuing Professional Certification is an 8-year program made up of two 4-year cycles. Currently, the requirements include maintaining board certification by recertifying, every 8 years, completion of 60 Class A (assessed) continuing education units and 40 Class B (professional development) continuing education units all in a 4-year cycle. There is also a voluntary set of core modules that are based in 4 core areas and 1 module should be completed in each core area within each both of the 4-year cycles.25 APRNs. There has been some work to move toward creating competencies for general nursing practice as well as nursing education. An example is the Quality and Safety Education for Nurses project, a global nursing initiative that developed recommendations for nursing competencies in the areas of: (1) patient-centered care; (2) teamwork and collaboration; (3) evidenced-based practice; (4) quality improvement; (5) safety; and (6) informatics.23 The National League for Nurses has created competencies for nursing education for development of nursing curriculum and continuing education.26 The Commission on Collegiate Nursing Education, an accreditor for nursing education programs, the American Association of Colleges of Nursing and the American Nursing Association have recommended, in a white paper on APRN practice, that clinical education and assessment should be competencybased, although no specific competencies were identified. The recommendation in the white paper states the need to standardize core competencies and assessment tools in nursing education programs for educators to utilize similar evaluative approaches for assessing competency with advanced practice nursing 72 The Journal for Nurse Practitioners - JNP students.27,28 Ostensibly these competencies in nursing education could also be used with board certification and clinical evaluation in the working environment. Some advanced practice nursing specialties have already begun work on specialtyspecific competencies. The Consensus Model for APRN Regulation: Licensure, Accreditation, Certification and Education has defined an APRN as someone with national certification; preparation in health promotion and assessment, diagnosis, and management of patient problems, which includes prescribing of nonpharmacologic and pharmacologic interventions, providing direct patient care; and graduate-level education in 1 of 4 recognized roles. These roles include: 1. CRNA. 2. CNM. 3. CNS. 4. Certified Nurse Practitioner.29 Although the Consensus Model just described does not define competencies, it does state that educational programs must prepare graduates with the nationally recognized ARPN core courses, role, and population-focused competencies. The 3 core courses are: (1) health assessment; (2) advanced physiology/pathophysiology; and (3) advanced pharmacology. The National Organization of Nurse Practitioner Faculties promotes NP education at the national and international levels. The organization has developed curriculum guidelines for NP educational programs and competencies for entry-level NP as well as domains and core competencies for NP practice with specific educational levels and specific population focus. Their work has created a way to standardize what the expectations are, but does not address how to measure individual practice competency in the same way the OPPE is designed to do. Overall, all APRN organizations recommend ongoing maintenance of competency in some form or fashion using board certification, continuing education, completion of various assigned modules for learning, or other requirements, such as a specified number of clinical hours in the specialty. However, each APRN specialty has its own requirements that must be met and kept updated. Volume 12, Issue 2, February 2016 Challenges Although the OPPE/FPPE process was required by The Joint Commission starting in 2008, before 2011 only physicians on medical staff were required to complete the OPPE/FPPE process, whereas nonphysician providers were allowed to have alternative methods for credentialing and privileging. However, after the 2011 release of the OPPE/FPPE BoosterPak, all APRNs and PAs who provide “medical level of care” must use the same medical staff process for credentialing and privileging as physicians.15 Only those APRNs and PAs who are not providing medical level of care are allowed to use an alternative pathway for these processes. This means all APRNs and PAs who seek to provide patient care in these hospitals undergo a credentialing process similar to that of physicians and are granted privileges through the authority granted to the medical staff through the board of directors.30 Therefore, most hospitals have opted to use the same method of OPPE and FPPE for physicians as well as APRNs and PAs. This necessitates an understanding of what both OPPE and FPPE measure and how it is applicable to nonphysicians, including ARPNs. Often data that could be collected to inform the OPPE/FPPE, such as the specific number of times certain procedures are performed or documented patient encounters performed, are billed and accounted for under the physician the APRN or PA is working for. This can make it hard to separate out the work each individual has done and the quality of work performed. The creation of metrics that are identifiable down to the individual provider are needed. Some data may be able to be identified for units that track statistics, or some may find they have to track their own data for documentation that supports the competency being maintained. For example, if a specific skill is performed, the individual may need to create a method to track these encounters and outcomes that may otherwise show up under the data for the physician they work with. Objectively demonstrating ongoing competency requires access and analysis to data that is meaningful. Noting only numbers of times something is done is not the same as measuring the quality of care performed or following through on outcomes to see that the care delivered was indeed www.npjournal.org appropriate. This is why, ideally, some of the data should have measureable objectives that can be also compared with other providers doing similar work. For example, are the outcomes with a certain procedure within the accepted norms for local, or national benchmarking results? Are readmission rates or infection rates at acceptable levels when compared with guidelines? If they are not, this may be because the results are stellar, or it may indicate they are suboptimal. In the latter case, a closer look may reveal a trigger for an FPPE for a particular provider who needs re-education on technique or instruction on when to offer or not offer a procedure. The OPPE is required to be completed more often than once a year to quickly identify triggers, or concerns, that can be addressed and corrected in a timelier manner than once every 2 years, as with previous credentialing methods. If concerns are serious, an FPPE may be indicated on the individual trigger while maintaining the rest of the OPPE cycle. Analysis of the data gives meaning to what is being accumulated and reported. Ideally, the individual provider will be able to see the results of this analysis and have an opportunity to respond with more positive results. The field of APN must continue to develop core competencies that APRN competency can be measured against. Nursing lags behind medicine, and PA’s, on identifying competency domains to measure against. Therefore advanced practice nurses find themselves being evaluated with six domains originally constructed to measure physician education and clinical performance. As noted earlier, there is an ongoing global nursing initiative to develop standardized general nursing competencies, but this has yet to be adopted either nationally or internationally. APRNs may have the same or differing needs for identified competencies as general nursing, but this also needs to be identified. If nursing does not continue to move this work forward, the 6 domains will remain in place and the unique qualities of what makes APN unique from physician practice will not be evaluated for the purposes of quality improvement, competency assessment, or decisions made in relation to credentialing and privileging. To this point, nursing organizations have remained silent on this issue. The Journal for Nurse Practitioners - JNP 73 Obtaining Data for the OPPE/FPPE Demonstrating competency through the OPPE/ FPPE process requires a mechanism for collection of data that drills down to the individual provider as well as having comparative data when appropriate. Data collected and analyzed can be used to fit within the required 6 domains identified by The Joint Commission. CONCLUSION The Joint Commission has required the OPPE and FPPE processes for all credentialed and privileged providers in hospitals they accredit. This process is mandatory for any physician, PA, APRN, CNM/ CM, or CRNA who provides medical-level patient care. The OPPE is an ongoing evaluation process that monitors for continuing competence by using both objective and subjective data. It is used to immediately identify any specific provider in need of performance improvement monitoring through the FPPE process. Ideally, the responsiveness to concerns will help improve overall health care quality by monitoring individual provider competence. The use of the 6 domains, with origins based in physician education and certification, allows for flexibility with regard to what data to include in the monitoring process. APRN educational, certifying, and professional organizations must work toward fully developing a robust set of competencies. Otherwise, APRNs will continue to be evaluated using a metric originally designed for evaluating physicians. References 1. American Association of Nurse Practitioners. NP fact sheet. 2015. http:// www.aanp.org/all-about-nps/np-fact-sheet. Accessed July 30, 2015. 2. American College of Nurse-Midwives. Essential facts about midwives. 2015. http://www.midwife.org/Essential-Facts-about-Midwives. Accessed August 16, 2015. 3. American Association of Nurse Anesthetists. Who are we. 2015. http:// www.aana.com/aboutus/Pages/Who-We-Are.aspx. Accessed August 16, 2015. 4. Brassard A, Smolenski, M. Removing barriers to Advanced Practice Registered Nurse Care: Hospital Privileges. Insight on the Issues, 55. 2011. http:// campaignforaction.org/sites/default/files/RemovingBarriers-HospitalPrivileges .pdf. Accessed August 16, 2015. 5. Wise RA. OPPE and FPPE: Tools to help make privileging decisions. [Web log comment]. 2013. http://www.jointcommission.org/jc_physician_blog/oppe_ fppe_tools_privileging_decisions/. Accessed August 21, 2013. 6. Hunt JL. Assessing physician competency: An update on The Joint Commission requirement for ongoing and focused professional practice evaluation. Adv Anat Pathol. 2012;19:388-400. 7. Ziaya, P. Using OPPE as a performance improvement tool. [Web log comment]. 2014. http://www.jointcommission.org/jc_physician_blog/using _oppe_as_a_performance_improvement_tool/. Accessed February 5, 2014. 8. Holley SL, Ketel C. Ongoing Professional Practice Evaluation (OPPE) & Focused Professional Practice Evaluation (FPPE): understanding the process from an advanced practice viewpoint. J Midwifery Women’s Health. 2014;59(4):453-459. 74 The Journal for Nurse Practitioners - JNP 9. Institute of Medicine. Crossing the quality chasm: The IOM health care quality initiative. 2013. http://www.iom.edu/Global/News%20Announcements/ Crossing-the-Quality-Chasm-The-IOM-Health-Care-Quality-Initiative.aspx. Accessed July 18, 2015. 10. Institute of Medicine. To err is human: Building a safer healthcare system. Committee on Quality of Health Care in America. 1999. Washington, D.C., National Academy Press. 11. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Committee on Quality of Health Care in America. 2001. Washington, D.C., National Academy Press. 12. Institute of Medicine. Vital signs: Core metrics for health and health care progress. 2015. Washington, D.C., National Academy Press. 13. Agency for Healthcare Research and Quality. Understanding quality measurement. 2012. http://www.ahrq.gov/professionals/quality-patient-safety/ quality-resources/tools/chtoolbx/understand/. Accessed July 18, 2015. 14. American Board of Medical Specialties. Based on core competencies. 2015. http://www.abms.org/board-certification/a-trusted-credential/based-on-core -competencies/. Accessed July 18, 2015. 15. The Joint Commission. Standards BoosterPak for Focused Professional Practice Evaluation/Ongoing Professional Practice Evaluation (FPPE/OPPE). 2011. www.jointcommissionconnect.org/NR/rdonlyres/A846669C-D456-44D5 -A1AF-DC47975CEE8C/0/BP FPPEOPPE.pdf. Accessed July 18, 2015. 16. U.S. Department of Health and Human Services. Credentialing & Privileging of Health Center Practitioners. 2015. http://bphc.hrsa.gov/ programrequirements/pdf/pin200116.pdf. Accessed July 18, 2015. 17. The Joint Commission. (n.d.). Ambulatory Care Program: The Who, What, When, and Where’s of Credentialing and Privileging. http://www.jointcommission.org/ assets/1/6/AHC_who_what_when_and_where_credentialing_booklet.pdf. Accessed July 18, 2015. 18. Nasca TJ, Philibert I, Brigham TP, Flynn TC. The next GME accreditation system: rationale and benefits. N Engl J Med. 2012;366(11):1051-1056. http:// dx.doi.org/10.1056/NEJMsr1200117. 19. Nasca TJ, Weiss KB, Bagian JP, Brigham TP. The accreditation system after the “Next Accreditation System”. Acad Med. 2014;89(1):27-29. http://dx.doi .org/10.1097/ACM.0000000000000068. 20. American Academy of Physician Assistants. Professional competence. Alexandria, Virginia. 2010. https://www.aapa.org/workarea/downloadasset. aspx?id¼810. Accessed July 16, 2015. 21. American Academy of Physician Assistants. Competencies for the physician assistant profession. Alexandria, Virginia. 2013. https://www.aapa.org/ WorkArea/DownloadAsset.aspx?id¼3104. Accessed July 16, 2015. 22. American College of Nurse Midwives. Core competencies for basic midwifery practice. Washington DC. 2012. http://www.midwife.org/ACNM/files/ ccLibraryFiles/Filename/000000002730/Core%20Competencies%20June %202012.pdf. Accessed July 17, 2015. 23. American College of Nurse-Midwives. Continuing competency assessment. Silver Spring, MD. [n.d]. http://www.midwife.org/Continuing-CompetencyAssessment. Accessed July 17, 2015. 24. American Midwifery Certification Board. Certificate maintenance program. Linthicum, MD. 2013. http://www.amcbmidwife.org/certificate-maintenance -program/objectives. Accessed July 17, 2015. 25. National Board of Certification & Recertification for Nurse Anesthetists. Background and history of the CPC program. Chicago, IL. 2015. http://www. nbcrna.com/cpc/Pages/Background-and-History.aspx. Accessed July 17, 2015. 26. Melnyk BM, Gallagher-Ford L, Long LE, Fineout-Overholt E. The establishment of evidenced-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and cost. Worldviews Evid Based Nur. 2014;11(1):5-15. 27. APRN Clinical Task Force. Current state of APRN clinical education [White Paper]. 2013. http://www.aacn.nche.edu/APRN-White-Paper.pdf. Accessed July 12, 2015. 28. Summers, L. Interprofessional task force tackles barriers to clinical training. Am Nurse. 2015. http://www.theamericannurse.org/index.php/2015/03/01/ interprofessional-task-force-tackles-barriers-to-clinical-training/. Accessed July 12, 2015. 29. APRN Consensus Work Group, & National Council of State Boards of Nursing APRN Advisory Committee. Consensus model for APRN regulation: licensure, accreditation, certification & education. 2008. http://www.aacn.nche.edu/ education-resources/APRNReport.pdf. Accessed July 17, 2015. 30. Kleinpell RM, Hudspeth R, Scordo KA, Magdic K. Defining NP scope of practice and associated regulations: Focus on acute care. J Am Acad Nurse Pract. 2012;24(1):11-18. 1555-4155/15/$ see front matter © 2016 Elsevier, Inc. All rights reserved. http://dx.doi.org/10.1016/j.nurpra.2015.08.037 Volume 12, Issue 2, February 2016