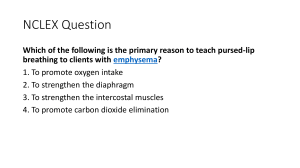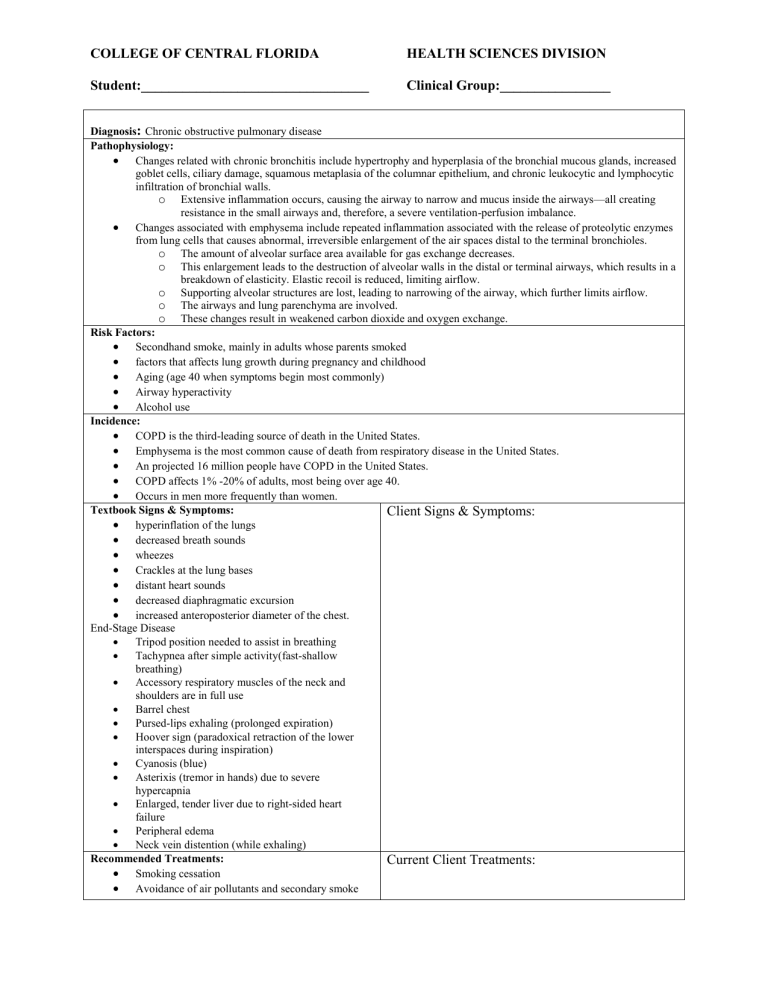
COLLEGE OF CENTRAL FLORIDA HEALTH SCIENCES DIVISION Student:_________________________________ Clinical Group:________________ Diagnosis: Chronic obstructive pulmonary disease Pathophysiology: Changes related with chronic bronchitis include hypertrophy and hyperplasia of the bronchial mucous glands, increased goblet cells, ciliary damage, squamous metaplasia of the columnar epithelium, and chronic leukocytic and lymphocytic infiltration of bronchial walls. o Extensive inflammation occurs, causing the airway to narrow and mucus inside the airways—all creating resistance in the small airways and, therefore, a severe ventilation-perfusion imbalance. Changes associated with emphysema include repeated inflammation associated with the release of proteolytic enzymes from lung cells that causes abnormal, irreversible enlargement of the air spaces distal to the terminal bronchioles. o The amount of alveolar surface area available for gas exchange decreases. o This enlargement leads to the destruction of alveolar walls in the distal or terminal airways, which results in a breakdown of elasticity. Elastic recoil is reduced, limiting airflow. o Supporting alveolar structures are lost, leading to narrowing of the airway, which further limits airflow. o The airways and lung parenchyma are involved. o These changes result in weakened carbon dioxide and oxygen exchange. Risk Factors: Secondhand smoke, mainly in adults whose parents smoked factors that affects lung growth during pregnancy and childhood Aging (age 40 when symptoms begin most commonly) Airway hyperactivity Alcohol use Incidence: COPD is the third-leading source of death in the United States. Emphysema is the most common cause of death from respiratory disease in the United States. An projected 16 million people have COPD in the United States. COPD affects 1% -20% of adults, most being over age 40. Occurs in men more frequently than women. Textbook Signs & Symptoms: Client Signs & Symptoms: hyperinflation of the lungs decreased breath sounds wheezes Crackles at the lung bases distant heart sounds decreased diaphragmatic excursion increased anteroposterior diameter of the chest. End-Stage Disease Tripod position needed to assist in breathing Tachypnea after simple activity(fast-shallow breathing) Accessory respiratory muscles of the neck and shoulders are in full use Barrel chest Pursed-lips exhaling (prolonged expiration) Hoover sign (paradoxical retraction of the lower interspaces during inspiration) Cyanosis (blue) Asterixis (tremor in hands) due to severe hypercapnia Enlarged, tender liver due to right-sided heart failure Peripheral edema Neck vein distention (while exhaling) Recommended Treatments: Current Client Treatments: Smoking cessation Avoidance of air pollutants and secondary smoke COLLEGE OF CENTRAL FLORIDA HEALTH SCIENCES DIVISION Student:_________________________________ Clinical Group:________________ Chest physiotherapy Ultrasonic or mechanical nebulizer treatments Venous thromboembolism (VTE) prophylaxis if hospitalized Adequate fluid intake High-calorie, protein-rich diet As tolerated with frequent rest periods Outpatient pulmonary rehabilitation a consideration for patients with moderate COPD Influenza vaccine yearly; pneumococcal vaccine at diagnosis and again in 5 years if first vaccine at < age 65 Pneumococcal conjugate vaccine Long-term oxygen therapy for patients with an SaO2 saturation of 88% at rest or less or arterial oxygen partial pressure (SpO2) of 55 mm Hg or less For patients with coexisting pulmonary hypertension, heart failure , or polycythemia (increased red cell mass) Extended oxygen therapy with a resting SaO2 of 88% to 93% or less or an SpO2 of 55 mm Hg to 60 mm Hg or less Lung transplantation for choice patients with very severe COPD (1-year survival rate is approximately 85%, while 5-year survival rate exceeds 50%) Teaching: disorder, diagnostic testing, cause, and treatment, including respiratory care measures and medications prescribed medications, including dosages, routes, schedules of administration, expected results, and possible adverse reactions (such as restlessness and tremors with short-acting bronchodilators) signs and symptoms of continual problems or problems and when to call the provider signs and symptoms of infection respiratory hygiene measures, including proper disposal of secretions infection control practices, including the need for hand washing energy-conservation measures and clustering of activities with frequent rest periods oxygen therapy at home, if mandatory, with safety actions in the home appropriate technique for inhaler use chest physiotherapy including postural drainage and percussion technique Coughing and diaphragmatic breathing exercises; pursed-lip breathing avoidance of air pollutants and people with known upper-respiratory tract infections immunizations, such as annual influenza and pneumococcal vaccines importance of a balanced, high-protein diet with adequate fluid intake to maintain nutrition and hydration possible irritants and ways to avoid exposure to them methods to prevent bronchospasm. Reference: Chronic obstructive pulmonary disease. Revised: July 12, 2019. In Lippincott advisor for education. Retrieved from https://advisor-edu.lww.com/lna/document.do?bid=4&did=791316&searchTerm=COPD&hits=copd