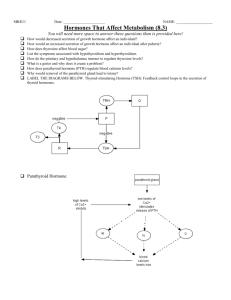
Endocrine System Endocrine System vs Nervous System Endocrine vs Exocrine Endocrine Release their secretions into the blood stream. The blood that carries the substances throughout the body until it reaches the target organ. - These secretions are useless and will have no effect on organs/tissues that don’t posses’ specific receptors for the secretions. Ductless Ex: Hypothalamus, Pituitary, Thyroid Exocrine - Glands that directly release their secretion into the target organ/tissue (is the one that will react to the secretion of the gland). Duct Ex: Sweat glands, Sebaceous glands Function of Endocrine System - - - - - - Metabolism and tissue maturation – regulate the rate of nutrient utilization and energy production and influences the development of tissue such as the nervous system Ion Regulation – helps regulate blood pH, as well as Na+, K+, and Ca2+ concentrations of the blood Water Balance – regulates water balance by controlling the solute concentrations in the blood Immune System Regulation – control the production of immune cells Heart rate and blood pressure regulation – to help the body for physical activity Control of blood glucose and other nutrients - regulates the levels of glucose and other nutrients in the blood Control of reproductive functions – control the development and functions of the reproductive system in male and females Uterine contractions and milk release – regulate uterine contractions during delivery and stimulates milk release from the breasts in lactating females © Jolo Tiongson and JC Elduayan BSPT2-2 Endocrine System Exerts control via circulation Chemical messengers are hormones – travel in the bloodstream Nervous System Exerts control via nerve impulses - Chemical messengers are neurotransmitters – has electrical impulses travelling along the nerve. - Often confine to one area of the body w/c makes the response localize Affects all cells – Affects the neurons, produce widespread muscles and gland. response usually noticed in many organs Onset takes hours or Onset takes days milliseconds Duration of effects are Duration of effects are longer brief Ex: Growth and Ex: Movement of the Development of limbs, Blinking Reproductive System How do you think the Endocrine Glands get their jobs done? - Hormones. Since hormones are carried in the blood, they reach all cells. However, a hormone causes an effect only on certain cells and not on others. The affected cells are called the ‘target cells’ and each hormone has its own specific target cell. When a hormone reaches a target cell, it binds the specific receptors, meaning no receptor = no effect and the number of receptors for each target cell may vary Cells can increase and decrease their sensitivity to hormone by regulating the number of their receptors Receptors are proteins and are manufactured by the cell itself, thus a cell can increase or decrease the number of receptors w/in its plasma membrane How do cells regulate the number of receptors? Up-Regulation – the number of receptors may increase when the amount of hormone is low. This causes the target tissue to become more sensitive to the hormone Down-Regulation – the number of receptors may decrease when the amount of hormone is high. This causes the target tissue to become less sensitive to the hormone Types of Hormones Based on Target Tissues 1. Circulating Hormone – Hormones carried by the blood to act on cells located some distance from the secreted cells. Their effects generally last from minutes to hours and are eventually inactivated by the liver and excreted by the kidney. For example, if the effects should be longer then the hormone must be steadily secreted. In some cases, when kidney or liver failed, excessive hormones may build-up in the blood © Jolo Tiongson and JC Elduayan BSPT2-2 2. Local Hormones – the cells that secrete them are quickly inactivated - Paracrines – Acts on cells located near the secreting cell. It acts on its neighbor cell - Autocrines – It act on the same cell that secrete them. Chemical Classes of Hormones 1. Steroid - Derived from cholesterol which belong to a chemical compound known as steroids - Ex: Sex hormone, adrenal cortex hormones 2. Amine - Hormones derived from the modification of amino acids referred to as amine hormones. Typically, the original structure of the amino acid is modified such that a COOH (carboxyl) group is removed whereas the NH3+ (amine) group remains. Amine hormones are synthesized from the amino acids tryptophan or tyrosine - Ex: An example of a hormone derived from tryptophan is melatonin, while tyrosine derivatives include thyroid hormones and catecholamines 3. Peptide - These hormones are made up of only few amino acid residues and they are usually present themselves in form of a linear chains - Ex: Oxytocin and Vasopressin 4. Protein - These hormones build up from large number of amino acid residues - Ex: Insulin, glucagon, somatotropin 5. Glycoprotein - These are conjugated protein bound to carbohydrates which include galactose, mannose, fructose - Ex: Luteinizing hormones, follicle stimulating hormones, thyroid stimulating hormones 6. Eicosanoid - Made up of small fatty acid derivatives with a variety of arachidonic acid - Ex: Prostaglandins Stimulation of Hormone Release Control of Humoral Stimuli - - This control or the release of hormone is being stimulated by the metabolites and molecules in the bloodstream. The cells that secretes the hormones have receptors for certain substances in the blood. Ex: In the bloodstream, there is low Ca2+ level. This low Ca2+ level/blood Ca2+ level will stimulate the endocrine cell to produce parathyroid hormone. This parathyroid hormone will have an effect on its target organ to increase the activity of osteoclast. Once the activity of osteoclast is increased, it will promote bone resorption and in effect, it will increase the blood Ca2+ level Control by Hormonal Stimuli © Jolo Tiongson and JC Elduayan BSPT2-2 - This occurs when the hormones stimulate the secretion of other hormones Ex: Hormones of the anterior pituitary gland/trophic hormones. o Step 1: The neurons in the hypothalamus release stimulatory hormones or the releasing hormones that will travel in the blood going to the anterior pituitary gland o Step 2: The releasing hormone will stimulate the trophic hormones of the anterior pituitary and then it will travel in the blood going to the target endocrine cell. o Step 3: The target endocrine cell then secretes its hormones into the blood where it travels to its target and produces a response o Step 4: The hormone from the target endocrine cell inhibits the hypothalamus and anterior pituitary from secreting the releasing hormone and the trophic hormone. This is what we call ‘negative feedback’ o Step 5: In some instances, the hypothalamus can also secrete inhibiting hormones w/c prevent the secretion of anterior pituitary/trophic hormones Control of Neural Stimuli Inhibition of Hormone Release 1. Inhibition of Humoral Stimuli – Often when a hormone is released, it is triggered by a particular humoral stimulus, there exist a companion hormone whose release is inhibited by the same humoral stimulus. - Companion Hormone - usually opposed the effect of the secreted hormone and counteract the secreted hormones action. - Ex: The adrenal cortex releases aldosterone in response to low blood pressure. However, if blood pressure goes up due to the elevated sodium levels brought about by aldosterone, the atria will secrete a hormone (atrial natriuretic peptide) which will lower the blood pressure to normal values. The ANP will be the companion hormone to oppose the effect of the secreted hormone 2. Inhibition of Hormonal Stimuli - Some hormones prevent the secretion of other hormones - Ex: When the anterior pituitary release the thyroid stimulating hormone to stimulate the thyroid gland to produce its hormone when the blood concentration for the hormones increases, that increase in hormones will inhibit the hormone release of the anterior pituitary and hypothalamus via the negative feedback 3. Inhibition of Hormone release by Neural Stimuli - Release of inhibitory neuron transmitter which will prevent the action of the endocrine gland - When an action potential in the neuron stimulates secretion of inhibitory neuron transmitter, the endocrine cell is inhibited and will not secretes its hormones © Jolo Tiongson and JC Elduayan BSPT2-2 Control of Hormone Level in Bloodstream A. Negative Feedback by Hormones Step 1: The anterior pituitary gland secretes a trophic hormone which travels in the blood to the target endocrine cell Step 2: The hormone from the target endocrine cell will travel to its target organ Step 3: At the same time, the hormone from the target endocrine cell will also have a negative feedback effect going back to the anterior pituitary and hypothalamus that will result to decrease secretion of the trophic hormone To further discuss, watch this video: https://www.youtube.com/watch?v=Vae5CcaPN_8&a b_channel=CarpeNoctum B. Positive Feedback by Hormones Hypothalamic Control of the Endocrine System - - - - Hypothalamic Hormones stimulates the pituitary to release stimulating hormones such as the ACTH, TSH, LH, and FSH At the same time, effector hormones such as GH and Prolactin are released or inhibited affecting the adrenal cortex, the thyroid and the gonads. Endocrine pathology develops as a result of this function of releasing trophic or effector hormones or when the effect occurs in the target tissue SUMMARY: The hypothalamus has a control for the anterior and posterior pituitary gland via neural stimulation and hormonal control. It will have an excitatory and inhibitory responses Feedback Mechanisms - Simple Negative Feedback - - - - The endocrine system meets the nervous system at the hypothalamic pituitary interface The hypothalamus, the main integrative center for the Endocrine and Autonomic Nervous system controls the function of the endocrine organs by neural and hormonal pathways Neural pathways connect the hypothalamus to the posterior pituitary providing the hypothalamus direct control over both the anterior and posterior portions of the pituitary gland Neural stimulation of the posterior pituitary provokes secretion of the two effector hormones, the ADH and the oxytocin The hypothalamus also exerts hormonal control at the anterior pituitary through releasing inhibiting factors, so both excitatory and inhibiting factors. © Jolo Tiongson and JC Elduayan BSPT2-2 - Complex Negative Feedback - - - Step 1: Stress would result to hypothalamus releasing CRH Step 2: The CRH will release or stimulate the anterior pituitary to release the ACTH Step 3: The ACTH will stimulate the adrenal gland to secrete/release adrenal cortisol Step 4: Once the adrenal cortisol increases in the blood or there is an increase serum cortisol, it will inhibit the ACTH by decreasing the CRH secretion Aka Hypophysis Cerebri Referred to as “Master Endocrine Gland” It is located inferior to the hypothalamus and is connected to it by a stock of tissue called the infundibulum Divided into two functional parts: o What are the different endocrine glands of the body? Pituitary Gland o Anterior (Adenohypophysis) – is divided into three parts: ▪ Pars Tuberalis ▪ Pars Intermedia ▪ Pars Distalis *The hormones secreted by the anterior pituitary are not neurohormones because it is derived from the epithelial tissue of the embryonic oral cavity and not from the neural tissue Posterior (Neurohypophysis) – it is continuous of the brain. Secretions are considered neurohormones Secretions from the Anterior Pituitary Gland 1. Growth Hormone (GH) © Jolo Tiongson and JC Elduayan BSPT2-2 - Target: stimulates growth in most tissues Increased: o Growth in tissues o Amino acids uptake and protein synthesis o Breakdown of lipids o Glycogen synthesis and blood glucose level *GH is somatotropin. It plays a major role in regulating growth in determining how tall a person becomes and it also regulate metabolism. It also regulates blood nutrient level after a meal and during periods of fasting - - Target: Adrenal Cortex, Stimulated Development and Secretion in Adrenal Cortex ACTH increases the secretion of hormones primarily the cortisol of the adrenal cortex and this ACTH + Melanocyte Stimulating Hormone (MSH) binds to the melanocytes and increase the skin pigmentation 3. Thyroid-Stimulating Hormone (TSH) *The direct effect of growth hormone includes breakdown of lipids, and decrease use of glucose as an energy source. *It also has an indirect effect on some tissues. For example, it can increase the production of polypeptide or the somatomedins that circulate in the blood and bind to the receptors of the target tissue. That somatomedins stimulate the growth in cartilage and bones and increase the synthesis of proteins in skeletal muscles primarily by the liver and also skeletal muscles and other tissues. *Usually when there is stress, it increases the GHRH and inhibits the GHIH secretion. Target: Thyroid Gland, Stimulated development and secretion in thyroid gland It stimulates the synthesis and secretion of the thyroid hormones from the thyroid gland The secretion is controlled by the TRH (Thyroid Releasing Hormone) from the hypothalamus and thyroid hormones from the thyroid glands. In contrast, thyroid hormones are being inhibited by the TRH and TSH secretions *Via negative feedback: When there is high level of GH, it will have a negative feedback effect on the production of GHRH by the hypothalamus. Gonadotropin – are hormones capable of promoting growth and function of the gonad’s w/c includes the ovaries and testis *This secretion of the growth hormone is controlled by two neurohormones—the Growth Hormone Releasing Hormones (GHRH) and the Growth Hormone Inhibiting Hormone (GHIH). 2. Adrenocorticotropin (ACTH) - - - © Jolo Tiongson and JC Elduayan BSPT2-2 The 2 major gonadotropins secreted from the anterior pituitary are the LH and FSH The LH, FSH and Prolactin (also secreted by the APH) play important role in regulating reproduction LH and FSH are released from anterior pituitary cells under the influence of the hypothalamic releasing hormone and/or gonadotropin releasing hormone 4. Follicle-Stimulating Hormone (FSH) - Target: F: Ovaries M: Testes - Function: F: Ovulation and progesterone production M: Testosterone synthesis and support for sperm cell production 6. Prolactin (PRL) - - Target: F: Follicles in ovaries M: Seminiferous tubules - - Function: F: Development of ovarian follicle, Estrogen secretion M: Development of testis, Sperm production - 5. Luteinizing Hormone (LH) It increases the number of receptor molecules for FSH and LH in the ovaries via the UpRegulation and it is therefore having a permissive effect for FSH and LH on the ovary Target: F: Ovaries and mammary glands Function: Milk production, increased response to LH and FSH. THERE IS NO PRL HORMONES FOR MALES The sucking motion of the baby stimulates prolactin secretion 7. Melanocyte Stimulating Hormone (MSH) - ACTH + MSH binds to the melanocytes and increase the skin pigmentation - Target: Melanocytes - Function: Increase melanin production Secretions from the Posterior Pituitary Gland 1. Antidiuretic Hormone (ADH) - It prevents the output of the large amounts of urine - Also called as the vasopressin, because it constricts the blood vessels and raises the © Jolo Tiongson and JC Elduayan BSPT2-2 blood pressure when large amounts are released. - - - It also causes contraction of the uterus for non-pregnant primarily during menstrual period and sexual intercourse Also responsible for milk ejection in lactating females by promoting contraction of smooth muscles surrounding the alveoli of the mammary glands NO EVIDENCE of existing oxytocin for the MALES Target: Uterus and mammary gland Function: Stimulates the uterine contraction. It also stimulates the mammary glands to eject milk Secretions from the Islets of Langerhans - - - - Target: Kidneys Function: Stimulates the reabsorption of water by the renal tubules The secretion rate for ADH changes in response to alterations in blood osmolality and blood volume. ADH plays a major role in these changes in urine formation. The osmolality of a solution increases as the concentration of solute in the solution increases. When blood osmolality increases, the frequency of action potentials in the osmoreceptors increases that would result to a greater frequency of action potential in the neurosecretory cells and as a consequence, the ADH secretion increases As for the blood pressure, when the blood pressure increases, the action potential for neurosecretory cells decreases thus resulting to less ADH secretion To simplify: ↑ Blood Osmolality = ↑ ADH secretion while ↑ Blood Pressure = ↓ ADH secretion 2. Oxytocin - Stimulates smooth muscles of the uterus - This hormone plays an important role in the expulsion of the fetus from the uterus during delivery by stimulating uterine smooth muscle contraction © Jolo Tiongson and JC Elduayan BSPT2-2 - The pancreas lies behind the peritoneum between the greater curvature of the stomach and the duodenum. It is considered as both exocrine gland and endocrine gland. Exocrine portion is composed of acini w/c produce pancreatic juice and a duct system w/c carries the pancreatic juice to the small intestine o Endocrine portion consist of pancreatic islet or the Islets of Langerhans w/c produce hormones that enter the circulatory system Each Islet is composed of alpha cells w/c secrete glucagon and beta cells w/c secrete insulin The islets of Langerhans are small clusters of cells located in the pancreas. The pancreatic hormones play an important role in regulating the concentration of critical nutrients in the circulatory system o - - 1. Insulin - Target: liver, skeletal mm and adipose tissue, satiety center (collection of neurons in the hypothalamus that controls the appetite). - Function: Increased uptake and used of glucose and amino acids - In general, the target tissues response to insulin is an increase in its ability to take up and use glucose and amino acids. The normal regulation of blood glucose level requires insulin - Blood glucose level can increase dramatically when too little insulin is secreted or when insulin receptors do not respond © Jolo Tiongson and JC Elduayan BSPT2-2 2. Glucagon - Target: Liver - Function: Increased breakdown of glycogen; release of glucose into the blood. - It primarily influences the liver although it has some effect on the skeletal muscle and adipose tissue - In general, the glucagon causes the breakdown of glycogen and increase glucose synthesis in the liver. It also increases the breakdown of fats *These two hormones have somatostatin, a growth hormone and inhibiting hormone, that is responsible for inhibiting insulin and glucagon secretion. Pineal Gland - - - - Is at the epithalamus of the brain that secretes hormones acting on the hypothalamus or the gonads to inhibit reproductive function Photoperiod - the amount of daylight and darkness that occurs each day in changes with the seasons of the year. When there is an increase in daylight, it will initiate action potential in the retina of the eye and then propagate it to the brain and cause a decrease in action potential that will result to decrease secretion by the pineal body. In the dark, action potential delivered to the body increases, thereby stimulating the secretion of pineal hormones In short, there is a large secretion of melatonin at night compared to daylight Thyroid Gland Secretions from the Pineal Gland 1. Melatonin - Target: hypothalamus - Function: Inhibits secretion of gonadotropinreleasing hormone thereby inhibiting reproduction Induce sleep - Can decrease gonadotropin-releasing hormone secretion from the hypothalamus and they inhibit reproductive functions through this mechanism - It also regulates the sleep cycle by increasing the tendency to sleep © Jolo Tiongson and JC Elduayan BSPT2-2 - Composed of two lobes connected by a narrow band of thyroid tissue called the isthmus. The lobes are lateral to the upper - portion of the trachea just inferior to the larynx and the isthmus extends across the anterior aspect of the trachea. The thyroid gland is one of the largest endocrine glands. It is highly vascular and it appears more red than its surrounding tissues - - Secretions of the thyroid gland - - - 1. Calcitonin - Target: Bone - Function: Increase calcium storage in bone - The major stimulus for increase calcitonin secretion is increase in calcium levels in the body fluids - The primary target tissue of calcitonin is the bone. - The calcitonin binds to the membrane-bound receptor then decreases the osteoclast activity and lengthens the life of the osteoblast. The result is the decrease in blood calcium and phosphate levels causing increase in bone deposition - The blood levels of calcitonin decreases with age to a greater extent of female than males. That is why osteoporosis increases with age and occurs to a greater degree in females than males because of a decrease in calcitonin level 2. Thyroxine (T4) and Triodothyronine (T3) - Target: most cells - Function: essential to BMR (basal metabolic rate) – the rate at w/c a person’s body burns calories while at rest; influences physical/mental development and growth © Jolo Tiongson and JC Elduayan BSPT2-2 The TSH from the anterior pituitary must be present to maintain the thyroid hormone synthesis and secretion. The normal rate of metabolism of an individual depends on the adequate supply of thyroid hormone which increases the rate at which glucose, fat and protein are metabolized The thyroid hormone also increases the activity of sodium-potassium exchange pump which contributes to an increase in body temperature The TRH from the hypothalamus and TSH from the anterior pituitary function together to increase T3 and T4 secretion from the thyroid gland Exposure to cold and stress cause increase TRH secretion and prolong fasting decreases TRH secretion thereby decreasing the T3 and T4 secretion Control of the Thyroid Hormone Secretion of the parathyroid gland 1. Parathyroid Hormone - - - - An increase temperature, the thyrotroponin releasing hormone, is secreted by the hypothalamus and stimulates the secretion of the TSH. Then the TSH will increase both the synthesis and secretion of thyroid hormones by the follicular cells Chronic TSH elevation can cause hypertrophy of the thyroid The thyroxine regulates the TRH receptors in the anterior pituitary thereby inhibits TSH receptors The thyroid hormones have a negative feedback effect on the hypothalamus and anterior pituitary gland. As the level of T3 and T4 increases, it will inhibit TRH and TSH secretion. Also, if the thyroid gland is removed or the T3 and T4 secretion declines, TSH secretion levels in the blood increase dramatically, thus resulting to abnormality. Parathyroid Gland - Are usually embedded on the posterior part of each lobe of the thyroid gland Usually, parathyroid glands are present with their cells organized in densely packed masses rather than in follicle © Jolo Tiongson and JC Elduayan BSPT2-2 - - - - - Important in the regulation of body fluids Target: bone, kidney, small intestine Function: Increase calcium removal from storage in bone, Produces active form of vitamin D in kidneys, Increase absorption of calcium by intestines, increase blood calcium level The PTH stimulates osteoclast activity in bone and can cause of number of osteoclast to increase Increase in osteoclast activity results in bone resorption and the release of calcium and phosphate causing the increase in blood calcium levels The PTH also induces calcium reabsorption within the kidneys so that less calcium leaves the body in urine It also increases the enzymatic formation of active Vitamin D in the kidney. As the PTH increases, the rate of active Vitamin D synthesis, it will result to increase rate in calcium and phosphate absorption in the intestine thereby elevating the blood levels of the calcium - - In this picture if there is a decrease in calcium level or decreased blood calcium level it will stimulate increase in the PTH secretion of the parathyroid hormone. Parathyroid hormone will promote calcium and phosphate resorption from bone. It also promotes calcium reabsorption and phosphate excretion from the renal tubule. - Also promotes calcium absorption from the GI tract. - This will result to increase serum calcium level and once the calcium level in the blood increases that will result to PTH secretion inhibition. - - - - © Jolo Tiongson and JC Elduayan BSPT2-2 In this picture is the one two five dihydrocoxy calciferol this is the active form of vitamin. The effect of the vitamin d of that active form of vitamin d is influenced by the parathyroid hormone. If the serum calcium levels are too high the release of the PTH or the parathyroid hormone will be suppressed. The result of that suppression or inhibition of the parathyroid hormone, the one two five dihydrocoxycolia calciferol the active form of vitamin d. will also decrease. And once that active form of vitamin D decreases it will also decrease the absorption of calcium from the intestines, bones and vinyl tubules thus causing calcium level to decrease. If the calcium level the blood calcium level increases it will suppress or inhibit the secretion of parathyroid hormone Since the parathyroid hormone influence the formation of the one two five dihydrocoxycolicalciferol the active form of vitamin D, once the formation of the active form of vitamin D decreases, it will affect or it will decrease the absorption of calcium from the intestine, bones and renal tubules thus resulting to decrease calcium level in the blood and that will result to homeostasis. - 2. Developmental • glucocorticoids or the cortisol are required for the maturation of tissues like fetal lungs and for the development of receptor molecules in target tissues for epinephrine and norepinephrine Adrenal glands - - - also called the supra renal glands. Located near the superior poles of the kidneys Like the kidneys, the adrenal glands are retroperitoneal and they are surrounded by the adipose tissue. Adrenal glands are enclosed by a connective tissue capsule and have a well-developed blood supply. It has a the inner medulla and the outer core. - - - The adrenal cortex secretes 3 hormone types: glucocorticoids, mineralocorticoids and androgen. Zono fasciculata of the adrenal cortex primarily secretes glucocorticoid hormones. © Jolo Tiongson and JC Elduayan BSPT2-2 Cortisol is the major or main glucocorticoid hormone. The responses of this hormone are classified as: 1. Metabolic • As the metabolic it increases, the fat and protein metabolism, blood glucose level and glycogen deposits in cells. 3. Anti-inflammatory • it decreased the intensity of the inflammatory response by decreasing both the number of WBC and secretion of inflammatory chemicals from the tissues The major secretory products of the zona Glomerulosa are the mineralocorticoids. 1. Aldosterone is the mineralocorticoids produced in the greatest amount. • increases the rate of sodium reabsorption by the kidneys thereby increasing blood levels of sodium. It also increases potassium excretion into the urine by the kidney thereby decreasing blood levels of potassium. It also increases the rate of hydrogen excretion into the urine. • In short aldosterone increases sodium in the blood and decrease blood level of potassium. 2. Androgen are secreted by the sauna reticularis and stimulates the pubic and axillary hair growth and sexual drive in females. Effect in males are very negligible in comparison to the effect of testosterone two males which is secreted by the testis. - Arginal medulla secretes two major hormones: 1. Epinephrine • accounts for 80 % • increase the blood glucose level the use of glucose and glycogen by the skeletal muscles. • It also increases the heart rate and the force of contraction. • It also caused vasoconstriction on the skin and viscera vasoconstriction and vasodilation on skeletal and cardiac muscle. 2. Norepinephrine • 20% of the adrenal medulla hormones • stimulates the cardiac muscle and caused constriction of the most of the peripheral blood vessels. - The target tissues are the heart, blood vessels liver and adipose tissues. Adrenal medulla hormones - Prepare the body for physical activity - A major component for the fight and flight response - The release of this hormones is mediated by the sympathetic nervous system in response to emotions, injury, stress, exercise and even low blood glucose levels. © Jolo Tiongson and JC Elduayan BSPT2-2 - Main endocrine gland of the female reproductive system are the ovaries. Function: depend on the secretion of the FSH and the LH follicle stimulating hormone and the luteinizing hormone from the anterior pituitary gland. Secretion of ovaries 1. Inhibin • which inhibits the follicle stimulating hormone secretion. 2. Estrogen and Progesterone • Control the female reproductive cycle • Prepare the mammary glands for lactation and maintain pregnancy • Also responsible for the development of the female reproductive organs and the female secondary sex characteristics. - During pregnancy the ovaries and the placenta secrete estrogen and progesterone which are essential to maintain pregnancy 3. Relaxin • which increases the flexibility of the connective tissue of the female symphesis pubis. Which helps dilate the cervix of the uterus. this will aid or facilitate the delivery of the mother. Thymus gland - it is in the neck and does appear and superior to the heart in the thorax. Secretions of the thymus 1. Thymosin • plays an important role in the development and function of the immune system. Pathology of the Endocrine System - Main endocrine gland of the male reproductive system is the testes. Function: depends on the secretion of the FSH and LH from the anterior pituitary same with the the female endocrine gland. Secretion of testes 1. Testosterone • regulates the production of the sperm cells by the testis and the development and maintenance of the male reproductive organs and secondary sex characteristics. 2. Inhibin • inhibits the secretion of the follicle stimulating hormone from the anterior pituitary. © Jolo Tiongson and JC Elduayan BSPT2-2 Hyperfunction - Results from overproduction of hormones or overstimulation of the pituitary gland. Hypofunction - Results from underproduction of hormones or understimulation of the pituitary gland. Hyporesponsiveness - Occurs when the target tissue has hormonal resistance - Hormone levels are normal but the main problem is the target tissue. Conditions 1. Diabetes Insipidus - involves a physiologic imbalance of water following deficiency or inaction of the antidiuretic hormone (ADH). - - - - Function of ADH? Antidiuretic hormone regulates water by increasing the permeability of the tubules of the kidney. Major function of your ADH is to promote water resorption by the kidney and to control the osmotic pressure of the extracellular fluid. If there will be injury or loss of function of the hypothalamus or the posterior pituitary gland it can result to diabetes incipidus. When the ADH production decreases, the kidney tubules will fail to reabsorb water End result is excretion of large amount of dilute urine. What are the possible effects of diabetes insipidus to the body? • Kidney tubules fail to rebsorb water • Urine is diluted • Dehydration (Excessive water loss) CLINICAL MANIFESTATION • Polydipsia (excessive thirst) • Noctoria (excessive urination at night) • Dehydration • Poor tissue turgor • Dry mucous membrane • Constipation • Muscle weakness • Dizziness • Hypotension Secondary effect • fatigue and irritability • secondary to sleep disruption associated with nocturia 2. Syndrome of Inappropriate ADH Secretion (SIADH) - Involves a physiologic imbalance of water following excessive release of the antidiuretic hormone (ADH). - Opposite of diabetes insipidus - Possible effects of SIADH to the body • Kidney tubules excessively reabsorb water • Urine is concentrated • Excessive water retention - Other symptoms • Edema is rare © Jolo Tiongson and JC Elduayan BSPT2-2 • • • • • Neurologic and neuromuscular sign and symptoms Predominate and are directly related to the swelling of brain tissue Sodium changes within neuromuscular tissues CNS dysfunction characterized by alterations in level of consciousness seizures and coma. Coma can occur when serum sodium falls. Hyponatremia - there is a low sodium concentration in the blood. This can result in diminished GI function. 3. Hyperthyroidism - Excessive secretion of the thyroid hormone. - Referred to as tyrotoxicosis a term used to describe the clinical manifestations that occur when the body tissues are stimulated by increased thyroid hormone. - Excessive thyroid hormone creates a generalized elevation of body metabolism the effects of which are manifested in almost every system. - Function of the thyroid hormones (T3 and T4): • Promote bone formation and maturation • Consumption of O2 and BMR are increased • Increased cardiac output • Hyperexcitability of the CNS • General catabolic effect - Changes in the body in patients with hyperthyroidism? • ↑ metabolic rate • Weight loss • ↑ heat production (sweating) • ↑ Cardiac output • Nervousness • Goiter (have mild symmetric enlargement of the thyroid) • diarrhea • tremor • palpitations • atrial fibrillation • precipitate congestive heart failure • increase the risk of underlying CAD or for myocardial infarction 4. Hypothyroidism - Insufficient secretion of the thyroid hormone. - More common compared to hyperthyroidism - Creates a generalized depression of body metabolism - Thyroid hormones play such an important role in body's metabolism lack of this hormones seriously upsets the balance of body processes. - Primary symptoms: • intolerance to cold • excessive fatigue and drowsiness • headaches • and weight gain so in women • menstrual bleeding may become irregular • can worsen the pre-menstrual syndrome • dryness of the skin • increasing brittleness of the hair and nails • there may also be nodules (irregularities of the thyroid palpable during interior neck examination) • dry scaly skin - Changes in the body in patients with hypothyroidism: • ↓ metabolic rate • Weight gain • ↓ heat production (cold intolerance) • ↓ cardiac output • Mental slowness 5. Addison’s Disease - Insufficient secretion of the Adrenocortical hormones (Cortisol and aldosterone). - A disorder within the adrenal gland itself. - Decrease production of cortisol and aldosterone - Can result to widespread metabolic disturbances - Can also cause hypoglycemia - Delivered glycogen deficiency the person grows - Weak - exhausted - hypotensive © Jolo Tiongson and JC Elduayan BSPT2-2 - - - Anorexia weight loss Nausea Emotional disturbances (ranging from mild neurotic to severe depressions) Diminish patient's resistance to stress Poor coordination Fasting hypoglycemia AND craving for specifically salty food Axillary and pubic hair growth in females DECREASE libido amenorrhea (absence of menstruation) Changes in the body in patients with Addison’s disease: • Hypoglycemia • Weightloss • Hyperpigmentation Secondary adrenal insufficiency refers to a dysfunction of the gland because of the insufficient stimulation of the cortex due to lack of pituitary ACTH Causes of secondary disease includes tumor of the hypothalamus or pituitary removal of the pituitary or rapid withdrawal of corticosteroid drugs. **** TAKE NOTE: clinical manifestations of secondary disease do not occur until the adrenal glands are almost completely non-functional and are primarily related to the cortisol deficiency. **** whenever corticosteroids are administered externally the increase in serum cortisol level triggers a negative feedback effect anterior pituitary gland to stop adrenal stimulation ***** important that if the patient is in corticosteroid medication it must be reduced gradually so that normal adrenal function can return. 6. Diabetes Mellitus - Insufficient secretion or action of insulin. - Chronic system systemic disorder characterized by hyperglycemia (excess glucose in the blood) - Involves disruption of the metabolism of carbohydrates fats and proteins - Insulin produced in the pancreas normally maintains a balance of the blood glucose level - Characterized as a by a group of metabolic diseases resulting from defects in the secretion of insulin action of insulin or both the chronic hyperglycemia of diabetes mellitus is associated with long-term or prolonged damage and dysfunction. - Changes in the body in patients with DM: • Increase in blood glucose • 3Ps: *polyphagia - means excessive hunger and eating *polydeptia - excessive thirst *polyurea - excessive or frequent urination Type 1: Insulin dependent Type 2: non-insulin dependent or adult-onset diabetes 7. HYPERPARATHYROIDISM (HYPERCALCEMIA) Pathologic fractures - Bone decalcification/osteoporosis - Severe muscle weakness © Jolo Tiongson and JC Elduayan BSPT2-2 8. HYPOPARATHYROIDISM (HYPOCALCEMIA) - Muscle tetany and cramps - Carpopedal spasm - Cardiac arrythmias