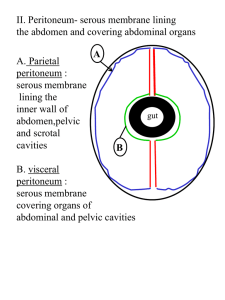
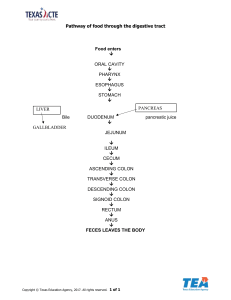
Peritoneum and Peritoneal Cavity 5.2.2 Abdominal cavity, peritoneum Peritoneum is a thin serous membrane, quite similar to pleura. It provides a continuous lining for the abdomino-pelvic cavity. The surfaces of the organs that lie within the abdominal cavity are also covered with a continuous layer of peritoneum. The visceral layer of peritoneum that covers the organs is continuous with the parietal layer that lines the cavity. The space between adjoining peritoneal surfaces is normally occupied by just a trace of serous fluid. Those organs that lie freely mobile within the abdominal cavity, like the small intestine here, are attached to the wall of the cavity by double sheets of peritoneum, in which their blood vessels run. 5.2.3 Stomach Along with the colon we'll remove this double sheet of peritoneum that goes from the stomach to the transverse colon, the gastro-colic ligament. Here's the inside of the stomach. Like all the parts of the gastro-intestinal tract, its wall is formed by an outer layer of smooth muscle, and an inner layer of mucosa. In the fundus the mucosal layer is smooth; in the pyloric antrum it's thrown into prominent longitudinal folds At the esophago-gastric junction the muscle coat of the esophagus forms a partly effective sphincter that keeps the contents of the stomach from passing upwards. At the pylorus the thickened muscular coat forms a highly effective sphincter that relaxes intermittently to let the contents of the stomach into the duodenum a little at a time. Here are the mucosal folds of the pylorus, protruding into the duodenum. 5.2.4 Greater and lesser omentum Two double-sided sheets of peritoneum, the greater omentum and the lesser omentum, extend from the greater curve and lesser curve of the stomach. The greater omentum is attached along the whole length of the greater curve, the lesser omentum is attached along the lesser curve: up here its attachment is quite wide. This is the lesser omentum. Parts of it are fatty, other parts are extremely thin. The lesser omentum goes from the lesser curve here, to the underside of the liver, where its attachment is just out of sight. It's attached up here to the underside of the diaphragm. The lesser omentum extends down here onto the duodenum, where it has a free lower border as we'll see. Behind the lesser omentum, which we'll divide along this line, we come into an extensive back-pocket of the peritoneal cavity, the omental bursa or lesser sac, that continues around behind the stomach. We'll see more of it later. The part of the greater omentum between the stomach and the transverse colon is called the gastro-colic ligament. 5.2.5 Omentum: development (animation) The foregut starts as a straight tube. As it develops, it rotates on its long axis, lengthens in a double curve, and expands to become the stomach, and the first part of the duodenum. The liver develops in the ventral mesogastrium, the spleen develops in the dorsal mesogastrium. The liver grows rapidly, pressing against the body wall, and obliterating these layers of peritoneum. These changes produce this almost separate pocket behind the stomach, the lesser sac. Here we're looking up into the upper part of the abdominal cavity This is the diaphragm. Here's the foregut, starting to develop, here's the liver developing in the ventral mesogastrium, and the spleen developing in the dorsal mesogastrium. 5.2.6 Duodenum The small intestine consists of the duodenum and the jejuno-ileum. The duodenum is the first part of the small intestine. It's also the hardest to see because there's so much in front of it. To see it we'll go to a dissection in which the lower ribs, which were here, have been removed. We've also removed the left lobe of the liver, the greater omentum, and the colon. The duodenum is partly hidden by the root of the mesentery, which is the peritoneal attachment of the jejuno-ileum. To see all of the duodenum, we'll remove the mesentery, and the jejuno-ileum. The duodenum starts at the pylorus by passing upwards and to the right, then turns to run in almost a full circle, ending here at its sharply angled junction with the jejunum, the duodeno-jejunal flexure. The discoloration up here is due to post-mortem staining from the nearby gall bladder. The duodenum is often described as having four parts, numbered one through four. The inner aspect of the curve of the duodenum is largely occupied by this structure, the head of the pancreas, which we'll see later. The pancreatic duct or ducts, which lie within the panreas, together with the common bile duct, join the second part of the duodenum, as we'll see. 5.2.7 Duodenum: development (animation: rotation of the midgut) Here's the aorta, here are the three arteries that supply the GI tract: the celiac for the foregut, the inferior mesenteric for the hindgut, and the superior mesenteric for the midgut. As the midgut develops it protrudes into the body stalk forming a loop, with the superior mesenteric artery forming the axis of the loop. 5.2.8 Attachments of the duodenum Before we leave the duodenum, we need to look at two special aspects of its peritoneal attachments: proximally, the distal part of the lesser omentum, and distally the suspensory ligament. We'll go back to this earlier stage of the dissection to see these. Here's the part of the lesser omentum that we've seen already. The lesser omentum continues along the upper surface of the first part of the duodenum, and comes to an end here. This is the free border of the lesser omentum, passing from the duodenum to the underside of the liver. Beneath the free border of the lesser omentum lies this hidden opening, the epiploic foramen, which is the only natural entry way to the omental bursa or lesser sac. Going to the distal end of the duodenum, this is the suspensory ligament, also known as the ligament of Trietz. It's a fold of peritoneum, reinforced with fibrous tissue, that holds up the duodeno-jejunal flexure 5.2.9 Jejuno-ileum the jejunum and the ileum. They're the sites of absorption of digested foodstuffs. Jejunum and ileum are names given to the proximal and distal parts of one continuous tube. There's no distinct boundary between them, and they're often spoken of together as the jejunoileum. The jejuno-ileum starts up here to the left of the mid-line. It runs downward and to the right, ending here. The jejuno-ileum lies within a space that's bounded by the ascending colon to the right, the descending colon to the left, and the transverse colon and its mesentery above. Since the attachment of the mesentery to the intestine is about thirty times longer than its attachment to the body wall, the mesentery is arranged like a richly folded fan. The mesentery carries the blood vessels of the jejunoileum, and its nerves and lymphatics. 5.2.10 Cecum and appendix the large intestine, where water and electrolytes are absorbed from the intestinal contents, the contents changing from liquid to semi-solid in the process. The large intestine consists of the cecum and appendix, the colon, the rectum, and the anal canal. The cecum is a blind side passage at the beginning of the large intestine. It hangs downward in the right iliac fossa, lying almost free of peritoneal attachments. Here's the appendix, sometimes called the vermiform appendix. It's a vestigial but potentially troublesome structure. The ileum projects a long way into the lumen of the cecum, opening at the ileo-cecal valve here. It's suspended by these two folds of mucosa. Despite its name and valve-like arangement, this opening is not an effective one-way valve. The appendix opens into the cecum below the ileo-cecal valve. 5.2.11 Wall of the colon The colon has four named parts: ascending, transverse, descending and sigmoid. Before we look at these let's look at the features of the colon that make it different from the small intestine. Here's a typical length of colon. In the colon the longitudinal muscle isn't continuous: it's gathered into three strips called the teniae coli, here's one of them, here's another. The tenia are effectively shorter than the rest of the wall of the colon, they have the effect of drawstrings, producing these bulging sacculations. In many adults these diverticuli develop over time. They're protrusions of mucosa though the muscular layer. Here's the colon on the inside. In between the outward bulges, which are called haustra, these impressive mucosal folds can divide the lumen into separate compartments when the muscle contracts strongly. Seen in close up, the mucous membrane of the colon is smooth: there are no villi. 5.2.12 Colon: ascending, transverse, descending, sigmoid the ascending colon. It's held in place by the peritoneum of the posterior abdominal wall, which covers it on the front and sides. The ascending colon ends a long way back at this sharp 90° turn, the right colic flexure, or hepatic flexure. The hepatic flexure lies just below the lowest part of the liver, and the gall bladder, and in front of the lower part of the right kidney In its natural location it's partly hidden by the geater omentum that clings to its anterior surface. The omentum isn't he real attachment of the transverse colon: it's only loosely adherent to it. The real attachment of the transverse colon, which we can see when we pull it upwards, is this double sheet of peritoneum, the transverse mesocolon. The transverse colon hangs down in a curve that's parallel to the greater curve of the stomach. The two structures are connected, as we've seen, by the part of the greater omentum that's known as the gastro-colic ligament. The transverse colon ends higher and even further back than it started, at this sharp downward turn, the left colic flexure, or splenic flexure. Below the splenic flexure is the descending colon. Just like the ascending colon, it's fixed to the posterior abdominal wall. The descending colon is quite short. 5.2.16 Liver: principal features The liver occupies the highest part of the abdominal cavity. It's just beneath the diaphragm, which is here. Much the greater part of the liver lies to the right of the midline Most of the liver is covered by peritoneum. There's an area behind that isn't, as we'll see. The liver is attached to its surroundings by peritoneal folds Here's the liver by itself, seen from in front. This small dark area is an abnormality: it's a benign tumor. The liver has two main surfaces, a highly irregular posterior surface that's approximately flat, and this much larger outward facing surface that's smooth and highly convex. 5.2.17 Liver: peritoneal attachments the falciform ligament. It's a slender fold that runs from the highest part of the liver, down to this pronounced notch on the anterior border, the hepatic notch. Here's the falciform ligament in a more intact dissection Its anterior border is attached to the anterior abdominal wall, and its posterior border hangs free, all the way down to the umbilicus. In its free border there's a cordlike structure, the ligamentum teres, the remnant of the umbilical vein. The ligamentum teres runs through the hepatic notch, onto the underside of the liver. The line of attachment of the falciform ligament, and the hepatic notch, divide the liver into a small left lobe, and a much larger right lobe. That division exists only on the surface: internally the liver is divided quite differently The coronary ligament is continuous with a line of peritoneal reflection that goes round the front of the inferior vena cava, and back to the top. Four double folds of peritoneum extend from the edges of the line of reflection. Passing to right and left near the top of the liver are the two triangular ligaments. 5.2.18 Liver: posterior surface This busy area above the gallbladder is the porta hepatis, where the portal vein and hepatic artery enter the liver and the hepatic ducts leave it. The posterior surface of the liver is indented from top to bottom by this deep vertical groove, which ends down here at the hepatic notch. The lower part of the groove is formed by the ligamentum teres, which we've seen from in front. The upper part of the groove is formed by a continuation of the same cord-like structure, the ligamentum venosum. These two cords are remnants of the umbilical vein, and ductus venosus. The porta hepatis lies just to the right of the middle part of the vertical groove. The part of the liver to the left of the vertical groove is referred to as the left lobe. The large area to the right of the groove is subdivided into three named areas, the large right lobe, the quadrate lobe between the groove and the gallbladder (here's the quadrate lobe from in front) and this irregularly shaped portion between the groove and the vena cava, the caudate lobe. (More often, the caudate lobe is shaped like this.) In front, the division between the right and left lobes is the line of attachment of the falciform ligament These named lobes are only surface features that have no functional significance. Embryology of Peritoneal Cavity When it is initially formed, the gut (embryonic digestive tube) is the same length as the developing body. It undergoes exuberant growth, however, to provide the large absorptive surface required by nutrition. By the end of the 10th week of development, the gut is much longer than the body that contains it. For this increase in length to occur, the gut must gain freedom of movement relative to the body wall at an early stage, while still maintaining the connection with it necessary for innervation and blood supply. This growth (and later, the activity of the gut) is accommodated by the development of a serous cavity within the trunk that houses the increasingly lengthy and convoluted gut in a relatively compact space. The rate of growth of the gut initially outpaces the development of adequate space within the trunk (body), and for a time, the rapidly lengthening gut extends outside the developing anterior body wall (see the Clinical Box “Brief Review of Embryological Rotation of the Midgut,” p. 481). Early in its development, the embryonic body cavity (intraembryonic coelom) is lined with mesoderm, the primordium of the peritoneum. At a slightly later stage, the primordial abdominal cavity is lined with parietal peritoneum derived from mesoderm, which forms a closed sac. The lumen of the peritoneal sac is the peritoneal cavity. As the organs develop, they invaginate (protrude) to varying degrees into the peritoneal sac, acquiring a peritoneal covering, the visceral peritoneum. A viscus (organ) such as the kidney protrudes only partially into the peritoneal cavity; hence, it is primarily retroperitoneal, always remaining external to the peritoneal cavity and posterior to the peritoneum lining the abdominal cavity. Other viscera, such as the stomach and spleen, protrude completely into the peritoneal sac and are almost completely invested by visceral peritoneum—that is, they are intraperitoneal. These viscera are connected to the abdominal wall by a mesentery of variable length, which is composed of two layers of peritoneum with a thin layer of loose connective tissue between them. Generally, viscera that vary relatively little in size and shape, such as the kidneys, are retroperitoneal, whereas viscera that undergo marked changes in shape owing to filling, emptying, and peristalsis, such as the stomach, are invested with visceral peritoneum. Intraperitoneal viscera with a mesentery, such as most of the small intestine, are mobile, the degree of which varies with the length of the mesentery. Although the liver and spleen do not change shape as a result of intrinsic activity (although they may slowly change in size when engorged with blood), their need for a covering of visceral peritoneum is dictated by the need to accommodate passive changes in position imposed by the adjacent, highly active diaphragm. As organs protrude into the peritoneal sac, their vessels, nerves, and lymphatics remain connected to their extraperitoneal (usually retroperitoneal) sources or destinations so that these connecting structures lie between the layers of the peritoneum forming their mesenteries. Initially, the entire primordial gut is suspended in the center of the peritoneal cavity by a posterior mesentery attached to the midline of the posterior body wall. As the organs grow, they gradually reduce the size of the peritoneal cavity until it is only a potential space between the parietal and visceral layers of peritoneum. As a consequence, several parts of the gut come to lie against the posterior abdominal wall, and their posterior mesenteries become gradually reduced because of pressure from overlying organs (Fig. 5.24). For example, during development, the growing coiled mass of small intestine pushes the part of the gut that will become the descending colon to the left side and presses its mesentery against the posterior abdominal wall. The mesentery is held there until the layer of peritoneum that formed the left side of the mesentery and the part of the visceral peritoneum of the colon lying against the body wall fuse with the parietal peritoneum of the body wall. As a result, the colon becomes fixed to the posterior abdominal wall on the left side with peritoneum covering only its anterior aspect. The descending colon (as well as the ascending colon on the right side) has thus become secondarily retroperitoneal, having once been intraperitoneal ([Moore et al., 2016]). The layers of peritoneum are now fused by means of a fusion fascia (of Toldt; see [Culligan 2012]), a connective tissue plane between the retroperitoneum and the former descending mesocolon in which the nerves, vessels, and lymph nodes of the descending colon continue to lie. Thus, the descending colon of the adult can be freed from the posterior body wall (surgically mobilized) by incising the peritoneum along the lateral border of the descending colon and then bluntly dissecting along the plane of the fusion fascia, elevating the neurovascular structures from the posterior body wall until the midline is reached. The ascending colon can be similarly mobilized on the right side. Several parts of the gastrointestinal tract and associated organs become secondarily retroperitoneal (e.g., most of the duodenum and pancreas as well as the ascending and descending parts of the colon). They are covered with glistening peritoneum only on their anterior surface. Other parts of the viscera (e.g., the sigmoid colon and spleen) retain a relatively short mesentery. However, the roots of the short mesenteries do not arise from the midline but shift to the left or right by a fusion process like that described for the descending colon. Peritoneal formations The peritoneal cavity has a complex shape. Some of the facts relating to this include the following: The peritoneal cavity houses a great length of gut, most of which is covered with peritoneum. Extensive continuities are required between the parietal and visceral peritoneum to convey the necessary neurovascular structures from the body wall to the viscera. Although the volume of the abdominal cavity is a fraction of the body's volume, the parietal and visceral peritoneum lining the peritoneal cavity within it have a much greater surface area than the body's outer surface (skin); therefore, the peritoneum is highly convoluted. Various terms are used to describe the parts of the peritoneum that connect organs with other organs, or to the abdominal wall, and the compartments and recesses that are formed as a consequence. A mesentery is a double layer of peritoneum that occurs as a result of the invagination of the peritoneum by an organ and constitutes a continuity of the visceral and parietal peritoneum. It provides a means for neurovascular communications between the organ and the body wall (Fig. 5.25A, E). A mesentery connects an intraperitoneal organ to the body wall—usually the posterior abdominal wall (e.g., mesentery of the small intestine). The small intestine mesentery is usually referred to simply as “the mesentery”; however, mesenteries related to other specific parts of the alimentary tract are named accordingly—for example, the transverse and sigmoid mesocolons (Fig. 5.25B), mesoesophagus, mesogastrium, and meso-appendix. Mesenteries have a core of connective tissue containing blood and lymphatic vessels, nerves, lymph nodes, and fat (see Fig. 5.48A). An omentum is a double-layered extension or fold of peritoneum that passes from the stomach and proximal part of the duodenum to adjacent organs in the abdominal cavity (Fig. 5.25). The greater omentum is a prominent, four-layered peritoneal fold that hangs down like an apron from the greater curvature of the stomach and the proximal part of the duodenum (Fig. 5.25A, C, & E). After descending, it folds back and attaches to the anterior surface of the transverse colon and its mesentery. The lesser omentum is a much smaller, double-layered peritoneal fold that connects the lesser curvature of the stomach and the proximal part of the duodenum to the liver (Fig. 5.25B, D). It also connects the stomach to a triad of structures that run between the duodenum and liver in the free edge of the lesser omentum (Fig. 5.23). A peritoneal ligament consists of a double layer of peritoneum that connects an organ with another organ or to the abdominal wall. The liver is connected to the anterior abdominal wall by the falciform ligament (Fig. 5.26). stomach by the hepatogastric ligament, the membranous portion of the lesser omentum. duodenum by the hepatoduodenal ligament, the thickened free edge of the lesser omentum, which conducts the portal triad: portal vein, hepatic artery, and bile duct (Figs. 5.23 and 5.26). The hepatogastric and hepatoduodenal ligaments are continuous parts of the lesser omentum and are separated only for descriptive convenience. The stomach is connected to the: inferior surface of the diaphragm by the gastrophrenic ligament. spleen by the gastrosplenic ligament, which reflects to the hilum of the spleen. transverse colon by the gastrocolic ligament, the apron-like part of the greater omentum, which descends from the greater curvature, turns under, and then ascends to the transverse colon. All these structures have a continuous attachment along the greater curvature of the stomach and are all part of the greater omentum, separated only for descriptive purposes. Although intraperitoneal organs may be almost entirely covered with visceral peritoneum, every organ must have an area that is not covered to allow the entrance or exit of neurovascular structures. Such areas are called bare areas, formed in relation to the attachments of the peritoneal formations to the organs, including mesenteries, omenta, and ligaments that convey the neurovascular structures. A peritoneal fold is a reflection of peritoneum that is raised from the body wall by underlying blood vessels, ducts, and ligaments formed by obliterated fetal vessels (e.g., the umbilical folds on the internal surface of the anterolateral abdominal wall, Fig. 5.13). Some peritoneal folds contain blood vessels and bleed if cut, such as the lateral umbilical folds, which contain the inferior epigastric arteries. A peritoneal recess, or peritoneal fossa, is a pouch of peritoneum that is formed by a peritoneal fold (e.g., the inferior recess of the omental bursa between the layers of the greater omentum, and the supravesical and umbilical fossae between the umbilical folds; see Fig. 5.13). Subdivisions of peritoneal cavity After the rotation and development of the greater curvature of the stomach during development (see the Clinical Box “Brief Review of Embryological Rotation of Midgut,” p. 481), the peritoneal cavity is divided into the greater and lesser peritoneal sacs (Fig. 5.27A). The greater sac is the main and larger part of the peritoneal cavity. A surgical incision through the anterolateral abdominal wall enters the greater sac. The omental bursa (lesser sac) lies posterior to the stomach and lesser omentum The transverse mesocolon (mesentery of the transverse colon) divides the abdominal cavity into a supracolic compartment, containing the stomach, liver, and spleen, and an infracolic compartment, containing the small intestine and ascending and descending colon. The infracolic compartment lies posterior to the greater omentum and is divided into right and left infracolic spaces by the mesentery of the small intestine (Fig. 5.27B). Free communication occurs between the supracolic and the infracolic compartments through the paracolic gutters, the grooves between the lateral aspect of the ascending or descending colon and the posterolateral abdominal wall. Flow is freest on the right side. The omental bursa is an extensive sac-like cavity that lies posterior to the stomach, lesser omentum, and adjacent structures (Figs. 5.23, 5.27A, and 5.28). The omental bursa has a superior recess, limited superiorly by the diaphragm and the posterior layers of the coronary ligament of the liver, and an inferior recess between the superior parts of the layers of the greater omentum (Figs. 5.26 and 5.28A). . The omental bursa permits free movement of the stomach on the structures posterior and inferior to it because the anterior and posterior walls of the omental bursa slide smoothly over each other. Most of the inferior recess of the bursa becomes sealed off from the main part posterior to the stomach after adhesion of the anterior and posterior layers of the greater omentum (Fig. 5.28B). The omental bursa communicates with the greater sac through the omental foramen (epiploic foramen), an opening situated posterior to the free edge of the lesser omentum (hepatoduodenal ligament). The omental foramen can be located by running a finger along the gallbladder to the free edge of the lesser omentum (Fig. 5.29). The omental foramen usually admits two fingers. The boundaries of the omental foramen are as follows: Anteriorly: the hepatoduodenal ligament (free edge of lesser omentum), containing the hepatic portal vein, hepatic artery, and bile duct (Figs. 5.23 and 5.26). Posteriorly: the IVC and a muscular band, the right crus of the diaphragm, covered anteriorly with parietal peritoneum. (They are retroperitoneal.) Superiorly: the liver, covered with visceral peritoneum (Figs. 5.28 and 5.29). Inferiorly: the superior or first part of the duodenum. Oesophagus, stomach, small intestine and large intestine Liver, biliary ducts and gall bladder