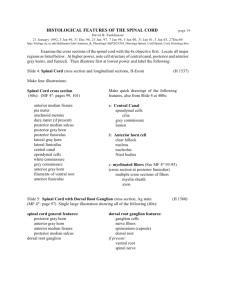
SPINAL CORD The spinal cord is an elongated cylindrical portion of the Central Nervous System. It extends from the upper border of the first cervical vertebra/ atlas (caudal border of the pyramidal decussation), upper limit is just above the level of the exit of the first spinal nerve and caudally, it terminates as the conus medullaris which is located in the lower border of L1 and upper L2. The spinal cord is a continuous unsegmented structure, paired spinal nerves but because of the presence of paired spinal nerves this gives the external segmentation appearance of the cord. These spinal nerves come from the cord segment. A cord segment is a part of the spinal cord that receives and gives off dorsal and ventral rootlets to a spinal nerve. For each cord segment, it has one pair of spinal nerves. There are 31 cord segments namely 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1 coccygeal. Spinal cord is protected by the meninges and CSF, vertebral bones and ligaments Up to the 3rd month, the cord will extend the entire length of the vertebral column, after that there is an equal rate of growth of cord and vertebral column so that the tip of the spinal cord is located higher than the vertebral tip of the vertebral column. At 1year old, the caudal tip of the spinal cord is located between L3 and L4, in adults it is located between L1 and L2 vertebra. The length of spinal cord is 42-45cm and it is longer in males than females and weighs around 35g. The spinal cord will occupy ⅔ of the vertebral column. In cases of spinal cord injury, we have the rule of 2 which states that in order to determine the cord segment involved, add 2 to the vertebral spine to be examined. For example, if you are examining T10 vertebral spine, T12 cord segment is involved. This rule is only applicable to C2-T10 cord segments. This rule is not that accurate/exact. For T11/T12, these are at the level of T10 vertebral spines. The caudal termination which is a cone shaped termination called conus medullaris and located at tip of it is the filum terminale which is the caudal extension of the pia matter. External Configuration For external configuration, the diameter of the cord is not uniform in length. There are some regions that have greater diameter which are the cervical and lumbosacral enlargements. The cervical enlargement is located in the C4-T1 and this corresponds to the brachial plexus. Lumbosacral enlargement extends from L 1-S2 and corresponds to the lumbosacral plexus. Another external configuration is the spinal nerves. One spinal cord segment has ventral and dorsal root. Along the course of the dorsal root is an oval elongation called the dorsal root or sensory spinal ganglion containing nerve cell bodies of the afferent fibers that enters the spinal cord and this dorsal root ganglion will enter the cord via the posterolateral sulcus. The ventral root ganglion will exit the cord via the anterolateral sulcus. Typical spinal nerves pass through the intervertebral foramen except for C1 which passes between upper cervical vertebral and base of occipital bone. C2-C7 intervertebral foramina above their corresponding vertebra. C8 will pass between C7 and T1 while the rest of the spinal nerves will pass through the intervertebral foramen below their corresponding vertebra.Since the spinal cord is shorter than the vertebral column, the lumbosacral nerve fibers will develop long roots called the cauda equina which extends within the spinal cistern and runs along the filum terminale. Grooves and Sulci Posteriorly, at the midline surface of the cord is the posterior median sulcus. On each side of the posterior median sulcus is the posterolateral sulcus which serves as the entrance of the dorsal roots. Between these is the posterointermediate sulcus that divides the posterior surface of the cord into two columns namely fasciculus gracilis and fasciculus cuneatus. On the anterior surface of the cord, you have a groove that is more prominent and wider than the posterior median sulcus and is called the anterior median fissure. Running along the anterior median fissure is the linea splendens which is a thickened band of the pia matter as well as the anterior spinal artery. The anterior median fissure will serve as a landmark determining the anterior surface of the cord because it is more prominent. On each side of the anterior median fissure is the anterolateral sulcus which serves as the exit for the ventral spinal nerves. Internal Configuration A cross section of the cord will show that it is divided into two symmetrical halves by the anterior median fissure and posterior median sulcus. Located at the central portion of the cord is the gray matter. This is an H-shaped nervous tissue containing nerve cell bodies and neuroglia. It has a dorsal horn which serves as the posterior limb of the gray matter. It has a constricted portion known as the cervix and a pointed dorsally located apex, dilated portion head, neck and base. Posterior or dorsal horn contains neurons that are sensory in nature. Anteriorly, we have the anterior or ventral horn which serves as the anterior limb of the gray matter and contain neurons that are motor in nature. The two halves of the gray matter are connected by the transverse bar known as the gray commissure which contains the central canal. Anterior to gray commissure is the anterior gray commissure and posterior to it is the posterior gray commissure. Surrounding the gray matter is the white matter. Within the white matter, this contains both descending and ascending myelinated nerve fibers arranged in parallel bundles known as tracts. This is divided into posterior funiculus, located between the posterior median sulcus and posterolateral sulcus and is divided into two by the sulcus intermedius. Between the posterolateral sulcus and anterolateral sulcus is the lateral funiculus. Between the anteromedian fissure and anterolateral sulcus is the anterior funiculus. The presence of the lateral extension of the gray matter between the junction between anterior and posterior horn: lateral horn. Prominent in the thoracic cord segments. Take note that the posterior horn will extend into posterolateral sulcus. Whereas the ventral horns will not extend into the anterolateral sulcus. Take note that the ventral horns of the cervical, lumbar, sacral segment are MASSIVE compared to thoracic segment. It is because they innervate skeletal muscles in the extremities. Ventral horns of the lumbar and sacral are much greater than cervical because of the greater muscle mass of the lower limb compared to upper extremities. There is more white matter in the cervical and upper thoracic region because as the tracts ascend, more fibers are added. This contains nerve fibers that connect the entire spinal cord to the higher centers. Whereas in the lumbar and sacral regions, this only contains nerve fibers serving the caudal region of the spinal cord. Tabulation of the differences of the spinal cord Components of Gray Matter In the CNS, groups of neurons having the same function and same type are called nuclei or nucleus. All of the neurons in the posterior horn are sensory in nature and they are grouped into four groups. 1. Nucleus posteromarginalis : conveys impulses in nociception, thermal sensation, light touch a. Located at the tip of the posterior horn b. More numerous in lumbosacral region 2. Substantia gelatinosa: for pain and temperature and touch sensation a. Anterior to the nucleus posteromarginalis b. Located at the apex and head region of the posterior horn c. More well developed in the sacral region. 3. Nucleus proprius cornu dorsalis: for pain,light touch and temperature, provide input to ventral and lateral spinothalamic tracts a. Head and neck portion of the posterior horn 4. Nucleus dorsalis of Clarke: Conveys information for position and movements of the individual muscles of the lower limb to the higher centers, for proprioception a. Medial aspect at the base of the posterior horn b. C8-L3 5. Nucleus intermediomedialis a. Opposite to the nucleus dorsalis of clark, at the base of the posterior horn b. Receives visceral afferent fiber, relay for visceral motor neurons 6. Nucleus intermediolateralis a. Lateral horn, this is definitely a thoracic segment because of the presence of the lateral horn b. C8-L3 c. Preganglionic fibers of the ANS Components of the White Matter In the white matter you will find descending and ascending fiber bundles. In the central nervous system, these groups of bundles having the same origin, course, termination and function are called tracts or funiculus. For the posterior funiculus, we have two. 1. Fasciculus gracilis: ascending sensory pathway of the lower half of the body a. Located between the posterior median sulcus and sulcus intermedius b. Touch, pressure, vibration, proprioception 2. Fasciculus cuneatus: ascending sensory pathway carrying impulses only from the upper half of the body a. Medial to the fasciculus gracilis b. Between sulcus intermedius and posterolateral sulcus c. Only until T7-T8 At the posterolateral sulcus between the periphery of spinal cord and tip of the spinal cord is the Zone of Lissauer. This serves as the pathway for pain and temperature sensation We proceed to the lateral funiculus of the white matter. 1. Posterior spinocerebellar tract a. Occupying the posterolateral periphery of the lateral funiculus b. L3 upward c. fine coordination of posture and movement of muscles of the lower limbs 2. Anterior spinocerebellar tract a. Anterolateral periphery of the lateral funiculus b. Extend up to L3 cord segment c. function for posture and movement from the entire lower limb rather than individual lower extremities Both spinocerebellar tracts are concerned with transmission to the cerebellum and impulses coming from the joints, tendons, and skin at the subconscious level. Both of these tracts are concerned primarily with the lower extremities. 3. Lateral spinothalamic tract a. Medial to the spinocerebellar tract b. Main pathway for pain and temperature sensation c. Crosses at spinal cord level 4. Lateral corticospinal tract a. Occupying the posterior half of the lateral funiculus b. Descending motor pathway c. Skilled, voluntary movements of the muscles of the distal extremities specifically of the hands and feet d. Crosses at the upper center, medulla At the anterior funiculus: 5. Anterior corticospinal tract a. Oval area just adjacent to the anterior median fissure b. Extend from C1 to upper thoracic segment c. Descending motor pathway concerned with skilled voluntary movements of the axial and upper limb and neck muscles 6. Anterior spinothalamic tract a. Anterior to the ventral horn b. Carries impulses for light touch c. Evoke by stroking skin with cotton or feather You can also group the components of the white matter as ascending and descending tracts. Take note that the posterior funiculus is purely sensory and composed of purely ascending tracts. While the Lateral and Anterior funiculi are a mixture of sensory and motor tracts. Dermatomes The sensory signals to the skin are established in bands known as dermatomes which represent the distribution of the spinal nerves responsible for innervating a particular cutaneous or skin region. These skin areas are supplied by the sensory fibers from a single dorsal root and its ganglion. Most of these dermatomes are supplied by fibers of 3 or more dorsal roots and adjacent dermatomes overlap. This means that if you cut one spinal nerve, it will not produce a detectable anesthesia. Cutting 3 or 4 dermatomes above or below will produce a complete anesthesia. Except for C2 which is the only spinal nerve that has no overlap so if you cut C2 alone, it will produce a complete anesthesia. Same with the trigeminal nerve that supplies the muscles of the face. The trigeminal nerve has 3 dermatomes namely the ophthalmic, maxillary and mandibular so there is no overlap for this nerve. Take note that there is no C1 because it does not have a sensory root therefore C2 will serve as the first dermatome. Dermal innervation of important landmarks of the body C2 innervates occiput. Nipple area is innervated by T4-T5. Umbilicus is innervated by T9-T10 Myotomes Muscles innervated by motor neurons from a single spinal cord segment or spinal nerves. Myotomes will also overlap. Examples : C5-C6 will supply the biceps brachii muscles which flexes the elbow. C6-C8 supplies the triceps brachii for elbow extension. Clinical importance of knowing dermatomes and myotomes: this will help us localize the neurologic levels particularly in radiculopathy or when there is a nerve root involvement or neuropathy. For example in herpes-zoster, the lesions will follow a specific dermatome. Knowing that the nipple area is supplied by T4 and the lesion is located above the nipple line, we can conclude that T2 or T3 dermatomes are affected. To check for dermatomes, use a cotton or pin, tell the patients to close their eyes and ask them to give feedback on the various stimuli. Testing should be done on specific dermatomes and compared bilaterally. If there is no sensation perceived, there is an affectation of that particular dorsal root. To check for myotomes, look for weakness. Check for elbow flexion, apply the resistance and ask the patient to flex against the resistance. Brown-Sequard Syndrome This is known as the brown-sequard hemiplegia or spinal hemiparaplegia and is a rare neurological condition. This is a hemisection of the spinal cord so one half of the spinal cord is damaged. This could be complete or incomplete. Hemisection of the spinal cord will produce loss of motor function on the ipsilateral side and loss of sensation on the contralateral side. Common causes include trauma or tumor. There is a loss of motor function of the ipsilateral side and loss of sensation on the contralateral side because this involves the 3 main neural pathways namely: - Lateral spinothalamic tract - Lateral corticospinal tract - Posterior columns- fasciculus gracilis and cuneatus For example if the right side of the cord segment is affected, take for example the lateral corticospinal tract which is a descending motor pathway. Involvement of this tract will produce a spastic paralysis on the same side of the lesion and below the level of the lesion due to the loss of moderation due to the loss of moderation coming from the upper motor neurons. At the level of the lesion, there will be flaccid paralysis because of the muscles supplied by the nerve at that level. There is involvement of the lower motor neurons at the level of the lesion. For the posterior column fibers, these are ascending sensory fibers, there will be ipsilateral loss of vibration, proprioception and fine touch. Upon touching the side of the lesion, the patient will not be able to localize where they are being touched. There is a contralateral loss of sensation because remember that the lateral spinothalamic tract is the main pathway for pain and sensation. As the fibers enter the spinal cord, it will synapse with the Zone of Lissauer and ascend 1-2 segments above and synapse again with the neurons of the posterior gray horn. It will cross the midline anterior to the central canal within the white anterior commissure and joins the lateral spinothalamic tract. Contralateral loss of sensations is due to the interruption of the crossed ascending fibers of the lateral spinothalamic tract. Best way to diagnose a spinal cord lesion is with the use of an MRI. Treatment is directed to the main pathology. If due to trauma, the patient has to undergo surgery. Medications are also given like anti-inflammatory drugs. If the patient is stabilized, he can be enrolled to physical/occupational therapy to regain motor and sensory loss. Source: Carpenter’s