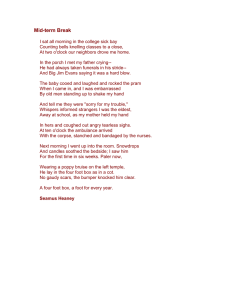
88 ORIGINAL ARTICLE The Foot Posture Index: Rasch Analysis of a Novel, Foot-Specific Outcome Measure Anne-Maree Keenan, MAppSc, Anthony C. Redmond, PhD, Mike Horton, BSc, Philip G. Conaghan, PhD, Alan Tennant, PhD ABSTRACT. Keenan A-M, Redmond AC, Horton M, Conaghan PG, Tennant A. The Foot Posture Index: Rasch analysis of a novel, foot-specific outcome measure. Arch Phys Med Rehabil 2007;88:88-93. Objective: To investigate the internal construct validity of a clinician-assessed measure of foot position, the Foot Posture Index (FPI), versions FPI-8 and FPI-6. Design: Rasch analysis of baseline FPI scores from studies conducted during the development of the instrument. Setting: A community-based and a hospital-based study, conducted at 2 institutions. Participants: Measures were obtained from 143 participants (98 men, 45 women; age range, 8 – 65y). Interventions: Not applicable. Main Outcome Measures: Rasch analysis was undertaken using RUMM2020 software in order to evaluate the following properties of the FPI: unidimensionality of each item included in the FPI, the differential item functioning (DIF) of each item, and item and person separation indices. Results: In the developmental draft of the instrument, the 8-item FPI-8 showed some misfit to the Rasch model (216 test⫽27.63, P⫽.03), indicating lack of unidimensionality. Two items were identified as problematic in the Rasch modeling: Achilles’ tendon insertion (Helbing’s sign), which showed illogical response ordering and “congruence of the lateral border of the foot,” which showed misfit, indicating that this item may be measuring a different construct (22 test⫽15.35, P⬍.01). All FPI-8 items showed an absence of DIF, and the person separation index (PSI) was good (PSI⫽.88). The revised FPI-6, which does not include the 2 problematic items, showed unidimensionality (212 test⫽11.49, P⫽.49), indicating a good overall fit to the model, and improvement over the preliminary version. With the removal of the 2 problematic items, there were no disordered thresholds; all items remained DIF free and all individual items displayed a good fit to the model. The person-separation index for the FPI was similar for both the 8-item (FPI-8⫽.880) and 6-item (FPI-6⫽.884) versions. Conclusions: The original FPI-8 showed significant mismatching to the model. The 2 items in the FPI-8 that were identified as problematic in clinical validation studies were also found to be contributing to the lack of fit to the Rasch model. The finalized 6-item instrument showed good metric proper- From the Academic Unit of Musculoskeletal Disease, University of Leeds, Leeds, UK. Presented in part to Health Outcomes 2005: Making a Difference, August 17–18, 2005, Canberra, Australia, and the British Society for Rheumatology, May 17–18, 2006, Glasgow, Scotland. No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated. Reprint requests to Anne-Maree Keenan, MAppSc, Academic Unit of Musculoskeletal Disease, University of Leeds, Chapel Allerton Hospital, Chapeltown Rd, Leeds, LS7 4SA, United Kingdom, e-mail: a.keenan@leeds.ac.uk. 0003-9993/07/8801-10886$32.00/0 doi:10.1016/j.apmr.2006.10.005 Arch Phys Med Rehabil Vol 88, January 2007 ties, including good individual item fit and good overall fit to the model, along with a lack of differential item functioning. This analysis provides further evidence for the validity of the FPI-6 as a clinical instrument for use in screening studies and shows that it has the potential to be analyzed using parametric strategies. Key Words: Foot; Rehabilitation; Treatment outcome. © 2007 by the American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation HE FOOT POSTURE INDEX (FPI) is a novel, footspecific outcome measure that was developed in order to T quantify variation in the position of the foot easily and quickly in a clinical setting. It is particularly intended for large sample studies where complex instrumented assessment (eg, gait laboratory assessment) is impractical or unnecessary. It has already been used in studies of risk factors for injury in athletes and naval recruits, treatment of plantar heel pain, and response to orthotic therapy in different foot types.1-5 The original draft of the FPI was based on clinician assessment of 8 characteristics of foot posture (a version known as the FPI-8) but after further validity and reliability investigations, the authors have suggested that the FPI-8 be reduced to a 6-item measure, the FPI-6.6 While the clinical validity and reliability of the FPI have been established,6-8 modern psychometric properties, such as unidimensionality and discriminatory ability, have yet to be determined. Foot Posture Index The FPI was developed in response to a commonly expressed need for better foot measures9-13 due to the absence of a widely accepted or adequately validated method for quantifying variation in foot posture in the clinical setting.14 The FPI consists of a series of criterion-based observations that combine to provide a quantification of postural variation in 3 major regions of the foot (rearfoot, midfoot, forefoot) in the 3 cardinal body planes. The scoring system uses a 5-point Likert-type scale where lower scores represent a more supinated foot position and higher scores a more pronated position. The original version of the FPI used 8 component scores (table 1) and demonstrated reasonable interrater and test-retest reliability across a number of patient populations.1,2,7 The original FPI-8 also demonstrated good construct validity6 when compared with the valgus index (a standing measure of foot position commonly used in research but cumbersome to use in a clinical setting),15,16 but only moderate concurrent validity measured against plain film radiographs.8 Item reduction based on a series of validation studies6 yielded a final 6-item version of the index, the FPI-6 (see table 1), which demonstrated good concurrent validity against a static lowerlimb kinematic model derived from an electromagnetic motion tracking system. Reliability is enhanced in the finalized version, and the capacity to predict dynamic foot postures during gait has been demonstrated to be better than for other clinical 89 FOOT POSTURE INDEX, Keenan Table 1: Individual Item Tests of Fit for the FPI-8 Items Item Item Difficulty (logits) SE Fit Res 2 Test df P Talar head palpation Curves above and below lateral malleoli Inversion and eversion of the calcaneus Bulge in the region of the TNJ Congruence of the medial longitudinal arch Abduction and adduction of the forefoot on the rear foot (too-many-toes) Congruence of the lateral border of the foot Helbing’s sign (curve of the Achilles’ tendon) ⫺1.24 1.05 ⫺0.48 0.70 ⫺1.01 1.68 ⫺0.43 ⫺0.27 .16 .17 .13 .16 .19 .15 .18 .19 0.89 1.20 0.05 ⫺1.28 ⫺1.68 ⫺1.41 1.88 0.72 2.00 1.02 1.01 2.91 3.19 1.83 15.35 0.32 2 2 2 2 2 2 2 2 .37 .60 .60 .23 .20 .40 ⬍.01 .85 NOTE. Location refers to the location the item is along the metric ruler, the standard error (SE) of the measure, and fit residuals (Fit Res), or how well each item relates to the overall model. A significant chi-square test indicates that an item does not fit the model. Abbreviation: TNJ, talo-navicular joint. measures.6 Further validation using modern psychometric standards17 provides valuable information about the performance characteristics and suitability of the measure to various methodologic applications. Rasch Analysis Rasch analysis is a probabilistic mathematical modeling technique used to assess properties of outcome measures including unidimensionality (the extent to which items measure a single construct), item difficulty (the relative difficulty of the items when compared to one another), and person separation (the extent to which items distinguish between distinct levels of functioning). Rasch analysis has been widely used in the development and validation of a number of outcome measures.17-20 The Rasch model is the current standard for the development of unidimensional scales (eg, of impairment or quality of life) delivering metric quality outcomes in health care.21 Data collected from ordinal questionnaires or scales, which are intended to be summated into an overall score, are tested against the expectations of this measurement model. The model defines the ideal item response characteristics if measurement (at the interval level) is to be achieved. The observed response patterns achieved are tested against expected patterns (a probabilistic form of Guttman scaling),22 and a variety of fit statistics determine whether fit is adequate to the model.23 Within the framework of Rasch measurement, the scale should work the same way, irrespective of the group being assessed (eg, items should behave similarly independent of age, sex, or disease characteristics).24 If, at the same overall level of impairment, groups do not display the same probability of affirming the item, then the item is deemed to display differential item functioning (DIF), thus violating the requirement of unidimensionality.25 Finally, Rasch modeling also transforms ordinal scores obtained by summing scores from each item into interval measures.26 Transformed scores (as logit values) form an internally valid and unidimensional measure that may be considered for parametric statistical analysis, which enables calculation of information such as percentage change, mean scores, and other values that cannot otherwise be expressed appropriately for ordinal data.27 The aim of this study was to assess the unidimensionality and DIF of the original FPI-8 and the finalized FPI-6 using Rasch analysis techniques. METHODS Data Capture In the first analysis, we captured FPI data from 143 people (98 men, 45 women) with a range of foot types, comprising 2 groups of participants involved in a series of validation experiments.6 Participants were either patients with Charcot-MarieTooth disease (n⫽12; 7 men, 5 women; age range, 8 – 63y) or healthy adults participating in a prospective injury study (n⫽131; 91 men, 40 women; age range, 18 – 65y). Ethics approval was granted by the university review boards of the University of Western Sydney, the University of Sydney, and the Children’s Hospital at Westmead in Sydney, as appropriate to the study site. All participants provided informed consent. Patients were assessed using all 8 items described in the original FPI and total scores were derived for both FPI-8 and FPI-6. Once the initial analyses of the FPI data to the Rasch model was finalized, we transformed the FPI scores to Rasch scores. The transformation of the raw FPI scores to Rasch scores is undertaken in order to change data that are ordinal in nature to Rasch transformed, interval scores. For the generation of transformed scores, large data sets are required; to undertake this transformation, a second data set (n⫽426) was used. This second data set included participants on whom demographic information (including sex and age) was not captured. As such, this data could not be included in the primary Rasch analysis, because assessment of DIF, a key aspect within the Rasch model, could not be included. Rasch analysis was repeated on the extended data set, prior to the transformation of the scores. We entered the data into both SPSSa and RUMM2020 software packages28,b using a Rasch partial credit model as the basis of analysis.29 Data were rescaled (⫹1 to ⫹5) to eliminate the negative numerals employed in the clinical scoring system (⫺2 to ⫹2). In the first instance, FPI-8 data was analyzed to evaluate initial fit of the data, threshold ordering and DIF. Re-analysis was then undertaken using the data from the modified FPI-6. General Tests of Fit To determine how the FPI fits the Rasch unidimensional model, we used a series of fit statistics. Item-trait interaction quantifies the fit of the observed data to the predicted model. This statistic, represented by the chi-square value, reflects the degree of invariance of each of the items and how they function together, so it represents how the items function across the 1 trait (or construct). A significant chi-square indicates that there are problems with fit of all the items: that is, that the score is not unidimensional. All of the items should assess the same (or a single) construct. For the FPI, each item included should be assessing foot posture; items should not be assessing muscle strength, flexibility, or range of motion. A further test to explore the unidimensionality of the instrument is to look at the residual fit statistics. The residuals are the standardized person-item differences between the observed data and what is expected by the model for every person’s Arch Phys Med Rehabil Vol 88, January 2007 90 FOOT POSTURE INDEX, Keenan response to every item. Because it is standardized, a perfect fit to the model would give a mean of zero and a standard deviation (SD) of 1 when summed over all items.30 Associated with the residual fit statistics, further evidence to support unidimensionality can be gathered by evaluating patterns in the residuals using principal components analysis of the fit residuals. The aim of this evaluation is to identify patterns of the residuals once the “Rasch factor” has been extracted. This is important in order to identify any subsets of items that may be loading together. The absence of any meaningful pattern in the residuals will be deemed to support the assumption of local independence of the items, where the response of 1 item is not conditional on the response of another.30 If any patterns are identified in the residuals, the significance of the pattern can be tested by comparing the person ability estimates (where one would expect the individual to score along the Rasch scale) generated from any subset of items that have been identified as loading together, to the person ability estimates generated from the entire item set. The person ability estimates are then compared via independent t tests. If less than 5% of the independent t tests are shown to be significant, then the assumption of local independence is supported.26 As well as considering unidimensionality, the fit statistics also consider the stability of the instrument, irrespective of the group being evaluated. While groups may be expected to have different foot postures (eg, women may have a slightly different FPI score than men; or people with Charcot-Marie-Tooth disease may have lower scores than those without), their group membership at any given level of the trait should not influence how they are scored. This type of analysis is referred to as DIF and is identified by a 2-way analysis of variance of the residuals31 with statistical significance indicating the presence of differential item functioning and, hence, compromise to the unidimensionality of the scale. Components should cover a range of less extreme and extreme characteristics (difficulty or severity) coherently. This is referred to as item difficulty or hierarchy and is expressed as a logit value, the natural logarithm of the odds of a person being able to perform a certain task.18 The hierarchy in the FPI scores relates to representation of the range of foot postures—from the most supinated through neutral to pronated foot types. The item difficulty reflects the internal construct validity of measure with the theoretical ordering of each of the items. The ability of the scale to discriminate among different groups of such patients is determined by the person separation index (PSI). Values above 0.7 indicate the ability to identify at Fig 1. Person-item threshold distribution for the FPI-8. Arch Phys Med Rehabil Vol 88, January 2007 least 2 groups of patients.32 The PSI in the Rasch model is analogous to the Cronbach ␣; 0.7 is considered a minimal value for group use and .85 for individual patient use.33 RESULTS The FPI-8 The initial overall item-trait interaction of the original FPI-8 indicated that some misfit to the Rasch model was apparent within the data (216 test⫽27.63, P⫽.03). The residual mean value for the items was .05, with an SD of 1.35. A significant item-trait interaction indicated that some items of foot positioning were not measuring in a consistent manner among discrete groups of people with differing foot postures. An analysis of the threshold ordering indicated that one of the items (Helbing’s sign) displayed disordered thresholds, meaning that the scoring response categories did not follow the expected ordering. All other 7 items displayed appropriately ordered thresholds. Given this fundamental lack of fit to the model, detailed principal components analysis of the fit residuals was not examined for the FPI-8. Further analysis of individual items indicated that the fit of another item, congruence of the lateral border of the foot, was also problematic (22 test⫽15.35, P⫽.01) and appeared to be measuring a separate dimension not related to the overall FPI. The misfit indicates that there was a lack of the expected probabilistic relationship between this particular item and the other items in the FPI-8. The possibility of sex differences in FPI rating was explored by analysis of DIF with Bonferroni adjustments for multiple comparisons. All items on the FPI-8 were DIF free, indicating a lack of bias associated with sex. A summary table of the individual item separation and tests of fit is presented in table 1. The person item threshold map is represented in figure 1. The distribution of the items indicated that range of difficulty covered by the items was comprehensive. The items were at least 0.1 standard errors (SEs) apart (see table 1), indicating appropriate discrimination between foot types. The person-fit separation index for the FPI-8 of .88 and the Cronbach ␣ of .86 indicating that there was good internal consistency with the measure. The FPI-6 To investigate whether the validation process and subsequent refinement of the instrument had improved its internal construct validity, Rasch analysis was performed on the final- 91 FOOT POSTURE INDEX, Keenan Table 2: Individual Item Tests of Fit for the FPI-6 Items Item Item Difficulty (logits) SE Fit Res 2 Test df P Talar head palpation Curves above and below lateral malleoli Inversion and eversion of the calcaneus Bulge in the region of the TNJ Congruence of the medial longitudinal arch Abduction and adduction of the forefoot on the rear foot (too-many-toes) ⫺1.64 0.98 0.53 ⫺1.25 1.68 ⫺0.30 .16 .18 .17 .20 .16 .21 0.26 1.55 ⫺0.91 ⫺1.29 ⫺0.86 1.33 0.87 3.32 3.35 1.90 0.80 1.25 2 2 2 2 2 2 .65 .19 .19 .39 .67 .54 NOTE. Location refers to the location the item is along the metric ruler, the SE of the measure, and fit residuals, or how well each item relates to the overall model. A significant chi-square test indicates that an item does not fit the model. ized FPI-6. Of note, the 2 items that had been removed following the clinical validation process (the lateral border of the foot and Helbing’s sign) were the same items that had proved problematic in the Rasch analysis of the FPI-8. Re-analysis using the data from the 6-item version of the FPI showed good item-trait interaction (212 test⫽11.49, P⫽.49), indicating a good overall fit to the model. The residual mean value for the items was .012, with an SD of 1.22. With the removal of the 2 problematic items, there were no disordered thresholds, all items remained DIF free and all individual items displayed a good fit to the model, in terms of chi-square probability and fit residuals (table 2). A principal components analysis of the residuals indicated that the first component accounted for 27.84% of the variance, thus supporting the notion that the scale is unidimensional. Furthermore, the person frequency distribution (fig 2) demonstrated that there was a large measurement range of the item thresholds in the FPI-6 and indicated that the measure was able to discriminate across different foot positions. Testing of the local dependency of the items once the FPI-6 was put through the Rasch model indicated that there was a minor pattern in the residuals; items associated with rearfoot measurement (frontal plane motion of the calcaneus; talar head palpation and curvature of the malleoli) loaded in 1 direction, while items associated with the midfoot (sustentaculum tali, medial longitudinal arch and adduction, abduction of the forefoot) loaded in the other direction. Person estimates were generated from the 2 subsets of items identified, and these were compared with the person estimates generated from the entire item set. The differences were proved to be trivial, however, and not statistically significant for any of the independent t tests exploring differences between the FPI-6 and the midfoot or rearfoot subscales. As with the FPI-8 analysis, all items on the FPI-6 were DIF free, indicating no sex differences in FPI measurements. Assessment of the item difficulty indicated that the distribution of the items indicated that range of difficulty covered by the items was comprehensive. The items are again at least .15 SE apart, indicating increased discrimination between foot types compared with the FPI-8. As with the FPI-8, the person-fit separation of the FPI-6 was good, with the PSI of .88 and the Cronbach ␣ of .87 indicating that there was good internal consistency with the measure. Transformation Scores for the FPI-6 Rasch analysis of the extended data set demonstrated good fit to the model (232 test⫽46.7, P⫽.11). Person location data was transformed and mapped onto raw FPI-6 scores. A transformation table is presented in table 3, which lists the transformation values from raw FPI scores to the Rasch transformed logit values. DISCUSSION The FPI was designed to provide an objective measure of foot posture quickly and easily in a clinical setting. While the validation and reliability of the FPI has been described previously, the aim of the current study was to describe in detail the internal construct validity of the FPI and to explore the fit of the data to the latest statistical models. Our results indicated that while the original FPI-8 demonstrated good internal consistency and may be of some clinical use, the data did not fit the Rasch model. Two items demonstrated poor metric properties—Helbing’s sign and the congruence of the lateral border of the foot— both of which were also identified as problematic in the clinical validation studies. Helbing’s sign demonstrated a Fig 2. Person-item threshold distribution for the FPI-6. Arch Phys Med Rehabil Vol 88, January 2007 92 FOOT POSTURE INDEX, Keenan Table 3: Conversion of Raw FPI-6 Scores to Rasch Transformed Scores FPI-6 Raw Score Transformed Score ⫺12 ⫺11 ⫺10 ⫺9 ⫺8 ⫺7 ⫺6 ⫺5 ⫺4 ⫺3 ⫺2 ⫺1 0 1 2 3 4 5 6 7 8 9 10 11 12 ⫺10.47 ⫺7.96 ⫺6.45 ⫺5.54 ⫺4.84 ⫺4.25 ⫺3.71 ⫺3.20 ⫺2.67 ⫺2.12 ⫺1.54 ⫺0.91 ⫺0.21 0.50 1.16 1.75 2.33 2.98 3.81 4.83 5.68 6.36 7.01 7.77 8.65 NOTE. Calculations derived from data (n⫽426) that included those data in the Rasch analysis (n⫽143) and additional data from 2 other studies (n⫽283) not included in the detailed Rasch analysis due to inadequate clinical detail for evaluation of DIF. lack of discrimination in the extreme range, with very few of the 143 participants demonstrating lateral bowing of the Achilles’ tendon. Furthermore, there was some inappropriate ordering of the scores on the scale of this item indicating apparent difficulty in identifying degrees of difference. The lateral border of the foot criterion demonstrated significant mismatching to the model. It appeared that this item was not reflective of overall foot posture and was measuring a different construct, perhaps associated with foot shape or size. The removal of the 2 items and reanalysis of the finalized FPI-6 addressed these issues, supporting the validity of the FPI-6 as a unidimensional measure. The FPI-6 demonstrated good metric properties, including good individual item fit and good overall fit to the Rasch model, along with a lack of differential item functioning. While the FPI was originally developed as an ordinal measure, the results of the Rasch modeling of the FPI-6 indicate that summative FPI-6 score can be mapped satisfactorily to a linear metric. Metric mapping of the FPI-6 total scores assists in the use of the FPI-6 as a research tool: with appropriate assessment of raw FPI data and transformation of raw scores through the Rasch measurement model there is potential for employing parametric statistical analyses in studies using the FPI-6. Using the Rasch transformed score (see table 3) allows better consideration of clinically important outcomes, including percentage change scores and smallest detectable differences. Furthermore, if appropriate to a study design, transformed scores have the potential to be used to establish appropriate numbers for powering a study. While the results of this study validate the internal construct validity of the FPI-6, 2 limitations must also be acknowledged. Arch Phys Med Rehabil Vol 88, January 2007 First, it must be noted that the study used 2 groups co-opted from other studies; 1 group with known neuromuscular disease and a second healthy group. DIF was not found for sex but it is possible that in other applications, factors not investigated here may demonstrate DIF. This warrants further study in specific target groups. Furthermore, the sample size used is moderately large for a clinical validation study but is relatively small for Rasch analysis and this may affect the precision of the estimates of the Rasch model. A large scale study is still required to establish normative values for FPI-6 scores and it would be appropriate to confirm the findings of the current Rasch analysis in a larger sample. Finally, in all the data collected, including those for the transformation scores, there were no extreme values recorded at either end of the scale. While this may reflect the true clinical picture, in that it is unlikely to see such pronated or supinated cases, the values of the extreme estimates in the logit transformation are therefore not true values but extrapolated from the modeling available within RUMM2020. CONCLUSIONS The original FPI-8 demonstrated limitations in its internal construct validity, with 2 of the items (Helbing’s sign, congruence of the lateral border of the foot) demonstrating significant mismatching to the model. The removal of these 2 items following the clinical validation phase has addressed these issues. The finalized FPI-6 demonstrated good internal construct validity including good individual item fit and good overall fit to the model, along with a lack of DIF. The FPI-6 raw scores can be converted to Rasch transformed scores, thereby allowing data generated to be used as interval data. This serves as evidence that the FPI-6 is a unidimensional measure of foot posture and may be suited to a range of clinical applications. References 1. Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med 2004;32:772-80. 2. Noakes H, Payne C. The reliability of the manual supination resistance test. J Am Podiatr Med Assoc 2003;93:185-9. 3. Burns J, Keenan AM, Redmond AC. Foot type and triathlon related overuse injury. J Am Podiatr Med Assoc 2005;95:235-41. 4. Burns J, Crosbie J, Ouvrier R, Hunt A. Effective orthotic therapy for the painful cavus foot. J Am Podiatr Med Assoc 2006;96:205-11. 5. Landorf KB, Radford JA, Keenan AM, Redmond AC. Effectiveness of low-dye taping for the short-term management of plantar fasciitis. J Am Podiatr Med Assoc 2005;95:525-30. 6. Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech (Bristol, Avon) 2006;21:89-98. 7. Evans AM, Copper AW, Scharfbillig RW, Scutter SD, Williams MT. The reliability of the foot posture index and traditional measures of foot position. J Am Podiatr Med Assoc 2003;93:203-13. 8. Scharfbillig RW, Evans A, Copper A, et al. Criterion validity of four criteria of the foot posture index. J Am Podiatr Med Assoc 2004;91:31-8. 9. McClay IS. Report of “Static and dynamic classification of the foot” meeting, Annapolis, Maryland. May 2000. J Orthop Sports Phys Ther 2001;31:158. 10. Saltzman CL, Domsic RT, Baumhauer JF, et al. Foot and ankle research priority: report from the Research Council of the American Orthopaedic Foot and Ankle Society. Foot Ankle Int 1997; 18:447-8. FOOT POSTURE INDEX, Keenan 11. Keenan AM. A clinician’s guide to the practical implications of the recent controversy of foot function. Aust J Podiatr Med 1997;31:87-93. 12. Kitaoka HB, Lundberg A, Luo ZP, An KN. Kinematics of the normal arch of the foot and ankle under physiologic loading. Foot Ankle Int 1995;16:492-9. 13. Kitaoka HB, Zong Ping L, An JN. Effect of the posterior tibial tendon on the arch of the foot during simulated weightbearing: biomechanical analysis. Foot Ankle Int 1997;18:43-6. 14. Razeghi M, Batt ME. Foot type classification: a critical review of current methods. Gait Posture 2002;15:282-91. 15. Rose GK. Pes planus. In: Jahss MH, editor. Disorders of the foot and ankle: medical and surgical management. 2nd ed. Philadelphia: WB Saunders; 1991. p 892-920. 16. Thomson CE. An investigation into the reliability of the valgus index and its validity as a clinical measurement. Foot 1994;4: 191-7. 17. Rasch G. Probabilistic models for some intelligence attainment tests. Chicago: Univ Chicago Pr; 1960. 18. Duncan PW, Bode RK, Min Lai S, Perera S, Glycine Antagonist in Neuroprotection Americas Investigators. Rasch analysis of a new stroke-specific outcome scale: the Stroke Impact Scale. Arch Phys Med Rehabil 2003;84:950-63. 19. Dawson J, Linsell L, Doll H, et al. Assessment of the Lequesne index of severity for osteoarthritis of the hip in an elderly population. Osteoarthritis Cartilage 2005;13:854-60. 20. Gerber BS, Pagcatipunan M, Smith EV Jr, et al. The assessment of diabetes knowledge and self-efficacy in a diverse population using Rasch measurement. J Appl Meas 2006;7:55-73. 21. Tennant A, McKenna SP, Hagell P. Applications of Rasch analysis in the development and application of quality of life instruments. Value Health 2004;7(Suppl 1):S22-66. 22. Guttman LA. The basis for scalogram analysis. In: Stouffer SA, Guttman EA, Suchman PF, Lazarsfield SA, Clausen JA, editors. Measurement and prediction. Princeton: Princeton Univ Pr; 1950. p 60-90. 93 23. Hunt AE, Fahey AJ, Smith RM. Static measures of calcaneal deviation and arch angle as predictors of rearfoot motion during walking. Aust J Physiother 2000;46:9-16. 24. Tennant A, Penta M, Tesio L, et al. Assessing and adjusting for cross-cultural validity of impairment and activity limitation scales through differential item functioning within the framework of the Rasch model: the PRO-ESOR project. Med Care 2004;42(1 Suppl): I37-48. 25. Holland PW, Wainer H. Differential item functioning. Hillsdale: Lawrence Erlbaum Associates; 1993. 26. Smith EV Jr. Metric development and score reporting in Rasch measurement. J Am Podiatr Med Assoc 2000;1:303-26. 27. Svensson E. Guidelines to statistical evaluation of data from rating scales and questionnaires. J Rehabil Med 2001;33:47-8. 28. Andrich D, Lyne A, Sheridon B. RUMM 2020. Perth: RUMM Laboratory; 2003. 29. Masters G. A Rasch model for partial credit scoring. Psychometrika 1982;47:149-74. 30. Pallant JF, Tennant A. An introduction to the Rasch measurement model: an example using the Hospital Anxiety and Depression Scale (HADS). Br J Clin Psychol. In press. 31. Hagquist C, Andrich D. Is the sense of coherence-instrument applicable on adolescents? A latent trait analysis using Raschmodelling. Pers Individ Diff 2004;36:955-68. 32. Fisher WP Jr. Physical disability construct convergence across instruments: towards a universal metric. J Outcome Meas 1997; 1:87-113. 33. Streiner DL, Norman GR. Health measurement scales. 2nd ed. Oxford: Oxford Univ Pr; 1995. Suppliers a. Version 11; SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL 60606. b. RUMM Laboratory Pty Ltd, 14 Dodonaea Ct, Duncraig 6023, WA, Australia. Arch Phys Med Rehabil Vol 88, January 2007