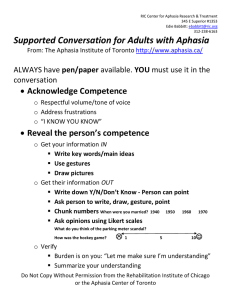
CLINICAL REVIEW Aphasia: an Overview Indexing Metadata/Description › Title/condition: Aphasia: an Overview › Synonyms: Dysphasia: an overview; agrammatic aphasia (nonfluent aphasia); aphasia, agrammatic (nonfluent aphasia); aphasia, expressive (nonfluent aphasia); aphasia, nonfluent; Broca's dysphasia (nonfluent aphasia); Broca's aphasia (nonfluent aphasia); dysphasia, Broca's (nonfluent aphasia); Broca-type aphasia; expressive aphasia (nonfluent aphasia); motor aphasia; nonfluent aphasia; sensory aphasia; fluent aphasia; receptive aphasia; jargon aphasia; Wernicke’s-type aphasia; aphasia, fluent; aphasia, sensory; aphasia, jargon; aphasia, receptive; Wernicke's aphasia (receptive aphasia, fluent aphasia); aphasia; Wernicke’s type; dysphasia, global; global aphasia; global dysphasia; transcortical sensory aphasia; aphasia, transcortical sensory; transcortical motor aphasia; aphasia, transcortical motor; conduction aphasia; aphasia, conduction; nominal aphasia; anomia, aphasia-associated; anomic dysphasia; aphasia, anomic; aphasia, nominal; aphasia-associated anomia; dysphasia, anomic; dysphasia, nominal; nominal dysphasia › Anatomical location/body part affected: The language centers of the brain › Area(s) of specialty: Adult Neurological Disorders › Description: Aphasia is an acquired communication disorder that occurs in patients who had previously learned and appropriately used language for communication.(98) Aphasia results from damage to the parts of the brain that control language abilities.(3) Aphasia can impair any or all of the following: speaking, listening, gestures, reading, and writing.(3,40,67) There are several distinct subtypes of aphasia, each of which results in a different combination of symptoms and communication deficits.(40,67,98) The subtypes of aphasia are Broca’s aphasia, Wernicke’s aphasia, global aphasia, anomic aphasia, transcortical motor aphasia, transcortical sensory aphasia, and conduction aphasia.(40,98) Author Heather Wiemer, MA, CCC-SLP Cinahl Information Systems, Glendale, CA Reviewers Amory Cable, PhD, CCC-SLP American Speech-Language-Hearing Association (ASHA) Rehabilitation Operations Council Glendale Adventist Medical Center, Glendale, CA Editor Sharon Richman, MSPT Cinahl Information Systems, Glendale, CA With each subtype of aphasia, severity can range from mild to profound.(18) For detailed assessment and treatment information on each subtype of aphasia, see the series of Clinical Reviews on this topic › G-codes • Motor Speech G-code set –G8999, Motor speech functional limitation, current status at time of initial therapy treatment/episode outset and reporting intervals –G9186, Motor speech functional limitation, projected goal status at initial therapy treatment/outset and at discharge from therapy –G9158, Motor speech functional limitation, discharge status at discharge from therapy/ end of reporting on limitation • Spoken Language Comprehension G-code set –G9159, Spoken language comprehension functional limitation, current status at time of initial therapy treatment/episode outset and reporting intervals –G9160, Spoken language comprehension functional limitation, projected goal status at initial therapy treatment/outset and at discharge from therapy –G9161, Spoken language comprehension functional limitation, discharge status at discharge from therapy/end of reporting on limitation October 5, 2018 Published by Cinahl Information Systems, a division of EBSCO Information Services. Copyright©2018, Cinahl Information Systems. All rights reserved. No part of this may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the publisher. Cinahl Information Systems accepts no liability for advice or information given herein or errors/omissions in the text. It is merely intended as a general informational overview of the subject for the healthcare professional. Cinahl Information Systems, 1509 Wilson Terrace, Glendale, CA 91206 • Spoken Language Expressive G-code set –G9162, Spoken language expression functional limitation, current status at time of initial therapy treatment/episode outset and reporting intervals –G9163, Spoken language expression functional limitation, projected goal status at initial therapy treatment/outset and at discharge from therapy –G9164, Spoken language expression functional limitation, discharge status at discharge from therapy/end of reporting on limitation • Other Speech Language Pathology G-code set –G9174, Other speech language pathology functional limitation, current status at time of initial therapy treatment/episode outset and reporting intervals –G9175, Other speech language pathology functional limitation, projected goal status at initial therapy treatment/outset and at discharge from therapy –G9176, Other speech language pathology functional limitation, discharge status at discharge from therapy/end of reporting on limitation ›. G-code Modifier Impairment Limitation Restriction CH 0 percent impaired, limited or restricted CI At least 1 percent but less than 20 percent impaired, limited or restricted CJ At least 20 percent but less than 40 percent impaired, limited or restricted CK At least 40 percent but less than 60 percent impaired, limited or restricted CL At least 60 percent but less than 80 percent impaired, limited or restricted CM At least 80 percent but less than 100 percent impaired, limited or restricted CN 100 percent impaired, limited or restricted Source: http://www.cms.gov . › Reimbursement: Reimbursement for therapy will depend on insurance contract coverage; no specific issues or information are identified regarding the reimbursement › Presentation/signs and symptoms: Each patient with aphasia will present with a unique set of symptoms. Although there are often similarities in language abilities between individuals with aphasia, it is not always possible to classify a patient’s aphasia according to the classically defined aphasia subtypes.(98) The following is a description of symptoms most commonly associated with each subtype of aphasia • Broca’s aphasia (expressive aphasia/nonfluent aphasia)(40,98) –Acalculia (mathematical deficits)(40) –Agrammatism(40) –Good awareness of language deficit(98) –Hesitant, awkward speech(98) –Impaired naming ability(98) –Impaired reading comprehension(40) –Impaired writing ability(18,40) –Limited vocabulary(98) –Nonprosodic speech(18) –Often presents with coexisting apraxia of speech (For detailed information on assessment and treatment of apraxia, see Clinical Review…Apraxia of Speech (Acquired); CINAHL Topic ID Number: T708586) –Paraphasias (word substitutions)(18) –Relatively preserved auditory comprehension; however, not completely intact(18,40) –Speech characterized by content words (nouns, verbs) and limited use of parts of speech (prepositions, conjunctions, pronouns)(98) –“Telegraphic” speech(40) –For detailed information about Broca’s aphasia, see Clinical Review…Aphasia, Broca's (Nonfluent Aphasia); CINAHL Topic ID Number: T708882 • Wernicke’s aphasia (receptive aphasia/fluent aphasia)(40,98) –Acalculia(40) –Fluent speech(40) –Frequent paraphasias and neologisms (nonsense word substitutions)(40) –Impaired auditory comprehension(40) - In a study conducted in the United Kingdom in which patients with Wernicke’s aphasia were compared to patients with other types of aphasia, researchers found that comprehension of spoken words was poorer than identification of the same concepts provided in a pictured form(131) - Additionally, auditory comprehension was slightly improved in patients with Wernicke’s aphasia (but not in people with other types of aphasia) when repetition of the information was provided(131) –Impaired reading comprehension(40,98) –Impaired writing ability(40,98) –Increased rate of speech/hyperfluency(40,98) –Jargon (incomprehensible speech comprised largely of nonsense words)(18) –Relatively good prosody of speech(18) –Reduced awareness of language deficit(98) –Reduced content of speech; limited appropriate use of nouns/verbs(40,98) –For detailed information about Wernicke’s aphasia, see Clinical Review…Aphasia, Wernicke's (Receptive Aphasia, Fluent Aphasia); CINAHL Topic ID Number: T708883 • Global aphasia(40,98) –Nonfluent speech(98) –Persistent stereotypical utterances (has also been found to occur in Broca’s aphasia; however, these utterances are much more common in global aphasia)(40,115) –Significant receptive and expressive language impairment(40) –Inability to read or write(98) –For detailed information about global aphasia, see Clinical Review…Aphasia, Global; CINAHL Topic ID Number: T708881 • Anomic aphasia(40) –Circumlocutions (vague verbal output; patient attempts to talk around the word he or she cannot produce)(98) –Good auditory comprehension(98) –Paraphasias(40) –Relatively fluent, prosodic, grammatical verbal output(18,40,98) –Significant word-finding and naming difficulty(40,98) –Reading and writing skills can be impaired; significant variation among patients with anomic aphasia(98) –For detailed information about anomic aphasia, see Clinical Review…Anomia Associated with Aphasia; CINAHL Topic ID Number: T708611 • Transcortical motor aphasia(98) –Nonfluent speech(98) –Good auditory comprehension(98) –Excellent repetition skills(98) –Significant naming impairment(98) –Relatively intact reading comprehension ability(98) –Impaired writing skills(98) –For detailed information about transcortical motor aphasia, see Clinical Review…Aphasia, Transcortical Motor; CINAHL Topic ID Number: T708868 • Transcortical sensory aphasia(98) –Impaired auditory comprehension(67) –Relatively fluent, prosodic verbal output(18,67) –Repetition preserved relative to auditory comprehension(18,98) –For detailed information about transcortical sensory aphasia, see Clinical Review…Aphasia, Transcortical Sensory; CINAHL Topic ID Number: T708866 • Conduction aphasia(98) –Spontaneous speech can be fluent or nonfluent(98) –Good auditory comprehension(98) –Naming impairment(98) –Very poor repetition skills; inability to repeat(18,98) –Reading and writing skills can be impaired; considerable variation among patients with conduction aphasia(98) –For detailed information about conduction aphasia, see Clinical Review…Aphasia, Conduction; CINAHL Topic ID Number: T708869 • Sometimes, pure word deafness is classified as an aphasic syndrome; pure word deafness refers to the loss of speech comprehension without any other language abnormalities; reading comprehension remains intact and nonverbal sounds are recognized without difficulty(18) –For detailed information on pure word deafness, see Clinical Review…Agnosia, Auditory Verbal; CINAHL Topic ID Number: T903016 • Aphasia most frequently occurs in adults; however, it can occur in children as well.(98) For detailed information on the assessment and treatment of aphasia in children, see Clinical Review…Aphasia, Acquired Childhood; CINAHL Topic ID Number: T708867 Causes, Pathogenesis, & Risk Factors › Causes: Aphasia is caused by central nervous system (CNS) disease or brain damage that compromises language structures of the brain in a focal (rather than generalized) manner(98) • Stroke is the most common cause of brain injury leading to aphasia. Other causes include severe blows to the head, brain tumors, brain infections, and other conditions of the brain(87) • Damage to the white matter of the left hemisphere of the brain is associated with language impairment; damage to the left arcuate fasciculus is common in patients with aphasia(130) › Pathogenesis: Each subtype of aphasia is associated with a brain lesion in a specific location • Broca’s aphasia/nonfluent aphasia: lesions of the frontal lobe of the left hemisphere; usually involving the third frontal convolution of the left hemisphere(18,98) • Wernicke’s aphasia/fluent aphasia: lesions in the left hemisphere in the posterior portion of the first temporal gyrus(98) • Global aphasia: extensive damage to the left hemisphere; sometimes bilateral damage(98) • Anomic aphasia: angular gyrus(98) • Transcortical motor aphasia: supplementary motor areas; superior or anterior to the pars opercularis(18,98) • Transcortical sensory aphasia: parieto-occipital lesion with spared preopercularparieto-temporal language areas; also documented with lesions of the posterior thalamus(18) • Conduction aphasia: parietal operculum or posterior superior temporal gyrus(98) • In a study of 31 patients with aphasia conducted in the United States, lesions on the following five areas of the brain were,most frequently,associated with aphasia: inferior frontal gyrus, inferior parietal region, superior/middle temporal lobe, insula, and basal ganglia(32) • In a study conducted in South Korea with 25 patients with aphasia following left hemisphere stroke, researchers used diffusion tensor tractography to examine the status of the left arcuate fasciculus (the part of the brain that connects Broca’s and Wernicke’s areas) in each patient. Researchers reported the following findings: –There was a significant, moderate positive correlation between aphasia quotient (AQ; ranges from 0 to 100 and is a representation of the severity of the patient’s aphasia; language is considered normal if the AQ is 93.8 or higher) and the voxel number of the left arcuate fasciculus. A voxel in diffusion tensor tractography represents functioning brain tissue; hence, the more voxels, or intact brain tissue of the left arcuate fasciculus, the milder the patient’s aphasia(117) –Poorer AQ scores were associated with discontinuation of the integrity of the left arcuate fasciculus(117) • In a study conducted in Poland with 30 subjects with aphasia, researchers found that impaired temporal information processing was associated with poor performance on assessments of both receptive and expressive language abilities(129) › Risk factors • Stroke –Advanced age (risk doubles each decade after age 55 years; peak incidence at 80–84 years of age)(2) –Sex (higher risk in women than men)(2) - Use of birth control pills and pregnancy can further increase the risk of stroke in women(2) –Family history of stroke(2) –History of stroke, heart attack, or transient ischemic attack (TIA)(2) –Cigarette smoking(2) –Hypertension(2) –Diabetes mellitus(2) –Carotid or another artery disease (including peripheral artery disease)(2) –Excess weight(2) –Hyperlipidemia(2) –Physical inactivity(2) –Alcohol and/or drug abuse(2) –Atrial fibrillation or another heart disease(2) –Sickle cell disease(2) –Poor diet high in fat(2) –Geographical location (in the United States, strokes are more common in the Southeast)(2) –Socioeconomic factors (there is some evidence that strokes are more common among persons of low income)(2) –For detailed information on assessment and treatment of patients following stroke, see Clinical Review…Stroke Rehabilitation: Speech Therapy; CINAHL Topic ID Number: T708774 • Traumatic brain injury (TBI) –Age - Children, especially the newborns to the age of 4 years(81) - Teenagers and young adults, especially between the ages of 15 and 24 years(81) - Adults over 75 years(81) –Male sex(81) –For detailed information on assessment and treatment of patients following TBI, see the series of Clinical Reviews on this topic • Brain tumor –Exposure to ionizing radiation(80) –Family history of brain tumor(80) –For detailed information on assessment and treatment of patients with brain tumor, see Clinical Review…Brain Tumors: Adult – Speech Therapy; CINAHL Topic ID Number: T708860 and Clinical Review…Brain Tumors in Childhood: Speech Therapy; CINAHL Topic ID Number: T708892 Examination › Contraindications/precautions to examination • Depression and anxiety are common among persons with aphasia and can adversely affect test performance, making patients seem more impaired than they are(16) • During a speech-language evaluation, it is of utmost importance to be aware of a patient’s tolerance level to pain and of frustration. The time of day and the number of previous evaluations can affect the patient’s alertness and performance. A patient’s culture and native language should also be considered to determine the appropriateness of examination questions and materials –The patient’s culture will shape his or her experience with aphasia. For example, in cultures where language binds the family and community together, aphasia could be devastating. However, in a culture that values silence or emphasizes on nonverbal communication or, the effects of aphasia will be experienced differently. It is essential that the clinician determine how aphasia is viewed and understood by the patient and family’s culture and proceed with the assessment, treatment, and education with that cultural perspective at the forefront(83) –In a survey-based study conducted in Australia with 188 responding speech-language pathologists (SLPs), researchers found that although the SLPs embraced a wide variety of therapeutic techniques and functional practices in both inpatient and outpatient settings, they also reported an overall low level of comfort and knowledge in treating culturally and lingually diverse patients with aphasia.(96) Appropriate education, training, and materials are critical for SLPs who work with individuals in culturally and lingually diverse populations • Patients with aphasia might not be able to complete standardized tests or answer questions regarding medical history. It recommended that the caregiver/family be involved in all assessment procedures › History • History of present illness/injury –Mechanism of injury or etiology of illness: What is the underlying cause of aphasia (e.g., stroke, TBI)? - What were the initial signs and symptoms of aphasia? Have any symptoms improved or worsened since onset? –Course of treatment - Medications for current illness/injury: Obtain a comprehensive list of medications prescribed and/or being taken (including over-the-counter drugs). The concurrent use of multiple medications is common among older adults with complex medical conditions, and the side effects of these medications can adversely affect cognitive and communicative functioning.(4) Contact a pharmacist or physician regarding questions about side effects(4) - Diagnostic tests completed: Note the results of any neurological (MRI, CT scan), blood, laboratory, neuropsychological, or psychological/cognitive tests - Home remedies/alternative therapies: Document any use and efficacy of home training programs or alternative therapies (e.g., acupuncture) - Previous therapy: Document whether the patient has had speech-language, occupational, or physical therapy for this or other conditions and what specific treatments were helpful or not helpful –Aggravating/easing factors - Are there times of the day when the patient has more/less difficulty communicating? - Are there specific situations in which it is more/less difficult for the patient to communicate? - Is the patient aware of the difficulties in communication? Is the patient frustrated by the difficulties in communication? - Sessions with an SLP might be more frustrating than conversations with significant others and family members at home.(120) During both evaluation and therapy sessions with a patient with aphasia and word-findingdifficulties, SLPs are less likely to give the patient help and will allow the patient to struggle to find the word independently more often than family members(120) - Does the patient suffer from a mood disorder (e.g., depression) that can affect motivation to communicate?(4) –Body chart: Use body chart to document location and nature of symptoms –Nature of symptoms: Document the nature of speech and language symptoms; symptoms will vary with the subtype of aphasia - See Presentation/signs and symptoms, above, for details on symptoms associated with specific subtypes of aphasia –Other symptoms: Document other symptoms the patient is experiencing that could exacerbate the condition and/or symptoms. Examples include depression, physical impairments, dysphagia, apraxia, overall health status, and vision deficits - Although the prevalence of pain in a patient with aphasia is reported to range from 43.8–87.5%,authors of a systematic review of pain and pain assessments in people with post-stroke aphasia found that there are no feasible, reliable, and valid assessments for pain assessment in patients with aphasia(133) –Respiratory status: Note respiratory status - Does the patient require supplemental oxygen? Tracheostomy tube, nasal cannula, or breathing mask? - Does the patient become short of breath? If so, when? Standing? Walking? With exercise? –Psychosocial status: Patients with aphasia often report feeling a loss of “self” or identity.(107) Depression and anxiety are common among persons with aphasia.(16) SLPs should be knowledgeable of symptoms of depression (e.g., loss of interest in daily activities, problems sleeping, feelings of sadness and hopelessness) and refer to a neuropsychologist or a clinical psychologist when signs are present.(4) Many depression scales and psychological scales have been used to assess patients who have had a stroke. The SLP can collaborate with the psychologist to determine the evaluation that is appropriate for the patient’s language abilities.(16) Some examples include: - Hospital Anxiety and Depression Scale (HADS) (mild aphasia)(16) - Depression Intensity Scale Circles (DISC) (moderate aphasia)(16) - Stroke Aphasic Depression Questionnaire (severe aphasia – to be completed by a caregiver)(16) - Visual Analogue Self-Esteem Scale(17) –Hearing: Document hearing ability - The prevalence of hearing loss is no higher in patients with aphasia than in the general population; however, the impact of a hearing loss is potentially greater for a patient with aphasia because of an impaired language system. Patients with both aphasia and hearing loss must be diagnosed accurately and treated with appropriate hearing aids to ensure that aphasia rehabilitation is as effective as possible(90) - Does the patient have a known hearing loss? If so, does he or she wear hearing aids? Left, right, or bilateral? - Refer to an audiologist for full audiological evaluation if hearing impairment is suspected –Barriers to learning - Are there any barriers to learning? Yes__ No__ - If Yes, describe _______________________ • Medical history –Medical history - History of same/similar diagnosis: Document any previous history of aphasia, a communication disorder, or cognitive deficits - Comorbid diagnoses: Refer to medical charts and ask patient or patient’s family about other problems, including hearing loss, vision deficits, diabetes, cancer, heart disease, and psychiatric disorders - Medications previously prescribed: Obtain a comprehensive list of medications prescribed and/or being taken (including over-the-counter drugs) • Social/occupational history –Patient’s goals: Document what the patient and the patient’s caregiver/family hope to accomplish with therapy and in general –Vocation/avocation and associated repetitive behaviors, if any - A patient/caregiver interview can be helpful to gain insight into the patient’s hobbies, family/community roles, interests, prior work status, and home responsibilities - What activities and hobbies does the patient enjoy? - Does the patient participate in any language-based hobbies? - Does the patient work? - Does the patient regularly use a computer/telephone? –Functional limitations/assistance with ADLs/adaptive equipment - Document if the patient uses any adaptive equipment to communicate (e.g., pen/paper) - Note if the patient wears hearing aids or glasses - If used, determine if hearing aids are in a working order and the glasses are the correct and current prescription - Note if the patient uses any devices to assist with mobility (e.g., walker, wheelchair) –Living environment:Number of stairs, and floors in the home, with whom the patient lives (e.g., caregivers, family members), and language(s) that the patient uses in the home - Does the patient speak another language? If yes: - Obtain information about the order of acquisition of each language and language history (e.g., language used in education)(85) - Which language is used in different situations (e.g., work, home, with relatives, with friends)?(85) - What modalities are used in each language (e.g., reading, speaking, writing)?(85) - Premorbid proficiency in each language can be compared to present proficiency using a 7-pointscale (e.g., 1 = not fluent, 7 = native proficiency)(29) › Relevant tests and measures: (While tests and measures are listed in alphabetical order, sequencing should be appropriate to patient medical condition, functional status, and setting.)Comprehensive evaluation of speech, language, and swallowing ability should determine the subtype and severity of the aphasia and coexisting impairments.(3) Standardized assessments of aphasia often include tests of confrontation naming; a spontaneous/conversational speech sample; repetition of digits, single words, multisyllabic words, and sentences of increasing length and complexity; a measure of comprehension of spoken language (single words, yes-no questions, following simple to complex commands); word retrieval measures; reading and reading comprehension (letters, single words, phrases, sentences, paragraphs); and writing (to dictation and spontaneously)(98) • Arousal, attention, cognition (including memory, problem-solving): Examination of cognitive, nonlinguistic impairment is standard during the evaluation of aphasia. In a study conducted in the Netherlands with 147 patients with acute aphasia, 88% of these patients had cognitive, nonlinguistic impairment in at least one domain at3 months post stroke; this percentage decreased to 80% at 1 year poststroke.(30) Psychological and cognitive evaluations can assist in informing the course of treatment and providing a prognosis for therapy. Measures of episodic memory should be administered if dementia is suspected. Working memory and selective attention are often impaired in patients with aphasia, especially for tasks involving spoken language.(21,122) Note that scores on tests that involve verbal responses might not be valid for patients with aphasia. Cognitive tests include: –Mini-Mental State Examination (MMSE) (36): To assess the cognitive status of adults. Sections include: Orientation to Time, Orientation to Place, Registration, Attention and Calculation, Recall, Naming, Repetition, Comprehension, Reading, Writing, Drawing –Wechsler Adult Intelligence Scale (WAIS):(111) To assess intellectual and cognitive abilities of adults –For patients with severe cognitive impairment, referral to neuropsychology is appropriate for extensive assessment and input regarding cognitive intervention • Assistive and adaptive devices: Assess the need for and ability to use augmentative and alternative communication (AAC). AAC for patients with aphasia can range from simple, low-tech options (e.g., pen and paper, pointing gestures) to complex, individualized high-tech options (e.g., speech-generating device or iPad).(51,69,118)Incorporate AAC into both evaluation and treatment session for patients who use or will use these methods to communicate on a daily basis –Multimodal Communication Screening Task for Persons with Aphasia (MCST-A) (39): Measures skills required to use AAC systems and strategies. Consists of 8 sections designed to assess communication tasks, including selecting pictorial symbols, telling a story by pointing to photos, choosing pictures to complete a daily transaction (e.g., buying medicine at a drugstore), and providing information about places by pointing to locations on a map - For detailed information on assessment for and treatment using AAC with patients with aphasia, seeClinical Review… Augmentative and Alternative Communication: Aphasia; CINAHL Topic ID Number:T709145 • Speech and language examination: When selecting tests for communication assessment, clinicians must consider the cultural and linguistic background of the patient and determine if the measurement was standardized on the relevant population.(4) Tests that have normative information on diverse groups should be used when possible(4) –Speech: A motor speech evaluation should be performed to identify or rule out coexisting apraxia and/or dysarthria - Apraxia commonly co-occurs in patients with Broca’s aphasia(5) - For detailed information on the assessment and treatment of apraxia, see Clinical Review…Apraxia of Speech (Acquired), referenced above. For detailed information on assessment and treatment of dysarthria (spastic, flaccid, ataxic, hypokinetic, and hyperkinetic), see the series of Clinical Reviews on dysarthria –Language: Standardized tests assess components of expressive and receptive language that are affected by aphasia, including naming, word finding, auditory comprehension, reading, and writing. Many tests determine the severity of aphasia, distinguish the type of aphasia, and guide remediation - Samples of spontaneous spoken language elicited from patients with aphasia can be highly variable from day to day; to determine the best picture of a patient’s functioning, take samples of his or her spoken language over several sessions to establish an accurate baseline measure(19) - Patients with aphasia sometimes rely on visual cues from pictures, facial expressions, letters, or other visual stimuli to assist with the auditory comprehension and/or word-finding, making them seem less impaired than they are.(40,99)Assess a patient’s expressive and receptive language skills with and without visual support to determine if there is a difference in accuracy(99) - Observe the patient’s language abilities in several contexts (e.g., telling a story about his or her own life, re-telling a popular fairy tale or fable, answering open-ended questions, answering specific fact-based questions). When the patient is speaking, observe and document the patient’s gestures.(123) Patients with semantically dense gestures (e.g., pantomiming how one makes a sandwich with accurate hand shapes and appropriate sequencing) likely have adequate underlying semantic knowledge. Patients who do not produce these types of contextual gestures and instead use pointing or other generic hand movements when supplementing verbal content may have impairment of semantic knowledge.(123)Determine if the patient’s spoken language is aided by gestures as this can be a target for therapy - Standardized language tests for aphasia include: - Boston Diagnostic Aphasia Examination – 3 (BDAE-3):(42,98) Assesses different modalities of language (auditory, visual, gesture) and processing functions - Pyramids and Palm Trees Test(53): Assesses a person's ability to access detailed semantic representations from words and pictures - Psycholinguistic Assessment of Language Processing in Aphasia (PALPA) (10,57): Assesses components of language structure such as orthography and phonology, word and picture semantics, and morphology and syntax - Neurosensory Center Comprehensive Examination for Aphasia (NCCEA) (98): A comprehensive assessment of language comprehension and production and also reading and writing - Western Aphasia Battery-R(60,98): To assess oral language (verbal fluency, language information content, comprehension, repetition, and naming), nonverbal language, and reading and writing. Contains a screening measure (Bedside WAB-R) - Main Concept Analysis (MCA): an assessment developed for assessment of oral conversation abilities for Cantonese speakers with aphasia; developed with culturally appropriate pictures for Cantonese speakers living in the Western and Eastern parts of the world. The MCA has been reported to be externally valid in multiple studies(128) - Taiwanese Mandarin Main Concept Analysis (TM-MCA): an assessment based on the MCA developed for Taiwanese Mandarin speakers; a culturally appropriate standardized assessment for Taiwanese Mandarin speakers with aphasia(128) –Voice: Briefly assess vocal function, including vocal quality, loudness, pitch, and endurance; if there are specific concerns regarding voice, refer to an otolaryngologist for a complete workup to rule out laryngeal pathologies before completing a full evaluation –Reading/writing: Assess reading and writing skills as part of a complete evaluation of aphasia.(74,98)Portions of standardized tests for aphasia provide standardized tests of both reading and writing - Determine the extent to which a patient with aphasia comprehends what is read, especially if reading and writing will be used as part of the patient’s AAC.(119) Reading ability of a patient with aphasia should be assessed hierarchically, beginning with the ability to recognize individual letters and moving on to word reading, phrase reading, sentence reading, and paragraph level reading. The semantic content (i.e., complexity) of a reading passage must also be considered.(119) Reading ability will be affected by the severity of aphasia and overall language impairment and also the cognitive abilities, including memory and executive functioning(119) • Oral structure and oral motor function: Complete a full oral mechanism exam. Assess lingual, labial, and velar strength, range of motion (ROM), coordination, and rate; patients with aphasia can also have dysarthria. Please see the series of Clinical Reviews on dysarthria for detailed information • Perception: Vision and hearing screening should always precede screening for aphasia. An audiologist should check for impacted cerumen before pure-tone audiometric screening and word recognition testing.(4) Informal assessment of vision is required if patient intends to support communication with visual methods (e.g., writing, gestures, pictures) –Even when patients with aphasia have intact hearing ability as judged by an audiological evaluation, impaired perception of the phonetic dimensions of speech can significantly affect the auditory comprehension(48) - Providing the patient with visual cues (such as speech reading) can improve the ability to perceive the phonetic dimensions of spoken language(48) –Researchers who conducted a study in the United States conducted a two-part study on rhythm processing in patients with aphasia.(116) Sometimes rhythm or tapping patterns are used as part of an intervention program for aphasia (e.g., verbal pacing strategies, melodic intonation therapy [MIT]). In the first part of the study, participants included 16 patients with aphasia (various subtypes) and 15 neurologically intact age-matched adults. Researchers found that the patients with aphasia had a reduced ability to discriminate between two rhythmic patterns, greater variability when tapping along with a rhythm, and reduced accuracy in tapping a rhythm from memory as compared to the control adults. As a group, the patients with aphasia had poorer rhythm processing than the control adults; however, not all patients with aphasia displayed rhythm processing deficits. In part two of the study, participants included 14 patients with aphasia (various types) and 16 neurologically intact age-matched adults. Researchers compared the auditory discrimination ability (for pitch and rhythm of both speech and tones) between the two groups and found that the group with aphasia performed worse than the control group overall. Detailed analysis of the data showed that the group with aphasia had a relative difficulty with rhythm processing versus pitch processing.(117) If the treating SLP is planning to use tapping strategies or rhythmic patterns as part of aphasia therapy (e.g., compensatory strategies for apraxia, melodic intonation therapy), rhythm processing should be assessed before creating the plan of care • Special tests specific to diagnosis –Quality of life: Aphasia will likely have a significant impact on an individual’s quality of life and ability to participate in social activities.(91) To assess the quality of life and functional outcomes, the SLP can administer quality of life scales, social participation indices, or ratings of communicative effectiveness(26,98,102) - Factors that affect the quality of life in patients with aphasia include relationships, social activities, psychosocial well-being, mobility, home, health, helplessness, and independence(26) - In a study in the United States of quality of life in 24 patients with aphasia, researchers found that physical functioning, not communication ability, was the greatest contributing factor in these patients’ overall health-related quality of life(24) - Determining the factors that influence an individual patient’s quality of life the most can assist with the development of appropriate goals in speech-language therapy(24) - In a study in Canada, researchers examined which factors facilitated or hindered social participation of 17 participants with chronic aphasia. Factors that facilitated participation were: (1) personality factors (e.g., determination, perseverance, motivation); (2) having family and friends who were well-adjusted to their aphasia and were available to help; (3) having opportunities for social participation through their community aphasia organization; (4) their satisfaction with rehabilitation services; (5) their ability to perform activities; and (6) tolerance of and positive attitude towards strangers. Factors that hindered social participation were: (1) the extent of their own physical or communication limits; (2) limited family/friend relationships or poorly adjusted family and friends; (3) personality factors (e.g., pride, fear, avoidance); (4) a lack of community services; and (5) ignorance in the public regarding aphasia(71) - When selecting tests, clinicians must consider the patient’s level of awareness and cultural and linguistic background(4) - Tests that have normative information on diverse groups should be used when possible(4) - Examples of quality of life scales for patients with aphasia include: - Aphasia Quality of Life Scale – 39 (SAQOL-39):An instrument designed for assessing health-related quality of life in patients who have had a stroke and also have aphasia(24) - In a study conducted in India, researchers translated the SAQOL-39 into Hindi and administered it to 84 Hindi-speaking patients with aphasia. In addition to being translated, the scale was further adapted by 6 Hindi-speaking SLPs from central and northern India to be socioculturally acceptable. With adaptations, the SAQOL-39 was found to have a high test-retestreliability and high internal consistency in Hindi for Hindi-speaking people with aphasia(127) - Quality of Communication Life (QCL): An instrument that measures the quality of one’s communication life as a distinct but related aspect of general quality of life(24) - Assessment for Living with Aphasia Toolkit (ALA) – Second Edition: a pictographic, self-report measure of aphasia-relatedquality-of-life based on the World Health Organization’s International Classification of Functioning, Disability and Health (ICF). In a research study conducted in the United States with 101 individuals with aphasia, researchers reported that the ALA was easy to administer and encapsulated key aspects of the experience of living with aphasia. Statistical analysis indicated that the ALA had acceptable test-retestreliability, internal consistency, and construct validity(101) –Bilingual assessment (as indicated) - Bilingual Aphasia Test (BAT) (88): Assesses the bilingual patient’s ability to use each language in different settings by a language use history questionnaire. A computer program is available to evaluate responses in more than 100 different languages - Other assessments have been adapted and standardized for Spanish speakers (e.g., BDAE, WAB-R, PALPA) - For detailed information on assessment of bilingual adults with aphasia, see Clinical Review…Language Disorders: Aphasia in Bilingual Adults; CINAHL Topic ID Number: T708880 –Functional communication and needs assessment (98) : Assessment of functional communication in patients with aphasia is necessary because a specific patient’s actual use of language in everyday, functional situations might not correspond to the degree of severity as measured by standardized language assessments.(98) Tests that assess pragmatic skills and communication used in daily living (e.g., calling for help, exchanging greetings, responding to yes/no questions) include: - Functional Communication Profile-Revised (FCP-R) (64,98): An assessment, rating, and inventory of the patient’s functional communication skills (e.g., sign, nonverbal, augmentative) - Communicative Activities of Daily Living-2(CADL-2) (50,98): Assessment of the following subtests of communication: Reading, Writing, and Using Numbers; Social Interaction; Divergent Communication; Contextual Communication; Nonverbal Communication; Sequential Relationships; and Humor/Metaphor Absurdity - Functional Assessment of Communication Skills for Adults (ASHA-FACS) (35,98): Assessment of functional communication in four areas: social communication; communication of basic needs; reading, writing, and number concepts; and daily planning - Communicative Effectiveness Index(73): Measure of change in functional communicative ability. Assesses four domains: Basic Need, Health Threat, Life Skill, and Social Need - Aphasia Needs Assessment(14): Assesses patient’s interests and situations in which the patient has difficulty communicating • Swallow examination: Complete a screen of the patient’s swallowing abilities; if indicated, complete a full evaluation of swallowing –Swallowing difficulties (dysphagia) are common among patients who have aphasia –For detailed information on assessment and treatment of dysphagia, see the Clinical Reviews on this topic • Tracheostomy examination: If present, assess tracheostomy tube and document date of placement, current respiratory status, and use of the speaking valve. For detailed information on assessment of patients with tracheostomies, seeClinical Review…Dysphagia: Adults with Tracheostomy; CINAHL Topic ID Number:T709084 and see Clinical Review… Dysphagia: Children with Tracheostomy; CINAHL Topic ID Number: T709082.For detailed information on assessment of a tracheostomy tube and use of a speaking valve, see Clinical Review…Passy-MuirTracheostomy & Ventilator Swallowing and Speaking Valve; CINAHL Topic ID Number: T708919 Assessment/Plan of Care › Contraindications/precautions • Only those contraindications/precautions applicable to this diagnosis are mentioned below, including with regard to modalities. Rehabilitation professionals should always use their professional judgment • Patients with this diagnosis are at risk for falls; follow facility protocols for fall prevention and post-fall prevention instructions at bedside, if inpatient. Ensure that patient and family/caregivers are aware of the potential for falls and educated about fall prevention strategies. Discharge criteria should include independence with fall prevention strategies • The relative benefits and risks of intensive therapy should be evaluated for each individual. Individual therapy for patients with aphasia often includes stimulus-response tasks focused on language modalities such as oral expression, auditory comprehension, and reading and writing. Treatment gains on these tasks can be documented clearly; however, it is more difficult to achieve and measure generalization of these skills and document the gains in functional communication • To ensure the relevance and appropriateness of treatment programs, decisions about goals and course of therapy should be made in collaboration with the patient, the caregivers/family, and other healthcare professionals.(100) Cultural background, language preference, occupation (if relevant), and patient interests must also be considered(100) • Treatment goals and objectives will shift with the recovery of the patient. It is recommended that outcome measures include assessment of functional communication(98,102) • Patients with aphasia are also at risk for swallowing and feeding difficulties. Ensure that the patient and family/ caregivers are aware of potential aspiration risks and educated about strategies when appropriate • Clinicians should follow the guidelines of their clinic/hospital and what is ordered by the patient’s physician. The summary below is meant to serve as a guide, not to replace orders from a physician or a clinic’s specific protocols › Diagnosis/need for treatment: The clinical diagnosis, to diagnose the subtype and severity of aphasia, is made collaboratively with information from the patient’s family and other professionals (e.g., physician, neuropsychologist, OT, SLP, PT) using a combination of measures, including CT scan, MRI, and standardized aphasia assessments.(3) Although the SLP delivers direct treatment of communication impairments in patients with poststroke aphasia, the best outcomes for patients occur when the patient is treated by a multidisciplinary team(135) › Rule out • Aphasia should be differentiated from primary progressive dementia and Alzheimer’s disease (AD)(11) • Speech disorders such as dysarthria and apraxia should be distinguished from a language deficit(67) • Diagnoses that must be ruled out in the differential diagnosis for aphasia include: –Confusion/delirium(67) –Depression(98) –Echolalia(67) –Neurogenic stuttering(67) –Palilalia (echoing, or repetition of one's own words)(67) –Schizophrenia(67) –Selective mutism(67) › Prognosis • The size and site of the brain lesion influence the course of recovery(7) –The neural reorganization is thought to contribute to the recovery of both language and motor skills in individuals with brain damage. In aphasia, fMRI studies have indicated that language processing after brain damage includes involvement of undamaged brain tissue in the language center of the brain (i.e., left hemisphere) as well as the right hemisphere homologs(113) –In addition to the neural reorganization, neural plasticity is thought to contribute to language recovery post stroke. Authors of a study conducted in the United States with 8 participants with chronic aphasia reported normalization of the inferior longitudinal fasciculus on a diffusion MRI following 3 weeks of intensive, group, constraint-inducedlanguage therapy. Also after the therapy, this normalization was associated with significant improvements in naming(134) • Psychological factors such as depression, premorbid personality, fatigue, and paranoia affect the prognosis(98) • Authors of a literature review of 23 treatment studies indicated that patients may make better progress when they receive the therapy in the chronic period of aphasia (more than 1-year post onset of aphasia)(84) • Complete recovery from aphasia is rare(7,98) –If complete recovery occurs, it generally happens within a matter of hours or days following onset as the underlying cause of the aphasia is treated and resolves(98) –Once aphasia has persisted for several weeks or months, it is unlikely that the premorbid communication skills will return(98) - At this point, the primary goal might be to improve the patient’s ability to use residual verbal skills in conjunction with contextual cues and nonverbal means to achieve effective communication in social situations(7) - Because complete recovery from aphasia is unlikely, discharge from speech-language therapy is often a complex issue,because sometimes the patients/families do not feel ready for the discharge(46) - Ensuring that discharge criteria and the subject of eventual discharge are discussed openly and honestly with the patient and family from the time of the initial evaluation can ease the transition out of long-term speech-languagetherapy when the patient is discharged(46) • In a study conducted in the United States of improvement in aphasia scores in the first 90 days poststroke, researchers found that initial severity accurately predicted recovery for patients with mild to moderate aphasia in those first 3 months(70) • In a longitudinal study conducted in the United Kingdom, researchers compared the relative outcomes of patients with different types of aphasia and found that patients with Broca’s aphasia improved more on the WAB-R than those with Wernicke’s aphasia during the first year of recovery(7) • In a study conducted in France with 338 patients with stroke and treated with thrombolysis (medications that break down blood clots), researchers found that the patients with aphasia following stroke experienced significantly better recovery (as long as there were no motor deficits in the extremities)(114) › Referral to other disciplines • Refer to occupational therapy for upper extremity impairment, training for activities of daily living (ADLs), and/or visual disturbances, if indicated • Refer to physical therapy for strengthening, endurance exercises, and/or balance and gait training, if indicated • Refer to a psychologist or counselor for depression or anxiety • Referral to a dietitian if the patient has any feeding or swallowing difficulties and may be at risk for malnutrition; the patient may require supplements or supplemental feedings • Refer to vocational counseling for assistance in reentering the workforce • Referral to audiology if the patient appears to have hearing loss • Referral to neuropsychology for significant cognitive impairment • Referral to ophthalmology or neuro-ophthalmology for assessment and treatment of visual disturbances › Other considerations • Aphasia therapy can be provided in individual and group sessions –Group treatment is effective in facilitating functional communication in a natural and social setting, providing a support network for patients, and assisting with the generalization of communication skills(6,77) –Group therapy has been reported to help alleviate some of the social isolation that is frequently associated with aphasia.(107,121) In addition to providing an opportunity for socialization, patients with aphasia who participate in therapy groups have reported additional psychosocial benefits such as feeling a sense of hope and encouragement, having the chance to feel connected to a community, and getting the opportunity to laugh(121) • In the early post-onset period, the SLP is sometimes involved in a supportive role rather than in a direct therapy role by(76): –Providing information to the family regarding the communication deficit –Educating other treatment team members on how to best communicate with the patient –Preventing the development of struggle behaviors that will negatively influence the patient’s ability to communicate • In a study conducted in Australia, researchers found that use of a standardized, prescribed very early aphasia direct therapy regimen (45 to 60 minutes per day for 20 sessions) resulted in significantly greater language recovery at both 4 to 5 weeks poststroke and 6months poststroke. In this study, there were two groups of patients, experimental (who received the very early aphasia rehabilitation as soon as possible after a stroke, mean of 6.1 days post-stroke) and a historical control group from a previous study. There were patients in this study in both groups with mild to severe aphasia of varying types. At the conclusion of the study, the researchers controlled for the variables of initial aphasia and stroke disability and found that participants who underwent the very early aphasia rehabilitation achieved 18% higher score on the Aphasia Quotient (AQ) and 1.5% higher scores on the Discourse Analysis (DA) compared to the historical control cohort. At 6 months postintervention, the experimental participants maintained a 16% higher score on the AQ and 0.6% (not statistically significant)higher score on the DA over the control group(41) • In a pilot study conducted in Italy with 12 patients who had mild-moderate aphasia poststroke, researchers randomly assigned these patients to the experimental group (daily therapy for 2 weeks beginning an average of 2.2 days post-stroke) or no therapy. The patients in the experimental group performed significantly better than the control group in naming, writing, and reading aloud as measured by the Aachen Aphasia Test (AAT) after the study. Additionally, researchers performed fMRI scans before and after therapy and found significantly increased activation of the left inferior frontal gyrus for the treatment group(79) • Direct therapy should consider the patient’s interests, health status, and occupation (if relevant) and the patient’s and caregiver’s goals and contextual factors (patient’s living environment, work environment)(76,100) › Treatment summary: Treatment goals, assessment approaches, and documentation practices vary considerably among therapists treating patients with aphasia.(102) The primary purpose of aphasia therapy is to improve communication with the goal of increasing participation in daily activities and enhancing the quality of life. Intervention should consider patient interests, patient and caregiver goals, and contextual factors.(102) Treatment has been categorized as two types: 1) restitutive (treatment to restore lost language function), and 2) substitutive (treatment to develop compensatory strategies to replace impaired function).(62,112) The substitutive treatment approach is based on the assumption that some impaired processes are irremediable.(112) Due to the individualized nature of treatment and the ethical issues regarding a “no treatment” control group in treatment studies involving subjects with aphasia, the methodological quality of current aphasia research is modest; most studies are not well controlled(108) • Authors of a systematic review that included randomized controlled trials (RCTs) for aphasia therapy up to the year 2009, authors found that speech-language therapy for persons with aphasia following stroke is effective(58) –Authors noted consistency in the results that supported intensive speech-language therapy versus conventional speech-language therapy(58) - Significantly more patients withdrew from intensive programs as compared to the conventional programs(58) –Additionally, when a therapist-trained/supervised volunteer facilitated speech-language therapy, the therapy appeared to be as effective as when delivered by an SLP(58) –There was not enough evidence to support the effectiveness of one speech-language therapy approach over another(58) • The author of a meta-analysis of 55 multiple subject studies found that the average effect size for recovery of treated patients with aphasia in the acute period was nearly double that of the recovery of untreated patients (e.g., treated recovery vs. spontaneous recovery).(93) These findings confirmed the results of an earlier, smaller meta-analysis (N = 21) by the same author(94) • In a study conducted in the United States involving 5 patients with moderate to profound word-finding deficits, fMRI scans were taken immediately pre- and post-treatment(25) –The treatment involved initiating picture-naming trials with the complex left-hand movement of opening a box and pushing a button(25) –Four of the 5 patients improved in naming abilities during the treatment; the patients who improved during this treatment demonstrated a significant shift in laterality toward the frontal lobe of the right hemisphere(25) • Authors of a review of pharmacological treatments for post-strokeaphasia advocated for more research on the effects of intensive speech-language therapy in conjunction with pharmacological agents. The following are some of the recently investigated pharmacological treatments(13): –Piracetam: Authors of a meta-analysis and systematic review of RCTs for aphasia in post-stroke patients found that piracetam did not improve the overall severity of aphasia; however, significant improvement was noted in written language abilities(103) –Bromocriptine/dexamphetamine: These drugs act on the catecholamine systems and have shown varying efficacy in case-series, open-label studies, and placebo-controlledtrials. Bromocriptine has been shown to be effective in patients with nonfluent aphasia with reduced initiation of output(13) - In a case-study with a 58-year-old female patient with nonfluent aphasia, researchers provided speech-language therapy alone and then in combination with bromocriptine. Outcome measures were performed at the following times: (1) at baseline before the drug was administered; (2) once the drug reached 30 mg dosage; (3) after the combined speech-language therapy and drug regimen; and (4) after drug and therapy withdrawal. The patient made some measurable improvements on bromocriptine without therapy; however, when she began combined speech-language therapy and bromocriptine,she showed significant improvements in standardized testing and overall behavior/verbal output. Researchers noted that these gains were maintained after the patient stopped taking the drug(38) –Donepezil: Donepezil acts on the cholinergic system and has shown promise in patients with chronic post-stroke aphasia in single-case-series, case-series, and an open-labelstudy(13) • Authors of another review of 10 pharmacological RCTs with persons with aphasia concluded that there was weak evidence that piracetam improved language recovery and that researchers should further examine the harmful effects as well as the long-term effects of pharmacological treatment. The reviewers could not conclude if drug therapy is more effective than speech-language therapy or if one drug is more effective than another(43) • For bilingual patients with aphasia, there is preliminary evidence that treatment in the nondominant language might better facilitate cross-linguistic generalization than treatment in the dominant language(29) –For detailed information on the treatment of bilingual adults with aphasia, see Clinical Review…Language Disorders: Aphasia in Bilingual Adults, referenced above • Treatments described in studies that have included patients with different subtypes of aphasia –Group therapy: Group therapy can include pragmatic objectives such as improving the ability to convey a message and initiating conversational exchanges. Also, group therapy may provide support for the patient, provide information about aphasia, and increase the patient’s confidence in communicative situations - The effects of group therapy on participants with chronic aphasia were investigated in an RCT conducted in the United States with two groups, immediate treatment and delayed treatment(31) - An SLP provided group therapy for 5 hours/week (2.5 hour periods/2 days a week) for 4 months. The control group participated in social activities (support, performance, movement groups) to control for the effects of social interaction. The first part of group therapy involved discussions of interest for the patients. Information exchange was facilitated by communicative drawing, role-playing, natural gestures, maps, pictures, personal notebooks, conversational prompting, and scripting. A break for refreshments included family members. The last part of the group session was spent wrapping up the initial discussion or talking about news events - Dependent measures included standardized tests: WAB AQ, CADL, SPICA. Results indicated that the immediate treatment group had significantly higher scores on the measures compared to the group not receiving treatment. Within-group performance revealed significant increases after 2 months of treatment and after 4 months of treatment. No significant decline occurred 1 month post-treatment(31) - In a small study conducted in the United States with 5 patients with aphasia, both fluent and nonfluent subtypes, researchers found significantly greater improved communication on the Aphasia Diagnostic Profile’s Alternative Communication subtest following 2 individual sessions and 6 sessions of group therapy when compared with a control group of 5 patients who received 8 individual sessions of speech therapy(77) –Supported conversation/conversation partner training - In a single-blind RCT conducted in Canada, researchers investigated the effects of training of volunteers (N = 40) on the conversational interaction of patients with aphasia(56) - Training included a 1-day workshop and 1.5 hours of hands-on experience to teach volunteers topics such as keeping the talk natural and avoiding being patronizing. They were also taught to ensure comprehension of the patient and use techniques such as gesturing, drawing, pictographic resources, and writing keywords - Measures were researcher-developed and designed to assess the skill of the conversational partner in “acknowledging and revealing the competence of adults with aphasia.” Another researcher-developedmeasure assessed the level of interaction of the patient - Trained volunteers scored higher than untrained volunteers on ratings of acknowledging competence and revealing competence. Persons with aphasia showed a change in social and message exchange skills(56) - An intervention study conducted in Denmark with 31 nurses supported the use of direct training of Supported Conversation for Adults with aphasia (SCA) for improving communication between nursing staff and patients with aphasia(75) –Promoting Aphasic’s Communicative Awareness (PACE) has been described as a functional therapy approach that promotes more realistic conversations to assist patients with aphasia to improve their communicative skills.(27) Some features of PACE include a free choice of communicative modality (gesture, speech), equal opportunity for the patient and the therapist to send and receive messages, the use of novel (rather than known) information, and natural feedback used to figure out the sender’s message. The patient and therapist take turns communicating the content represented on a picture card. Picture cards are drawn from a stack so that only the “message sender" knows the content (novel information). The turn ends when the message is conveyed successfully. The clinician’s role is to model effective communicative behaviors that are within the patient’s capacity and to give the patient opportunities for successful communication. Other conversational partners (spouse) can take part in therapy to learn strategies - Although several treatment studies have examined the efficacy of PACE, the evidence is mixed due to methodological reasons (e.g., use of a modified version of PACE, comparison with an unequal type of treatment, lack of control of other factors influencing recovery)(20,27) –Semantic Feature Analysis (SFA) therapy for naming impairments(132) - A treatment for naming deficits in patients with aphasia - The patient is presented with a target picture in the center of a chart and asked to name it; regardless of whether or not the patient can name the picture, he or she is then asked to identify semantic features of the target item such as: - What does it look like? - How is it used? Why is it used? - To which category does it belong? - What are other items associated with it? - What is an opposite item/concept? - SFA can help in training people to self-cue for word-finding strategies when they encounter word-finding deficits in real life situations - Authors of a systematic literature review of SFA, the found that SFA is an effective treatment for people with aphasia. There were 21 studies included in the review with 55 total subjects,and the results indicated that the treatment was effective despite having a variety of methodologies and variations to the treatment protocol(132) –Phonological Components Analysis (PCA) treatment for naming impairments(72) - A treatment for naming deficits in patients with aphasia; modeled on the framework of SFA therapy(72) - The patient is presented with a target picture in the center of a chart and asked to name it; regardless of whether or not the patient can name the picture, he or she is then asked to identify five phonological aspects about the target item(72): - What does this rhyme with? - What sound does it start with? - What other word starts with the same sound? - What sound does it end with? - How many beats (syllables) does the word have? - In a single-subject, multiple baseline study conducted in Australia with 10 participants with various types of aphasia (Broca’s, mixed, anomic, nonfluent, Wernicke’s), each participant took part in PCA sessions 3 times per week for 1 hour for a maximum of 15 sessions(72) - According to outcome measures, 7 out of 10 participants improved in naming ability; these naming improvements were maintained on follow-upmeasures 4 weeks after treatment concluded(72) - Generalization to untreated items was observed for 3 of the 7 improved patients(72) –Picture-naming therapy(22) - Preliminary evidence suggests that picture-namingtherapy (for both nouns and verbs) in patients with various subtypes of aphasia can be generalize to improved connected speech(22) - In a study conducted in the United Kingdom involving 7 patients with various subtypes and severity of aphasia, researchers found that after 5 weeks, 2 sessions per week, confrontation naming ability improved in all participants; additionally, some participants showed improved verbal output for picture-supported narratives; the least amount of improvement was found on spontaneous/unsupportive narrative generation(22) –Bilingual patients with aphasia: For bilingual patients with aphasia, there is preliminary evidence that treatment in the nondominant language may better facilitate cross-linguisticgeneralization than treatment in the dominant language(29) - For detailed information on the assessment and treatment of bilingual adults with aphasia, seeClinical Review… Language Disorders: Aphasia in Bilingual Adults, referenced above –AAC - An AAC needs assessment must be performed to determine the patient’s ability to use AAC and to identify the most appropriate type of AAC(14) - AAC options include picture boards, symbol sets, paper tablets, communication notebooks with customized phrases, remnant books, photographs, written words, alphabet cards (for self-cueing), and voice output devices(14) - For detailed information on the assessment and treatment for AAC with patients with aphasia, seeClinical Review… Augmentative and Alternative Communication: Aphasia, referenced above –Adjunct brain stimulation - Transcranial direct current stimulation (tDCS)(126) - Involves constant, low-intensity current being passed through two electrodes placed on the head. There are two types of stimulation with tDCS: anodal stimulation and cathodal stimulation. Anodal stimulation is used to excite neuronal activity, and cathodal stimulation inhibits or reduces neuronal activity(126) - Authors of a Cochrane systematic review including 12 clinical trials that compared tDCS to sham tDCS as an adjunct to speech therapy reported low-quality evidence and concluded that there is no evidence to support the effectiveness of any tDCS in improving the outcomes of speech therapy in patients with aphasia following stroke(126) - Repetitive transcranial magnetic stimulation (rTMS): rTMS allows for painless, noninvasive stimulation of the brain with low-frequency magnetic fields to create electrical currents in specific regions of the brain(45,78) - Applying rTMS to a specific part of the brain in the undamaged hemisphere can suppress the inhibitory process of that area and allow for the reactivation of some areas within the damaged hemisphere, thereby promoting functional recovery(78) - In several small research studies, combining rTMS with traditional speech therapy has been associated with significantly greater improvement in language recovery compared to speech therapy alone.(45,78,125) Although showing initial promise in research studies, rTMS is in the early stages of the investigation and is not widely available for clinical use as a treatment for aphasia • Treatment approaches targeting specific subtypes of aphasia –Broca’s aphasia - Linguistic treatment(8) - Treatment of Underlying Forms (TUF) is a meta-linguistic therapy approach found to increase verbal production of grammatically intact sentences in patients with agrammatic aphasia(105,106) - Constraint-Induced Aphasia Therapy (CIAT) is based on the principles of Constraint-Induced Movement Therapy (CIMT) for motor rehabilitation following stroke(89,104) - Principles of CIAT include: - Constraint: not allowing the patient to use compensatory strategies for communication (e.g., drawing, writing, gesturing)(104) - Forced use: forcing the use of speech during communicative exchanges(104) - Massed practice: participating in therapy in high, concentrated doses (such as 2 to 4 hours per day, 4 to 5 days per week)(89,104) - For detailed information on CIAT, see Clinical Review…Aphasia: Constraint-Induced Language Therapy; Number: T902529 - Melodic Intonation Therapy (MIT): MIT involves a hierarchically structured treatment program that focuses on practice in speaking with exaggerated prosody.(12,52) For detailed information on MIT, see Clinical Review…Aphasia, Broca's (Nonfluent Aphasia), referenced above - Functional communication training - Reduced Syntax Therapy (REST): Therapy that focuses on training German- and English-speakingpatients with agrammatic aphasia to produce simple utterances with a reduced syntactic structure; also referred to as elliptical style (such as “I…pill” or “man…angry”)(97) - For detailed information on the treatment for Broca’s aphasia, see Clinical Review…Aphasia, Broca’s (Nonfluent Aphasia), referenced above –Wernicke’s aphasia - CIAT(68,89) - Therapy to decrease perseveration; increasing naming ability(9) - Therapy for short-term memory (e.g., recalling sentences of increasing length)(33,65) - Situational therapy with a gesture: Situational therapy consists of training the patient to use gesture and other means of nonverbal communication in daily situations (e.g., going to the grocery store)(1) - For detailed information on the treatment for Wernicke’s aphasia, see Clinical Review…Aphasia, Wernicke’s (Receptive Aphasia, Fluent Aphasia), referenced above –Global aphasia - Computer-based Visual Input Communication (C-VIC):The C-VIC sentence production training program is a computer-based program that involves learning a specific iconic vocabulary to produce sentences/phrases for communication(82) - AAC(49,54) - For detailed information on the treatment for global aphasia, see Clinical Review…Aphasia, Global, referenced above –Anomic aphasia - SFA(15,62,110) - Complexity Account of Treatment Efficacy (CATE): A semantically based approach in which training of words proceeds from complex to simple items (e.g., atypical to typical: ostrich vs. robin)(61,62,63) - Phonemic cues to facilitate oral naming(28,44,59,95,109) - Patients with anomic aphasia are better able to produce a word after hearing the initial phoneme; the goal of this approach is for the patient to eventually self-generate phonemic cues - Spaced Retrieval (SR): A memory intervention designed to facilitate recall of words over progressively longer intervals of time(37) - For detailed information on the treatment for anomic aphasia, see Clinical Review…Anomia Associated with Aphasia, referenced above –Transcortical motor aphasia - Movement training to increase verbal initiations(92) - For detailed information on the treatment for transcortical motor aphasia, see Clinical Review…Aphasia, Transcortical Motor, referenced above –Transcortical sensory aphasia - For detailed information on the treatment for transcortical sensory aphasia, see Clinical Review…Aphasia, Transcortical Sensory, referenced above –Conduction aphasia - Case studies have described treatments to improve cognitive, rather than language, skills (e.g., attention, memory) in patients with conduction aphasia; however, there is little evidence that treatment generalizes to functional communication and untrained functions(65,86) - Therapy to improve verbal repetition(66) - Self-monitoring and speech production therapy(23,34) - For detailed information on the treatment for conduction aphasia, see Clinical Review…Aphasia, Conduction, referenced above . Problem Goal Intervention Expected Progression Home Program Broca’s aphasia Increase fluency of speech; increase naming abilities; improve the grammatical construction of the verbal output Functional training _ Linguistic treatment _ _ CIAT _ _ MIT _ _ REST _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Wernicke’s aphasia Increase auditory comprehension; reduce perseveration in fluent speech; increase awareness of deficits; increase the communicative value of the verbal output Functional training _ CIAT _ _ Therapy to decrease perseveration _ _ Therapy for short-term memory _ _ Situational therapy with a gesture _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Global aphasia Provide the patient with Functional training a form of functional _ communication C-VIC _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Anomic aphasia Increase naming Functional training abilities; improve word- _ finding SFA _ _ CATE _ _ Phonemic cues to facilitate oral naming _ _ SR _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Transcortical motor aphasia Increase spontaneous speech; improve naming abilities; increase fluency of speech Functional training _ Movement training to increase verbal initiations _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Transcortical sensory aphasia Improve auditory comprehension, semantic jargon, improve naming abilities Functional training _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Conduction aphasia Reduce paraphasias in connected speech; improve repetition Functional training _ Cognitive therapy _ _ Therapy to improve verbal repetition _ _ Self-monitoring and speech production therapy _ _ Group therapy _ _ Supported conversation _ _ PACE _ _ PCA _ _ Picture-naming therapy _ _ Prescription, application of devices and equipment _ AAC _ _ See Treatment summary, above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Apraxia (if present) Increase fluency of speech; increase verbal output; increase spontaneous speech; improve speech intelligibility Apraxia therapy _ For detailed information on the assessment and treatment of apraxia, see Clinical Review… Apraxia of Speech, Acquired, referenced above Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Dysarthria (if present) Improve speech intelligibility Dysarthria therapy _ For detailed information on assessment and treatment of dysarthria, see the series of Clinical Reviews on dysarthria (including spastic, flaccid, ataxic, hypokinetic, and hyperkinetic) Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Acquired dyslexia (if present) Improve reading ability Dyslexia therapy _ For detailed information on assessment and treatment of acquired dyslexia, see the series of Clinical Reviews on dyslexia Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Acquired agraphia (if present) Improve written language skills Agraphia therapy _ For detailed information on assessment and treatment of acquired dyslexia, see Clinical Review… Agraphia: Speech Therapy;CINAHL Topic ID Number: T708854 Progression of therapy Home program will tasks will depend vary with respect to the on the goals of the goals of the patient patient; when shortterm goals are met, SLP will determine the appropriate progression of goals Dysphagia (if present) Increase swallow safety; improve nutritional intake; improve secretion management Dysphagia therapy _ Therapy will vary according to the results of a swallow evaluation. Treatment can include strategies for airway protection, strategies for facilitating the oral phase of swallowing, and dietary adjustments _ _ For detailed information on treatment of dysphagia, see the series of Clinical Reviews on this topic Progression of Home program will dysphagia therapy will vary with respect to the vary according to the goals of the patient results of a swallowing evaluation, carefully progressing the patient to more difficult food and liquid textures as swallowing improves . Desired Outcomes/Outcome Measures › Improved quality of life(26,98,102) • SAQOL-39 • QCL • ALA › Community reintegration(98) › Effective external modifications(102) › Family education regarding aphasia and communicating more effectively with the patient(102) › Improved language ability › Improved functional communication ability(98,102) • FCP-R • CADL-2 • ASHA-FACS • Communicative Effectiveness Index • Aphasia Needs Assessment • Aphasia Communication Outcome Measure (ACOM)(124) –A 59-item patient-reported outcome (PRO) measure that appears reliable and valid for patients with aphasia(124) –The author of the test has created a free software application for the ACOM that can be used to administer and score the test(124) • Therapy Outcome Measure (TOM)(47) –A tool developed to assess outcome in each dimension of the World Health Organization (WHO) classification: impairment, activity, participation, well-being(47) –In a study conducted in the United Kingdom, researchers found that the TOM was an effective outcome measure of functional communication for assessment of conversational speech for patients with aphasia and/or dysarthria(47) › Increased communication with external support(102) › Increased independence(102) › Increased participation in social, vocational, and avocational activities(98,102) Maintenance or Prevention › Clinic-based treatment should eventually be transferred to home-basedroutines so that the patient and caregivers can continue treatment independently Patient Education › Patient and partner education should include information about the effects of aphasia, treatment options, and the prognosis. When possible, the partner or patient’s family should be educated about facilitative techniques to use when assisting the patient with communication › All the educational information and consent forms for therapy, presented the patient, should be in “aphasia-friendly” format, which might include pictures, large print text, simplified language, or limited amount of text per page(55) › See “Aphasia” from the National Institute on Deafness and Other Communication Disorders athttps://www.nidcd.nih.gov/ health/aphasia › See NINDS Aphasia Information Page from the National Institute of Neurological Disorders and Stroke athttps://www.ninds.nih.gov/Disorders/All-Disorders/Aphasia-Information-Page › See “Aphasia” from the American Speech-Language-Hearing Association at https://www.asha.org/public/speech/disorders/ Aphasia.htm › See information and support network: Hope Aphasia Hope Network of the Aphasia Hope Foundation at http:// aphasiahope.wpengine.com/ › See “Aphasia: Frequently Asked Questions” from the National Aphasia Association at https://www.aphasia.org/aphasia-faqs/ Coding Matrix References are rated using the following codes, listed in order of strength: M Published meta-analysis SR Published systematic or integrative literature review RCT Published research (randomized controlled trial) R Published research (not randomized controlled trial) RV Published review of the literature PP Policies, procedures, protocols RU Published research utilization report X Practice exemplars, stories, opinions QI Published quality improvement report GI General or background information/texts/reports L Legislation C Case histories, case studies PGR Published government report G Published guidelines PFR Published funded report U Unpublished research, reviews, poster presentations or other such materials CP Conference proceedings, abstracts, presentation References 1. Altschuler EL, Multari A, Hirstein W, Ramachandran VS. Situational therapy for Wernicke's aphasia. Med Hypotheses. 2006;67(4):713-716. (X) 2. American Heart Association. Stroke risk factors. http://www.strokeassociation.org/STROKEORG/AboutStroke/UnderstandingRisk/Understanding-Risk_UCM_308539_SubHomePage.jsp. Accessed February 14, 2017. (GI) 3. American Speech-Language-Hearing Association. Aphasia. American Speech-Language-Hearing Association Web site. http://www.asha.org/public/speech/disorders/ Aphasia.htm. Accessed February 14, 2017. (GI) 4. American Speech-Language Hearing Association. Dementia. American Speech-Language-Hearing Association Web site. http://www.asha.org/Practice-Portal/Clinical-Topics/Dementia/. Accessed February 14, 2017. (G) 5. Ardila A. A proposed reinterpretation and reclassification of aphasic syndromes. Aphasiology. 2010;24(3):363-394. (RV) 6. Ashley J, Duggan M, Sutcliffe N. Speech, language, and swallowing disorders in the older adult. Clin Geriatr Med. 2006;22(2):291-310. (GI) 7. Bakheit AMO, Shaw S, Carrington S, Griffiths S. The rate and extent of improvement with therapy from the different types of aphasia in the first year after stroke. Clin Rehabil. 2007;21(10):941-949. (R) 8. Ballard KJ, Thompson CK. Treatment and generalization of complex sentence production in agrammatism. J Speech Lang Hear Res. 1999;42(3):690-707. (R) 9. Basso A. Perseveration or the Tower of Babel. Semin Speech Lang. 2004;25(4):375-389. (R) 10. Bate S, Kay J, Code C, Haslam C, Hallowell B. Eighteen years on: What next for the PALPA?. Int J Speech Lang Pathol. 2010;12(3):190-202. (RV) 11. Bayles KA, Boone DR, Tomoeda CK, Slauson TJ, Kazniak AW. Differentiating Alzheimer's patients from the normal elderly and stroke patients with aphasia. J Speech Hear Disord. 1989;54(1):74-87. (R) 12. Belin P, Van Eeckhout P, Zilbovicius M. Recovery from nonfluent aphasia after melodic intonation therapy: a PET study. Neurology. 1996;47(6):1504-1511. (R) 13. Berthier ML. Poststroke aphasia: epidemiology, pathophysiology and treatment. Drugs Aging. 2005;22(2):163-182. (RV) 14. Beukelman DR, Garrett KL. Aphasia Needs Assessment. http://cehs.unl.edu/documents/secd/aac/assessment/aphasianeeds.pdf. Published 2006. Accessed February 14, 2017. (PP) 15. Boyle M. Semantic feature analysis treatment for anomia in two fluent aphasia syndromes. Am J Speech Lang Pathol. 2004;13(3):236-249. (R) 16. Brumfitt S. Psychosocial aspects of aphasia: speech and language therapists' views on professional practice. Disabil Rehabil. 2006;28(8):523-534. (R) 17. Brumfitt SM, Sheeran P. The development and validation of the Visual Analogue Self-Esteem Scale (VASES). Br J Clin Psychol. 1999;38(Pt 4):387-400. (R) 18. Brust JCM. Aphasia, apraxia, and agnosia. In: Gonzalez EG, Myers SJ, Edelstein JE, Lieberman JS, Downey JA, eds. Downey and Darling's Physiological Basis of Rehabilitation Medicine. 3rd ed. Boston, MA: Butterworth Heinemann; 2001:711-719. (GI) 19. Cameron RM, Wambaugh JL, Mauszycki SC. Individual variability on discourse measures over repeated sampling times in persons with aphasia. Aphasiology. 2010;24(6-8):671-684. (R) 20. Carlomagno S. Pragmatic Approaches to Aphasia Therapy: Promoting Aphasics’ Communicative Effectiveness. San Diego, CA: Singular Pub. Group; 1994. (GI) 21. Christensen SC, Wright HH. Verbal and non-verbal working memory in aphasia: What three n-back tasks reveal. Aphasiology. 2010;24(6-8):752-762. (R) 22. Conroy P, Sage K, Ralph ML. Improved vocabulary production after naming therapy in aphasia: can gains in picture naming generalize to connected speech?. Int J Lang Commun Disord. 2009;44(6):1036-1062. (R) 23. Corsten S, Mende M, Cholewa J, Huber W. Treatment of input and output phonology in aphasia: a single case study. Aphasiology. 2007;21(6-8):587-603. (C) 24. Cranfill TB, Wright HH. Importance of health-related quality of life for persons with aphasia, their significant others, and SLPs: Who do we ask?. Aphasiology. 2010;24(6-8):957-968. (R) 25. Crosson B, Moore AB, McGregor KM. Regional changes in word-production laterality after a naming treatment designed to produce a rightward shift in frontal activity. Brain Lang. 2009;111(2):73-85. (R) 26. Cruice M, Hill R, Worrall L, Hickson L. Conceptualising quality of life for older people with aphasia. Aphasiology. 2010;24(3):327-347. (R) 27. Davis GA. PACE revisited. Aphasiology. 2005;19(1):21-38. (RV) 28. del Toro CM, Altmann LJP, Raymer AM, Leon S, Blonder LX, Gonzalez Rothi LJ. Changes in aphasic discourse after contrasting treatments for anomia. Aphasiology. 2008;22(7-8):881-892. (R) 29. Edmonds LA, Kiran S. Effect of semantic naming treatment on crosslinguistic generalization in bilingual aphasia. J Speech Lang Hear Res. 2006;49(4):729-748. (R) 30. El Hachioui H, Visch-Brink EG, Lingsma HF, et al. Nonlinguistic cognitive impairment in poststroke aphasia: a prospective study. Neurorehabil Neural Repair. 2014;28(3):273-281. doi:10.1177/1545968313508467. (R) 31. Elman RJ, Bernstein-Ellis E. The efficacy of group communication treatment in adults with chronic aphasia. J Speech Lang Hear Res. 1999;42(2):411-419. (RCT) 32. Faroqi-Shah Y, Solomon T, Liu J, Park S, Allen GB. Lesion analysis of language production deficits in aphasia. Aphasiology. 2014;28(3):258-277. (R) 33. Francis DR, Clark N, Humphreys GW. The treatment of an auditory working memory deficit and the implications for sentence comprehension abilities in mild "receptive" aphasia. Aphasiology. 2003;17(8):723-750. (C) 34. Franklin S, Buerk F, Howard D. Generalised improvement in speech production for a subject with reproduction conduction aphasia. Aphasiology. 2002;16(10-11):1087-1114. (C) 35. Frattali C; American Speech and Hearing Association. Functional Assessment of Communication Skills for Adults (ASHA FACS). Rockville, MD: ASHA; 1995. (PP) 36. Folstein MF, Folstein SE, McHugh PR, Fanjiang G. Mini-Mental State Examination. Odessa, FL: Psychological Corporation; 2001. (PP) 37. Fridriksson J, Holland AL, Beeson P, Morrow L. Spaced retrieval treatment in anomia. Aphasiology. 2005;19(2):99-109. (R) 38. Galling MA, Goorah N, Berthier ML, Sage K. A clinical study of the combined use of bromocriptine and speech and language therapy in the treatment of a person with aphasia. Aphasiology. 2014;28(2):171-187. (R) 39. Garrett KL, Lasker J. The Multimodal Communication Screening Task for persons with Aphasia (MCST-A). University of Nebraska-Lincoln College of Education and Human Sciences Web site Web site. http://cehs.unl.edu/aac/aphasia-assessment-materials/. Accessed February 14, 2017. (PP) 40. Gillen G. Cerebrovascular accident/stroke. In: Pendleton HM, Schultz-Krohn W, eds. Pedretti's Occupational Therapy: Practical Skills for Physical Dysfunction. 8th ed. St. Louis, MO: Mosby Elsevier; 2018:827-830. (GI) 41. Godecke E, Ciccone NA, Granger AS, et al. A comparison of aphasia therapy outcomes before and after a Very Early Rehabilitation programme following stroke. Int J Lang Commun Disord. 2014;49(2):149-161. doi:10.1111/1460-6984.12074. (R) 42. Goodglass H, Kaplan E, Barresi B. Boston Diagnostic Aphasia Examination-3. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. (PP) 43. Greener J, Enderby P, Whurr R. Pharmacological treatment for aphasia following stroke. Cochrane Database Syst Rev. 2001:4. Art No: CD000424. doi:10.1002/14651858.CD000424. (SR) 44. Greenwood A, Grassly J, Hickin J, Best W. Phonological and orthographic cueing therapy: a case of generalised improvement. Aphasiology. 2010;24(9):991-1016. (C) 45. Hamilton RH, Sanders L, Benson J. Stimulating conversation: enhancement of elicited propositional speech in a patient with chronic non-fluent aphasia following transcranial magnetic stimulation. Brain Lang. 2010;113(1):45-50. (C) 46. Hersh D, Cruice M. Beginning to teach the end: the importance of including discharge from aphasia therapy in the curriculum. Int J Lang Commun Disord. 2010;45(3):263-274. (C) 47. Hesketh A, Long A, Patchick E, Lee J, Bowen A. The reliability of rating conversation as a measure of functional communication after stroke. Aphasiology. 2008;22(9):970-984. (R) 48. Hessler D, Jonkers R, Bastiaanse R. The influence of phonetic dimensions on aphasic speech perception. Clin Linguist Phon. 2010;24(12):980-996. (R) 49. Ho KM, Weiss SJ, Garrett KL, Lloyd LL. The effect of remnant and pictographic books on the communicative interaction of individuals with global aphasia. Augment Altern Commun. 2005;21(3):218-232. (R) 50. Holland A, Frattali CM, Fromm D. Communicative Abilities in Daily Living-2 (CADL-2). Austin, TX: Pro-Ed; 1999. (PP) 51. Hoover EL, Carney A. Integrating the iPad into an intensive, comprehensive aphasia program. Semin Speech Lang. February 2014;35(1):25-37. doi:10.1055/s-0033-1362990. (R) 52. Hough MS. Melodic intonation therapy and aphasia: another variation on a theme. Aphasiology. 2010;24(6-8):775-786. (C) 53. Howard D, Patterson K. Pyramids and Palm Trees Test. London: Harcourt Assessment; 1992. (PP) 54. Jacobs B, Drew R, Ogletree BT, Pierce K. Augmentative and alternative communication (AAC) for adults with severe aphasia: where we stand and how we can go further. Disabil Rehabil. 2004;26(21-22):1231-1240. (RV) 55. Jayes M, Palmer R. Initial evaluation of the Consent Support Tool: a structured procedure to facilitate the inclusion and engagement of people with aphasia in the informed consent process. Int J Speech Lang Pathol. April 16, 2014;16(2):159-168. doi:10.3109/17549507.2013.795999. (R) 56. Kagan A, Black SE, Duchan FJ, Simmons-Mackie N, Square P. Training volunteers as conversation partners using "Supported Conversation with Adults with Aphasia" (SCA): a controlled trial. J Speech Lang Hear Res. 2001;44(3):624-638. (RCT) 57. Kay J, Lesser R, Coltheart M. Psycholinguistic Assessments of Language Processing in Aphasia. Hove, UK: Lawrence Erlbaum Associates. Ltd; 1992. (PP) 58. Kelly H, Brady MC, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2010;5. Art No: CD000425. doi:10.1002/14651858.CD000425. (SR) 59. Kendall DL, Rosenbek JC, Heilman KM. Phoneme-based rehabilitation of anomia in aphasia. Brain Lang. 2008;105(1):1-17. (R) 60. Kertesz A, Raven JC. Western Aphasia Battery-Revised. San Antonio, TX: Pearson; 2006. (PP) 61. Kiran S. Typicality of inanimate category exemplars in aphasia treatment: further evidence for the semantic complexity. J Speech Lang Hear Res. 2008;51(6):1550-1568. (R) 62. Kiran S, Bassetto G. Evaluating the effectiveness of semantic-based treatment for naming deficits in aphasia: what works?. Semin Speech Lang. 2008;29(1):71-82. (RV) 63. Kiran S, Thompson CK. The role of semantic complexity in treatment of naming deficits: training semantic categories in fluent aphasia by controlling exemplar typicality. J Speech Lang Hear Res. 2003;46(3):608-622. (R) 64. Kleiman LI. Functional Communication Profile-Revised. East Moline, IL: LinguiSystems; 2003. (PP) 65. Koenig-Bruhin M, Studer-Eichenberger F. Therapy of short-term memory disorders in fluent aphasia: a single case study. Aphasiology. 2007;21(5):448-458. (C) 66. Kohn SE, Smith KL, Arsenault JK. The remediation of conduction aphasia via sentence repetition: a case study. Br J Disord Commun. 1990;25(1):45-60. (C) 67. Kortte JH, Palmer JB. Speech and language disorders. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2015:833-838. (GI) 68. Kurland J, Baldwin K, Tauer C. Treatment-induced neuroplasticity following intensive naming therapy in a case of chronic Wernicke's aphasia. Aphasiology. 2010;24(6-8):737-751. (C) 69. Kurland J, Wilkins AR, Stokes P. iPractice: piloting the effectiveness of a tablet-based home practice program in aphasia treatment. Semin Speech Lang. February 2014;35(1):51-63. doi:10.1055/s-0033-1362991. (R) 70. Lazar RM, Minzer B, Antoniello D, Festa JR, Krakauer JW, Marshall RS. Improvement in aphasia scores after stroke is well predicted by initial severity. Stroke. 2010;41(7):1485-1488. (R) 71. Le Dorze G, Salois-Bellerose E, Alepins M, Croteau C, Hallé M. A description of the personal and environmental determinants of participation several years post-stroke according to the views of people who have aphasia. Aphasiology. 2014;28(4):421-439. (R) 72. Leonard C, Rochon E, Laird L. Treating naming impairments in aphasia: findings from a phonological components analysis treatment. Aphasiology. 2008;22(9):923-947. (R) 73. Lomas J, Pickard L, Bester S, Elbard H, Finlayson A, Zoghaib C. The Communicative Effectiveness Index: development and psychometric evaluation of a functional communication measure for adult aphasia. J Speech Hear Disord. 1989;54(1):113-124. (R) 74. Lynch KE, Damico JS, Damico HL, Tetnowski J. Reading skills in an individual with aphasia: the usefulness of meaning-based clinical applications. Asia Pac J Speech Lang Hear. 2009;12(3):221-234. (C) 75. Jensen LR, Løvholt AP, Sørensen IR, et al. Implementation of supported conversation for communication between nursing staff and in-hospital patients with aphasia. Aphasiology. 2015;29(1):57-80. doi:doi:10.1080/02687038.2014.955708. (R) 76. Marshall RC. Aphasia treatment in the early postonset period: managing our resources effectively. Am J Speech Lang Pathol. 1997;6(1):5-21. (X) 77. Marshall RS, Wallace TJ. The effect of combined individual and group treatment on functional communication in aphasia after acquired brain injury. Med Speech Lang Pathol. 2009;17(3):111-124. (R) 78. Martin PI, Naeser MA, Ho M. Overt naming fMRI pre- and post-TMS: Two nonfluent aphasia patients, with and without improved naming post-TMS. Brain Lang. 2009;111(1):20-35. (R) 79. Mattioli F, Ambrosi C, Mascaro L, et al. Early aphasia rehabilitation is associated with functional reactivation of the left inferior frontal gyrus: a pilot study. Stroke. 2014;45(2):545-552. doi:10.1161/STROKEAHA.113.003192. (R) 80. Mayo Clinic staff. Brain tumor. MayoClinic.com Web site. http://www.mayoclinic.org/diseases-conditions/brain-tumor/symptoms-causes/dxc-20117134. Accessed February 14, 2017. (GI) 81. Mayo Clinic Staff. Traumatic brain injury. MayoClinic.com website. Web site. http://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/basics/risk-factors/con-20029302. Accessed February 14, 2017. (GI) 82. McCall D, Shelton JR, Weinrich M, Cox D. The utility of computerized visual communication for improving natural language in chronic global aphasia: implications for approaches to treatment in global aphasia. Aphasiology. 2000;14(8):795-826. (R) 83. McLellan KM, McCann CM, Worrall LE, Harwood MLN. “For Mori, language is precious. And without it we are a bit lost”: Mori experiences of aphasia. Aphasiology. 2014;28(4):453-470. (R) 84. Moss A, Nicholas M. Language rehabilitation in chronic aphasia and time postonset: a review of single-subject data. Stroke. 2006;37(12):3043-3051. (SR) 85. Muñoz ML, Marquardt TP, Copeland G. A comparison of the codeswitching patterns of aphasic and neurologically normal bilingual speakers of English and Spanish. Brain Lang. 1999;66(2):249-274. (R) 86. Murray LL, Keeton RJ, Karcher L. Treating attention in mild aphasia: evaluation of attention process training-II. J Commun Disord. 2006;39(1):37-61. (C) 87. National Institute on Deafness and Other Communication Disorders. Aphasia. http://www.nidcd.nih.gov/health/voice/pages/aphasia.aspx. Accessed February 14, 2017. (GI) 88. Paradis M, Libben G. The Assessment of Bilingual Aphasia. Hillsdale, NJ: Lawrence Erlbaum Associates; 1987. (PP) 89. Pulvermuller F, Berthier ML. Aphasia therapy on a neuroscience basis. Aphasiology. 2008;22(6):563-599. (RV) 90. Rankin E, Newton C, Parker A, Bruce C. Hearing loss and auditory processing ability in people with aphasia. Aphasiology. May 2014;28(5):576-595. (R) 91. Rautakoski P. Communication style before and after aphasia: a study among Finnish population. Aphasiology. 2014;28(3):359-376. (R) 92. Raymer AM, Rowland L, Haley M, Crosson B. Nonsymbolic movement training to improve sentence generation in transcortical motor aphasia: a case study. Aphasiology. 2002;16(4-6):493-506. (C) 93. Robey RR. A meta-analysis of clinical outcomes in the treatment of aphasia. J Speech Lang Hear Res. 1998;41(1):172-187. (M) 94. Robey RR. The efficacy of treatment for aphasic persons: a meta-analysis. Brain Lang. 1994;47(4):585-608. (M) 95. Rochon E, Leonard C, Burianova H. Neural changes after phonological treatment for anomia: an fMRI study. Brain Lang. 2010;114(3):164-179. (R) 96. Rose M, Ferguson A, Power E, Togher L, Worrall L. Aphasia rehabilitation in Australia: current practices, challenges and future directions. Int J Speech Lang Pathol. 2014;16(2):169-180. doi:10.3109/17549507.2013.794474. (R) 97. Ruiter MB, Kolk HH, Rietveld TC. Speaking in ellipses: the effect of a compensatory style of speech on functional communication in chronic agrammatism. Neuropsychol Rehabil. 2010;20(3):423-458. (R) 98. Sarno MT, Galgano J. Neurogenic disorders of speech and language. In: O'Sullivan SB, Schmitz TJ, Fulk GR, eds. Physical Rehabilitation. 6th ed. Philadelphia: FA Davis Company; 2014:1266-1293. (GI) 99. Silkes JP, Rogers MA. Perception of visually masked stimuli by individuals with aphasia: A methodological assessment and preliminary theoretical implications. Aphasiology. 2010;24(6-8):763-774. (R) 100. Simmons-Mackie N, Kagan A. Application of the ICF in aphasia. Semin Speech Lang. 2007;28(4):244-253. (G) 101. Simmons-Mackie N, Kagan A, Victor JC, et al. The assessment for living with aphasia: reliability and construct validity. Int J Speech Lang Pathol. 2014;16(1):82-94. doi:10.3109/17549507.2013.831484. (R) 102. Simmons-Mackie N, Threats TT, Kagan A. Outcome assessment in aphasia: a survey. J Commun Disord. 2005;38(1):1-27. (R) 103. Zhang J, Wei R, Chen Z, Luo B. Piracetam for Aphasia in Post-stroke Patients: A Systematic Review and Meta-analysis of Randomized Controlled Trials. CNS Drugs. July 2016;30(7):575-587. doi:10.1007/s40263-016-0348-1. (GI) 104. Thompson CK, Choy JJ, Holland A, Cole R. Sentactics®: Computer-Automated Treatment of Underlying Forms. Aphasiology. 2010;24(10):1242-1266. (R) 105. Thompson CK, Shapiro LP. Complexity in treatment of syntactic deficits. Am J Speech Lang Pathol. 2007;30-42. (R) 106. Thompson CK, Shapiro LP. Treating agrammatic aphasia within a linguistic framework: Treatment of Underlying Forms. Aphasiology. 2005;19(10-11):1021-1036. (R) 107. Thompson J, McKeever M. The impact of stroke aphasia on health and well-being and appropriate nursing interventions: an exploration using the Theory of Human Scale Development. J Clin Nurs. 2014;23(3-4):410-420. doi:10.1111/j.1365-2702.2012.04237.x. (R) 108. Togher L, Schultz R, Tate R. The methodological quality of aphasia therapy research. Aphasiology. 2009;23(6):694-706. (SR) 109. Vitali P, Tettamanti M, Abutalebi J. Generalization of the effects of phonological training for anomia using structural equation modelling: a multiple single-case study. Neurocase. 2010;16(2):93-105. (R) 110. Wambaugh JL, Ferguson M. Application of semantic feature analysis to retrieval of action names in aphasia. J Rehabil Res Dev. 2007;44(3):381-394. (R) 111. Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. San Antonio, TX: The Psychological Corporation; 1997. (PP) 112. Whitworth A, Webster J, Howard D. A Cognitive Neuropsychological Approach to Assessment and Intervention in Aphasia. New York: Psychology Press; 2005. (GI) 113. Sandberg C, Kiran S. Analysis of abstract and concrete word processing in persons with aphasia and age-matched neurologically healthy adults using fMRI. Neurocase. August 2014;20(4):361-88. doi:10.1080/13554794.2013.770881. (R) 114. Denier C, Flamand-Roze C, Dib F, et al. Aphasia in stroke patients: early outcome following thrombolysis. Aphasiology. 2015;29(4):442-456. doi:10.1080/02687038.2014.971220. (R) 115. Rodrigues IT, Castro-Caldas A. Aphasia with recurring utterances: Old syndrome, new perspectives. Aphasiology. 2014;1350-1363. doi:10.1080/02687038.2014.921884. (R) 116. Zipse L, Worek A, Guarino AJ, Shattuck-Hufnagel S. Tapped out: do people with aphasia have rhythm processing deficits? J Speech Lang Hear Res. December 2014;57(6):2234-45. doi:10.1044/2014_JSLHR-L-13-0309. (R) 117. Tak HJ, Hang SH. Relation between aphasia and arcuate fasciculus in chronic stroke patients. BMC Neurol. March 8, 2014;14:46. doi:10.1186/1471-2377-14-46. (R) 118. Klippi A. Conversation and aphasia: Advances in analysis and intervention. Pointing as an embodied practice in aphasic interaction. Aphasiology. 2015;29(3):337-354. (R) 119. Chesneau S, Ska B. Text comprehension in residual aphasia after basic-level linguistic recovery: a multiple case study. Aphasiology. 2015;29(2):237-256. doi:10.1080/02687038.2014.971098. (R) 120. Laakso M. Collaborative participation in aphasic word searching: comparison between significant others and speech and language therapists. Aphasiology. 2015;29(3):269-290. doi:10.1080/02687038.2013.878450. (R) 121. Rotherham A, Howe T, Tillard G. “We just thought that this was Christmas”: Perceived benefits of participating in aphasia, stroke, and other groups. Aphasiology. 2015;29(8):965-982. doi:10.1080/02687038.2015.1016887. (R) 122. Pompn RH, McNeil MR, Spencer KA, Kendall DL. Intentional and reactive inhibition during spoken-word stroop task performance in people with aphasia. J Speech Lang Hear Res. 2015;58(3):767-780. doi:10.1044/2015_JSLHR-L-14-0063. (R) 123. Pritchard M, Dipper L, Morgan G, Cocks N. Language and iconic gesture use in procedural discourse by speakers with aphasia. Aphasiology. 2015;29(7):826-844. (R) 124. Hula WD, Doyle PJ, Stone CA, et al. The Aphasia Communication Outcome Measure (ACOM): Dimensionality, item bank calibration, and initial validation. J Speech Lang Hear Res. 2015;58(3):906-919. doi:10.1044/2015_JSLHR-L-14-0235. (R) 125. Yoon TH, Han SJ, Yoon TS, Kim JS, Yi TI. Therapeutic effect of repetitive magnetic stimulation combined with speech and language therapy in post-stroke non-fluent aphasia. NeuroRehabilitation. 2015;36(1):107-114. doi:10.3233/NRE-141198. (R) 126. Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving aphasia in patients with aphasia after stroke. Cochrane Database Syst Rev. 2015;5. Art No: CD009760. doi:10.1002/14651858.CD009760.pub3. (R) 127. Mitra IH, Krishnan G. Adaptation and validation of stroke-aphasia quality of life (SAQOL-39) scale to Hindi. Ann Indian Acad Neurol. 2015;18(1):29-32. (G) 128. Kong AP, Yeh CC. A Taiwanese Mandarin Main Concept Analysis (TM-MCA) for quantification of aphasic oral discourse. Int J Lang Commun Disord. September 2015;50(5):580-592. doi:10.1111/1460-6984.12157. (R) 129. Oron A, Szymaszek A, Szelag E. Temporal information processing as a basis for auditory comprehension: clinical evidence from aphasic patients. Int J Lang Commun Disord. September 2015;50(5):604-615. doi:10.1111/1460-6984.12160. (R) 130. Geva S, Correia MM, Warburton EA. Contributions of bilateral white matter to chronic aphasia symptoms as assessed by diffusion tensor MRI. Brain Lang. November 2015;150:117-128. doi:10.1016/j.bandl.2015.09.001. (R) 131. Thompson HE, Robson H, Lambon Ralph MA, Jefferies E. Varieties of semantic 'access' deficit in Wernicke's aphasia and semantic aphasia. Brain. 2015;138(Pt 12):3776-3792. doi:10.1093/brain/awv281. (R) 132. Efstratiadou EA, Papathanasiou I, Holland R, Archonti A, Hilari K. A Systematic Review of Semantic Feature Analysis Therapy Studies for Aphasia. J Speech Lang Hear Res. May 17, 2018;61(5):1261-1278. doi:10.1044/2018_JSLHR-L-16-0330. 133. de Vries NJ, Sloot PH, Achterberg W. Pain and pain assessment in stroke patients with aphasia: a systematic review. Aphasiology. 2017;31(6):703-719. 134. McKinnon ET, Fridriksson J, Glenn GR, et al. Structural plasticity of the ventral stream and aphasia recovery. Ann Neurol. July 2017;82(1):147-151. doi:10.1002/ana.24983. 135. Stephens M. The Effectiveness of Speech and Language Therapy for Poststroke Aphasia. Am J Nurs. November 2017;117(11):19. doi:10.1097/01.NAJ.0000526741.00314.d9.