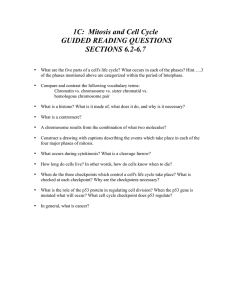
THYROID Volume 10, Number 11, 2000 Mary Ann Liebert, Inc. Anaplastic Changes Associated with p53 Gene Mutation Differentiated Thyroid Carcinoma After Insufficient Radioactive Iodine (131l) Therapy Nobuko Sera,1 Kiyoto Ashizawa,1 Takao Ando,1 Akane Ide,1 Yasuyo Abe,1 Toshiro Usa,1 Eri Ejima,1 Tomayoshi Hayashi,2 Isao Shimokawa,3 and Katsumi Eguchi1 Tan in Tominaga,1 Thirty-two patients with differentiated thyroid carcinomas with distant metastasis were examined using a ra¬ dioactive iodine (131I) tracer dose prior to 131I therapy and followed up for 10 years or until death (whichever occurred first). Nineteen patients who received 131I therapy had an accumulation of 131I in the métastases (group I) and 15 of those patients were alive more than 10 years after the first 131I treatment. In contrast, all 13 patients in whom the métastases did not show accumulation of 131I died within 10 years. Of the latter group, eight pa¬ tients had received 131I therapy (group II), four of whom died with anaplastic changes within 5 years of treat¬ ment. p53 gene mutation was identified by immunohistochemistry in primary thyroid carcinoma tissue from patients with anaplastic changes that were evident during total thyroidectomy. Five patients did not receive 131I therapy (group III), of whom one, who also had a p53 gene mutation in the original tumor, died with anaplastic change 10 years after thyroidectomy. Seven patients in group I had p53 gene mutations in their thy¬ roid carcinoma tissues, but none showed anaplastic changes. Our results suggest that 131I therapy may be use¬ ful for patients with distant métastases, with or without p53 gene mutations, which show accumulation of 131I from tracer and therapeutic doses. In contrast, 131I therapy is apparently not effective in patients who do not show sufficient accumulation of 131I, but rather, may cause early anaplastic changes with a p53 gene mutation. Introduction is extensive literature on the treatment and prog¬ nosis of metastatic thyroid carcinoma. Radioactive io¬ dine (131I) has been used in the therapy of differentiated thyroid carcinoma since 1942 (1). Many publications have supported the benefit of 131I therapy in metastatic thyroid carcinoma (2-5), but, conversely, some have not reported any benefit (6,7). Iodine accumulation in métastases is an important aspect of 131I therapy (8). Severe side-effects of 131I therapy have only rarely been reported. These include secondary malignancy (9,10) and, in some patients with metastatic differentiated thyroid carcinoma, the tumor exhibited anaplastic change (6,11). However, a causal relationship between 131I therapy and such side-effects has not been established (12). In some cases, anaplastic carcinomas arise from preexisting well-differentiated thyroid carcinomas (13). Several studies have shown that p53 gene mutations are more frequent in poorly differentiated and anaplastic carcinomas than in well-differentiated papillary and follicular carcinomas (14,15). In this study, we examined the relation- There ship between anaplastic change and p53 gene mutation oc¬ curring after 131I therapy. Material and Methods Patiente Between 1965 and 1995, a total of 195 patients were hospitalized in our department at Nagasaki University Hospital, Nagasaki, Japan, for treatment of thyroid carcinoma. In this study, 32 patients from these 195 patients were selected, The patients who were selected included those who: (1) had undergone total thyroidectomy followed by T4 replacement therapy; and (2) had distant métastases at primary diagnosis. Métastases were surveyed by radiologie workups such as standard X-rays, computed tomography (CT), scintigraphy, or ultrasonographic scanning, prior to total thyroidectomy. The selected patients were followed up for longer than 10 years from the date of ,31I tracer scintigraphy or until they died of thyroid carcinoma during this period. Patients with metastatic thyroid carcinoma but who died of unrelated dis¬ dirsi Department of Internal Medicine, and 2Department of Pathology, Nagasaki University Hospital, Nagasaki, 3First Department of Pathology, Nagasaki University School of Medicine, Japan. 975 SERA ET AL. 976 Table 1. Patients Patient No. Gender Age (yrs) F F F F F F M M F F F F M F F F M F F 44 19 45 63 70 45 55 37 53 52 66 23 78 63 72 51 35 68 72 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 His. at ope Site of metastasis Tg (ng/mL) Bone NE 169 NE NE NE NE 899 NE 621, 23700. Lung P F P P P F Bone Bone, Lung Lung Lung Bone, Lung Bone, Lung F F F F P P Bone Bone, Lung Bone Lung Lung Lung Lung, Kidney P P Med. LN F F P Kidney Med. LN Hilar LN P Group I of Dose J3JJT (mCi) uptake 150 150 150 150 150 150 90 150 150 84 148 150 129 126 50 + + + + + + + + + + + + + + + + + + -¬ 259. 21. 419. 39. 1680. 1532. 180, 0, 120 150 100 150 NE p53 gene Anaplastic changes Outcome mutation Cause of death His. at Autopsy + A A A A A A A A A A A A A A NE D(4)b + + D(9) D(9) + NE NE + + NE + RF HF HF RF D(10) His., histologie diagnosis; Tg, thyroglobuline at administration of 131I tracer dose; P, papillary carcinoma; F, follicular carcinoma; LN, lymph node; Med. LN, mediastinal LN; +, accumulation of 131I outside thyroid bed by 131uptake posttherapy scans; A, alive; D, deceased; NE, not examined; RF, respiratory failure; HF, heart failure. aTherapeutic dose. bNumbers between parentheses represent the survival period (years) after thyroidectomy. within the observation period (10 years) were excluded from this study. Thirty-two patients who met the above criteria were divided into three groups. Group I (n 19) was comprised of patients in whom iodine uptake was observed outside the thyroid bed after the 131I tracer dose and who were then treated with doses of 50-150 mCi of 131I (Table 1). Group II (n 8) was comprised of patients in whom iodine uptake in distant métastases was not observed after the 131I tracer dose, but who were treated with doses of 50-150 mCi of 131I (Table 2). Group III (n 5) was comprised of untreated patients in whom iodine uptake in distant métastases was not observed after the 131I tracer dose (as in Group II) (Table 3). Because this was a retrospective ease = = = analysis, patients were in either group II and III based on nonrandomized treatment decisions. 1311 total-body scans 131I tracer was administered 2 weeks after total thy¬ roidectomy, when patients developed hypothyroidism (low FT4 and high thyrotropin [TSH] value). All patients had a serum TSH concentration of 30 mlU/L or more. All patients put on an iodine-restricted diet 1 week before admin¬ istration of the 131I tracer dose. We did not measure the uri¬ nary iodine value of the subjects in this study. Nagataki, et al., reported that the average urinary iodine excretion was were Table 2. Patients No. Gender F F F F F M M M Age (yrs) 74 51 45 52 70 59 54 55 His. ope Site of metastasis at F Bone, Bone, Tg (ng/mL) 16.9 351.6 N.E 688.9 38.5 286.0 Lung, Trachea 244.5 1710.0 Bone Lung Lung Lung Lung Bone, Lung Lung of Group II Dose" 131I (mCi) uptake 52 150 126 150 150 50 150 50 Outcome D(4)b D(5) D(3) D(2) D(2) D(2) D(3) D(2) p53 gene Anaplastic mutation changes NE + + NE + + + Cause of death RF RF RF RF RF RF RF RF His. at Autopsy F Ana Ana Ana Ana His., histologie diagnosis; Tg, thyroglobuline at administration of 131I tracer dose; P, papillary carcinoma; F, follicular carcinoma; (-), no accumulation of 131I outside thyroid bed by posttherapy scans in 131uptake; D, deceased; NE, not examined; RF, respiratory failure; HF, heart failure; Ana, Anaplastic carcinoma. aTherapeutic dose. bNumbers between parentheses represent the survival period (years) after thyroidectomy. 977 131l THERAPY FOR PATIENTS WITH METASTASES FROM THYROID CANCERS Table 3. Patients Patient No. Gender Age (yrs) M F F F F 68 55 51 48 68 His. at Site of metastasis ope NE 251.0 93.0 NE 261.0 Mediastinal LN Lung Lung, Adrenal Mediastinal LN Group III Outcome Tg Bone, Lung, Heart F P P F P of D D D D D p53 gene mutation Anaplastic changes (0)b Cause of death DIC RF RF RF RF (3) (10) (0) (8) His. at Autopsy F P Ana F His., histologie diagnosis; Tg, thyroglobuline at administration of 131I tracer dose; P, papillary carcinoma; F, follicular carcinoma; LN, lymph node; D, deceased; RF, respiratory failure; Ana, Anaplastic carcinoma; DIC, disseminated intravascular coagulation aNumbers between parentheses represent the survival period (years) after thyroidectomy. less than 200 ese ¿ig/day on the iodine-restricted diet in Japan¬ patients (11). An 131I total-body scan was performed both 24 hours after administration of 131I tracer dose for each pa¬ tients, and 5-7 days after therapeutic 131I doses of 50-150 mCi for patients of group I and group II, using a large view¬ ing field -camera. Radiation therapy therapy was performed 2 weeks after the 131I tracer dose was administered. Therapeutic doses were adminis¬ tered to patients in whom iodine uptake was evident out¬ side the thyroid bed (group I) and to patients in group II who showed no evidence of iodine uptake outside the thy¬ roid bed. The remaining patients with no extrathyroid iodine uptake did not receive 131I therapy (group III). 131I p53 Immunohistochemistry Thyroid carcinoma tissues were obtained from each patient 15, group II, 6; group during thyroidectomy (group I, III, 5). All samples showed differentiated thyroid carci¬ nomas (papillary carcinoma, 17; follicular carcinoma, 9). Paraffin sections were prepared and after deparaffinization, each specimen was boiled four times, 5 minutes each, in phosphate buffered saline in a microwave oven, and then = = = = = fixed in 0.3% H202 with distilled deionized water (DDW) to block endogenous peroxidase activity. The sections were stained with anti-p53 antibody (MAb D07 Dako, Glostrup, Denmark) diluted 1:100 for 1 hour at room temperature, us¬ ing the streptavidin horseradish peroxidase technique. Results Tables 1-3 show the results of investigations in all 32 pa¬ tients. Seventeen patients died within 10 years of surgery. Table 4. Summary Type Group I II 6 III 5 F F Total p53 15 F 26 of 7 6 0 3 2 26 Patients (group I) in whom métastases showed accumula¬ tion of 131I after both the tracer dose and therapeutic dose of 131I, exhibited a higher survival rate than patients in whom métastases did not show accumulation of 131I (groups II and III). Patients in group I, who were alive, did not have any clinical symptoms and signs suggesting anaplastic changes, such as rapid tumor growth, high fever, and pain during ob¬ servation. In our study, all patients in group II died within 5 years of surgery and four of the eight exhibited anaplastic changes in the métastases. However, in group III, two pa¬ tients survived longer than 5 years (8 and 10 years), one of whom exhibited anaplastic changes in the métastases after 10 years. The principal causes of death related to thyroid car¬ cinoma were respiratory failure caused by infection or pul¬ monary bleeding (i.e., disseminated intravascular coagula¬ tion) or trachéal obstruction by the large mass of metastatic carcinoma. Anaplastic changes were observed in 5 of 17 de¬ ceased patients during autopsy (Tables 2 and 3). Eleven of twenty-six (42.3%) excised thyroid tissue sam¬ ples showed strong (mutant) p53 expression via immuno¬ histochemistry (Table 4). Comparison of cancer type showed mutant p53 expression in 7 of 17 (41.2%) papillary carcino¬ mas and 4 of 10 (40.0%) follicular carcinomas. Seven of the fifteen patients examined (46.7%) in group I exhibited mu¬ tant p53 expression, of whom three patients with papillary carcinomas survived, but two of four patients with follicu¬ lar carcinomas died, one from respiratory failure after 4 years and the other from heart failure after 9 years. Three of six (50.0%) patients (all with papillary carcinoma) in group II exhibited mutant p53 expression. Furthermore, all three of these mutant p53-positive tumors exhibited anaplastic changes within 5 years of 131I therapy. Figure 1A shows his¬ tologie sections of one such patient with papillary configu¬ rations present in the primary tumor (Table 2, Patient No. 3) during total thyroidectomy. Consecutive sections from the p53 Immunohistochemistry mutation (%) 3 4 3 0 1 0 (37.5) (57.1) (50.0) (0.0) (33.3) (0.0) 11 Alive Deceased Anaplastic changes o 2 3 0 1 0 0 0 3 0 1 Ü 6 4 978 SERA ET AL. ' 'S II s t * specimen shown in Figure , 4 , 1A exhibited strong p53 expres¬ immunohistochemistry (Figure IB). This tumor un¬ derwent anaplastic changes after 3 years (Figure 1C). In con¬ - sion via 4# ¿,,6 trast, all p53-negative patients in group II died within the study period without undergoing anaplastic changes. In group III, only one of five tumors (20%) exhibited mutant p53 expression. This tumor exhibited anaplastic change and the patient died from thyroid carcinoma related complica¬ tions 10 years after 131I tracer scintigraphy. Discussion * B C rv,y> mmamm , FIG. 1. A. Microscopy of differentiated papillary carcinoma in a section during total thyroidectomy. B. Positive p53 immunostaining in consecutive sections from the differentiated papillary carcinoma shown in A. C. Microscopy of anaplas¬ tic carcinoma from a section at autopsy from the same pa¬ tient (see Table 2: Patient #3). Anaplastic changes developed after 131I therapy. Magnification X 400. The results showed that patients with tumors that accu¬ mulated 131I did better than patients whose tumors that did not. A significant benefit from 131I therapy was observed in patients with remote métastases that showed accumulation of 131I after both the tracer and therapeutic doses, but not in patients with remote métastases that failed to show such ac¬ cumulation. In our study, all patients in group II died within 5 years of surgery, and four of the eight exhibited anaplastic changes in the métastases. However, in group III, two patients sur¬ vived longer than 5 years (8 and 10 years), one of whom ex¬ hibited anaplastic changes in the métastases after 10 years. However, statistically, there was no significant difference be¬ tween groups II and III with Kaplan-Meier analysis (Data not shown). Crile, et al. (12) and Leeper (6) reported two cases of rapidly fatal anaplastic carcinoma in patients with papillary-thyroid cancer treated with 131I. However, it has been reported that 131I therapy does not cause anaplastic transformation (13). Our results suggest that insufficient 131I therapy may, in fact, trigger early anaplastic changes. Be¬ cause this study was a retrospective analysis, there is a pos¬ sible bias for our results. The p53 tumor-suppressor gene has been implicated in tu¬ mor progression in the thyroid gland. Several studies have shown that both p53 overexpression and p53 gene mutations are far more frequent in poorly differentiated and anaplas¬ tic carcinomas than in well-differentiated papillary and fol¬ licular carcinomas (15-17). In order to evaluate the relation¬ ship between early anaplastic change after insufficient 131I therapy and p53 mutation in primary thyroid-carcinoma tis¬ sues, we examined p53 gene mutations via immunohisto¬ chemistry in 26 thyroid carcinomas obtained via total thy¬ roidectomy. Wild-type p53 protein has a short half-life, but mutation of the p53 gene confers a longer half-life on the mu¬ tant protein (18,19) thereby leading to its accumulation. Positive p53 expression therefore represents mutated p53 (18,20). Eleven of twenty-six tumors analyzed in our study exhibited p53 gene mutations. Further analysis of our results showed that neither tumor histology (papillary or follicular carcinoma) nor 131I uptake correlated with p53 gene muta¬ tion. Recent reports have suggested that p53 plays a role in thy¬ roid tumor progression via cell dedifferentiation and/or en¬ hanced biologic aggressiveness (21), and the presence of p53 gene mutations confers a poor prognosis (22). Our results, however, demonstrated no relationship between p53 gene mutation and prognosis in patients who underwent suc¬ cessful 131I therapy. Furthermore, three differentiated thy¬ roid carcinomas with p53 gene mutations, which were treated with 131I therapy but exhibited no 131I uptake, all de- 979 THERAPY FOR PATIENTS WITH METASTASES FROM THYROID CANCERS veloped anaplastic changes within 5 years of therapy. One patient with a p53 gene mutation, who did not receive 131I therapy because of poor 131I accumulation, developed anaplastic changes, but not until 10 years after the 131I tracer dose. 131I therapy has not previously been reported as a pos¬ sible trigger for anaplastic changes but our results suggest this possibility. After therapeutic neck irradiation, Fogelfeld, et al. (23) reported an increased frequency of p53 gene mu¬ tation in thyroid carcinomas. In this regard, Namba and coworkers (24) postulated that the p53-WAFl/Cipl pathway play a role in induction of Gl arrest in human thyroid ep¬ ithelial cells following irradiation. The absence of Gl arrest following low-dose irradiation suggests a failure of the deoxyribonucleic acid repair process. Furthermore, the lack of 131I concentrating activity already implies some loss of dif¬ ferentiation. We postulate that this process results in pro¬ gressive dedifferentiation of the carcinoma cells until, finally, producing anaplastic changes. In conclusion, 131I therapy may be useful for patients with distant métastases from thyroid cancer, with or without p53 gene mutations, when such tumors show accumulation of 131I after tracer doses. Conversely, 131I therapy is ineffective in patients who do not show an accumulation of 131I, and in such patients, p53 gene mutation may trigger early anaplas¬ tic changes. 12. 13. 14. 15. 16. 17. 18. 19. References 1. Herts S, Robert A 1942 Application of radioactive iodine therapy in Graves' disease. J Clin Invest 21:624-628. 2. Mazzaferri EL 1987 Papillary thyroid carcinoma: Factors influencing prognosis and current therapy. Semin Oncol 20. Young RL, Mazzaferri EL, Rahe AJ, Doifman SG 1980 Pure follicular thyroid carcinoma: Impact of therapy in 214 pa¬ 21. 14:315-332. 3. tients. Semin Nucl Med 21:733-737. Cady B, Sedgwick CE, Meissner WA 1979 Risk factor analy¬ sis in differentiated thyroid cancer. Cancer 43:810-820. 5. Mazzaferri EL, Jhiang SM 1994 Long-term impact of initial surgical and medical therapy on papillary and follicular thy¬ roid cancer. Am J Med 97:418^28. 6. Leeper RD 1973 The effect of 131I therapy on survival of pa¬ tients with metastatic papillary and follicular thyroid carci¬ noma. J Clin Endocrinol Metab 36:1143-1152. 7. Ruegemer JJ, Hay ID, Bergstralh EJ, Ryan JJ, Offord KP, Gor¬ man CA 1988 Distant métastases in differentiated thyroid carcinoma: A multivariate analysis of prognostic variables. J Clin Endocrinol Metab 67:501-508. 8. Eishima K, Izumi M, Tominaga T, Kimura H, Yokoyama N, Morita S, Nagataki S 1993 The significance of 131I treatment of metastatic thyroid carcinoma. Int J Oncol 2:877-882. 9. Shimon I, Kneller A, Olchovsky D 1995 Chronic myeloid leukemia following 131I treatment for myroid carcinoma: A report of two cases and review of the literature. Clin En¬ 4. docrinol 43:651-654. 10. Brown AP, Greening WP, McCready VR, Shaw HJ, Harmer CL 1984 Radioiodine treatment of metastatic thyroid carci¬ noma: The Royal Marsden Hospital experience. Br J Radiol 57:323-327. 11. Nagataki S 1993 Status of iodine nutrition in Japan. In: De- Dunn JT, Glinoer D Iodine Deficiency in Europe. New York, Plenum Press, pp 141-148. Crile G Jr, Antunez AR, Esselstyn CB Jr, Hawk WA, Skillern PG 1985 The advantages of subtotal thyroidectomy and sup¬ pression of TSH in the primary treatment of papillary car¬ cinoma of the thyroid. Cancer 55:2691-2697. Maxon HR, Smith HS 1990 Radioiodine-131 in the diagno¬ sis and treatment of metastatic well-differentiated thyroid cancer. Endocrinol Metab Clin North Am 19:685-718. Kapp DS, LiVolsi VA, Sanders MM 1982 Anaplastic carci¬ noma following well-differentiated thyroid cancer. Yale J Biol Med 55:521-528. Ito , Seyama , Mizuno , Tsuyama , Hayashi Y, Dohi , Nakamura N, Akiyama M 1993 Genetic alterations in thy¬ roid tumor progression: Association with p53 gene muta¬ tions. Jpn J Cancer Res 84:526-531. Soares P, Cameselle-Teijeiro J, Sobrinho-Simoes M 1994 Immunohistochemical detection of p53 in differentiated and undifferentiated carcinomas of thyroid. Histopathology 24:205-210. Fagin JA, Matsuo K, Karmakar A, Chen DL, Tang SH, Koeffler HP 1993 High prevalence of mutation of p53 gene in poorly differentiated human thyroid carcinomas. J Clin In¬ vest 91:179-184. Levine AJ, Momand J, Finlay CA 1991 The p53 tumor sup¬ pressor gene. Nature 351:453-456. Kastan MB, Onyekwere O, Sidransky D, Vogelstein , Craig RW 1991 Participation of p53 protein in the cellular response to DNA damage. Cancer Res 51:6304-6311. Mosnier J, Perret AG, Vindimian M, Dumollard JM, Balique JG, Perpoint B, Boucheron S 1996 An immunohistochemical study of the simultaneous expression of bcl-2 and p53 oncoproteins in epithelial tumors of the colon and rectum. Arch Pathol Lab Med 120:654-659. Donghi R, Longoni A, Pilotti S, Michieli P, Della Porta G, Pierotti MA 1993 p53 gene mutations are restricted to poorly differentiated and undifferentiated carcinoma of the thyroid gland. J Clin Invest 91:1753-1760. Godballe C, Asschenfeldt P, Jorgensen KE, Bastholt L, Clausen PP, Hansen TP, Hansen O, Bentzen SM 1998 Prog¬ nostic factors in papillary and follicular thyroid carcinomas: p53 expression is a significant indicator of prognosis. Laryn- lange F, 22. goscopy 108:243-249. Fogelfeld L, Bauer TK, Schneider AB, Swartz JE, Zitman R 1996 p53 gene mutations in radiation-induced thyroid can¬ cer. J Clin Endocrinol Metab 81:3039-3044. 24. Namba H, Hara T, Tukazaki T, Migita K, Ishikawa N, Ito , 23. Nagataki S, Yamashita S 1995 Radiation-induced Gl arrest is selectively mediated by the p53-WAFl/Cipl pathway in human thyroid cells. Cancer Res 55:2075-2080. Address reprint requests to: Katsumi Eguchi First Department of Internal Medicine Nagasaki University School of Medicine Prof. 1-7-1 SaL·moto Nagasaki 852-8501 Japan E-mail: Eguchi@net.nagasaki-u.ac.jp