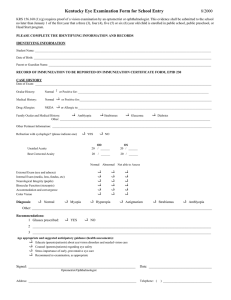
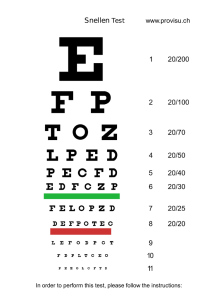
Eye Symptoms and Eye Examination TEMUJIN F.R. MADRID, M.D. Eye Complaints How do you proceed with a patient with eye complaints Be observant Ask the right questions Listen carefully History and PE are paramount Eye History 1. Patient demographic – age , sex, occupation, residence, status 2. Chief Complaint – symptoms, laterality, duration, 3. History of Present Illness- duration, intensity, progression 4. Review of systems Eye Symptoms 1. Abnormalities in Vision 2. Abnormalities in Appearance 3. Abnormalities in Ocular Sensation Abnormalities of Vision Loss of visual acuity Locate problem along the optical and neurologic visual pathway Abnormalities in vision Anatomic obstruction – lid ptosis Interference of ocular media Retinal pathology Visual pathway problems Refractive Error Metamorphopsia Amsler Grid Visual Distortion in Amsler Grid Abnormalities in vision Central Peripheral Scotomas- focal Hemianopia – larger defects Visual field defects Scotoma Scotoma Scotoma Hemianopia Abnormalities in vision Temporal profile- transient of persistent Degree of Visual Impairment Aggravating/ Mitigating Factors Visual Aberrations Glare/ Halos Visual Distortion Flashes/Flickering Lights Floating Spots Oscilloscopia Diplopia – monocular/ binocular Abnormalities in appearance Lid and Periocular Lesions Ptosis Proptosis Conjunctival problems Corneal problems Ocular surface problems Abnormalities in Ocular Sensation Periocular Ocular Retrobulbar Poorly Localized/ Vague Eye Irritation Eye irritation Itching Dryness Burning Grittiness Foreign Body Sensation Tearing Secretions/Discharge Eye examination A. Visual Acuity B. Gross Examination/ External Eye Exam C. Extraocular Movement D. Intraocular Pressure Determination E. Fundus Examination (Direct and Indirect) Visual acuity Measurement relating testing distance to the minimal object size resolvable at that distance Target subtends a visual angle of 5 minutes of arc with the subject 20 feet away from the target Visual Acuity Distance Visual Acuity Test – uses Snellen/ ETDRS/ Chart Projector Near Visual Acuity Test – uses Jaeger Chart Both test different aspects of Central/ fine detail vision Both utilize corrective lenses Distance Acuity – Snellen Chart Distance Testing – ETDRS Chart Distance Visual Acuity 1. Subject at 20 foot distance from a well illuminated chart 2. Occlude the poorer eye 3. Ask the patient to identify the letter or number on the lines successively from left to right 4. Note the visual acuity on the last line that the patient could read 5. If the patient misses half or fewer than half the letters on the smallest readable line, record how many letters were missed. (E.g. 20/40 -2) 6. Repeat with spectacle correction. 7. If VA is less than 20/20, repeat with pinhole occluder 8. Repeat process for the contralateral eye Visual Acuity Notation CC (With Correction) VAOD OS SC( Without Correction VAOD OS Pinhole visual acuity 1.Position the patient and occlude the eye not being tested, as done for the distance acuity test. 2. Ask the patient to hold the pinhole in front of the eye that is to be tested. 3. Instruct the patient to look at the distance chart through the single pinhole 4. Instruct the patient to use small hand or eye movements to align the pinhole to resolve the sharpest image on the chart. 5. Ask the patient to begin to read the line with the smallest letters that are legible as determined on the previous vision test without the use of a pinhole. 6. Record the Snellen acuity obtained and precede with the abbreviation. PHOD OS Poor visual acuity If the patient is unable to see the biggest optotype on the card, the progression (from better to worse) is 1. Counting fingers (CF) 2. Hand motions (HM) 3. Light perception (LP) with projection 4. LP without projection 5. No light perception (NLP). Visual acuity in children Use Allen Chart For children who are too young to use Allen pictures, employ the “central, steady, maintain (CSM)” approach. 1. Central: Is the corneal light reflex in the center of the pupil? 2. Steady: Can the patient continue fixating when the light is slowly moved around? 3. Maintain: Can the patient maintain fixation with the viewing eye when the previously covered eye is uncovered? Allen Charts Near Acuity Testing 1. Patient wears habitual corrective for near reading 2. Position Jaeger chart at 14 inches distance 3. Poorer eye is occluded 4. Read each word on the line of the smallest characters legible 5. Repeat the procedure for the other eye 6. Record the acuity value separately for each eye 7. Repeat the procedure, using BINOCULAR vision 8. Record biocular acuity JOD OS JOU Jaeger Chart External Eye Examination 1. Inspection 2. Palpation 3. Auscultation INSPECTION Follows a specific sequence 1. Head and face 2. Bones, muscles, nerves 3. Skin 4. Lymph nodes 5. Mouth, nose and paranasal sinuses 6. Orbit 7. Eyelids 8. Lacrimal System 9. Globe INSPECTION Eyelids and Eyelashes Conjunctiva Episclera and Sclera Cornea and Anterior Chamber EYELIDS AND EYELASHES Tumors Hordeolum – abscess of a sebaceous gland 1. Internal – meibomian gland abscess 2. External – glad of Zeis Chalazion – granuloma surrounding lipid due to blocked sebaceous gland Folliculitis – abscess surrounding a lash follicle; staphylococcal Angioedema Verruca Seborrheic Keratosis Basal Cell Carcinoma Internal Hordeolum External Hordeolum Chalazion BLEPHARITIS Anterior (Marginal) blepharitis 1. Staphylococcal Blepharitis – collarettes ( thin flakes around eyelashes) 2. Seborrheic Blepharitis – Scurf ( dandruff like flakes) 3. Demodectic blepharitis – Demodex folliculorum (mite) ; waxy cuff around eyelashes Staphylococcal Blepharitis Seborrheic Blepharitis Demodectic Blepharitis BLEPHARITIS Posterior Blephatitis/ Meibomianitis – excessive secretions of meibomian glands Angular Blepharitis – medial or canthal area; ulcerative/eczematoid Blepharitis causes : 1. Madarosis – loss of eyelashes 2. Poliosis – whitening of eyelashes 3. Trichiasis – misdirection of eyelashes Posterior Blepharitis (Meibomianitis) Posterior Blepharitis (Meibomianitis) Angular Blepharitis Trichiasis Madarosis Poliosis CONJUNCTIVA Conjunctival Hyperemia – dilation of blood vesses; diffuse redness ; nonspecific Ciliary (Limbal) Flush – ciliary vessels seen to extend radially from limbus; red, circumcorneal ring of dilated blood vessels; Corneal, episcleral, scleral or intraocular inflammation Conjunctival Hyperemia Ciliary Injection ; Ciliary Flush SECRETIONS AND DISCHARGE Watery discharge – excessive tearing (epiphora); caused by irritation Mucus – goblet cell secretion ; clear, sticky; non specific Mucopurulent Discharge – neutrophils with mucus; mild bacterial or allergic conjunctivitis Purulent Discharge – mainly of neutrophils; copious; gonococcal, meningococcal, bacterial or fungal conjunctivitis; corneal ulcers Watery Secretion Mucuopurulent Discharge Purulent Discharge Chemosis Edema of or beneath the conjunctiva Thickening or ballooning of conjunctiva Allergy, less often in other types of eye inflammation Chemosis Chemosis EPISCLERITIS Immunologically mediated inflammation Between conjunctival stroma and sclera Blanches with phenylephrine/epinephrine Benign, short lived No tenderness, ciliary pain or anterior segment inflammation Episcleritis SCLERITIS Immunologically mediated inflammation of the sclera Pain, hyperemia and tenderness Prolonged Does NOT blanch with phenylephrine/ epinephrine May cause severe eye damage and complications Systemic illness in half of patients Scleritis Scleritis PIGMENTATIONS Congenital Melanosis Oculi – deep gray/slate patches in sclera and episcleral Blue Nevus – deep conjunctiva/episcleral; dark blue color Congenital Melanosis Oculi Congenital Melanosis Oculi Blue Nevus Pterygium Squamous Cell Carcinoma Subconjunctival Hemorrhage CORNEA AND ANTERIOR CHAMBER Best examined with slit lamp Penlight may be used for regular clinical purposes CORNEA AND ANTERIOR CHAMBER Pannus- superficial corneal vascularization; due to necrosis or hypoxia Band Keratopathy – calcium deposits; usually seen across cornea Corneal Scars ( Leukoma) – grey- white; opaque and permanent Corneal Edema – Corneal haze; due to dysfunction of endothelium, epithelium or stroma Hyphema – blood in the anterior chamber usually from trauma Hypopyon – purulent exudates (pus) in anterior chamber; corneal or intraocular infections Corneal Pannus Band Keratopathy Band Keratopathy Corneal Leukoma Corneal Edema Corneal Edema Hyphema Hypopyon Corneal Ulcer With Hypopyon PALPATION Involves tactile, proprioceptive and temperature changes 1. Use the middle finger for pre auricular lymph nodes 2. Use index finger and thumbs to open eyelids wide apart 3. Ask the patient to gaze in different directions to expose ocular surface 4. Judge and record, composition any mass due to its size, shape, composition, tenderness and movability AUSCULTATION Used to detect orbital bruit Bell of the stethoscope placed on the closed eye as the patient holds breathing A bruit signifies 1. Carotid cavernous fistula 2. Arteriovenous malformation OCULAR MOTILITY Monocular Binocular DUCTIONS – monocular eye movements VERSIONS/vergences – binocular eye movement 1. Convergence – both eyes move nasally 2. Divergence – both eyes move temporally Yoke Muscles – muscles in each eye that work together to move both eyes in the same direction (conjugate movement) DUCTIONS 1. ADDUCTION – movement nasally 2. ABDUCTION – movement temporally 3. ELEVATION – movement upward 4. DEPRESSION – movement downward 5. INTORSION – nasal rotation of the superior vertical corneal meridien 6. EXTORSION – temoral rotation of superior vertical corneal meridian Extraocular Muscle Movements CARDINAL POSITIONS OF GAZE 1. Right and Up 2. Right 3. Right and Down 4. Left end Up 5. Left 6. Left and Down CARDINAL POSITIONS OF GAZE ASSESSING OCULAR MOTILITY 1. Sit facing the patient 2. Hold your finger 14 inches from the patient looking in primary position 3. Ask the patient to follow your finger as you move it into the six cardinal fields and up and down along the midline 4. Elevate the upper lid with your free hand to observe downgaze 5. Note any abnormalities in amplitude. Rate amplitudes by percentage 6. Note any nystagmus (abnormal eye movements) and note prescence, direction and amplitude Ocular Motility Please watch and study this video https://www.youtube.com/watch?v=MsBDVWgdF0&list=PLStZ9ETiSvr0vowVPOQTJl7nlaozjnMSu&index=5 Tonometry Measurement of intraocular pressure Aids in diagnosis management of glaucoma Also detects ocular hypotony in iritis and retinal detachment Measured in mmHG. Normal value 10 – 21 mmHg Types of Tonometry Goldmann Applanation Tonometry 1. Tonopen 2. Air puff Tonometry 3. Shiotz Tonometry 4. Digital Tonometry 5. Applanation Tonometry APPLANATION TONOMETRY APPLANATION TONOMETRY TONOPEN TONOPEN AIR PUFF TONOMETRY AIR PUFF TONOMETRY SCHIOTZ TONOMETER SCHIOTZ TONOMETER DIGITAL TONOMETRY Uses the examiners fingertips to indent the globe Rough estimate ; may be inaccurate Used only for estimation of large differences between patients eyes DIGITAL TONOMETRY 1. Patient looks down, but does not close eyes 2. Rest your fingers on the forehead 3. Put both forefingers on the superior aspect of the right globe 4. Gently and alternately depress both forefingers and assess tone 5. Repeat for the left eye DIGITAL TONOMETRY 1. NORMOTENSIVE - about tone of tip of your nose 2. ELEVATED PRESSURE – tone of glabella 3. HYPOTENSIVE – tone of lips FUNDUS EXAMINATION 1. Direct Fundoscopy Handheld Ophthalmoscope Virtual Upright view Monocular vision No stereopsis/ depth perception 15 times magnification Relatively small field of view (10-15 degrees) Illumination is relatively dim Mild opacities in media can interfere with examination Close proximity to patient FUNDUS EXAMINATION 2. Indirect Ophthalmoscopy Binocular view Wide field of view (35 degrees), can see up to Pars plana with indentation Working distance is 35 – 40 cm Drawing of lesions is easy since one hand is free Can be used to examine fundus during surgery Excellent illumination 2- 5 times magnification Real and inverted image DIRECT OPHTHALMOSCOPY DIRECT OPHTHALMOSCOPY Handle Head Light source Peephole Dial up lenses Filters Direct Ophthalmoscopy 1. Examine the patient’s right eye with your right eye, left with left. Tell patient to look straight at a distance 2. Focus by twisting the Lens/Rekoss disc. Optium focus depends on both patient’s and examiner’s refractive error and the examination distance 3. Obtain the patient’s red-orange reflex at 2 feet and zoom in slowly. 4. Steady instrument by resting side of hand against the patient’s cheek. The free hand thumb raises the upper lid. 5. Dial lens to focus. Optimal view is at 2 -3 cm from patient’s eye 6. Angle ophthalmoscope 15degrees temporal to fixation. Optic disk will be visible Direct Ophthalmoscopy 7. Focus on optic disk by following retinal blood vessels. Assess cup disk ratio 8. From optic disk, follow dic outwards to all portons of the retina 9. Note : Vascular color, caliber, bifurcations, crossings and background. Look for hemorrhages and exudates 10. Examine the macular area for irregularities 11. Repeat examination for the other eye Direct Ophthalmoscopy Normal cup-to –Disc ratio is 0.3-0.4 Fovea – two disk diameters temporal from edge of disc; pinpoint reflex Macula- bounded by major branch retinal vessels Arteries – lighter Veins – darker; wider Direct Ophthalmoscopy Please watch and study this video https://youtu.be/7lhvhKvK_iM Indirect Ophthalmoscopy Requires pupillary dilatation Supine positioning of the patient preferable Indirect ophthalmoscope worn on head Binocular viewing using a lens of fixed power (usually 20 Diopter) Light source directed to the patient’s eye Patient looks to the direction of the quadrant being examined Convex lens is used to focus light onto the retina Indirect Ophthalmoscopy Indirect Ophthalmoscopy Please watch and review this video https://youtu.be/Zg0eUd3aCFI 8 Part Eye Exam Study and Review the 8 part eye exam on this website https://studylib.net/doc/25249162/hand-out-of-8-part-eye Thank You