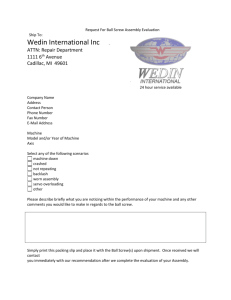
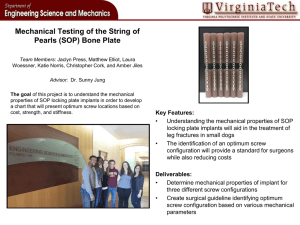
THE JOURNAL OF PROSTHETIC DENTISTRY BINON Evaluation of the effectiveness of a technique to prevent screw loosening Paul P. Binon, DDS, MSDa Roseville, Calif. Statement of problem. Abutment screw loosening of single and multiple fixed partial dentures attached to external hexagonal implants is commonly encountered. Purpose. A technique that has been reported to prevent abutment screw loosening was tested with cyclic loading to determine its effectiveness. Material and methods. A sample using identical components and test protocol, with the abutment screw tightened to 20 Ncm, was used as control. Results. On the basis of the data obtained, the recommended technique does not increase resistance to screw loosening. The control sample sustained a mean number of cycles to screw loosening of more than twice that of the technique evaluated. (J Prosthet Dent 1998;79:430-2.) CLINICAL IMPLICATIONS The procedure evaluated in this article cannot be relied on to keep abutment screws from loosening. Long-term screw joint stability can only be obtained when all critical controlling factors are optimized. A butment screw loosening of single and multiple fixed partial prostheses attached to external hexagonal implants is a commonly encountered occurrence.1-9 To mitigate this problem, Cavazos and Bell10 advocated an abutment screw tightening protocol that involves the application of hand torque, the addition of undercuts in the internal surface of the screw access chamber, the injection of impression material, and the condensation of a cotton pellet into the material before set. The rationale is that once the impression material sets and engages the head of the screw and the undercuts in the chamber, it prevents screw “back out” due to any functional micromovements of the abutment. Anecdotal reports of apparently useful clinical techniques frequently have substance and merit. However, techniques that involve the critical parameters that affect implant prosthesis stability require more prudent and thorough clinical and laboratory evaluation before acceptance. The purpose of this study was to evaluate the effectiveness of the screw stabilizing protocol when subjected to cyclic loading. MATERIAL AND METHODS Standard 3.75 × 10 mm external hexagonal implants (ASTM Grade 3 CPT, Implant Support Systems, Irvine, Calif.) were selected from a pack of implants, which have a mean hexagonal flat to net dimension of 2.684 mm (STD 0.007). Each implant was embedded in a sample a Private Practice; Assistant Research Scientist, Department of Restorative Dentistry, School of Dentistry, University of California San Francisco, San Francisco, Calif.; and Adjunct Professor of Prosthodontics, Indiana University, Indianapolis, Ind. 430 THE JOURNAL OF PROSTHETIC DENTISTRY Fig. 1. Control group implant–abutment test assembly. Nonsegmental (UCLA) type abutment has 0.1085-inch hexagonal recess. cup with Sample-kwick resin (Bushier, Lake Bluff, Ill.), as described in a previous study.11 Custom conical nonsegmented (UCLA type) abutments, 8 mm long with a major diameter of 8 mm and a loading table of 3 mm, made of ASTM grade 3 titanium were used to replicate the prosthetic element (Fig. 1). VOLUME 79 NUMBER 4 BINON THE JOURNAL OF PROSTHETIC DENTISTRY Table I. Cyclic loading test sample Sample 1 2 3 4 5 Mean SD Cycles 1,826,430 1,184,500 2,067,355 492,430 136,645 1,141,472 830,544 Table II. Cyclic loading reference sample Sample Cycles 1 2 3 4 5 Mean SD 2,038,950 2,530,920 1,716,099 2,177,180 3,772,920 2,447,214 796,654 The abutment had a midrange size hexagonal receptacle of 0.1085 inch, with a rotational tolerance (misfit) of 7 degrees. Abutments were connected to the implants with standard ASTM titanium grade 23 abutment screws (Implant Support Systems). For the experimental group, the abutment was attached to the implant in accordance with the following technique.10 PROCEDURE The abutment was attached to the implant and a ½ round bur was used to place four dimples inside the abutment cylinder immediately above the screw head at 90degree intervals. The implant abutment stack was then disassembled and the parts were debrided with an air syringe. The stack was reassembled and the screw was tightened to maximum finger torque. After 10 minutes, the screw was retightened. A 30-gauge needle was placed into the screw hexagonal to act as an air vent. With a free flow disposable syringe, the chamber was filled with Impregum impression material (Espe America, Norristown, Pa.) while aspirating with the 30-gauge needle syringe. Before set, a small cotton pellet was condensed on top of and into the impression material with an amalgam condenser. Excess impression material was removed with the condenser head. Immediately after set, any flash remaining on the screw access chamber wall was removed with an explorer. Fermit composite (Ivoclar Vivadent Inc., Amherst, N.Y.) was placed and light cured to achieve an occlusal seal (Fig. 2). The control reference sample was made up of identical components, without modification to the inside of the screw access chamber. The abutment screw was tightAPRIL 1998 Fig. 2. Schematic of implant–abutment test assembly with four dimples (D) immediately above screw, injected impression material (A), condensed cotton pellet (B), and Fermit occlusal seal (C) as advocated by Cavazos and Bell.10 Nonsegmental (UCLA) type abutment has 0.1085-inch hexagonal recess. ened to 20 Ncm of torque with a torque wrench (Lifecore Biomedical, Chaska, Minn.) as recommended by the manufacturer. No impression material/cotton plug was introduced into the screw access chamber. The test samples were allowed to bench set overnight. They were inserted into split collect sample holders and placed into the cyclic loading stations. The samples were cyclically loaded using the instrumentation and protocol previously published.11,12 The instruments loading head delivers a 30 pound (133.3 N) load to each abutment through a 0.090-inch diameter stylus. The samples were rotated counterclockwise, 360 degrees off-axis under the loading styli. A minute counter tracked the number of loading cycles and an automatic cut-off system monitored screw joint failure. Screw joint failure is defined as abutment mobility resulting from screw loosening, screw fracture, or implant fracture. During the test, when the cut-off system shorted, abutment mobility was verified manually. If mobility was questionable, the cut-off pointer was recalibrated and the instrument restarted. This was repeated until mobility was manually verified. The number of cycles to failure (screw loosening) was reported under these identical loading conditions. Five samples of each group were tested at different time intervals. Instrumentation was recalibrated and standardized in an identical manner for both groups at 1 million cycles interval, for all samples. The only variable in the study was the screw stabilizing technique advocated by Cavazos and Bell,10 which con431 THE JOURNAL OF PROSTHETIC DENTISTRY sists of maximum hand tightening the abutment screw and the addition of an impression material plug over the screw. RESULTS The test results are presented in Table I. Screw joint failure ranged from 136,645 to 2,067,355 cycles with a sample mean of 1,141,472 (SD 830,544). Failure constitutes screw back out that was verified manually with abutment mobility. None of the implants or screws fractured during the test. The control group recorded a mean of 2,447,214 (SD 796,654) cycles (Table II). BINON statistical analysis of the data is not relevant. However, it established a clear trend and demonstrated that the proposed screw stabilizing technique did not appear to offer superior performance. CONCLUSIONS Test results in this study indicated the following. 1. The hand tightening, impression material/cotton pellet screw access sealing technique does not inhibit screw back out. 2. The impression material/cotton pellet technique is a viable method of sealing the screw access hole. DISCUSSION REFERENCES Results obtained with identical components, assembled per manufacturer’s recommendations, and tested in an identical manner, were significantly better than in the test sample that used the impression material/cotton pellet sealing technique (Table II).11 The control test, recorded a mean of 2.4 million cycles to screw loosening compared with 1.1 million cycles for the impression material/cotton pellet technique. This may be attributed to several factors. Foremost is that the experimental technique recommended and relied on finger tightening of the abutment screw. In the reference sample, the abutment screw was tightened to 20 Ncm as recommended by the manufacturer. Standardized torque application with a calibrated torque gauge has been documented to be more consistent and predictable in obtaining optimal torque and preload in a screw.13 The second consideration is that regardless of its inherent rigidity, impression materials will not inhibit vibration or lateral movement within the implant– abutment complex. On the basis of the results of this test, the advocated screw stabilizing protocol does not improve screw resistance to screw loosening when compared with the conventional technique that calls for the application of 20 Ncm of tightening torque with a torque wrench. Sakaguchi and Borgersen14 have demonstrated that off axis loading results in micromovement within the screw joint complex that ultimately leads to screw loosening. The impression material/cotton plug technique did not appear to inhibit micromovement within the screw joint complex. The technique may be a viable method of obturating the screw access channel. Clinical experience also indicated that it permits easy access for reentry; however, improved screw joint stability was not demonstrated. Because the number of samples tested is small, 1. Sones AD. Complications with osseointegrated implants. J Prosthet Dent 1989;62:581-5. 2. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated implants: the Toronto study. Part III: problems and complications encountered. J Prosthet Dent 1990;64:185-94. 3. Jemt T, Linden B, Lekholm U. Failures and complications in 127 consecutively placed fixed partial prostheses supported by Brånemark implants: from prosthetic treatment to first annual checkup. Int J Oral Maxillofac Implants 1992;7:40-4. 4. Jemt T. Fixed implant supported prostheses in the edentulous maxilla: a five year follow-up report. Clin Oral Implants Res 1996;5:142-7. 5. Lekholm U, van Steenberghe D, Hermmann I, Bolender C, Folmer T, Gunne J, et al. Osseointegrated implants in the treatment of partially edentulous jaws: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants 1994;9:627-35. 6. Wie H. Registration of localization, occlusion and occluding materials for failing screw joints in the Brånemark implant system. Clin Oral Implants Res 1995;6:47-53. 7. Jemt T, Laney WR, Harris D, Henry PJ, Krogh PH Jr, Polizzi G, et al. Osseointegrated implants for single tooth replacement: a 1-year report from a multicenter prospective study. Int J Oral Maxillofac Implants 1991;6:2936. 8. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent 1995;74:51-5. 9. Balshi TJ, Hernandez RE, Pryszlak MC, Rangert B. Comparative study of one implant versus two replacing a single molar. Int J Oral Maxillofac Implants 1996;11:372-8. 10. Cavazos E, Bell FA. Preventing loosening of implant abutment screws. J Prosthet Dent 1996;76:566-9. 11. Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont 1996;9:149-60. 12. Binon PP, McHugh MJ. The effect of eliminating implant/abutment rotational might on screw joint stability. Int J Prosthodont 1996;9:511-9. 13. Goheen KL Vermilyea SG, Vossoughi J, Agar JR. Torque generated by handheld screwdrivers and mechanical torquing devices for osseointegrated implants. Int J Oral Maxillofac Implants 1994;9:149-55. 14. Sakaguchi RL Borgersen SE. Nonlinear finite element contact analysis of dental implant components. Int J Oral Maxillofac Implants 1893;8:665-61. 432 Reprint requests to: DR. PAUL P. BINON 1158 CIRBY WAY ROSEVILLE, CA 95661 Copyright © 1998 by The Editorial Council of The Journal of Prosthetic Dentistry. 0022-3913/98/$5.00 + 0. 10/1/89040 VOLUME 79 NUMBER 4