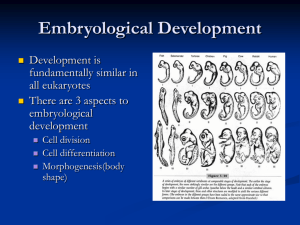
[MEDICAL EMBRYOLOGY] Yazan Al-Habil 2020 There are two fields of embryology: 1. General: • • • • The first period of fetal life. Lasts up until week 8. Called the embryonic period. Gives rise to the main tissues and “seeds” of the systems and organs which are yet to mature. 2. Fetal: • Called systemic embryology since it studies each system on its own. Unisex info: • • • • • [Gametogenesis] gametes are haploid (unlike somatic cells). Starts in week 2 o The baby is a 2 layered flat disc structure, consisting of: ▪ The upper epiplast, which is blue (figure) and columnar in shape. ▪ the amniotic cavity is above it. ▪ The hypoblast which is yellow (figure) and cuboidal in shape. ▪ the yolk sac is below it. o During week 2: some of the epiplasts start to obtain their own and unique and characteristics, forming PGCs. o At the end of week 2: the epiplast starts to prosper and spread throughout the embryonic disc (aka the bilaminar germ disc), forming primal tissues. The PGCs migrate to the yolk sac’s wall and settle there until the gonads are formed — week 4. The embryo’s body is no longer a flat disc but a cylindrically shaped structure, with the gonads forming in the back of the embryo. The PGCs undergo active mitosis and cytodiffrentiation; forming spermatogonia in males and oogonium in females. In females: • • • The PGCs immerse themselves in the ovarian tissues and reside under the surface of the ovary — which is covered by simple cuboidal epithelial cells; the germinal epithelium. Oogonia exist in groups covered by a single flat cell layer derived from the germinal epithelium. Give rise to: o Primary oocytes (with each one having its own cover made from follicular cells — together forming the primordial ovarian follicle). ▪ Undergoes meiosis 1 but is arrested at prophase, because: follicular cells (which surround it) produce an inhibiting factor which disrupts meiosis 1 until puberty (or ovulation to be more exact). ▪ Females have only primordial ovarian follicles and primary oocytes before puberty. ▪ The number of oogonia in the fifth month is 7 million, decreasing - by means of cell death - to about 600-800 thousand at birth, and to about 40 thousand primary oocytes at puberty. ▪ Note: only 300-400 are ovulated throughout the lifetime of a female. o The ovarian follicle becomes the growing ovarian follicle when the flat structure becomes granular and cuboidal in shape — so that the secretory granules and follicular cells become granulosa and secrete glycoproteins (which separate them from the primary oocyte — forming zona pellucida). o The granulosa then become layered and surrounded by theca cells (basement membrane) — forming the primary follicle. o The granular cells secrete a fluid which will slowly accumulate between these cells — forming the secondary ovarian follicle. This fluid forms a pool or space called the antrum, which: ▪ • 1. Forms the antral follicle (in which the antrum’s size is petite). 2. When the antrum widens and covers the entire primary oocyte and forms two layers of granulosa cells (ext. and int.) and another connects these two layers — forming the vesicular/mature/grafian follcile (big antrum) and it is the last stage that follicles exist in prior to ovulation. ▪ ▪ Recall: these changes occur at maturity so children, toddlers, and infants have primordial ovarian follicles only. Maturity is controlled by hormones: • • • • • • • The hypothalamus produces GNRH and it causes the anterior pituitary to release FSH and LH (site of action: gonads). FSH handles the first 14 days of the cycle which terminate in ovulation. Then, the sharp LH surge weakens the mature follicles’ wall at a point called stigma — rupturing the follicle and completing the first meiotic division, resulting in a secondary oocyte and first polar body (both are haploid). o Note that the sec. oocyte is surrounded by the corona radiata The rest of the mature ovarian follicles form the corpus luteum. However, the sec. oocyte, polar body, and corona radiata leave. Thus, we can say that the LH induces ovulation. The corpus luteum secretes progesterone and this continues on for about 14 days. If conception doesn’t occur, it becomes the corpus albicans. Usually, 10 to 20 follciles undergo this entire process. However, only one actually succeeds. Additionally, those who fail will form the corpus atritacum (which consists of primary oocytes unlike the other corpuses). The secondary oocyte undergoes the second meiotic division - if fertilization occurs, that is — producing: the ootid and another polar body (note that the first polar body may also produce another polar body). o o o ▪ The ootid is what will unite with the sperm and form the zygote. The zygote will migrate to and implants into the endometrium. If this process fails, the bleeding phase occurs. The Endometrial Cycle: • • • • • • • • • • • • • • The bleeding or menstrual phase: is due to ischemia and vasoconstriction. Lasts from day 1 to day 5. The proliferative phase: from day 5 to 14. The endometrium rebuilds itself — due to estrogen from the follicular cells —. The secretory phase: from day 14 to 28. Controlled by endometrial secretions (along with the glands which surround it — and which also nurture the endometrium). Prepares the corpus luteum and endometrium for implantation. The menstrual cycle normally starts when the girl is 10-14 gears old depending on many factors such as: race, geographical place, etc. The first menses is called menarche. Is anovulatory and irregular because the hormones won’t be 100% set up — this can last up to six months. Menopause is also preceded by an anovulatory and irregular phase. Normal range 17-35 days and average at day 28. It can be helpful determining the time of ovulation to have successful pregnancies. Menses symptoms can be abdominal pain (middle pain or middle schmirz) and acute hyperthermia. The embryonic testes have PGCs, seminferous or sex cords, and supporting cells. The cords have no lumen- so not tubules PGCs are surrounded by supporting cells and this can last up until delivery. The testes have PGCs and supporting cell (which later become sertoli cells or sustancular cells) at puberty: o GNRH causes the anterior pituitary to release FSH and LH — when cerebral maturity occurs. ▪ FSH matures the cord to be luminated - become a tubule - by secreting special fluids (by acting on the supporting cells) and androgens receptor synthesis. ▪ LH stimulates the Leydig cells (peripheral) to produce testosterone — which affects the androgen receptors in Sertoli cells and causes them to induce PGCs development. o Semienfirous tubules’ lumen mature during puberty o Sertoli cells produce the fluid which matures the tubules and androgen receptor proteins. [Sperm Development] • PGCs undergo cytodiffrentiation and mitosis, thus become: o o o Type A (dark color) — they are connected by cytoplasmic bridges (in all generations) and this ensures less movement of sperms before maturation ((but migrate towards the lumen as they proliferate until the late spermatid stage and the excess cytoplasm become residual bodies and the sperms are set free at this stage, and the acrosome is also made at this stage: ▪ they contain lysosomal enzymes. ▪ cap the nucleus from one end and another end makes up the neck of the sperm by means of mitochondria and centrioles — the tail matures here. then the sperms migrate to the epididymus which marks the beginning of the vas defrens; and they get their motility here and are stored here until ejaculation. Note: the last stage which contains the cytoplasmic bridges are the residual bodies — lost ctyoplasm; eaten up by Sertoli cells. o o o o o o o o o • Type B (light color) Primary spermatocytes (diploid) — but is arrested for 22 days in prophase Each PS produces two secondary spermatocytes (haploid) — complete the second meiotic division Each SS produces 4 spermatids — early which mature into late ones. Those mature by structural changes to produce sperms (by means of spermiogenesis). The entire cycle takes 74 days. Each day 300 million sperms are produced. Move from semi-infirious tubules to epididymys and they mature there. The process in which spermatids become sperms: ▪ The cytoplasm is lost to ease movement. ▪ reorientation of structures: ▪ Golgi appartus settles at one side of the nucleus and the acrosome is formed on top of it. ▪ On the other side the centrioles settle and form the neck of the sperm. ▪ The tail arises from the centriole. ▪ Caudal to the centriole the mitochondria gather to form the middle piece of the sperm. During ejaculation they move through the vas deferens by means of peristalasis towards the ejaculatory duct. Random facts: o o o o normally 100 million sperms are produced per ml. normally we produce 2-6 ml per ejaculation. minimum production is 20 million per ml or 50 million per ejaculation to reproduce but below it infertility can occur. if the latter happens they need assisted reproduction techniques: ▪ the sperm is directly injected into the secondary oocyte (intracytoplasmic injection) ▪ Note: IVF basically means fertilization outside of the body regardless of injection or not. ▪ Oligospermia is reduced sperm count. Azospermia is a zero sperm count. ▪ in this case a biopsy is taken from the testes is performed to get any sperm. Mature sperm structure abnormalities: ▪ it has two heads or two tails ▪ too big ▪ qualitative and quantitative measurements are crucial. ▪ all prevent fertilization ▪ Normally, 10% of sperms have such abnormalities but if the percentage increases they need assistance. ▪ as age increases such abnormalities increase as well During gestation female eggs outnumber male sperms but the opposite occurs during adulthood. Primary oocyte and spermatocyte are both diploid. meiosis in males result in residual bodies and 4 sperms but in females polar bodies and one egg. Causes of oligo and azospermia: ▪ varicose veins — increase temperature— and thus kill sperms. ▪ Hormonal issues such as low FSH or testosterone. Contraceptive methods: ▪ Mechanical — condoms ▪ Hormonal — pills: ▪ o o o o o o 1. some pills have progesterone only 2. some pills have both progesterone and estrogen 3. these everyday pills cause the negative feedback to affect the anterior pituitary so it stops secreting FSH and LH (gonadotropic hormones). Thus, the menses will be anovulatory and the endometrium won’t be ready for implantation. There are contraceptives for males but they are not effective. Each method has a specific failure rate In females, IUCDs are t-shaped structures covered with either copper or progesterone so that a mucus layer can be formed to prevent sperm entry and the secretory phase to occur. Surgical tubal ligation and vasectomy can be performed and are reversible but only sometimes, Sperm production: • • Glands which produce semen are: prostate, seminal vesicle (60%), bulbourethral glands — in deep perineal pouch — and those have PGs which ease the movement of sperms. The sperms move slowly in the vagina due to its acidic nature but they move quickly in the uterus due to its alkaline nature. Then, they move into the uterine tube in which their motility and sensitivity to the ovum becomes more profound due to the fact that they lose the glycoprotein layers (capacitation process). Fertilization occurs at the ampulla. • • • • • SO layers are zona pellucida and corona radiate/granulosa cells which sperms try to penetrate by secreting hyalurinidase and the uterine tube mucuss eases the process. The lacrimal reaction occurs at the zona pellucida in which the acorsome secrets the enzymes so that the sperm can trespass the area between the cell membrane and zona pellucida. Then, the cell membrane of the sperm and oocyte unite and the nucleus of the sperm is injected into the SO. Note: these cortical granules make the zona pellucida more aggressive towards other sperms (zona pellucida reaction) by secreting their contents into the membrane. The ootid stays for a couple of hours only until the sperm comes and the zygote is produced which — 24 hours later — proliferates. Note: the sex is determined at conception. [The Results of Fertilization] • • • • The secondary oocyte completed its meiotic division and produces the third polar body and the ootid. The sex is determined. Diploid member is returned. Metabolic mechanisms — for fast division. [Post-fertilization] • • • • • • 30 hours later the cells start to divide and proliferate more and prodcude smaller cells called blastomeres (note that the zona pellucida still exists). as it divides the zygote keeps moving towards the uterine cavity and when the number of cells reaches 16 they become something called the morula — almost in day 3. Then the morula undergoes the compaction process in which tight junctions are formed and the central cells of the morula (which have gap junctions) and this process produces inner cell mass (which proliferated) and the external cell mass (which didn’t). o the inner cells are also called embryoblast — which will give rise to the fetal tissues. o the outer cells are also called trophoblast — which will give rise to the placenta and supporting tissues. The process in the uterine tubes takes about 4-5 days and when the morula reaches the uterine cavity: o the endometrial fluid nurtures the morula ▪ it fills the potential space and turns it into a real one. o it then becomes the blastocyst in which the inner cells move towards the embryonic pole and the outer cells towards the abembryonic pole. o note that the zona pellucida still exists at this stage. the endometrium will be in the secretory stage so that implantation can occur. it has two layers: o the basal layer (myometrium) the functional layer (it has a very thick sublayer called the spongy layer and a less thick layer called the compact layer) at this stage the fluids cause the zona pellucida to fade away from the embryonic pole and attractive forces between the wall of the uterus and the embryonic pole so that implantation can occur at the end of week 1 — by means of a reaction between the embryonic pole and the endometrium. Note: the trophoblast is what secrets HCG — which keeps the corpus luteum functioning: progesterone secretion. when the trophoblast fuses with the endometrium the cells start to divide and their cell membranes start to fade away and become multi-nucleated; forming two subtypes: o The cytotrophoblast which has no cell membrane death. o The sensetyotrophoblast which does ▪ it is what keeps digging into the endometrium - just like osteoclasts ▪ at the end of week 1 the sensetyotrophoblast can injure the endometrial blood vessels (in the spongy layer) and the woman may falsely think that it is true menses — since it also occurs right before the normal menses timing. The functional layer comes and goes but the basal always exists. The spongy layer contains the blood vessels and the secretory part of glands. The compact layer has the gland ducts and the endings of blood vessels. o the blood vessels are spirally-shaped in the spongy layer but straight in the compact and basal layers. As the sensetyotrophoblast digs more into the endometrium the adjacent endometrial cells secrete more glycogen along with other secretions — the process is called decediual reaction — and it becomes the decidua. The zona pellucida disappears at the end of day 5. o • • • • • • • • [Further Notes on IVF] • • • • • • • Testing males for any problems is done first because their problems are easily detected. If the root cause of infertility in females is hormonal we can administer hormones. To obtain eggs to be used in IVF we can, through the posterior vaginal cortex (a space) and the aid of ultrasound technology, collect the to-be-ovulated follicles (about 5-6). ICSI helps us in injecting sperms into ova. o can be done in cases of oligo and azospermia and blocked uterine tubes. Hystersalpingography is a way to detect defects in the Fallopian tubes: o we administer shining materials into the female reproductive system and observe whether or not there are any blocks in the tubes. o it is diagnostic and can also be therapeutic. We can obtain blastomeres or the polar bodies and perform DNA tests and study genetic disorders. On average, statistics about 50% of pregnancies undergo spontaneous abortion during the first 3 months due to genetic defects. o can come and go unacknowledged.