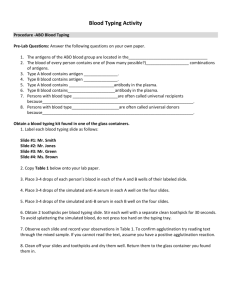
THE ABO BLOOD GROUP SYSTEM Chapter 6 KARL LANDSTEINER • Opened the doors to blood banking • Took blood from himself and 5 others • Mixed cells with each other’s serum and observed reactions. • First forward and reverse group typing ABO SIGNIFICANCE • One of the most important Blood Group Systems • Causes major transfusion problems with cell incompatibility • The only blood group system that has antibodies to antigens that are ABSENT from their RBC’s ABO TESTING: FORWARD AND REVERSE GROUPING • Forward grouping: • Using known sources of reagent antisera to detect antigens on a person’s RBC’s • Anti-A and Anti-B • Reverse grouping: • Using known sources of reagent RBC antigens to test for the person’s ABO group antibodies • Reagent cells A1 and B FORWARD TYPING KNOWN ANTISERA + UNKNOWN PATIENT CELLS REVERSE TYPING KNOWN RBC’S + UNKNOWN PATIENT SERUM GRADING REACTIONS: TUBES 4+: One solid button/Clear background 3+: 2-3 large buttons/Clear background 2+: Multiple smaller buttons 1+: Small clumps Hemolysis: Positive reactionComplement fixation Negative: Sea of red cells MIXED FIELD REACTIONS • Serum from group A persons will agglutinate group B red cells R E AC T I O N S • Antibody to B antigens present (anti-B) • Serum from group B persons will agglutinate group A red cells • Antibody to A antigens present (anti-A) • Serum from group O persons will agglutinate both A and B red cells R E AC T I O N S • Antibody to both A and B antigens present • Serum from group AB does not agglutinate either A or B red cells • Antibody to neither A or B antigens present ABO FORWARD GROUPING Patient’s RBC’s 1 2 3 4 Reaction with Anti-A Negative + Negative + (SEE CHART) Reaction with Anti-B Negative Negative + + Interpretation of Blood Group O A B AB + indicates visual agglutination ABO REVERSE GROUPING (SEE CHART) Patient’s Serum Reaction with A1 Cells Reaction with B cells Interpretation of Blood Group 1 + + O 2 Negative + A 3 + Negative B 4 Negative Negative AB + indicates visual agglutination FREQUENCY OF BLOOD GROUPS (SEE CHART) Phenotype O White % Black % Mexican % 45 49 56 Asian % 43 A1 33 19 22 27 A2 8 8 6 Rare B 10 19 13 25 A1B 3 3 4 5 A2B 1 1 Rare Rare • Naturally occurring is misnomer ABO ANTIBODY PRODUCTION • Sources of stimulation found in nature • Bacteria • Seeds from plant • Pollinating plants • Foods ABO ANTIBODIES • Unique in that it does not require introduction of foreign red cells by pregnancy or transfusion • Not present at birth • Titers not detectable until 3 to 6 months • Antibody production peaks at 5 to 10 years of age • Declines with advanced age • After 65 have low titers that may be undetectable in reverse typing OTHER BLOOD GROUPS • Some blood groups other than ABO can occasionally cause the production of antibodies without transfusion or pregnancy • These antibodies are usually IgM in type • They are not consistently present in all patients that have the recessive antigen TESTING FOR ABO • Easy to perform • Lacking the corresponding antigen serves as confirmation of the forward grouping results • Very rare (0.01% or random population) to see complete absence of Anti-A and/or Anti-B in normal, healthy individuals unless, of course, the person has AB blood type • Treacherous if wrong ABO group is given • Severe if not fatal complications ABO TYPING • Forward and Reverse typing on all patients, note reciprocal relationship of antigens and antibody (discrepancy) • O is universal donor • AB is universal recipient ABO ANTIBODIES • IgM – • Cold reacting • Bind complement (causing lysis) • Does not cross placenta • Group A and/or B individuals contain • Anti-B and/or Anti-A – IgM only (MAJORITY) • Anti-B and/or Anti-A – IgM and IgG • Anti-B and/or Anti-A – IgM, and IgA • Anti-B and/or Anti-A – IgM, IgG and IgA • IgM is always predominate • Group O individuals contain • Anti-A • Anti –B • IgG anti-A and anti-B are produced far more commonly in group O people than in group A or B people • Anti-AB ABO ANTIBODIES • Separate cross-reacting antibody that is a mixture of IgG and IgM or IgG, IgM and IgA • Crosses the placenta more frequently than anti-A or anti-B • Produced in response to exposure to A or B cells by transfusion or pregnancy • Knowing the amount of IgG anti-A, anti-B and anti-AB allows prediction or diagnosis of hemolytic disease of the newborn (HDN) caused by ABO incompatibility INHERITANCE OF ABO BLOOD GROUPS • Inherit one gene from ABO group from each parent • Chromosome 9 has one position for the ABO group • A or B refer to the phenotypes • What is detectable by testing (EXPRESSED) • AA, AO, BB, BO, OO denote genotypes • What genes are on each chromosome (EXPRESSED AND NON EXPRESSED) Parent Phenotypes Parent Genotypes Offspring Possibility A XA AA X AA AA X AO AO X AO A(AA) A(AA or AO) A(AA or AO) or O (OO) BXB BB X BB BB X BO BO X BO B (BB) B(BB OR BO) B(BB or BO) or O (OO) AB O G ROUP S OF T H E OFFSP R I NG FROM VAR I OUS P OSSI B L E AB O MATI NG S ( SE E CH ART ) Parent Parent Phenotypes Genotypes Offspring Possibility Pheno & Genotypes AB X AB AB X AB AB(AB) OR A (AA) OR B (BB) OXO OXO O(OO) AA X BB AO X BB AA X BO AO X BO AB(AB) AB(AB) or B(BO) AB(AB) or A(AO) AB(AB) or A(AO) OR B(BO) OR O (OO) AXB AB O G ROUP S OF T H E OFFSP R I NG FROM VAR I OUS P OSSI B L E AB O MAT I NG S ( SE E CH ART ) FORMATION OF A, B, H ANTIGENS • A, B, and H antigens are not fully developed at birth • Development begins at 6 weeks of fetal life • Not fully developed until 2-4 years old • ABO genes do not actually code for the production of ABH • Code for enzymes (glycosyltransferases) that add sugars to basic precursor substances on the red blood cell • H gene is inherited independently from ABO genes FORMATION OF A, B, H ANTIGENS • H is the backbone on which other genes are expressed • H gene is found on Chromosome 19 INTERACTION OF HH AND ABO GENES • Inheritance of at least one H gene causes production of enzyme (alpha-2-L-fucosyl-transferase) that transfers a sugar • Genotype HH or Hh is possible (h is an amorph of H) • Gene is found on Chromosome 19 INTERACTION OF HH AND ABO GENES • H gene is known as FUT-1 gene • 99.9% of population has the H gene • “h” amorph is very rare – known as the Bombay phenotype • Lacks normal expression of ABH antigens even though person has A and B genes INTERACTION OF HH AND ABO GENES • H substance MUST be formed for other sugars to be attached to the RBC (regardless to the inherited A or B gene) • Bombay people are devoid of all ABO antigens • Bombay types contain Anti-A, -B, -AB & -H • They can only be transfused with another Bombay type ABO ANTIGENS 1. The blood group is determined by the terminal sugars on the membranes of their red cells. 2. If neither the A or B gene is present “the O condition” the antigen is H 3. In the presence of the B gene, the sugar galactose is added 4. In the presence of the A gene, the sugar N-acetyl galactosmine is added TERMINAL SUGAR PLACEMENT Antigen Structure Minimal determinant structure H B A *: residue could be glucose in case of glycolipids; yellow shade: minimal determinant or core structure; blue arrow: residue added by blood group gene product; examples of type 1 and 2 core structures are illustrated above but they can vary widely, as they can be assembled on at least six possible types of carbohydrate chains; they can reside on a variety of protein or lipid glycan structures containing branches, repeats, etc. ABO ANTIGENS ABO Grp Substance In Saliva A B H O NONE NONE ++ A ++ NONE + B NONE ++ + AB ++ ++ + * Non-secretors (sese) will have NO ABH substances in saliva FOR MATI ON OF A, B AND H SOL UB L E ANT I G E NS • The presence of ABH soluble antigens can also be found in all body secretions IF they inherit the Se gene. • Those who inherit the SeSe or Sese gene will secret these soluble antigens in body fluids. If they inherit the sese gene, they will not be secretors. 1911 discovery of 2 types of A antigen A1 and A2 make up 99 percent of all A groups ABO SUBGROUPS A1 reacts with both Anti-A and Anti-A1 sera A2 reacts with only Anti-A sera 80 % of all Group A (or AB) are A1 (or A1B) Note: Anti-A1 sera is NOT the same as A1 cells ABO SUBGROUPS • Antigens present on the RBC surface of A1 and A2 are presented in two ways: • Group A1: A and A1 antigens • Group A2: A antigen only • Characteristics of A1 & A2 are found in Table 6-14 (page 131) • Reactivity of anti-H antisera or anti-H lectin with the different ABO blood groups (figure 6-11) _____ > _____ > B > ______ > ______ > ______ ADDITIONAL WEAK A SUBGROUPS • A3 – demonstrates a mixed field pattern with anti-A and most of anti-B • Ax – will not be agglutinated by anti-A reagent but will agglutinate with anti-AB reagent. WEAK B SUBGROUPS • Very rare; less frequent • Recognized by variations in the strength of reaction using anti-B and Anti-A,B. • B3, Bx, Bm and Bel • See table 6-15 for characteristics of the B Phenotypes BOMBAY PHENOTYPE (OH) • First reported in 1952 in Bombay, India • Inheritance of a double dose of the “h” gene producing the very rare genotype hh. • Causes the ABO genes NOT to be expressed (No H gene = No place for sugars to attached) • RBCs are void of normal ABH antigens and fail to react with anti-A, anti-B and anti-H • Would phenotype as O blood group • See Box 6-6 & 6-7 for Bombay Characteristics ABO DISCREPANCY • Unexpected reactions in the forward and reverse results of an ABO blood group typing. • The forward grouping does not correspond to the results of the reverse grouping OR • There is abnormal reactivity present (i.e. mixed field reaction) Discrepancies can be due to technical error ABO DISCREPANCY • Cell suspension too heavy or too light • Clerical errors • Missed hemolysis • Failure to add reagents Discrepancies can be due to other factors. • • • • • Patients age Diagnosis Previous transfusion Medication Previous pregnancy ABO DISCREPANCY: 4 GROUPS • Group 1 • Associated with unexpected reactions in the reverse grouping due to weakly reacting or missing antibodies • Group 2 • Associated with unexpected reactions in the forward grouping due to weakly reacting or missing antigens • Group 3 • Associated with discrepancies between forward and reverse grouping caused by protein or plasma abnormalities resulting in rouleaux formation. • Group 4 • Associated with discrepancies between forward and reverse grouping due to miscellaneous problems. ABO DISCREPANCY – GROUP 1 Causes of Group I Discrepancies Newborns: Lack antibodies Elderly: Depressed Antibodies Resolve Group I Discrepancies GOAL: Enhance weak or missing reaction Leukemia 1. Immunosuppressive Drugs ABO Subgroups Bone Marrow Transplants & Plasma Transfusions Incubate at Room Temperature for 15 – 30 minutes & centrifuge 2. If there is still no reaction, then incubate at 4° for 15 – 30 minutes & centrifuge Always remember to use an auto and O cell control with reverse typing ABO DISCREPANCY – GROUP 2 Causes of Group II Discrepancies Subgroups of A OR B Leukemia weakened A or B antigens Hodgkin’s disease Resolve Group II Discrepancies GOAL: Enhance weak or missing reaction 1. Incubate at Room Temperature for 15 – 30 minutes & centrifuge 2. If there is still no reaction, then incubate at 4° for 15 – 30 minutes & centrifuge “Acquired B” phenomenon 3. RBC’s can be treated with enzymes and retested with antisera. In the case of suspected “Acquired B”, treat RBC’s with acetic anhydride reacetylates and retest. ABO DISCREPANCY – GROUP 3 Causes of Group III Discrepancies Elevated levels of globulin-multiple myeloma, Waldenstroms macroglobinemia Elevated levels of fibrinogen Plasma expanders such as dextran and polyvinylpyrrolidone Resolve Group III Discrepancies GOAL: Remove interfering substance 1. Perform a saline dilution or saline replacement to free cells Wharton’s jelly in cord blood samples 2. Wash cells 6 – 8 times with saline to alleviate the rouleaux due to Wharton’s jelly ABO DISCREPANCY – GROUP 4 Causes of Group IV Discrepancies Resolve Group IV Discrepancies Cold reactive autoantibodies GOAL: Eliminate spontaneous agglutination Circulating RBC’s of more than one ABO group due to transfusion or transplant 1. Forward: Incubate at 37° for a short time and then wash at 37° 3 times and retype Unexpected ABO isoagglutinins Unexpected non-ABO alloantibodies 2. Reverse: Warm to 37° mix and test at 37° * If forward doesn’t resolve with 1, then treat patient’s cells with DTT. * If reverse doesn’t resolve with 2, try an autoabsorbtion from the serum and then use the absorbed serum to repeat the typing at room temperature . HOMEWORK • CHAPTER 6 • Review ABO discrepancies and case study (PGS. 136-145) • Review ABO Discrepancy Tutorial online and case studies