Maternity - Labour and Birth Risk and Postpartum Quick Note
advertisement

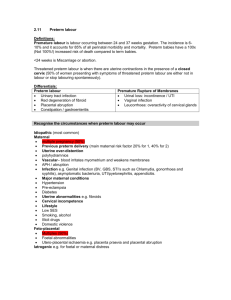
Week 4 CAN – L&B Risk and Postpartum Preterm Labour and Birth Preterm vs Low-birth weight time of birth < 2500 g not weight Preterm labour Cervical changes and uterine contractions occurring btwn 20-37 weeks of pregnancy Preterm birth: Any birth that occurs before 37 weeks of preg Causes: Infections Idiopathic preterm births Sociodemographic factors poverty, low education, lack of social support, smoking, Ø prenatal care, intimate partner violence, stress Predicting preterm labour and birth Biochemical markers – Fetal fibronectins Endocervical length Nursing Care Management: Prevention Prevention strategies to address risk factors Education aims at health promo and disease preventions Educate about preterm labour signs Teach what to do if symptoms occur Women may ignore b/c of ignorance or they think it is expected Bed rest Early Recognition Gestational age between 20-37 weeks Uterine activity (contractions) Progressive cervical change (effacement 80%, dilation >2cm) Lifestyle modifications These activities should be curtailed Sexual activity Riding long distances (car or bus) Carrying heavy load Standing >50% of time Heavy housework Climbing stairs Hard physical work Unable to stop and rest when tired Tocolytics – to suppress uterine activity Afford opportunity to administer antenatal glucocorticoids Accelerate fetal lung maturity Not indicated if: Cord prolapse, chorioamnionitis, Abruptio Placentae Reduce severity of sequalae in preterm births Management of Inevitable Preterm Birth Labour progressed to cervical dilation 4cm → preterm birth Preterm birth in tertiary care centres lead to better outcomes Women at risk be transferred quickly – give antenatal glucocorticoids before transfer Preterm Premature Rupture of Membranes (PPROM) Membrane ruptures before 37 weeks gestation Often preceded by infections Cause unknown Women complains of sudden gush or slow leak of vaginal fluid Dystocia abnormal slow progress of labour > 4 hours of < 0.5cm per hour of cervical dilation in active lab Dysfunctional labour from abnormal uterine contractions Cervical dilation, effacement, descent Factors than can increase risk for uterine dystocia: Body build Uterine abnormalities Malpresentation and position of fetus Cephalopelvic disproportion (CPD) Overstimulation with oxytocin Factors that can increase risk for dystocia: Maternal fatigue, dehydration, E imbalance, fear Inappropriate timing of analgesic or anaesthetic admin Dysfunction of uterine contractions Hypertonic or primary dysfunctional labour Hypotonic or secondary uterine inertia Pelvic dystocia contractures of pelvic diameter that reduce capacity of bony pelvis, inlet mid-pelvis or outlet Soft Tissue Dystocia results from obstruction of birth canal by anatomical abnormality other than bony pelvis Psychological responses – body’s response to stress → dystocia Abnormal Labour Patterns precipitous - < 3h from onset of contractions Post term Pregnancy, Labour, and Birth Maternal risk excessively large infant Increased risk: dysfunctional labour, birth canal trauma Interventions likely to be necessary Fatigue and psychological reactions Fetal Risks Prolonged labour Shoulder Dystocia Birth trauma Asphyxia from macrosomia Compromising effects of an aging placenta Nursing Care Management Controversial Suggest induction at 41-42 weeks, while other up to 43 weeks With assessment of fetal well-being normal Version Internal version and External Cephalic Version Trial of labour Inductions or augmentation Stimulation of uterine contractions after labour has started but progress is unsatisfactory Oxytocin infusion, amniotomy, nipple stimulation Oxytocin use Special caution: Multifetal presentation, breech presentation, part above pelvic inlet, abnormal FHR, polyhydramnios, grand multiparity, history of c-section, maternal cardiac disease Cervical ripening methods Chemical agents – prostaglandins Amniotomy Mechanical methods Forceps-assisted birth Maternal indications Shorten second stage in event of dystocia Compensate for deficient expulsive efforts Reverse a dangerous condition Fetal indications Distress or certain abnormal presentations Arrest of rotation Delivery of head in a breech presentation Vacuum-assisted birth Attachment of vacuum cup to fetal head, using negative pressure to assist birth of head Risk to newborn of cephalohematoma, scalp lacerations, subdural hematoma Week 4 CAN – L&B Risk and Postpartum Caesarean birth Immediate postop care Pain relief and discharge teaching/planning Vaginal birth after section Shoulder Dystocia Head is born but should is stuck, likely NB experience injury Mother’s primary risk from excessive blood loss b/c laceration, extension of episiotomy or endometritis Prolapse umbilical cord cord lies below presenting part of fetus Long cord, malpresentation (breech) transverse lie, unengaged presentation part Ruptured Uterus VERY SERIOUS OB INJURY Caused by separation of scar of prev C-section, uterine trauma, congenital uterine anomaly Amniotic fluid embolism Sudden death debris enter CV system Triggers a rapid complex series of patho events Post Partum Period Period after 4th stage of labour and lasts 6 weeks (varies) Uterus Involution: return or uterus to nonpregger state Fundus descends 1-2 cm every 24 hours Subinvolution: failure of uterus to return common causes retained placental pieces or infection Contractions Oxytocin released (b/c breastfeeding) strengthen and coordinate uterine contractions, (afterpains) Cervix Soft immediately after birth Within 2-3 days, it is shorted Lacerations delay production of estrogen which influences cervical mucus production → ↑risk for infection Vagina and perineum gradually returns to size by 6-10 weeks episiotomies heal within 2-3 wks hemorrhoids and anal varicosities are common Recommend Kegel exercises – 6 months to regain tone Abdomen Abd wall is relaxed – still looks pregnant return takes about 6 wks Placental Hormones expulsion of placenta → dramatic changes to hormone levels ex. Significantly lower blood sugar levels estrogen and progesterone levels drop lowest @ 1 wk Pituitary hormones and ovarian function lactating and non lactating women differ in timing of first ovulation and menstruation when lactating, serum prolactin levels remain elevated and suppress ovulation 70% of non-breastfeeding mothers menstruate within first 12 weeks Urine Components no more glycosuria May have lactosuria in lactating women Elevated BUN due to autolysis of involuting uterus Diuresis Within 12 hours of delivery Profuse often occurs at night for first 2-3 days Urethra and bladder Full bladder can displace uterus → excess bleeding Decrease urge to void → encourage scheduling void q2hr Appetite Most new mother are very hungry If BF, ensure moms know to eat for more nutrients for both baby and herself - elf Care momma Bowel evacuation spontaneous bm may take 2-3 days offer laxative to help with the first bm Breasts Breastfeeding mothers Before lactation, a yellowish fluid, colostrum can be expressed Tenderness may persist for 48 hours after start of lactation Non Breastfeeding moms Engorgement can occur but also resolves spontaneously Cool ice pack, fresh cabbage leaves to reduce swelling Blood Volume Returns to normal 2 weeks post partum Decreases due to Blood loss in childbirth Diaphoresis and diuresis within first 2-3 days Elimination of placenta, diverting 500-750 mls of blood Rapid reduction in sze of uterus = more blood into CV system Cardiac Output Remains increased for 48hrs after childbirth CO generally returns within 6 wks, SV+end-diastolic volume+SVR = remain elevated for 12 weeks Vitals HR and BP normal within few days Respiratory function to normal by 6-8 days Risk for orthostatic hypotension for 48 hr d/t engorgement of organs Blood Components Hemoglobin and hematocrit: ↑ up to 72 hours WBC count: elevated 10-14 days w/o infection then to norm Coagulation: normally elevated during pregnancy, ↑ DVT risk Post Partum Chill first 2 hours uncontrollable shaking Offer warm blanket and reinforce it is normal Headaches – careful assessment may be caused by PIH, stress, and leakage of cerebrospinal fluid into extradural space during epidural or spinal anesthesia Hyperpigmentation of areolae and linea nigra and varies whether it fades or not Immune system Mom may need rubella vaccine or Rho(D) to prevent RH isoimmunization Nursing care focuses on transition to parenting Woman’s physiological recovery Psychological well-being Impact of birth experience Maternal self-image Adaptation to parenthood Family structure and functioning Impact of cultural diversity Ability to care for herself and baby Needs of other family members, strategies in plan of care to assist family in adjusting to baby Discharge teaching self-management and signs of complication sexual activity and contraception prescribed medications routine mother and baby check ups