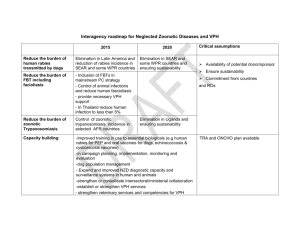
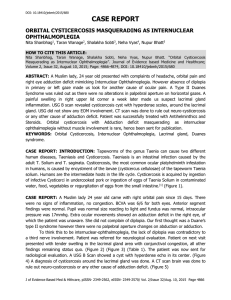
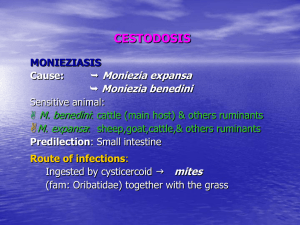
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/284355667 Oral cysticercosis: A rare case presentation with ultrasound and MRI findings Article · January 2015 DOI: 10.4103/0972-1363.170178 CITATIONS READS 3 640 4 authors, including: Revath Vyas Devulapalli Lakshmi Kavitha Nadendla Legacy clinics, KIGALI, Rwanda kamineni institute of dental sciences 4 PUBLICATIONS 18 CITATIONS 20 PUBLICATIONS 115 CITATIONS SEE PROFILE All content following this page was uploaded by Revath Vyas Devulapalli on 07 December 2016. The user has requested enhancement of the downloaded file. SEE PROFILE [Downloaded free from http://www.jiaomr.in on Wednesday, December 07, 2016, IP: 41.216.97.34] Case Report Oral cysticercosis: A rare case presentation with ultrasound and MRI findings Revath Vyas Devulapalli, Balaji Babu Bangi, Lakshmi Kavitha Nadendla, Archana Pokala Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India ABSTRACT Taenia solium, the larvae of pork tapeworm, can cause the parasitic infection known as cysticercosis. It is commonly seen in developing countries. The World Health Organization estimates that over 50,000 deaths per year are caused by neurocysticercosis worldwide. It can occur anywhere in the body. Cysticerci in the muscles generally do not cause symptoms; they present as nodules and can be felt as lumps under the skin or they can present as muscular pseudohypertrophy. The condition rarely involves musculature of the orofacial region and presents a difficulty in clinical diagnosis. Here, we present a case report of a healthy middle-aged female patient who had a painless swelling below the lower lip. The ultrasound examination revealed an intramuscular cysticercosal cyst. The diagnosis was confirmed using magnetic resonance imaging and by histopathology. The case was managed by conservative enucleation of the cyst. Key words: Cysticercosis, diagnosis, magnetic resonance imaging, Taenia solium, ultrasonography T Introduction aenia solium or pork tapeworm, a cyclophyllid cestode, has three distinct morphological verities.[1] Of these, cellulose cysticercus type has a fluid-filled bladder with an invaginated scolex. Human beings are infected by eating uncooked or partially cooked pork, which is an intermediate host for cysticercus cellulose. Sometimes humans act as intermediate hosts, where eggs laid by larva develop in the alimentary tract. They may enter the alimentary tract as a result of retroperistalsis or by having food or by using hands contaminated with those eggs.[2] Encystment of larvae can occur in the central nervous system, subcutaneous tissue, striated muscle, and rarely in other tissues. High muscular activity and metabolic Access this article online Quick Response Code: Website: www.jiaomr.in DOI: 10.4103/0972-1363.170178 rate of oral tissues in humans might act against the lodgment and development of cysticercosis in this location.[3] Here, we present one such rare presentation of oral cysticercosis in the mentalis muscle. Case Report A healthy, 30-year-old female patient visited the outpatient department with the complaint of a painless firm, non-tender swelling measuring approximately 2 cm × 2 cm on the left side, below the lower lip [Figure 1]. The swelling was present since 5 months. Swelling was sudden in onset and gradually increased in size for This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms. For reprints contact: reprints@medknow.com How to cite this article: Devulapalli RV, Bangi BB, Nadendla LK, Pokala A. Oral cysticercosis: A rare case presentation with ultrasound and MRI findings. J Indian Acad Oral Med Radiol 2015;27:322-6. Address for correspondence: Dr. Revath Vyas Devulapalli, Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Nalgonda District, Telangana, India. E-mail: revath.vyas@gmail.com Received: 04-12-2015 Accepted: 12-10-2015 Published: 21-11-2015 322 © 2015 Journal of Indian Academy of Oral Medicine and Radiology | Published by Wolters Kluwer - Medknow [Downloaded free from http://www.jiaomr.in on Wednesday, December 07, 2016, IP: 41.216.97.34] Devulapalli RV et al.: Oral cysticercosis 2 months. Later, it remained constant in size. There were no palpable cervical lymph nodes. The patient had no headache, seizure, or any focal neurological deficit. There was no family history of similar complaints in other family members. Patient consumes mixed diet, but never consumed pork. Intraorally, the swelling was causing obliteration in the vestibular region of 32, 33, and 34 [Figure 2]. The lesion appeared to be peripheral in origin, well encapsulated, present subcutaneously, freely mobile, and not attached to the underlying periosteum. Based on these clinical features, pre-operative provisional diagnosis of fibroma was made. Under differential diagnosis, lesions such as lipoma, pleomorphic adenoma, and peripheral adenomatoid odontogenic tumor were considered. Fibroma was considered because it is the most common benign connective tissue tumor and can occur anywhere in the oral cavity as a firm, painless swelling in the 3rd to 5th decade of life. But generally it occurs as a reactive lesion rather than a benign tumor, and it more commonly occurs on the buccal mucosa and tongue as a pedunculated mass. Lipoma was considered because it can occur more commonly in females as a painless swelling with a smooth surface. Yellowish color and slip sign that are characteristic of superficially present lipoma were not seen in this case. Pleomorphic adenoma in the lower vestibule is unusual, but may develop from the lower lip and extend into the vestibule. Peripheral odontogenic lesions are very rare, but can occur close to soft tissues adjacent to the tooth apparatus. Conventional radiographs like periapical radiographs, mandibular cross-sectional occlusal radiograph, and orthopantomograph showed no bony changes, confirming the lesion to be peripheral. On ultrasound examination (USG), there was a well-defined hypoechoic area measuring 1.75 cm × 1.8 cm and containing a small echogenic mass at one end close to the bone [Figure 3]. The USG picture suggested a benign, thick-walled cystic lesion surrounding a nidus. This nidus most probably appeared to be the scolex of the larva. Based on the USG, a probable diagnosis of cysticercosis in the left mentalis muscle was made. To check for any bony involvement, computed tomography (CT) of the mandible was performed. To exclude the possibility of any involvement of brain and other orofacial regions, magnetic resonance imaging (MRI) was performed. The CT showed [Figure 4] hypodense lesion within the soft tissues causing scalloping of the cortical bone, which may be a pressure indentation caused by the lesion. Figure 2: Intraoral photograph showing solitary diffuse swelling in the lower lip causing vestibular obliteration Figure 1: Extraoral photograph showing solitary diffuse swelling in the chin region on the left side Figure 3: Ultrasound image showing a well-defined hypoechoic (H) area with an echogenic nidus (E) at one end suggestive of larval head or scolex Figure 4: Axial and sagittal sections of T1 MRI picture showing hypointense lesion in the mentalis region with an eccentrically placed hyperintense nidus seen in axial section suggestive of scolex of the larva Journal of Indian Academy of Oral Medicine & Radiology | Apr-Jun 2015 | Vol 27 | Issue 2 323 [Downloaded free from http://www.jiaomr.in on Wednesday, December 07, 2016, IP: 41.216.97.34] Devulapalli RV et al.: Oral cysticercosis The MRI showed a lesion within the mentalis muscle, which was hypointense in T1 [Figure 5] and hyperintense in T2 [Figure 6], suggestive of fluid within the lesion. Scolex of the larva was better seen in T1 images as a hyperintense nidus close to the alveolar bone. No evidence of disseminated or intracranial cysticercosis was found in the MRI. The findings in MRI supported cysticercosis as a radiological diagnosis. A mucosal incision [Figure 7] was given to expose the mass which was translucent. Mentalis muscle fibers were resected and the cystic mass was separated from all the muscle attachments with utmost care, and complete enucleation of the cyst [Figure 8] was done. The specimen was sent for histopathology. Gross specimen [Figure 9] was approximately 2 cm × 2 cm in diameter. When the specimen was cut open, it yielded plain water-like fluid, which was fixed on a slide for cytological examination. The inner surface of the specimen was white in color and showed the scolex of the larva as an evagination from the cystic wall [Figure 10]. Cytological examination of the cystic fluid showed no associated inflammatory component. Microscopic examination of the cystic lining showed well-defined host capsule surrounding the cyst and artifactual space created by shrinkage of the larvae [Figure 11]. Host capsule showed duct-like invaginations and inflammatory cell infiltrate [Figure 12]. With these characteristic histological findings, a definitive diagnosis of cysticercosis was made. As a precaution and to treat any disseminated infection, anti-helminthic drug albendazole 400 mg twice daily was prescribed for 28 days and a periodic follow-up was advised.[4] Patient is under follow-up, with no recurrence and with no other complaint. Discussion Cysticercus cellulosae is a rare condition in human beings. Oral cysticercosis is still rarer and up to 2010, only 135 cases were reported in the English literature. [5] Oral cysticercosis usually manifests as painless, nodular masses. Most of the cases reported in the literature presented with such painless, nodular masses. [4] Cysticercosis is rarely included in the pre-operative differential diagnosis due to the relative rarity of the condition, inadequate knowledge of parasitic infections and their oral manifestations, and most importantly, due to negligence at the time of taking the medical history. Modern radiological modalities such as USG, CT, and MRI are very effective in detecting cysticerci pre-operatively. [6] Except for a Figure 5: Axial and coronal sections of T2 MRI picture showing a well-defined hyperintense lesion within the mentalis muscle Figure 6: Axial section showing scalloping and 3D CT section showing depression on the labial surface of mandible caused by the overlying well-defined hypodense lesion Figure 7: Photograph showing surgical incision exposing the underlying translucent lesion 324 Figure 8: Photograph showing enucleation of the cyst Journal of Indian Academy of Oral Medicine & Radiology | Apr-Jun 2015 | Vol 27 | Issue 2 [Downloaded free from http://www.jiaomr.in on Wednesday, December 07, 2016, IP: 41.216.97.34] Devulapalli RV et al.: Oral cysticercosis Figure 9: Gross specimen of size approximately 20 mm × 20 mm × 15 mm Figure 11: Microscopic examination of the cystic lining showing well-defined host capsule surrounding the cyst and artifactual space created by shrinkage of the larvae few cases in which fine needle aspiration cytology was performed pre-operatively, [7] almost all the reported lesions had been diagnosed as cysticercosis only after histopathologic examination. Our case was one such case diagnosed pre-operatively based on USG and MRI. In this case report, we emphasize the importance of radiological examination for a proper pre-operative diagnosis. The diagnostic feature of a cysticercus granuloma is the presence of an oval or rounded well-defined hypoechoic cystic lesion with smooth walls and an eccentric hyperechoic nidus representing the scolex within. The cyst, particularly the scolex, may be better visualized by USG than MRI, in muscular lesions. [8] Diagnosis can be done precisely with various serological laboratory methods. [9,10] Laboratory findings in patients with cysticercosis reveal eosinophilia, raised immunoglobulin E (IgE), and most importantly, a positive enzyme-linked immunosorbent assay (ELISA) test against cysticercus cellulosae. In our case, no specific laboratory investigations for cysticercosis were Figure 10: Cut section of the gross specimen showing milky white internal wall, thin transparent membrane, and larval head Figure 12: Histopathology showing host capsule with duct-like invaginations and inflammatory cell infiltrate done as the diagnosis was confirmed by radiological investigations. Histopathologic examination is the gold standard for the diagnosis of cysticercosis. Histopathologic examination helps in the diagnosis of cysticercosis by the detection of a cystic space containing the cysticercus cellulosae. After a period of about 3 years, the larva dies and after about another 2 years, the cyst undergoes calcification, which may also be appreciated on radiographs as rice grain type of calcifications.[11] Fine needle aspiration cytology can also aid in diagnosis as reported in some series, but is subject to sampling error and may fail to confirm the diagnosis.[7] Treatment includes medical and surgical modalities. The management of cysticercosis is also site-dependant. Drugs such as praziquantel (50 mg/kg/day in three doses for 15 days) and albendazole (15 mg/kg/day in three doses for 28 days) are potent antihelminthics used in the treatment of cysticercosis. Praziquantel, Journal of Indian Academy of Oral Medicine & Radiology | Apr-Jun 2015 | Vol 27 | Issue 2 325 [Downloaded free from http://www.jiaomr.in on Wednesday, December 07, 2016, IP: 41.216.97.34] Devulapalli RV et al.: Oral cysticercosis however, has no effect on calcified parasites.[12] Since both albendazole and praziquantel provoke inflammatory responses, patients receiving either drug should be hospitalized and given high doses of glucocorticoids. Surgical excision of accessible solitary lesions is still the “gold standard” of treatment, with no evidence of recurrence reported.[13] Conclusion In spite of better diagnosis and prompt treatment, precautions have to be taken for the prevention of cysticercosis, which may be even fatal with unusual complications. The major means of preventing infection is the adequate cooking of pork, decreasing the opportunities for ingestion of fecally derived eggs by means of good personal hygiene, effective fecal disposal, and treatment and prevention of human intestinal infections. Financial support and sponsorship Nil. Conflicts of interest There are no conflicts of interest. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. References 1. Rabiela M, Rivas A, Flisser A. Morphological types of Taenia solium cysticeci. Parasitol Today 1989;5:357-9. 326 View publication stats 13. Garcia HH, Del Brutto OH. Taenia solium cysticercosis. Infect Dis Clin North Am 2000;14:97-119, ix. Jay A, Dhanda J, Chiodini PL, Woodrow CJ, Farthing PM, Evans J, et al. Oral cysticercosis. Br J Oral Maxillofac Surg 2007;45:331-4. Sethi PK, Sethi NK, Torgovnick J, Arsura E. Cysticercosis of temporalis muscle: An unusual cause of temporal headaches. A case report. J Headache Pain 2007;8:315-6. Gadbail, AR, Korde S, Wadhwan V, Chaudhary M, Patil S. Oral cysticercosis: Report of two cases with review of literature. Oral Surgery 2010;3:51-6. Richards F Jr, Schantz PM. Laboratory diagnosis of cysticercosis. Clin Lab Med 1991;11:1011-28. Saran RK, Rattan V, Rajwanshi A, Nijkawan R, Gupta SK. Cysticercosis of the oral cavity: Report of five cases and review of literature. Int J Paediatr Dent 1998;8:273-8. Jankharia BG, Chavhan GB, Krishnan P, Jankharia B. MRI and ultrasound in solitary muscular and soft tissue cysticercosis. Skeletal Radiol 2005;34:722-6. Delgado-Azañero WA, Mosqueda-Taylor A, Carlos-Bregni R, Del Muro-Delgado R, Díaz-Franco MA, Contreras-Vidaurre E. Oral cysticercosis: A collaborative study of 16 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:528-33. Diaz Camacho SP, Candil Ruiz A, Suate Peraza V, Zazueta Ramos ML, Felix Medina M, Lozano R, et al. Epidemiologic study and control of Taenia solium infections with praziquantel in a rural village of Mexico. Am J Trop Med Hyg 1991;45:522-31. Kinnman J, Chi CH, Park JH. Cysticercosis in otolaryngology. Arch Otolaryngol 1976;102:144-7. Singh S, Sreenivasan V, Garg K, Wazir ND, Rajput JS, Sandhu Virk P. Cysticercosis involving muscle of mastication: A review and report of two cases. Case Rep Dent 2013;2013:814126. Subramanian B, Krishnaraj S, Agrawal K, Soundararagavan J. Cysticercosis of the oral cavity: An often misdiagnosed entity. J Laryngol Otol 2008;122:1005-7. Journal of Indian Academy of Oral Medicine & Radiology | Apr-Jun 2015 | Vol 27 | Issue 2