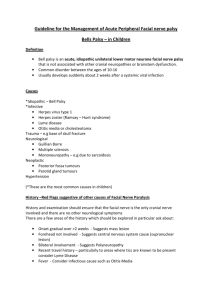
What causes Bell’s palsy? Bell’s palsy occurs when the seventh cranial nerve becomes swollen or compressed, resulting in facial weakness or paralysis. The exact cause of this damage is unknown, but many medical researchers believe it’s most likely triggered by a viral infection. The viruses/bacteria that have been linked to the development of Bell’s palsy include: herpes simplex, which causes cold sores and genital herpes HIV, which damages the immune system sarcoidosis, which causes organ inflammation herpes zoster virus, which causes chickenpox and shingles Epstein-Barr virus, which causes mononucleosis Lyme disease, which is a bacterial infection caused by infected ticks It is believed to be due to a swelling of the nerve that controls the muscles of the face. It can be worrying, but most people make a full recovery how it occurs ? Most doctors believe that it’s due to damage to the facial nerve, which causes swelling. This nerve passes through a narrow, bony area within the skull. When the nerve swells -- even a little bit -- it pushes against the skull's hard surface. This affects how well the nerve works Researchers have long believed that viral infections may also play a role in the development of Bell's palsy. They’ve found evidence that suggests the herpes simplex 1 virus (a common cause of cold sores) may be responsible for a large number of cases. Facial nerve AltWith Bell's palsy, the nerve that controls your facial muscles, which passes through a narrow corridor of bone on its way to your face, becomes inflamed and swollen — usually related to a viral infection. Besides facial muscles, the nerve affects tears, saliva, taste and a small bone in the middle of your ear. Other commonly mentioned triggers include: stress, trauma, fever, and tooth extractions. . Who gets it? Bell's palsy afflicts approximately 40,000 Americans each year. It affects men and women equally and can occur at any age, but it is less common before age 15 or after age 60. It disproportionately attacks people who have diabetes or upper respiratory ailments such as the flu or a cold. Assessment of bell's palsy :_ In patients presenting with facial weakness, the first priority is to exclude an upper motor neurone lesion; important associated signs may include concurrent limb weakness, hyper-reflexia, upgoing plantars, or ataxia Check for causes of a lower motor neurone lesion by examining the ears, mastoid region, oral cavity, eyes, scalp, and parotid glands Bell’s palsy is a diagnosis of exclusion, and oral steroids are needed within 72 hours to increase the chance of complete recovery. Prognosis is usually good compared with other causes of lower motor neurone weakness, such as tumours and Ramsay Hunt syndrome Eye protection is crucial if lid closure is impaired The facial nerve is responsible for motor supply to the muscles of facial expression (frontalis, orbicularis oculi, buccinators, and orbicularis oris) and stapedius, parasympathetic supply to the lacrimal and submandibular glands, and sensory input from the anterior two thirds of the tongue. Thus, as well as a facial droop, patients may present with a dry eye, reduced corneal reflex, drooling, hyperacusis, altered taste, otalgia, and speech articulation problems.5 Upper motor neurone After identifying the affected side, it is important to establish whether an upper motor neurone lesion is responsible for the facial weakness. Although not an infallible sign,3classic neurology describes a bilateral innervation of that part of the facial nuclei supplying the forehead, and thus preserving forehead movement in upper motor lesions. Lower motor neurone disorders of the main nerve trunk result in a weakness of the entire side of the face. Patients may have risk factors for stroke, which include older age (>60 years), hypertension, previous stroke or transient ischaemic attack, diabetes, high cholesterol, smoking, and atrial fibrillation.6Corroborative evidence may also be found by examining for abnormalities in other cranial nerves and the peripheral nervous system—increased tone, limb weakness, hyper-reflexia, upgoing plantars, and sensory loss.4 When an upper motor neurone lesion is suspected, it may help to determine whether this is localised to the brainstem or cerebral cortex. Brainstem disease may present with vertigo, ataxia, or crossed neurology signs (ipsilateral cranial nerve involvement and contralateral hemiplegia). A cortical lesion often affects the contralateral limbs and involuntary movements of the face, such as spontaneous smiling, may be spared.6Urgent referral to secondary care (neurology or acute medical unit) is needed at this stage to assess the need for thrombolysis. Lower motor neurone PHYSICAL EXAMINATION