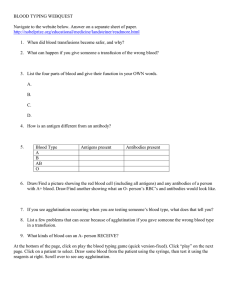
Week 1/ ABO and Rh blood group systems H and ABO blood group system [Hh system] H gene is dominant, h gene is recessive H gene 100% in all population hh gene approx. 1 in 106 caucasian abnormal phenotypes e.g. Bombay and para-bombay group due to point mutation in H gene H antigen is the precursor for production of A and B antigens H antigen Type 1 found in secretion, plasma, adsorbed to RBCs Type 2 found in RBC membranes Type 3 found in mucin, repetitive structure, RBCs Type 4 found in glycolipids on kidney and RBCs Membrane associated form of antigen is a glycosphingolipid Low expression at birth and increase as branched forms later in life Amount of H antigen expressed is determined by A and B gene and efficiency of resultant glycosyl transferase O > A2 > B > A2B > A1 > A1B > Oh Type 1 H antigen (product of secretor gene) in secretions is a glycoprotein Membrane and soluble forms if Se gene inherited Found on most cells in body Present in gram negative bacteria as membrane associated and soluble lipopolysaccharide Found on cells of other animal species Histo-blood group (associated with cell interaction and tissue development) Infections O blood group protection against P. falciparum, pancreatic Ca but susceptible to Y pestis (plague) A blood group more susceptible to smallpox, high level of coagulation proteins and thromboembolism B blood group more susceptible to gonorrhoea, S. pneumoniae, E.coli H abnormal phenotypes Para-bombay groups Single point mutation in H gene lead to fructosyl transferase defect Results in reduced H antigen production leading to reduced A and/or B antigen expression Ah, Bh or ABh, OH Antibodies and serology Alloantibody is very rare, only found in Bombay and some para-bombay individuals Autoantibodies is common, most often found in compound anti-IH in A1 pregnant women Usually IgM cold reactive antibody Occasionally IgG antibody that fixes complement Clinically significant in Bombay individuals Test for H antigen using lectin Ulex europaues (gorse) 凝集素 Genetics Gene locus in chromosome 9 q34.1 – q34.2 A and B gene are co-dominant O gene is amorph (deletion at codon 87 produces frameshift resulting in premature stop codon can lead to nonfunctional protein) Point mutations results in enzymes with different substrate specificities and glycosylation efficiencies – leads to variant antigens including O variants Blood group A B AB O Antibodies in plasma Antigen in RBCs Anti-B Anti-A None A antigen B antigen A and B antigen Anti-A and AntiB None Phenotypes patterns Antigen A1 A2 B O A1B A2B Oh Genotype A1A1, A0, A1A2 A2A2, A2O BB, BO OO A1B A2B hh, any ABO gene Antibodies Anti-B Anti-B (2-8% anti-A1) Anti-A, anti-A1 Anti-A, A1, B, A,B None None Anti-A, A1, B, H Importance of ABO blood group Performed IgM antibodies in the circulation Ag/Ab interaction will activate classical pathway of complement quickly Induces intravascular haemolysis through incompatible ABO transfusion ABO blood group system has high density and distribution in body Soluble forms of ABH in the body Highly immunogenic In HDFN IgG anti-A, B can cross the placenta ABO discrepancies 1) Variant antigens A3 and B3: characterised by mixed field agglutination (many small agglutinate in agglutinated cells) Ax: no reaction with anti-A, weak reaction with anti-A,B, may have anti-A1, soluble A-antigen if secretor Am: no reaction with anti-A, weak/no reaction with anti-A, B, no anti-A, no soluble A-antigen Cis-AB: appears as group AB but have allo-anti-B in reverse group due to abnormal A gene that produces enzyme capable of adding both A and B carbohydrates B(A): detecte with monoclonal antisera which anti-B detects weak expression of A antigen on B cells Ael, Abantu, Alae 2) Mixed filed reactions: many small agglutinates in a sea of unagglutinated cells Often missed with tube techniques Best seen with tile or CAT Accidental/deliberate transfusion of ABO mismatched blood Feto-maternal bleed Maternal contamination of cord specimen Twin-twin transfusion in utero Chimeras Bone marrow transplant Subgroups of A and B (A3, B3 and some other will not be seen with monoclonal reagents) Polyagglutination (will not be seen with monoclonal typing reagents) 3) Antigen alteration Unexpected antigens Whartons jelly in cord samples Autoagglutinable cells Polyagglutination Acquire A or B antigen Preservative/dye dependent reactions Weakened antigens Subgroups Cord cells Disease related (leukaemia and hodgkins disease) Variant antigens e.g. A2 A1 = A+A1, A2 = A, therefore A2 can produce anti-A1 A1 =Aa, Ab, Ac, Ad, A2 = Aa and Ab, therefore anti-A1 = anti-Acd A2 allele leads to substitution of leucine for proline at position 156 in the N-acetylgalactosamyl transferase leading to elongation of protein, results in less efficient enzyme leading to qualitative and quantitative difference between A1 and A2 e.g. cis-AB (ABO genotype) Genotype AB + OO offspring with unequal cross-over (rare) to have genotype ABO (cis-AB) offspring Cis-AB expression in a number of cases is due to structural mutation in either A or B gene producing single abnormal enzyme with bifunctional activity Bombay Testing Oh 1. Anti-A1 + Oh = no reaction 2. Anti-B + Oh = no reaction 3. H-lectin (act as anti-H) + Oh = no reaction (because Oh group do not have any H-antigen therefore will not react with anti-H) ABH antigen and disease 1. Reduced expression maybe found in 1) Translocation involving chromosome 9 2) Leukaemia 3) Haemopoietic stress conditions 2. Acquired antigens Rh blood group system Gene location: 1p36.11, locus linked to elliptocytosis gene locus Number of genes = 2, RH(D) and RH(CE) polypeptides Genes are inherited as haplotypes (50:50) Rh protein Multi-pass membrane protein Cross RBC membrane 12 times No sugars attached D negative Caucasians lack the RH(D) gene D negative blacks and Japanese have abnormal RH(D) gene Weak D type – do not make anti-D Missense mutation in RH(D) encoding transmembrane/cytoplasmic portion of D Less protein inserted into RBC membrane can type as Rh(+) or Rh(-) by direct agglutination with monoclonal IgM anti-D regents Type 1 and 2 (3 and 4) account for 90% of weak D, do not produce anti-D Type 4.2, 5, 11, 15, 19, 20 known to form anti-D when exposed to D+ RBCs IS: 0, D IAT: 3, Ct. IAT: 0 Partial D type - Weak expression of D able to make anti-D Partial D: hybrid RH(D) allels (DVI, DIIIa, DIVa/B) Del: detection by adsorption/elution D epitopes on RH(CE) gene IS: 0/3, D IAT: 3, Ct. IAT: 0 E.g. partial DVI gene results from 3 exons of RH(CE) gene inserted into RH(D) gene Del Type as D-nega (IS&IAT) only adsorb and elute anti-D Severely reduced protein Individuals may make anti-D after receiving D+ blood Cause by exon 9 deletion in Asians (10-30%) Reasons to resolve weak expression 1) Conserve Rh-neg blood for D-neg recipients (high risk of making anti-D) 2) Avoid giving RhIG to women who do not need it (Rh status is confirmed for historical discrepancies) 3) Resolve early in pregnancy to eliminate false-positive rosette tests Weak Rh(D) antigen expression Partial D results from lack of D epitopes (these people may type as D-pos but can make anti-D to the epitopes they lack) Numerous categories based on epitope profile: DII, DIII, DVI, DDBT D weak due to error in pre-mRNA processing or due to C in trans relationship to D (C and D genes are on opposite chromosomes) Summary 3-5% RhIG goes to women with weak D types Switch of Rh status is needed when: molecular test is permanent solution, weak D types 1-4 are RH+ as a recipient and donor Informed consent for administration of RhIG: avoid blood product where it is not needed, RhIG shortage, new infectious disease Rh variants Mechanisms Rearrangement of RH(CE) and RH(D) D - - : lack of expression of C and E antigens Increased expression of D (as IgG anti-D may directly agglutinate these cells) Point mutation Non-sense mutation Deletion of nucleotides with resultant frameshift Compound antigens C and E antigen combinations when the genes are in cis relationship (on the same chromosome) ce (f) present in R0 and r Ce present in R1 and r’ cE present in R2 and r’’ CE present in Rz and ry G antigens Antigen present on both RhD and RhC proteins Due to common residues in second extracellular loop encoded by exon 2 Not a compound antigen Antibody often seen as anti-CD mixture, actually could be anti-D+G or anti-C+G or anti-D+C+G Very rare to get a pure anti-G 2 stage adsoption to prove/disprove the presence of anti-G Rh null Lack expression of ALL normal Rh antigens Haemolytic anaemia of varying severity Increase osmotic fragility (24 hrs) Stomatocytic red cell morphology Abnormal cation flux of RBC membrane Inheritance: amorph type DcE/--- + DCe/--- = DcE/--- or - - -/- - Regulator type: (due to mutation affecting RHAG gene that affects RhAG needed for normal Rh antigen expression) DCe/Dce, X1r/X0r + DCe/dce, X1r/X0r = Rh null, X0r/X0r or DCe/DCe, X1r/X1r Rh and disease Rh and HDFN in Caucasian patients Reduced expression of RhD has been seen in patients with myelodsplastic syndromes (patient change from D-pos to D-neg) Rh linked with one form of HE Reduced expression of Rh antigens in SE Asian Ovalocytosis Rh null and compensated haemolytic anaemia Rh and warm AIHA Landsteiner-Weiner system (LW) LW(a+b-) 97%, LW(a+b+)3% More LW on D-pos than D-neg cells More LW on cord cells than adult cells No LW expression on Rh null cells Accessory proteins and cytoskeletal interaction Function of Rh and RhAg proteins Evidence suggests RhAG is involved in ammonia transport Non-erythroid homologues presence in kidney, liver, skin, testis and brain RhAG homologs identified in earthworms Structural role in maintaining red cell shape RhD and RhCE have possible role in CO2 transport Rh phenotyping Reagents: polyclonal (rarely used) 1. mixture of high avidity anti-D sera, 2. potentiaed to produced direct agglutination, 3. MUST run a reagent control. Reagents: monoclonal (commonly used) 1. Human cell lines 2. IgM and IgM/IgG blends 3. Not potentiated Donors: true RhD-neg (i.e. rr), tested for weak D (all variants, especially DVI) Patients: test for PhD using reagent that doesn’t detect DVI (maternity cases are the exception), if negative transfuse with RhD-neg donors Rh alloantibodies Generally immune (IgG1 and IgG3) Involved in HTR and HDFN Naturally occurring antibodies do exist: Anti-E most common but anti-Cw and anti-D exit as well Mixtures of antibodies common e.g. Anti-D+C, anti-E+c in R1R1 person React best by enzyme (low avidity antibodies) and antiglobilin techniques DO NOT fix complement (Rh antibodies do not activate complement due to the distance between antigens but is probably due to a lack of mobility) Reactivity of Rh antibodies is enhanced by enzyme treatment of the test RBCs and most react optimally at 37C Week 2/ Haemagglutination and serological techniques – compatibility testing Haemagglutination and serological techniques Affinity: related to the closeness of fit between the hapten/epitope and the antibody binding site Avidity: related to the closeness of fit between individual epitope/binding site unions and the number of different epitope/binding site reaction Blood group antigens are heterogenous with respect to biochemistry, epitope configuration, distribution w/n body, # and cellular density Antigen epitope configurations: AB antigens: at least 4 different configurations, Rh antigens: D antigen known to have 30 different epitopes Antigen distribution: AB antigens: on virtually all cells in body (soluble antigen in Se positive individuals ~80%) Kell and Rh antigens only found on red cells Primary antigen-antibody interaction (Ag + Ab AgAb) Specific, fast, invisible, energy changes occurs Factor influencing primary interaction: ags/abs concentration, proteolysis of red cell membrane, ionic strength, pH, temp Ags/abs concentration: promote formation of ag/ab complex: increase conc. of abs relative to ags by adding larger volume of serum/plasma, decrease ag conc relative to abs by using weaker cell suspensions [if abs conc is low, use weak cell suspension (tube or CAT tech), if ags expression is weak, use strong cell suspension (tile technique)] Proteolysis of RBC membrane: treating RBC with proteolytic enzymes (papain, ficin) can remove surface structures including some blood group antigen and additional antigen sites and decrease negative charge of RBC. Proteolytic digestion of RBC membrane can expose 30% more Rh(D) antigen sites Ionic strength: reduction the ionic strength of a red cell suspension can enhance the rate of primary union of antigen and antibody by up o 1000-fold, this is achieved by increasing the ionisation of cell surface antigens and promoting the formation of ionic bonds pH (H+ conc) generally ag-ab reactions work best at neutral pH, some reactions work best at slight acidic pH (pH6.5) e.g. reactions favouring acid conditions include some anti-M and anti-P1 abs temp: influence of temp is determined by the thermal characteristics of ag-ab reaction, the thermal characteristics of reaction are influenced by the predominating non-covalent bonds, predominating non-covalent bonds are largely influenced by the biochemistry of the antigen non-covalent bonds (e.g. ionic, H, hydrophobic, dispersion forces): relatively weak bonds which contribute to the reversible nature of ag-ab reaction, bond strength is dependent on the proximity of the epitope and ab-binding site Secondary antigen-antibody interaction (Ag + Ab + AgAb AgnAbn) Specific, slow, visible, little energy change Factor influencing secondary interaction: size relationship b/w ab and RBC surface, zeta potential, water of hydration RBC interspace 25nm, best fit for IgM but not best for IgG Zeta potential: cloud of positive cations (Na+) surrounded negative charged RBC surface, resulting in the repulsion from other negatively charged red cells. 1) Inversely proportional to dielectric constant and ionic strength of medium 2) Dielectric constant is a measure of the charge dissipating ability of the suspending medium 3) Zeta potential can be altered by changing RBC surface charge and/or altering the suspending medium 4) Dielectric constant can be increased by the addition of material such as albumin 5) Increase in ionic strength will decrease zeta potential but at the same time decrease the rate of primary ag-ab reactions Water of hydration: electro-negative charge RBC surface binds water through H bond, abs with stronger H-bond ability displace the H-bonded water when they combine with their epitope, the more water released the closer the cells can become leading to cross-linking by IgM and IgG abs Reducing the electro-negative charge of cell (e.g. proteolysis, decreases the amount of H bonded water) where antigen conc is high (e.g. A and B antigens, large amounts of specifically bound IgG antibody can displace sufficient H bond water allowing cells to come close enough for IgG ab to crosslink them Haemagglutination Ag determines: the Ig class of the ab, how much and where ab can attach to the RBC surface, the thermodynamics of ag-ab reaction Both zeta potential and wate of hydration operate to keep RBC apart and required modification if IgG ab are to produce direct haemagglutination Titre: measure of ab conc, significant difference requires at least 2 tube difference in titre Scors: measure of ab concentration and avidity, significant difference requires a score which differs by 10 or mote Reaction vessels: 1. Test tube (easty to hanle, can be centrifuged, good for weak abs); 2. Microtiter: plates U and V bottom (convenient for batch testing, economical with reagents, good for weak ab, require special microplate carriers for centrifugation) 3. Tiles: glass or plastic: possible to perform multiple tests, good for weak ag expression and cell mixtures, tiles retained for repeat observation 4. Capillary tubes (chown): very economical on regents, difficult to handle and label capillary tubes, reading difficult 5. Solid-phase red cell adherence: reading based on monolayer or pellet of indicator cells, economical on reagents, solid-phase coated plates can fixed/stored, good for batch testing and weak abs, requires microplate carriers and accurate centrifugation condition, can be read using image analysis, can’t discriminate cell mixtures 6. Lateral flow: immobilised ab captures ag positive cells and unattached cells are washed away leaving bands of red cells to indicate phenotypes 7. Magnetised red cell separation: red cells are coated with magnetised beads that allow them to be separated based on a magnetic field and carefully controlled shaking of a microtitre plate Serology techniques – Saline Direct haemagglutination (ABO, H, I, P, Lweis, MNS, IgM warm reacting abs can be detected) Primary or secondary AgAbs reactions occur Mainly IgM abs but can be IgG Usually react best at RT and below, can react up to 37C Usually performed as IS and following 15min incubation at 37C Serology techniques – anti-human globulin Techniques to detect IgG and/or C3b/C3d’ sensitised red cells (primary ag/ab reaction only) Direct: sensitisation has occurred in vivo Indirect: sensitisation has occurred in vitro Variation in technique relate to optimisation of primary ag/ab reaction (LISS, PEG) 37C saline test performed before washing can indicate direct agglutination which could be carried through to the AGH phase Low avidity abs can be eluted form the cells during the washing steps CAT DO NOT require washing step Serology techniques – manual anti-human globulin False negative Inadequate washing of cells AHG regent neutralised or deteriorated AHG not added Serum/plasma not added in indirect test Serum non-reactive (C’ inactive) Inadequate incubation conditions Cell suspension too weak/heavy Poor reading techniques False positive Auto-agglutinable cells DAT positive cells used in indirect test Bacterial contamination of cells’saline Poor reading techniques Preservative or LISS dependent abs CAT: diamed only abs, warm/weak reactive no appaerent specificity (WRNAS) Serology techniques – anti-human globulin Detects: Rh, Kell, Kidd, Duffy, S s U, Diego, Vel and others Manual technique detects 200-300 IgG molecules/RBC CAT more sensitive than manual technique Manual technique may miss low avidity abs Serology techniques – enzyme (proteases: papin, ficin, bromelin) Detects Rh, Jk and some Kell abs, cold, auto and enzyme only abs Destroys Fy(a) Fy(b), M, N, S antigens (In, Kn/McC, Ch/Rg, JMH) Can be performed as single (mixed red cells, enzyme and serum, two-stage: mix red cells and enzyme, wash and add serum/plasma, techniques) Tube two stage most sensitive of the enzyme techniques Considered to be overly sensitive to non-clinically significant abs hence not used routinely False positive if red cells are over-treated with enzyme Can be used with CAT Manual technique can be adapted to an enzyme-AHG technique Summary Different abs react best by different techniques therefore resolving ab problems requires use of a range of serological techniques CAT has introduced standardisation, automation and simplification to red cell serology CAT has limitations in its flexibility to resolve ab investigations and sometime is too sensitive Clinical significance of blood group antibodies Clinical significance of blood group antibodies are those that results in 1) shortened survival of transfused cells, 2) results in products from an antigen antibody reaction that produce adverse clinical effects in the recipient Generally react at 32C+ temp and results in complement activation and/or phagocytosis and/or ADCC (can be sequestration of agglutinated RBCs, apoptosis, membrane perturbation/eryptosis) Complement activation pathways: activation > amplification > Membrane attack complex MAC formation 1. Classical pathway: ag-ab interaction (C1qrs, Ca2+) > C2, C4 amplification > C3 amplification > C5,6,7 > C8,9 > MAC 2. Alternate pathway: C3 hydrolysis > factor D/B, properdin,C3 amplification > C3 amplification> C5,6,7 > C8,9 > MAC 3. MBL pathwaylectin binding to bacteria mannose > C2, C4 amplification > C3 amplification> C5, 6, 7 > C8, C9 > MAC Classical pathway activation sequence 1. Recognition phase: ab (IgM, IgG3, IgG1, IgG2) + C1q (ca2+), C1r and C1s 2. Amplification phase: a) C1s acts on C4 > produce C4a, C4b; act on C2 > produce C2a, C2b b) C4b and C2a combine to produce C4b2a (C3 convertase) which is stabilised by binding to CR1 sites on RBC c) C4b2a acts on C3 > produce C3a, C3b. d) C3b combines C4b2a > produce C4b2a3b (C5 convertase), some C3b binds to other CR1 sites for further activation e) C4b2a3b act on C5 > produce C5a, C5b f) C5b combine C5 convertase (C4b2a3b) or attach weakly to other sites on RBCs 3. MAC formation a) C5b attract C6, C7 > produce C5b67 on RBC surface b) Lesion stat to appear on surface c) C8 combine C5b67 > produce pores in RBC membrane d) C9 combine C5b678 > act as catalyst to enhance pore formation e) Cell is unable to maintain osmotic balance, water flows in and the cell eventually bursts Complement activation products C2b: kinin like activity C3b opsonisation C3a and C5a: chemotaxis and anaphylaxis C5b67: reactive lysis C8, C9: membrane lysis Phagocytosis 1. Splenic sequestration: IgG3, IgG1 [EVH] 2. Hepatic sequestration: C3b (IgG3, IgG1) [IVH] ADCC Perforin and granzymes IgG3 and IgG1, macrophages, NK cells, neutrophils Mediators of clinical effects 1. 2. 3. 4. Anti-inflammatory: IL-1ra Proinflammatory: IL1, TNFa, IL6 > fever, shock, coagulation Chemokines: IL8, MCP > infiltration degranulation C3a, C5a activated monocyte/macrophage Factors influencing clinical significance 1. 2. 3. 4. Antigen: immunogenicity, biochemistry, density and distribution in the body Antibody: Ig class and subclass, conc, avidity Complement: activation and regulation Monocyte/macrophage system: activity Immunogenicity of blood group antigen: D > K > c > E > k > e > Fy(a) > C > Jk(a) > S Summary Antigens are the primary factors in determining clinical significance in blood transfusion Antibody characteristics and the reaction with antigens can caused red cell destruction by number of mechanisms which are not mutually exclusive The interaction between antigen and antibody can produce a range of biologically active mediators that cause clinical changes in a transfusion recipient Week 3/ Clinical significance of blood group antibodies Antibody detection ABO reverse groups Screening cells Purpose to detect abs to the most common clinically significant blood group ags Consist of: 2-3 group O cells containing all of the ags to the most commonly occurring abs, with homozygous expression of ags known to demonstrate dosage e.g. Rh, Fy, Jk, MNS Dosage Effect is a phenomenon in which red cells from homozygous people possess more antigens per red cell than do cells from heterozygous people. The effect is exhibited by the corresponding antibodies reacting more strongly with cells from homozygous people With increasing reliance on abs screening to release blood, screening cells should express important low frequent antigens Zygosity and dosage 1. 2. 3. 4. Jka/Jka (homozygous): dosage 4+/12 > antibody production: anti-Jkb Jka/Jkb (heterozygous): dosage 2+/8 > antibody production: none Jkb/Jkb (homozygous): dosage 0/0 > antibody production: anti-Jka Jk/Jk: dosage 0/0 > antibody production: anti-Jk3 Antibody detection – techniques Those capable of detecting clinically significant red cell abs reactive by haemagglutination and/or haemolysis at 37C: IS, 37C, IAT CAT indirect antiglobulin technique (IAT) IS: detecting MNS, P1, Lewis (I, H) IAT: detecting Rh, Kell, Fy, Jk and others Enzyme: detecting Rh, [Kell], Jk, P1, Lewis, (I, H) Antibody identification Panel cells Purpose to confidently identify the single abs or simple ab mixtures Consist of 11 to 16 group O cells of known phenotype that provide sufficient ags positive and negative cells to allow 95%confidence of abs identification Should express ags which may be unique to the racial groups (e.g. V, VS, Mia, Mur, Gerbich) Indication of high and low frequency ags and additional ag typings May include a pool of group O cord cells which are negative for the following ags: I, lewis, Sid Collected into preservative colution giving expiry of at least 8-10 weeks from collection Basic rules Include original reactive cells where possible: if performing investigation following initial ID in crossmatch Include patients own cells (autocontrol) Use a variety of techniques Record results quantitatively Include A1 and A2 cells as appropriate: if querying anti-A1 or anti-H Panel interpretation Autocontrol: allo- or autoantibody or both Single o multiple abs: reaction in different tech, different strength of reaction in one tech (dosage or multiple abs) Consider negative reactions first: abs can not be directed against antigens on cells which are non-reactive, start with the techniques that has most negative reactions Match pattern of reactions Interpretation of reaction In which techniques are the reaction occurring? IgG or IgM (warm or cold abs)? Is haemolysis present in 37 saline? Do reactions occur with different cells in different techniques? Multiple abs reacting with different ags in their preferred techniques e.g. Rh enhanced in enzyme, Fy negative in enzyme Do reaction strength differ with different cells in one technique (multipe abs, single abs showing dosage) All cells reacting: autoabs (note auto-control), abs to high frequency ags or HTLA, oreservative dependent (panel cells positive, auto-control negative, DAT negative), reagent dependent abs (all cells positive including auto, patient DAT negative) Confirmation of identification Consider reaction characteristics of possible abs What is/are the most probable abs and what can’t be excluded Extend the panel to eliminate abs that can not be excluded Must have at least two cells with only one of the antigens for the most probable abs reactimg positively and/or negatively Phenotype the patient and donor units if part of a cross match Calculate probability Phenotype patient and donor units Ethnic background of patient may provide clue to likely abs specificity If allo-abs, patient should lack ags to most probable abs Compatible donor units must lack ags to most probable abs Incompatible donor units must express one or more of the antigens which have not been excluded Calculate probability 95% probability requires 3 ags positive and 3 ags negative cells reacting accordingly (fisher race calculation and AABB guidelines) BCSH and AABB guidelines indicate 2 ags positive and 2 ags negative cells are all that is required to confirmed abs specificity Extent the panel when mixtures existed Should be used in conjunction with serological information e.g. anti-Fya reactivity by IAT and NOT by enzyme is strong evidence of presence, irrespective of probability calculation Unexplained reaction 1. 2. 3. 4. Poor technique Antibody only reacts with homozygous cells Abs reacting with ags not indicated on panel i.e. low frequency/private ags Preservative or reagent dependent abs e.g. neomycin, thiomersal, inosine, glucose, EDTA etc Problem - Complex mixture/abs to high frequency ags Autocontrol negative, no negative reactions in panel Reactions are wek and confusing (maybe HTLA or HLA related) Problem - Autocontrol is positive Autoabs present in sample and may mask presence of alloabs Resolving complex mixture: 1. Separate antibodies a) Dilution of sample: low titre abs don’t react b) Change incubation time and/or temperature: limits reactivity of some abs in mixture c) Differential absorption and elution: absorb some specificities from mixture, use cells that are giving strong reactions to absorb multiple abs or those at highest titre, or weakest reaction to absorb fewer abs and those at lower titre 2. Extend the panel by selecting appropriate antigen positive and negative cells, use null phenotype cells 3. Modify antigens on cekks a) Enzyme destroy MNS, P, Fya, Fyb, Xg1, In, Kn/McC, Ch/Rg and JMH b) Aminoethylisothiouronium bromide AET and dithiothreitol DTT destroy Kell system antigens, destroy/weaken LW, In, Kn/McC, Gya, Hy, Joa, Yt 4. Neutralise antibodies a) ABH, Lewis using saliva b) P1 using hydratid cyst fluid, pigeon egg ovalbumin c) I using colostrum d) Sid using urine e) Ch/Rg and HLA using fresh inert serum 5. Adsorb the antibodies e.g. Bg/HLA abs can be absorbed using expired pooled platelets 6. Use special techniques: combine enzyme/AHG (where abs masked by Fy, weak Jk abs) 7. Use rare and different cells (Reference labs) a) Rabbit red cell stoma: high in I ags b) Monkey, horse cell cells: high in i ags c) Dog red cells: use in differentiating Pr abs d) Pig red cells: express A(p) ags Compatibility testing Purpose to prevent transfusion reaction Blood product will be of maximum benefit to the patient Clinical decision on need for blood and type of product Request for blood/sample collection Grouping, antibody screening and crossmatching Release of blood and setting up transfusion Monitoring the patient Crossmatching Check for major discrepancies in ABO grouping Check for presence of pre-formed abs which may lead to premature destruction of transfused red cells Cannot detect all ABO mismatches and mistake RhD typing Do not guarantee transfused RBCs will have normal survival Do not guarantee recipient will not have a reaction or produce abs to transfused blood Require: patient ID (full name, dob, UR, ward), full history (diagnosis, therapy, pregnancy, known abs), type and volume of produce required, date and time required, request signed Acute blood loss (injury/surgery) Type of product and rate of transfusion dependent on situation Massive blood loss (volume equivalent to patient blood volume transfused in 24hrs or 5 units in 4 hrs) Massive transfusion protocol/pack (MTP) a) 4 units RBC (ABO matched but uncrossmatched blood or O RhD neg) b) 4 units fresh frozen plasma (FFP) (group AB if group unknown) c) One platelet pool (4 individuals) or one apheresis pack Laboratory protocol for need to crossmatch in place (e.g. don’t crossmatch after 10 units given) Elective surgery or chronic blood loss Maximum (surgical) blood order schedule (MSBOS) Indication of likely need for blood associated with different surgical procedures determined by hospital transfusion committee, regularly reviewed and updated Crossmatch transfusion ratio ≤2:1 considered to be desirable (>2:1 unnecessary testing being performed) Patient blood samples collected Within 72hrs of transfusion if previously transfused Positive patient ID (direct questioning for full name and dob), policy in place for ID of unconscious, irrational, foreign speaking ir patient w/o wrist band Volume and anticoagulant appropriate (EDTA plasma or serum) Labelling: patient name written on tube immediately after collection, date and time of collection noted on tube and request slip, request slip signed Transport immediately to laboratory Laboratory check on ID, match sample to request form, consult laboratory records for previous testing ABO and Rh(D) type sample First time testing: test twice, two people independently confirm results, use twoo different anti-D reagents Repeat testing: confirm result with laboratory records Antibody screen Three cell panel to cover ag system showing dosage Techniques: manual procedure IS, 37C saline, IAT or CAT IAT Antibody screen negative and no previous history of antibody detection: 1. Issue ABO and Rh(D) matched units 2. IS to check ABO mismatch 3. Check computer crossmatch/electronic release Antibody screen positive or history of previous antibodies 1. Identify antibodies 2. Crossmatch ABO, RhD matched and antigen negative donor unit a) Negative for identified antibodies and any antigen likely to stimulate more antibodies e.g. K for pregnant women, R1R1 with anti-c 3. Record results which should include: a) Full patient ID b) Sample collection date/time and expiry c) ABO and Rh(D) type, antibody screen and antibody ID d) Blood product type and donation/batch numbers e) ABO, Rh(D) type and extended phenotype as appropriate f) Compatibility results, time performed and by whom g) Date and time of issue Blood of same group not available AB use group A red cell concentrate first (note expirt of available unites) A or B use group O red cell concentrate change to patients true group once any transfused isohaemagglutinins no longer detected by IAT RhD positive blood only to RhD negative males or post-menopausal females BMT patient with different ABO donor group Laboratory protocol for group of products to be used at different times post-transplant Change patient record for blood group Check ABO and RhD type of donor units before release for transfusion Label units for patient and hold in appropriate section of the blood bank refrigerator for agreed time Print compatibility or issue report (including patient ID, ABO Rh(D) group, product detail, testing results, appropriate interpretation and clinical comments, details of any special requirements e.g. pre-warm to transfusion Autologous blood Autologous blood collected by the red cross must meet all of the normal donor requirements Autologous blood collected by other agencies may not meet the red cross requirements but the individual must be healthy enough to have two-three units collected in the two to three weeks prior to surgrty Individual should sign each of the packs collected and they should be stored in the blood bank fridge in a special section for autologous donations Prior to transfusion the normal crossmatching protocols should be adopted before the blood is released for transfusion e.g. check blood groups, antibody screen If conscious, the person should identify their signature on the blood pack prior to transfusion commencing If blood not transfused during or post-surgery, it should be discarded Releasing product for transfusion Visually check products for evidence of gross contamination prior to release to ward or theatre Release units only with positive patient ID being provided In ward or theatre two people positively ID patient and donor units Laboratory must be able to trace every blood component/product received through to its final destination e.g. patient, clinical area (ambulance), another facility or disposal See remote release Computer crossmatch/electronic release can be used when: 1. 2. 3. 4. ABO and Rh(D) group confirmed No antibodies in screening test No history of clinically significant antibodies Comprehensive validated software system exists Computer crossmatch/electronic release software features 1. 2. 3. 4. 5. 6. 7. Only release group specific blood if records on current G and S exist Group specific blood not released on historic record O Rh(D) pos or neg blood only released in emergency where no current G and S exists Warning for special blood products provided e.g. CMV negative, irradiated, autologous Mechanism to ensure that blood component is labelled for specific patient Unique label generated at release of unit and checks that group of blood component and patient match Issue report produced with release of blood component to allow documentation of transfusion episode Use of software Must be validated before use a) Cross tabulation of donor and recipient groups for all crossmatched blood products b) Validation recorded and checked by senior staff member Must be revalidated if any software modification undertaken Software modification only by authorised staff All transaction logged and traceable to individual staff e.g. audit trail Random access to database prohibited Remote release Used where blood stocks are held at local centre but all testing is performed centrally a) Extension of computer crossmatch b) Local centre can interrogate the patient records for ABO, Rh(D) group, G and S results and history c) If all conditions are met, check through stocks for appropriate unit and generate label and transfusion documentation. Summary Proper patient and donor ID essential throughout all stages of compatibility process Serological crossmatch is only required on patient with identified antibody/ies or history of antibodies Validated software can be used to safely release blood products for transfusion