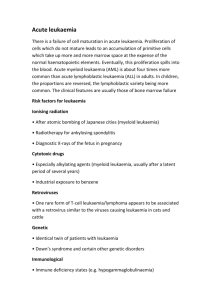
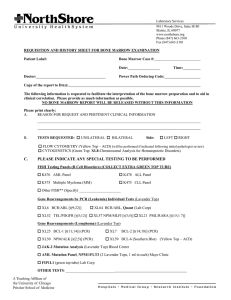
Q18. Acute leukaemia, definition, aetiology, pathogenesis, FAB and WHO classifications, clinical and laboratory features, diagnostic parameters, principle of treatment. Leukaemia: ❖ Tumorous disorders of the haematopoietic system with primary lesion in bone marrow ❖ Tumours disease whose malignant cell is derived from the haematopoietic system and manifests its expansion in the bone marrow as a rule of peripheral blood involvement. ❖ Leukaemia: white blood due to a lot of WBC. Acute leukaemia Tumorous disorders of the haematopoietic system with the primary lesion in the bone marrow, morphological substrate of which is the blasts cells Tumour blast cells similar to blast cells progenitor of specific line of blood cells differentiation (myeloblast, lymphoblast, erythroblast, monoblast) Pathogenesis: ❖ AML (Acute myeloid leukaemia) is clonal disorder of haematopoiesis; at diagnosis, haematological malignancies are characterized by presence of dominant, monoclonal cell populations. The evidence comes from use of molecular markers. Cytogenetic study of these malignant cells has revealed that recurrent chromosomal change that occurs in 1⁄2 of leukaemia. ❖ Mechanisms by which disrupted or deregulated genes cause leukaemia can be broadly classified to 2 categories: ➢ Gene fusion: creates a unique chimeric fusion protein, this mech predominates in myeloid leukaemia. ➢ Gene activation: chromosomal translocations that result in gene activation usually occur in lymphoid tissue and lead to deregulation of gene expression. ❖ Leukaemia cells accumulate in bone marrow cavity, on case of ultimately replacing most of normal haematopoietic cells, thus resulting in the signs and symptoms of bone marrow failure and its signs and symptoms of bone marrow failure and its consequences anaemia, haemorrhage and infection. ❖ Leukaemia cells circulate into blood and other tissue throughout the body. FAB (French-American-British) Classification : ❖ according to morphology and cytochemistry of tumour cells ❖ FAB system divides acute leukaemia into ALL (acute lymphoblastic leukaemia) and ANLL or AML. ❖ ALL included 3 morphologic subtypes (L1, L2, L3) ➢ L1 - small; scanty cytoplasm; uniform appearance ➢ L2 - large; more cytoplasm; heterogeneous in size, shape ➢ L3 - large; moderately abundant basophilic cytoplasm; cytoplasmic vacuolation; cells similar to those in Burkitt's lymphoma ❖ AML has 8 subtypes (M0-M7) ➢ M0, undifferentiated undifferentiated blasts myeloblastic identified by myeloid monoclonal antibodies or peroxidases; ➢ M1, myeloblastic w/o predominantly myeloblasts, maturation little or no maturation; ➢ M2, myeloblastic with myeloblasts and promyelocytes, maturation further maturation abnormal ➢ M3, promyelocytic predominantly promyelocytes, often hypergranular ➢ M4, myelomonocytic evidence of both granulocytic + monocytic maturation, > 20% in blood or marrow ➢ M5, monocytic predominantly monoblasts (M5a) or promonocytes (M5b) ➢ M6, erythroleukaemia > 50% erythroblasts, often bizarre, multinucleate, megaloblastic ➢ M7, megakaryocytic predominantly megakaryocytes or micromegakaryocytes, often associated with acute myelofibrosis WHO classification: 1) AML a) AML with recurrent cytogenetic abnormalities (includes acute promyelocytic leukaemia with t(15;17) or variants b) AML with multi-lineage dysplasia (usually secondary to a pre-existing myelodysplastic syndrome) c) Therapy related AML d) AML-other (includes minimally differentiated AML) e) Acute biphenotypic leukaemia (acute leukaemia expressing both lymphoid and myeloid phenotype) 2) ALL a) Precursor B acute lymphoblastic leukaemia b) Burkitt cell leukaemia c) Precursor T acute lymphoblastic leukaemia Clinical and laboratory features, diagnostic parameter: 2 main syndromes: 1) Syndromes of the depression of normal haematopoiesis a) Anaemia b) Neutropenia c) Thrombocytopenia 2) Syndromes of existence and growth of the tumour cells a) Hyperplastic syndrome: i) Absolute criteria of acute leukaemia: Blast cells > 20% in BM b) the tumour intoxication i) Loss of weight ii) Sweatiness iii) Sub febrile fever *A common presentation of childhood ALL is with joint and muscle pain. ALL does not infiltrate extramedullary tissues - lymph nodes, spleen, liver, meninges - as much as AML. Phases: 1) First attack Acute leukaemia in a newly diagnosed patient 2) Early death Death during two course of chemotherapy in a newly diagnosed patient 3) Resistant disease No complete remission after 1 or 2 course of chemotherapy in a newly diagnosed patient 4) Complete remission No clinical and laboratory evidence of acute leukaemia: Blast cell in the bone marrow les then 5%, in the blood Hb>10.0 g/dl, Le > 1.0 x 10 /l, Pl>100,0x 10 /l 9 9 5) Terminal stage Infiltration of vitality important organs with incompatible life disturbance of their function 6) Relapse Clinical and laboratory evidence of acute leukaemia in the patient after complete remission Investigation: ❖ peripheral blood ➢ pancytopenia with circulating blasts is characteristic ➢ WBC - normal or raised; 50% of individuals have count less than 10 x 10^9/l; 20% have count greater than 100 x 10^9 /l; usually a preponderance of blasts but 10% have aleukaemic leukaemia - blasts absent from peripheral blood although still present in marrow ➢ red cells - anaemia - usually normocytic but may be macrocytic; progressive, may become severe ➢ platelets - usually reduced ❖ bone marrow - hypercellular; diagnosis is made on having more than 30% blasts in the marrow ❖ CSF - blasts present in meningeal leukaemia ❖ CXR - often mediastinal mass in ALL especially T cell ❖ blood cultures - always if patient is febrile ❖ coagulation studies - DIC indicated by reduced fibrinogen, increased prothrombin time, presence of fibrin degradation products hyperuricaemia and hypokalaemia often seen ❖ important to distinguish between AML and ALL: ➢ morphological - Auer rods pathognomonic of AML ➢ histochemical stains for myeloid enzymes such as peroxidase or chloroacetate confirm AML ➢ surface markers characteristic of primitive lymphoid cells identify ALL, e.g. terminal deoxynucleotide transferase present in 95% of cases of ALL ➢ primitive B lymphocyte antigens such as CALLA, B1, BA1 may help to identify ALL ➢ T cell ALL diagnosed by rosette formation with sheep erythrocytes or identification of cell markers by monoclonal antibodies such as Leu-1 or Leu-9 Differential diagnosis: The differential diagnosis of AML includes: ➢ acute lymphoblastic leukaemia ➢ other myeloproliferative disease ➢ chronic myeloid leukaemia ➢ myelodysplastic syndrome ➢ left - shifted bone marrow which is recovering from a previous toxic insult ➢ aplastic anaemia Management: Remission induction (AML) Remission induction is attempted using a combination of cytotoxic agents such as cytosine arabinoside, thioguanine and daunorubicin. However this therapy will lead to myelosuppression and possibly severe infection. The incidence of major infection may be a major limiting factor in trying to achieve complete remission and the patient may be treated prophylactically with antibiotics Leukaemia myeloblasts in AML require cytotoxic agents which are highly toxic to normal marrow cells. An example of combination therapy is: Cytosine arabinoside (Ara-C) Thioguanine Daunorubicin Treatment is scheduled to exploit the slower regeneration time of leukaemic cells compared to normal cells. Commonly, aplasia of the bone marrow results which may take 2-3 weeks to recover. Intensive supportive care is essential because of the myelosuppression. Ara-C - IV; intermediate dose twice daily for 3 days Remission of ALL is achieved with combination chemotherapy: Daunorubicin Vincristine Prednisolone Asparaginase Myelosuppression is minimal and remission achieved in a high proportion of people. A maintenance schedule is beneficial and continued for 2 years. CNS prophylaxis involves cranial irradiation and intrathecal methrotrexate to prevent meningeal sequestration of leukaemic cells - leukaemic cells can cross the blood-brain barrier but many cytotoxic agents cannot. Supportive care for acute myeloblastic leukaemia: 1) Monitoring: a) Daily or alternate daily: blood count, electrolytes, liver function b) Weekly: bacteriological screen, CXR c) When indicated: Blood culture, bone marrow aspirate 2) Anaemia: a) Transfusions of packed RBC to maintain Haemoglobin above 10g/dL 3) Haemorrhage a) Transfusions of 3-12 donor units of platelets to maintain count above 10- 20*100 b) Regular coagulation screens: replacement of coagulation factors with fresh frozen plasma 4) Infection prevention a) Protective isolation: single room reverse-barrier isolation, clean food b) Oral antibiotics: septrin/ ciprofloxacin/ colistin/ neomycin c) Oral antifungal: amphotericin/ nystatin/ fluconazole d) Herpes simplex labialis: oral acyclovir 5) Infection treatments a) Fever regimen: initiated if T> 38C b) First line: aminoglycosides + broad spectrum penicillin IV c) Second line: (no response after 48 hr) d) Ceftazidime and vancomycin IV e) 3 line: (no response after 48 hr, no o’ism isolated: Amphotericin IV 6) Nutritional a) Parenteral feeding if >10% loss of body weight b) IV analgesia for painful stomatitis 7) Psychological a) Frank discussion, optimistic attitude, regular daily visits and progress updates, family support, early discharge as soon as thermodynamically recovery patients. rd Post-remission therapy: Remission is not synonymous with cure. Further treatment is required to prevent recurrence. Therapies include: Repeated intensive chemotherapy High-dose chemo radiotherapy with allogeneic bone marrow transplantation High-dose chemotherapy with autologous bone marrow transplantation The medications used to treat acute leukemia cause severe bone marrow depression. Only physicians specifically trained in their use should administer these medications. In addition, access to appropriate supportive care is required. Drug Category: Corticosteroids -- May be used during induction, consolidation, and/or maintenance therapy. Drug Name Prednisone (Deltasone, Orasone, Sterapred) -- Has a wide range of activities. In ALL, used because of direct antileukemic effects. Adult Dose 60 mg/m PO qd for 28 d during induction; followed by 10-d taper Contraindications Documented hypersensitivity; viral infection, peptic ulcer disease, hepatic dysfunction, connective tissue infections, and fungal or tubercular skin infections; GI disease Precautions Patients must be monitored for toxic effects, such as hyperglycemia, hypertension, increased risk of infection, and avascular necrosis (long-term use); patients may have life-threatening infections with only subtle signs and symptoms of infection Drug Category: Antineoplastics -- Used for induction, consolidation, maintenance, and CNS prophylaxis. Drug Name Vincristine (Oncovin, Vincasar) -- Vinca alkaloid that acts by arresting cells in metaphase. Adult Dose 2 mg/m IV push qwk for 5 wk during induction Most cap the vincristine dose at 4 mg for Contraindications Documented hypersensitivity; preexisting Precautions Inadvertent intrathecal administration has resulted in deaths; extravasation at injection site results in severe local tissue damage; after IV use, monitor patients for symptoms of peripheral neuropathy and constipation Drug Name Asparaginase (Elspar) -- Breaks down extracellular asparagine into aspartic acid and ammonia. Normal cells are capable of synthesizing their own asparagine but many malignant cells are not. Adult Dose 6,000-12,000 U/m IM Contraindications Documented hypersensitivity; history of pancreatitis Precautions Monitor patients for potential toxic effects, including allergic reactions, pancreatitis, thrombotic or bleeding episodes (due to effects on clotting factors), and hyperglycemia Drug Name Methotrexate (Folex, Rheumatrex) -- Antimetabolite of folic acid analog type. Inhibits dihydrofolate reductase, resulting in inhibition of DNA synthesis, repair, and cellular replication. Adult Dose 15 mg/m PO qwk during maintenance therapy Contraindications Do not use high dose in patients with a CrCl <60 mL/min; increased toxicity can occur in patients with ascites or pleural effusions Precautions Monitor CBC counts monthly and liver and renal function q1-3mo during therapy (monitor more frequently, i.e., daily, during initial dosing, dose adjustments, or when risk of elevated levels, e.g., dehydration); has toxic effects on hematologic, renal, GI, pulmonary, and neurologic systems Discontinue if significant drop in blood counts; aspirin, NSAIDs, or low-dose steroids may be administered concomitantly (possibility of increased toxicity with NSAIDs, including salicylates, has not been tested) Drug Name Cyclophosphamide (Cytoxan) -- Alkylating agent of nitrogen mustard type. Inhibits cell growth and proliferation. Adult Dose 1 g/m IV during induction Contraindications Documented hypersensitivity; severely depressed bone marrow function Precautions Regularly examine hematologic profile (particularly neutrophils and platelets) to monitor for hematopoietic suppression; regularly examine urine for RBCs, which may precede hemorrhagic cystitis Drug Name Daunorubicin (Cerubidine) -- Anthracycline that inhibits topoisomerase II. Also 2 2 2 2 2