IAP Immunization guidelines.
What has changed in last few years ? and Why ?
Types of Vaccines
6.
7.
4.
5.
1.
2.
3.
Inactivated Vaccine
Live Attenuated Vaccine
Toxoid
Subunit Vaccine
Conjugated Vaccine
Combination Vaccine
Component Vaccine
Combination Vaccines
7.
8.
5.
6.
3.
4.
1.
2.
9.
10.
11.
12.
DTwP – HiB
DTwP – HepB
DTwP – HiB – HepB
DTwP – IPV
DTwP – IPV – HIB
DTaP
DTaP – HiB
DTaP – IPV
IPV – HIB – HepB
DTaP – HiB – HepB – IPV
HepA – HepB
MMR-Varicella
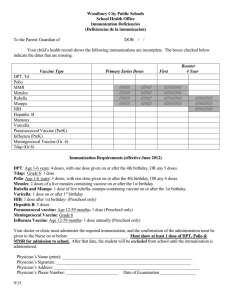
2016 Immunization Schedule
Age
Birth
6 weeks
Vaccines
BCG, OPV 0, Hep-B 1
DTwP 1, IPV 1, Hep-B 2, Hib 1, Rotavirus 1, PCV 1
10 weeks
14 weeks
DTwP 2, IPV 2, Hib 2, Rotavirus 2, PCV 2
DTwP3, IPV3, Hib3, PCV 3, Rotavirus 3
6 months OPV 1, Hep B 3
9 months OPV 2, MMR 1
9-12 months Typhoid conjugate vaccine
12 months Hep A 1
15 months MMR 2, Varicella 1, PCV booster
16-18 months DTwP B1/ DTaP B1, IPV B1, Hib B1
18 months Hep A2
2 years TCV Booster
4-6 years DTwP B2/DTaP B2, OPV 3, Varicella 2, MMR 3
10 – 12 years Tdap/Td, HPV
Specific recommendations
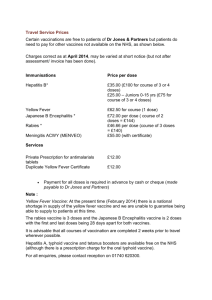
Hepatitis B vaccination
Hepatitis - B:
Birth dose is needed in areas with high or moderate endemicity to prevent perinatal transmission.
Multiple schedule options were available
& all are immunogenic and do not need boosters.
Hepatitis - B:
‘ Birth-6 weeks-6 months’ is recommended as most preferred schedule instead of earlier ‘0- 6 weeks-14 weeks’ schedule.
This schedule is not only more closer to immunologically ideal and most widely used 0-1-6 months schedule, but also conforms to latest ACIP recommendations wherein the final
(third or fourth) dose in the Hepatitis-B vaccine series should be administered no earlier than age 24 weeks and at least
16 weeks after the first dose.
Specific recommendations
Polio vaccination
Poliovirus Immunization:
• The committee has now decided to adopt a
sequential IPV ‐ OPV schedule.
• Ultimate adoption of all-IPV schedule in future considering the inevitable cessation of OPV from immunization schedules owing to its safety issues.
• Phased removal of Sabin viruses, beginning with highest risk (type 2).
Why changes in polio immunization schedule?
•
• Previous combined OPV+IPV schedule to maximize individual immune response.
India is wild polio free since 2011 & Type 2
WPV eradicated in 1999.
• Now safety is more important & cVDPVs &
VAPP can not be overlooked anymore !
New polio endgame strategy
• Phased removal of Sabin viruses, beginning with highest risk (type 2).
• Elimination of VDPV type 2 by switching from tOPV to bOPV for routine EPI & campaigns.
• This switch would result in early introduction of
IPV, at least in high risk areas for VDPVs, to provide type 2 protection.
Poliovirus Immunization
• Considerable evidence to show that sequential schedules that provide IPV first, followed by
OPV, can prevent VAPP while maintaining the benefits conferred by OPV (i.e., high levels of gut immunity)
The earlier schedule:
• Birth dose of OPV + 3 primary doses of IPV at
6, 10 and 14 weeks + 2 doses of OPV at 6 &
9 months + IPV at 15 ‐ 18 months (booster) +
OPV at 5 yrs
The current schedule
• OPV at birth + 2 doses of IPV at 8 and 16 weeks (i.e. 2
& 4 mo ) + OPV at 6 & 9 months + IPV at 15 -18 months + OPV at 5 yrs
> Immunologically superior to EPI
> Number of IPV doses is reduced
> Will be more cumbersome due to extra visits
> incompatibility with combination formulations.
> Child would be susceptible to WPV infection for the first 2 months of life.
OPV: Birth dose
• The committee has retained the birth dose of
OPV as recommended earlier.
• Providing the first OPV dose at age when the infant is still protected by maternally derived antibodies may, at least theoretically, also prevent VAPP.
• A birth dose of OPV is considered necessary in countries where the risk of polio virus transmission is high.
Polio vaccines and polio immunization in the preeradication era : WHO position paper.
Wkly Epidemiol Rec. 2010;85:213-- ‐ 28.
Polio immunization:
• If IPV is unaffordable or unavailable, the primary series must be completed with three doses of
OPV given at 6, 10, and 14 weeks
• No child should be left without adequate protection against wild polio virus!!
• All OPV doses(mono, bi, or trivalent ) offered through supplemental immunization activities
(SIAs), should also be provided.
Catch up schedule:
• IPV may be offered as ‘catch up vaccination’ for children less than 5 years of age who have completed primary immunization with OPV.
• IPV can be given as 3doses; 2 doses at 2 months interval followed by a 3 rd dose after 6 mos.
• This schedule will ensure a long lasting protection against poliovirus disease.
ID
A
B
I/M
A
B
Catch up
IPV
6 weeks
8 weeks
0
6 weeks
6 weeks
10 weeks
16 weeks
2 months
14 weeks
6 months later
18 months
18 months
14 weeks 8 weeks later full dose IM
8weeks later IM 8weeks later IM
Specific recommendations
Pertusis vaccination
Pertusis immunization:
• Ideally DTwP vaccines to be used for primary immunization.
• DTaP vaccines in certain specific circumstances
/ conditions only & may be as boosters if affordable.
• If aP is to be used it should have 3 or more components in it.
• 1 dose of Tdap vaccine recommended at 10 yrs in place of Td & in pregnant women with every pregnancy.
• No need of repeating / giving additional doses of wP vaccine to children who had earlier completed their primary schedule with aP vaccine-containing products.
Why no aP in primary immunizations ?
Recent resurgence of Pertusis in western world.
aP vaccines are less effective than previously believed.
Priming with wP is more at sustained prevention than aP vaccines.
Available evidence favours use of 3 or more component aP rather than 1 or 2 component.
age
DPT
primary 1 st booster
6-12 mnths later
2 nd booster
5 yrs later
10 yrs Every
10yrs
< 4yrs
4-7yrs
0,1,2 [DPT]
0,1,2 [DPT]
+ [DPT]
+ [DPT]
+ [DPT] Tdap
-----------Tdap
7-10yrs 0,1 [Tdap, Td] + [Td]
11-18 yrs 0 [Tdap] --------------
--------------
--------------
-------------
--------------
Td
Td
Td
Td
Specific recommendations
Pneumococcal Conjugate vaccination
Pneumococcal diseases in India
•
PCV to be offered to healthy children upto 5 yrs & in special cases upto 18 yrs and all adults
> 50 yrs
Protective efficacy against Invasive disease,
Pneumonia, Otitis media
Pneumococcal vaccine schedule
Age at first dose Primary series* booster dose†
6wks–6 mos 3 doses 1 dose at 12–15 mos
7–11mos
12–23mos
2 doses
2 doses
1 dose at 12–15 mos
NA
24–59 mos ( healthy ) 1 dose
24–71mos ( high risk) 2 doses
NA
NA
Alternative schedules
Two doses before six months of age (at intervals of one or two months) plus a booster dose around 12 months of age
("2 + 1" schedule)
Three doses before six months at intervals of one month, plus a booster dose around 12 months of age ( "3 + 1" schedule).
PCV13
Children <24 months: : 2, 4, 6, and 12 to 15 months of age.
◦ The first dose can be given as early as six weeks of age.
◦ A minimum of four weeks between the three doses is acceptable in children younger than one year.
◦ The fourth dose should be given at 12 to 15 months of age but at least eight weeks after the third dose.
Preterm infants should receive PCV13 according to their chronologic age
High-risk children
<24 months : as per schedule for healthy children.
≥2 years of age: additional 23-valent PPSV23 at least eight weeks after they have completed immunization with PCV13
◦ High-risk children (younger than 72 months ) with PCV 7 &
PPSV 23 vaccination schedule should receive a single dose of
PCV13 at least eight weeks after the last dose of PCV7 or
PPSV23.
6 through 18 years with anatomic or functional asplenia, human immunodeficiency virus (HIV) or other immunocompromising condition, chronic renal failure, nephrotic syndrome, cochlear implant, or cerebrospinal fluid leak : a single dose of PCV13, followed ≥8 weeks later by a dose of PPSV23
◦ those who received PPSV23 but not PCV13 should be given a single dose of PCV13 at least 8 weeks after PPSV23 (whether or not they received PCV7)
One booster PPSV 23 to be given 3-5 years after first dose of PPSV 23
Immunocompetent children with chronic illness : second booster of PPSV 23 not recommended
PCV13 vs PCV10 :
Which vaccine to choose ?
• “since there is scarcity of data on the prevalence of pneumcoccal serotypes including serotypes 3,
6A and 19A, and non-typeable haemophilus
influenzae (NTHi) in India, ……impossible to comment on the exact superiority of one product over other”
• “… in the absence of head to head trials it is difficult to determine if either vaccine has a clear advantage over other”
Recommendations for premature & LBW infants
• Prematurity (PT) & very low birth weight
(VLBW) infants are high risk category for pneumococcal vaccination.
Specific recommendations
Rotavirus vaccination
Rotavirus Vaccine recommendations
For both rotavirus vaccines
• maximum age for first dose is 14 weeks 6 days
• minimum interval between doses is 4 weeks
• maximum age for second dose is 8 months 0 days
MMWR 2009;58:(RR-2)
Rotavirus disease in India
• There is Sufficient burden of RV dis in India
• In developing countries with high burden, even moderate to low vaccine efficacy translates into significant numbers of severe
RVGE cases prevented and into significant public health impact.
Rotavirus vaccine schedule
• Administration schedule of RV1 ( Rotarix ) revised
• Two-dose schedule to begin at 10 weeks, 2nd dose at
14 weeks
RECOMMENDATIONS FOR IAP IMMUNIZATION TIMETABLE, 2013
More interference by Maternal antibodies at early age & hence decreased immunogenicity if RV1 is started at 6 weeks.
Types of rotavirus vaccines
RV 1 = rotarix
RV5 = rotateq
RV 116E = rotavac
Safety of RV vaccines
• ..there is definite albeit a small risk of Ac.
Intussusception following use of current generation of rotavirus vaccines
• ……the benefits of RV vaccination against severe diarrhea & death from RV infection far exceed the miniscule risk of intussusceptions
• History of intussusception in the past will be an absolute contraindication for RV vaccine (RV1 and RV5) administration
Specific recommendations
MMR vaccination
MMR: 2 doses
3 doses of MMR are now recommended.
• 1 st year Dose at 9 months
• 2 nd year Dose at 15 months ( or at any time 8 weeks after 1 st dose in 2 nd year)
• No stand alone measles dose at 9 months
• No MMR at 4-6 years of age
All school aged / adolescents have TWO doses of
MMR 8 weeks [ three doses if first dose given before 1 year]
All the currently licensed preparations of MMR vaccine are safe and effective and any one may
For the first doses of measles, mumps, rubella, and varicella vaccines:
◦ We suggest separate MMR and varicella vaccines (ie, administered at the same visit, but at different sites) for children 12 through
47 months of age
◦ We suggest MMRV for children 48 months through 12 years of age
For the second doses of measles, mumps, rubella, and varicella vaccines:
◦ We suggest MMRV for children between 15 months and 12 years of age
◦ We suggest separate measles, mumps, rubella, and varicella vaccines for children ≥13 years of age can be given as early as 28 days after the first dose, provided that both doses are given at ≥12 months of age
The first and second doses of varicellacontaining vaccines should be separated by at least three months. However, if the second dose is administered at least 28 days after the first dose, the second dose does not need to be repeated
MMR is preferred to immune globulin for
postexposure prophylaxis in incompletely immunized children ≥12 months of age who have been exposed to measles virus within the previous
72 hours
First dose
1-4 yrs
4-13 yrs
> 13 yrs
1-4 yrs
Second dose 4-13 yrs
> 13 yrs
MMRV x x x x x
MMR x x x
Varicella x
HIV infection- severe immunosuppression
CD4 % <15 percent at any age
or
<750/microL for children ≤12 mths of age
<500/microL for children 1-5 years of age
<200/microL for children >5 years of age
Systemic immunosuppressive therapy, including large daily doses of corticosteroids (equivalent to
≥ 2 mg/kg per day or ≥20 mg per day of prednisone) for ≥ 2 weeks
MMR should be avoided for at least one month after high-dose corticosteroid therapy.
Interval between receipt of immune globulin or antibody containing blood products and administration of MMR varies between 3 and 11 months depending upon the product
Egg allergy is not a contraindication to
MMR or MMRV;
Specific recommendations
Typhoid vaccination
Polysaccharide Typhoid vaccine
Till 2013 IAP recommends the administration of the Vi polysaccharide vaccine 0.5 ml IM every 3 years beginning at the age of 2 years.
A child with history of enteric fever may be vaccinated 4 weeks after recovery if he/she has not received the vaccine in the past 3 years
Considering epidemiology of Typhoid there was a definite need of protection below 2 yrs also.
Conjugate Typhoid vaccine
• In 2014 recommendations a slot for single dose of
‘typhoid conjugate vaccine’ for primary immunization at
9-12 months of age.
• Recommendation applicable only for Typbar-TCV and
Peda Typh.
• Booster of either Typbar-TCV or Vi-polysaccharide
(Vi-PS) vaccine at 2 years of age
• Typhoid revaccination every 3 years, if Vipolysaccharide vaccine is used.
Specific recommendations
Hepatitis A vaccination
Hepatitis A Vaccine
In 2012 age for 1 st dose changed from 18 months to 12 month. Why?
Till 2013 for both killed & live vaccines 2 doses are recommended.
In 2014 Single dose administration of live attenuated H2 strain hepatitis A vaccine at 12 months & Two doses for inactivated (killed)
Hepatitis-A vaccine
Hepatitis A
India a highly endemic country is shifting to intermediate endemicity.
Studies show a reduction in cord blood seropositivity .
Several outbreaks of hepatitis A in various parts of India have been recorded in the past decade
Antibody titres with vaccination at 12 months are comparable to those achieved at 18 mths- 2 years.
There is no need for HAV booster vaccination after completion of the primary two-dose vaccination series.
Specific recommendations
Chicken pox vaccination
Varicella Vaccine
The IAP now recommends two doses of varicella vaccine for children of all age groups.
For primary immunization, the first dose should be given at the age of 15 mths and the second dose at 4-6 years ( earliest 3 months after dose 1).
The risk of breakthrough varicella is less if 1 st dose is given at 15 mths or later.
Varicella Vaccine
For catch up vaccination, children below the age of 13 years should receive 2 doses 3 months apart and those aged 13 years or more should receive 2 doses at an interval of 4-8 weeks
Varicella Breakthrough varicella
1 dose v/s 2 doses
PARAMETER
Overall seroprotection 86%
Efficacy against any disease 70-90%
1 DOSE
Efficacy against combined moderate & severe disease
98.3%
99%
>95%
2 DOSES
100%
Duration of Efficacy
Breakthrough Varicella
7-10 years
15%
7 – 10 years
<5%
Specific recommendations
HPV vaccination
Modified schedule for HPV vaccine
• Two doses of HPV vaccine for adolescent/preadolescent girls aged 9-14 years
• For two-dose schedule, the minimum interval between doses should be 6 months
• Three dose schedule ( 0,1-2 mths & 6 mths ) for adolescent girls aged 15 years and older to continue
HPV Vaccine – IAP Stand
The IAPCOI recommends offering HPV vaccine to all females
Since protection is seen only when the vaccine is given before infection with HPV, the vaccine should preferably be given prior to sexual debut.
The vaccine should preferably be introduced to parents as a cervical cancer preventing vaccine and not as a vaccine against a sexually transmitted infection (STI).
HPV Vaccine – IAP COI Stand
Vaccines are not a replacement for periodic screening.
Both the available vaccines ( bivalent & quadrivalent ) are equally efficacious and safe for protection against cervical cancer.
The quadrivalent vaccine additionally protects against anogenital warts.
Vaccines recommended for high risk children
1. Influenza
2. Meningococcal vaccine
3. Jap. Encephalitis vaccine
4. Cholera vaccine
5. Rabies vaccine
6. Yellow fever vaccine
7. Pneumococcal polysacch vac ( PPSV 23 )
High risk category of children
Cong or acquired immunodef ( incl HIV )
Chr cardiac, pulm, ( Asthmatics on oral steroids ) hemato, renal, ( Nephrotics ) liver dis & DM
Children on long term steroids or immunosuppresants
Cong or acquired Asplenia or hyposplenia
DM,CSF leak, Coch implants, Malignancies
Lab persons, health workers
Travellers
Specific recommendations
Influenza vaccination
Influenza vacccines
IAP recommends seasonal influenza vacs only for high risk children like, Chr med conditions like asthma, HD, Nephrotics & DM. Immunodef children
& those on longterm aspirin therapy.
Live attenuated [ LAIV] or trivalent inactivated
[ TIV].
6 mth – 9 yrs : 2 doses 1 mth apart, > 9 yrs : 1 dose
& then Annual vac with single dose.
All currently available trivalent vacs contain H1N1 ag.
Influenza vacccines
Best time to vaccinate
◦ As soon as the new vac is released & available in market
◦ Just before onset on rainy season.
Specific recommendations
Meningococccal vaccination
Meningococcal vaccines
Recommended only for high risk conditions.
Conjugate vac should be preferred over PS ones as can be used < 2 yrs; more immunogenic
& better herd protection.
For epidemics : Serotype A containing conjugate vacs.
For international travellers like [< 21 yrs ] students going to US, to Haj pilgrimage or
African nations.
Specific recommendations
Japanese encephalitis vaccination
JE immunization:
• Two doses of live attenuated SA-14-14-2 vaccine
First dose of the vaccine can be administered at 9 months along with measles vaccine and second at 16 to 18 months at the time of 1st booster of DTP vaccine.
• Guidelines are provided for the use of new inactivated JE vaccines, JEEV® and
JENVAC ®
Specific recommendations
Cholera vaccination
Cholera Vaccine: IAPCOI
To be used in special circumstances.
These include travel to or residence in a highly endemic area and circumstances where there is risk of an outbreak such as during pilgrimages like Kumbh Mela etc.
Protection starts 2 weeks after receipt of the
2nd dose.
Rabies vaccine
Category 1: Touching or feeding of animals, licks of animal on intact skin.
Post-exposure prophylaxis is not recommended for category 1 exposures.
Category 2: Nibbling of uncovered skin by animal with resultant minor scratches or abrasions (without bleeding).
Post-exposure prophylaxis for category 2 exposures includes wound disinfection and administration of vaccine only. In contrast, the ACIP guidelines recommend both vaccine and RIG for this type of exposure..
Category 3: Single or multiple transdermal bites or scratches, licks on broken skin, contamination of mucous membrane with saliva, exposures to bats.
Post-exposure prophylaxis for category 3 exposure includes adequate wound care and RIG plus vaccine, as recommended by the ACIP.
Rationale for pre-exposure prophylaxis
Provides protection for inapparent exposures to rabies virus, such as in laboratory workers
Eliminates the need for rabies immune globulin (RIG) for post-exposure prophylaxis; this is particularly important in areas where RIG may be unavailable or unsafe
Affords some protection when postexposure prophylaxis may be delayed
Human-to-human transmission —
Human-to-human transmission of rabies can theoretically result from bite and non-bite exposures, but reports are very rare and poorly documented. However, human to human transmission arising from transplantation (corneas, organs, tissues) is well documented (see below).
Routine delivery of health care to a patient with rabies is only considered to constitute a rabies exposure if mucous membranes or nonintact skin come in contact with potentially infectious body fluids or tissues (such as saliva, CSF, and neural tissue)
cases of rabies have been reported in animals thought to be vaccinated, and therefore, we agree with current guidelines that suggest observation of such animals after an exposure occurs.
Small rodents, such as squirrels, chipmunks, rats, hamsters, gerbils, guinea pigs, mice, and lagomorphs (rabbits and hares) are almost never identified as infected with rabies virus; there has never been a case of transmission to a human from one of these animals.
The CDC guidelines for vaccine administration for postexposure prophylaxis in unvaccinated persons exposed to rabies changed in 2010, from a five-dose schedule of vaccine (given intramuscularly) starting immediately (day 0) after exposure and on days 3, 7, 14, and 28 after the first dose to a four-dose schedule eliminating the day 28 dose of the series [ 34,35 ]. This change was based on the following
[ 34,36 ]:
•Global epidemiologic studies demonstrating that rabies had not developed in any patient who received appropriate wound care, HRIG, and four doses of vaccine
•Immunogenicity studies showing that the fifth dose of rabies vaccine did not lead to a further increase in antibody titers
The WHO guidelines vary depending on the category of exposure. The WHO guidelines still recommend a five-dose schedule for intramuscular rabies immunization for category 2 or 3 exposures, but now cite the four-dose intramuscular schedule (days 0, 3,
7 and 14) as an alternative for exposed people who receive wound care plus highquality RIG plus rabies vaccine (approved by the WHO).
Another alternative four-dose regimen (two doses on day 0, and one dose on days 7 and 21) is sometimes used for category 2 exposures, when postexposure treatment does not include administration of RIG.
guidelines recommend the five-dose schedule in immunocompromised hosts
A previously vaccinated person who has had a potential rabies exposure should receive two intramuscular doses of vaccine; the first dose should be given on day 0, as soon after exposure as possible, and the other three days later.
The WHO guidelines also recommend two alternative intradermal regimens [ 1 ]:
One intradermal injection of 0.1 mL rabies vaccine at a single site on days
0 and 3
Four intradermal injections of 0.1 mL rabies vaccine in the upper arm or thigh all given on the same day
Furthermore, since latency periods between exposure and onset of disease as long as one to eight years have been reported [ 40,41 ], postexposure prophylaxis should be given following a rabies exposure, regardless of the length of the delay. Postexposure prophylaxis is never too early and is only too late when signs of clinical rabies are developing.
If a patient misses an injection, the immunization series should be continued until all doses have been administered.
Vaccine should be administered according to the regular intervals (eg, if day 7 vaccine is given on day 10, the next dose should be on day 17, 7 days later, etc.).
Failure of prophylaxis has been associated with:
Improper wound cleaning
Inadequate dosing of RIG
Absence of RIG administration in the wound site
Vaccine administration in the gluteal area
Intradermal schedule
WHO recommended the following intradermal regimen and vaccines for use by the intradermal route:
2-site intradermal method (2-2-2-0-1-1) for use with
PVRV (Verorab TM, Imovax TM, Rabies vero TM, TRC
Verorab TM) and PCECV (Rabipur TM)
For 2-site intradermal method (2-2-2-0-1-1)
The volume per intradermal site is:
0.1 ml for PVRV (Verorab TM, Imovax TM, Rabies vero
TM, TRC Verorab TM)
0.1 ml for PCECV (Rabipur TM)
Abbreviated multisite schedule
In the abbreviated multisite schedule, the 2-
1-1 regimen, one dose is given in the right arm and one dose in the left arm at day 0, and one dose applied in the deltoid muscle on days 7 and 21. The 2-1-1 schedule induces an early antibody response and may be particularly effective when post-exposure treatment does not include administration of rabies immunoglobulin.
Intramuscular schedules
One dose of the vaccine should be administered on days 0, 3, 7, 14 and 30. All intramuscular injections must be given into the deltoid region or, in small children, into the anterolateral area of the thigh muscle. Vaccine should never be administered in the gluteal region.
For category I no treatment is required, whereas for category II immediate vaccination and for category III immediate vaccination and administration of rabies immune globulin are recommended in addition to immediate washing and flushing of all bite wounds and scratches. Depending on vaccine type, the postexposure schedule prescribes intramuscular doses of
1 ml or 0.5 ml given as four to five doses over four weeks. For rabies-exposed patients who have previously undergone complete pre-exposure vaccination or post-exposure treatment with cellderived rabies vaccines, two intramuscular doses of a cell-derived vaccine separated by three days are sufficient. Rabies immune globulin treatment is not necessary in such cases.
Thank you.
Are you registered with www.idsurv.org
?