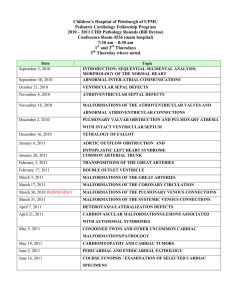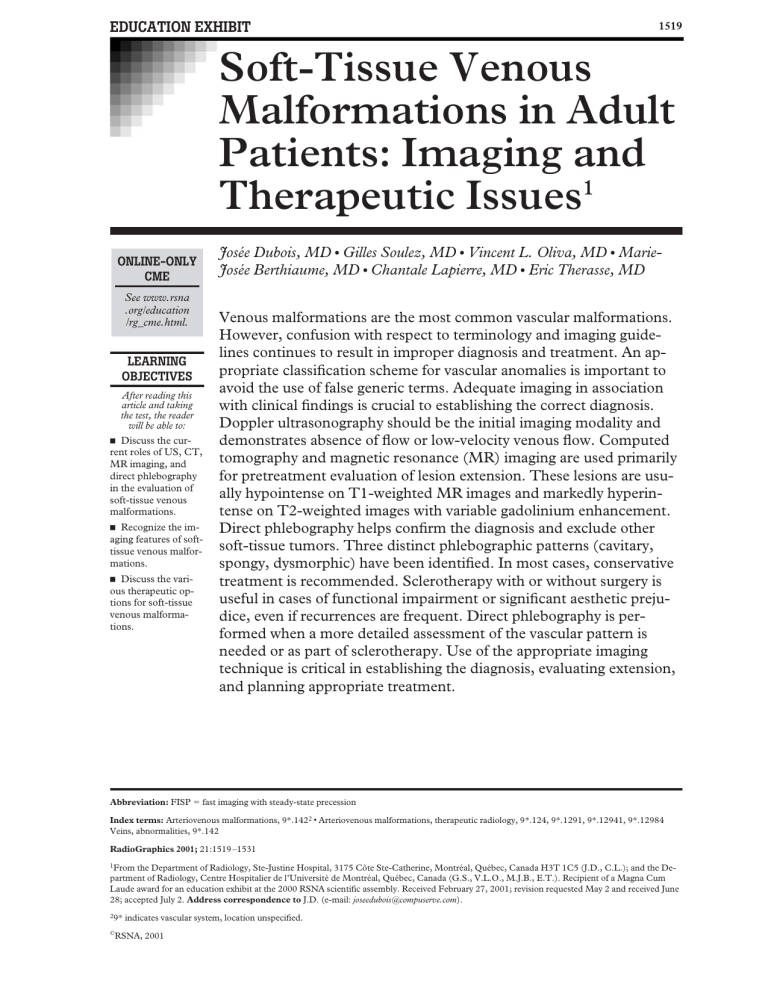
EDUCATION EXHIBIT 1519 Soft-Tissue Venous Malformations in Adult Patients: Imaging and Therapeutic Issues1 ONLINE-ONLY CME See www.rsna .org/education /rg_cme.html. LEARNING OBJECTIVES After reading this article and taking the test, the reader will be able to: 䡲 Discuss the current roles of US, CT, MR imaging, and direct phlebography in the evaluation of soft-tissue venous malformations. 䡲 Recognize the imaging features of softtissue venous malformations. 䡲 Discuss the various therapeutic options for soft-tissue venous malformations. Josée Dubois, MD ● Gilles Soulez, MD ● Vincent L. Oliva, MD ● MarieJosée Berthiaume, MD ● Chantale Lapierre, MD ● Eric Therasse, MD Venous malformations are the most common vascular malformations. However, confusion with respect to terminology and imaging guidelines continues to result in improper diagnosis and treatment. An appropriate classification scheme for vascular anomalies is important to avoid the use of false generic terms. Adequate imaging in association with clinical findings is crucial to establishing the correct diagnosis. Doppler ultrasonography should be the initial imaging modality and demonstrates absence of flow or low-velocity venous flow. Computed tomography and magnetic resonance (MR) imaging are used primarily for pretreatment evaluation of lesion extension. These lesions are usually hypointense on T1-weighted MR images and markedly hyperintense on T2-weighted images with variable gadolinium enhancement. Direct phlebography helps confirm the diagnosis and exclude other soft-tissue tumors. Three distinct phlebographic patterns (cavitary, spongy, dysmorphic) have been identified. In most cases, conservative treatment is recommended. Sclerotherapy with or without surgery is useful in cases of functional impairment or significant aesthetic prejudice, even if recurrences are frequent. Direct phlebography is performed when a more detailed assessment of the vascular pattern is needed or as part of sclerotherapy. Use of the appropriate imaging technique is critical in establishing the diagnosis, evaluating extension, and planning appropriate treatment. Abbreviation: FISP ⫽ fast imaging with steady-state precession Index terms: Arteriovenous malformations, 9*.1422 ● Arteriovenous malformations, therapeutic radiology, 9*.124, 9*.1291, 9*.12941, 9*.12984 Veins, abnormalities, 9*.142 RadioGraphics 2001; 21:1519 –1531 1From the Department of Radiology, Ste-Justine Hospital, 3175 Côte Ste-Catherine, Montréal, Québec, Canada H3T 1C5 (J.D., C.L.); and the Department of Radiology, Centre Hospitalier de l’Université de Montréal, Québec, Canada (G.S., V.L.O., M.J.B., E.T.). Recipient of a Magna Cum Laude award for an education exhibit at the 2000 RSNA scientific assembly. Received February 27, 2001; revision requested May 2 and received June 28; accepted July 2. Address correspondence to J.D. (e-mail: joseedubois@compuserve.com). 29* © indicates vascular system, location unspecified. RSNA, 2001 1520 RG f Volume 21 November-December 2001 ● Number 6 ISSVA Classification of Vascular Anomalies Vascular Malformations Vascular Tumor Simple Hemangioma Proliferative phase Involutive phase Other tumors Capillary malformation Lymphatic malformation (macrocystic, microcystic, mixed) Venous malformation Combined Arteriovenous fistula, arteriovenous malformation, capillary-venous malformation, capillarylymphatic-venous malformation (KlippelTrenaunay syndrome) Lymphatic-venous malformation, capillaryarteriovenous malformation (Parkes-Weber syndrome), capillary-lymphatic-arteriovenous malformation ... Note.—ISSVA ⫽ International Society for the Study of Vascular Anomalies. Source.—Reference 2. Introduction Venous malformations are part of a spectrum of vascular malformations commonly found in adults. A venous malformation is defined as a simple malformation with slow flow and an abnormal venous network. However, confusion in terminology, with misnomers such as hemangioma, cavernous hemangioma, phlebangioma, and phlebangiomatosis, continues to be responsible for improper diagnosis and illogical treatment. Venous malformations can be distinguished by their characteristic imaging findings at Doppler ultrasound (US), computed tomography (CT), magnetic resonance (MR) imaging, and direct phlebography. Interventional radiologic techniques play an important role in the management of venous malformations. In this article, we describe the imaging features of venous malformations that permit accurate classification and review the therapeutic options currently available for these lesions. Classification of Vascular Anomalies The most helpful classification scheme for vascular anomalies was described by Mulliken and Glowacki in 1982 (1). They have classified vascu- lar anomalies as either vascular tumors with endothelial hyperplasia or vascular malformations secondary to an error of embryonic development with normal endothelial turnover. This classification scheme is supported by clinical, histologic, histochemical, and biochemical differences as well as imaging features. A classification scheme for vascular anomalies based on cellular features, flow characteristics, and clinical behavior was updated during the 1992 meeting of the International Society for the Study of Vascular Anomalies (ISSVA) (Table) (2). Vascular malformations are also classified as slow-flow malformations (capillary, venous, lymphatic, capillary-venous, and capillary-lymphaticvenous malformations) and high-flow malformations (arteriovenous fistulas, arteriovenous malformations). Clinical Characteristics Venous malformations are characterized by a soft, compressible, nonpulsatile tissue mass. The overlying skin usually has a bluish tint, but occasionally it may appear normal. The main locations are the head and neck (40% of cases), extremities (40%), and trunk (20%). Venous malformations typically expand after the Valsalva maneuver and may be flattened with applied pressure. They tend to grow over time in proportion to the growth of the patient. They often enlarge during puberty RG f Volume 21 ● Number 6 Dubois et al 1521 Pathologic Features Histopathologic examination of venous malformations reveals thin-walled, dilated spongelike channels varying in size from capillary to cavernous dimensions, with sparse smooth muscle cells, adventitial fibrosis, thrombosis, and phleboliths (3). Smooth-muscle actin staining reveals muscle in clumps instead of the normal smooth-muscle architecture. The mural muscular anomaly is probably responsible for the gradual expansion (3). Genetic Features Figure 1. Venous malformation of the right parotid gland. Conventional radiograph demonstrates phleboliths (arrows). and pregnancy (due to hormonal influence) and do not regress. Symptoms are related to size and location. Although most venous malformations are in the skin and subcutaneous tissues, they also frequently involve underlying muscle, bone, and abdominal viscera. Most venous malformations are solitary, but multiple cutaneous or visceral lesions can occur. Deep cutaneous or intramuscular lesions usually cause discomfort, often in the early morning on awakening or with exertion. Intraoral venous malformations can bleed, distort dentition, cause speech problems, and obstruct the upper airway and pharynx. Thrombosis, swelling, and pain are common in venous malformations. Only symptomatic malformations or lesions causing important aesthetic prejudice require treatment. Coagulopathic Features A coagulation profile should be performed for any patient with an extensive venous malformation, especially if there is a history of easy bruising or bleeding. Stagnation within a venous malformation can cause localized intravascular coagulopathy (3). Venous anomalies usually occur sporadically, but families with dominant inheritance have been identified. In these families, a linkage to chromosome 9p21 has been established (4). This mutation causes ligand-independent activation of an endothelial cell–specific receptor tyrosine kinase, TIE-2. Familial forms of venous malformations with glomus cells (glomangioma) have also been linked to chromosome 1p21-p22 (5). Consequently, venous anomalies could be caused by gene mutations that regulate angiogenesis. Imaging Features Conventional Radiography Conventional radiography usually demonstrates a soft-tissue mass with occasional phleboliths and, occasionally, adjacent skeletal anomalies (Fig 1). Doppler US Doppler US is essential in differentiating venous malformations from other vascular anomalies. US should be performed with a high-frequency lineararray transducer (5–10 MHz). Exploration begins with a gray-scale examination to delineate the margins of the malformation. Venous malformations appear as hypoechoic or heterogeneous lesions in 80% of cases (6,7). Anechoic channels can be visualized in less than 50% of cases (Fig 2a). Sometimes, isoechoic thickening of the subcutaneous tissues without a solid mass or discernible channels is the only feature. Hyperechoic foci 1522 November-December 2001 RG f Volume 21 ● Number 6 Figure 2. Venous malformation of the cheek. (a) Gray-scale US image shows hypoechoic structures (arrows). (b) Doppler US image helps confirm the presence of low venous flow within the malformation. with posterior acoustic shadowing are seen in less than 20% of cases (6). In most cases, Doppler US demonstrates monophasic, low-velocity flow (Fig 2b). In 20% of lesions, no flow is demonstrated. This absence of flow may reflect thrombosis or be caused by equipment limitations (6). Computed Tomography At CT, venous malformations are hypoattenuating or heterogeneous lesions that enhance slowly and peripherally after bolus injection of contrast material (Fig 3a). CT usually demonstrates lesion extension, but MR imaging is more accurate in assessing the extension of venous malformations owing to its superior contrast resolution (Fig 3b, 3c). Phleboliths are more clearly depicted and fatty components are sometimes demonstrated at CT (Fig 4). Figure 4. Venous malformation of the left thigh. CT scan demonstrates a heterogeneous lesion in the vastus lateralis muscle. The hypoattenuating peripheral portion of the lesion (arrows) suggests the presence of fat. RG f Volume 21 ● Number 6 Dubois et al 1523 Figure 3. Venous malformation of the right masseter muscle. (a) Contrast material– enhanced CT scan shows a heterogeneous mass of the right masseter muscle with faint peripheral enhancement surrounding hypoattenuating areas. The presence of a phlebolith (arrow) confirms the diagnosis of venous malformation. (b) Fast spin-echo T2-weighted MR image depicts a cavitary lesion with septation. The lesion is clearly hyperintense. (c) Gadolinium-enhanced T1weighted MR image shows the lesion with partial heterogeneous enhancement, a finding that suggests partial thrombosis of the venous malformation. MR Imaging MR imaging is excellent for defining the extension of venous malformations and their relationship to adjacent structures. Examination protocol should begin with spin-echo or fast spin-echo T1weighted imaging for basic anatomic evaluation (Fig 5a). The extension of the malformation should be assessed with short-inversion-time in- version recovery (STIR) T2-weighted imaging with a 512 matrix (Fig 5b). Fat-suppressed fast spin-echo T1-weighted imaging should be performed after contrast material injection to evaluate perfusion of the malformation (Fig 5c, 5d). Gradient-echo T2*- 1524 November-December 2001 RG f Volume 21 ● Number 6 Figure 5. Venous malformation of the right plantar region. (a) Spinecho T1-weighted MR image shows diffuse enlargement of the medial plantar muscles. The lesion is hypointense and is difficult to differentiate from the normal muscular structures. (b) STIR T2-weighted image (512 matrix) clearly demonstrates the malformation within the plantar muscles. (c, d) Unenhanced (c) and contrast-enhanced (d) coronal T1-weighted images show perfusion of the malformation, which involves the first three layers of the plantar muscles. weighted imaging can also be used to demonstrate calcification or hemosiderin (Fig 6). The examination can be completed with three-dimensional fast imaging with steady-state precession (FISP) phlebography to appreciate the drainage of the malformation (Fig 7) (8). Venous malformations are usually hypo- or isointense at T1-weighted MR imaging. In cases of hemorrhage or thrombosis, heterogeneous signal intensity can be observed on T1-weighted images. Abnormal veins can be observed in the area of the malformation (Fig 8). At T2-weighted MR imaging, venous malformations display bright signal intensity. Areas of hypointensity related to thrombosis, septation inside the malformation, or phleboliths can also be observed (Fig 9). On T2-weighted MR images, the extension of the malformation into adjacent structures is Figure 6. Venous malformation of the right parotid gland. Gradient-echo T2*-weighted MR image clearly demonstrates a malformation within the right parotid gland with extension into the right parapharyngeal space. Phleboliths are well visualized as areas of hypointensity (arrows). RG f Volume 21 ● Number 6 Dubois et al 1525 Figure 7. Venous malformation of the right thigh. (a) Coronal STIR MR image demonstrates dysmorphic veins (arrows). (b, c) Gadolinium-enhanced MR phlebograms obtained with three-dimensional FISP show dysmorphic veins in the territory of the deep femoral vein (arrows). Figures 8, 9. (8) Venous malformation of the left arm. (a) Clinical photograph of the left arm demonstrates a softtissue lump. The bluish discoloration of the overlying skin suggests a venous malformation. (b) Sagittal spin-echo T1-weighted MR image reveals infiltration of the subcutaneous fat by a low-signal-intensity mass. Dysmorphic veins are present in the vicinity of the mass (arrow). (9) Venous malformation of the hand. T2-weighted MR image shows dysmorphic veins (arrows). 1526 November-December 2001 RG f Volume 21 ● Number 6 Figure 10. Venous malformation with extension. (a) Axial T1-weighted MR image shows a venous malformation infiltrating the fat surrounding the femoral vessel in the right inguinal region (arrows). (b) On a STIR T2-weighted MR image, the malformation is clearly demonstrated in the inguinal region (arrow). Involvement of the parametrium is also noted. Figure 11. Venous malformation of the elbow. (a) Spin-echo T1-weighted MR image shows an isointense mass (arrowheads) infiltrating the periarticular fat and the triceps muscle. Subtle infiltration of the subcortical bone medulla is also seen (arrow). (b) Axial T2-weighted MR image clearly demonstrates the malformation with involvement of the distal humeral bone and infiltration of the olecranon fossa and the distal portion of the triceps muscle. (c) Gadolinium-enhanced T1-weighted MR image demonstrates perfusion of the entire malformation. RG f Volume 21 ● Number 6 Dubois et al 1527 Figure 12. Venous malformation in a middle-aged woman with dysphagia and dysphonia. (a) Sagittal T2weighted MR image shows a large venous malformation of the cervical prevertebral region inducing compression of the pharynx. (b) T1-weighted MR image obtained after three sessions of sclerotherapy with alcoholic solution of zein and alcohol reveals significant shrinkage of the malformation, which now demonstrates heterogeneous signal intensity with small hyperintense areas. This finding may be related to recent thrombosis. (c) Gadolinium-enhanced MR image shows the malformation with heterogeneous enhancement (arrows). This finding may be related to a posttherapeutic inflammatory reaction and to residual perfusion of the malformation. usually clearly delineated (Fig 10). Gadoliniumenhanced T1-weighted imaging is useful in evaluating the circulatory portion of the malformation (Fig 11). After sclerotherapy, venous malformations demonstrate heterogeneous signal intensity on both T1- and T2-weighted images. A delay of up to several months is necessary to evaluate the therapeutic response after sclerotherapy, allowing time for the transient inflammatory reaction to resolve. In most cases, progressive shrinkage of the malformation is observed (Fig 12a, 12b). Gadolinium-enhanced imaging is useful in demonstrating residual perfusion of the malformation and directing additional treatment (Fig 12c). Although MR imaging is very sensitive for identifying and assessing the extension of venous malformations, it is not very specific. Findings must be correlated with clinical findings and Doppler US findings to make the diagnosis. In cases of atypical clinical or imaging findings, percutaneous phlebography must be performed to confirm the diagnosis. If phlebographic findings are inconclusive, percutaneous or surgical biopsy must be performed to rule out malignant disease. In summary, a standard MR imaging examination should include fast spin-echo T1-weighted imaging with and without fat saturation. STIR is the preferred T2-weighted sequence, and gradient-echo T2*-weighted imaging is useful in evaluating bleeding or thrombosis or demonstrating calcification. Gadolinium-enhanced fat-suppressed fast spin-echo T1-weighted MR imaging is mandatory. Phlebography is optional and can be used if dysplastic veins are suspected. During posttreatment follow-up, MR imaging should be performed with the same specifications as those used for the baseline examination. Direct Percutaneous Phlebography Direct percutaneous phlebography can be performed as a diagnostic procedure in cases of atypical venous malformation. Opacification of abnormal venous cavities allows confirmation of the diagnosis of venous malformation and exclusion of other diagnoses such as benign or malignant soft-tissue tumors. Direct percutaneous phlebography is also frequently performed as the initial step during sclerotherapy. Direct needle puncture of the malformation is performed with a 20- or 21-gauge needle. US or CT can be useful 1528 November-December 2001 RG f Volume 21 ● Number 6 Figure 14. Direct phlebography and sclerotherapy of a venous malformation of the foot. (a) Clinical photograph shows a sclerotherapeutic procedure. Because the lesion was superficial, we used a 21-gauge butterfly needle. Venous return was observed, confirming the proper positioning of the needle. (b) Direct phlebogram demonstrates a venous malformation with a cavitary portion (straight arrow) and drainage into dysmorphic veins (curved arrow). Figure 13. CT scan demonstrates direct needle puncture of the venous malformation in the same patient as in Figure 12. in guiding the needle, especially if the malformation is located deep in the soft tissues (Fig 13). The needle is connected to a syringe through a length of extension tubing and is progressively withdrawn while applying slight suction (Fig 14a). Once blood return is observed, a small Figure 15. Venous malformation of the elbow. Direct phlebogram demonstrates a venous malformation with a cavitary pattern. amount of low-osmolarity iodinated contrast material is injected to obtain a phlebogram (Fig 14b). Three different phlebographic patterns can be observed with venous malformation opacification. The most common of these is a cavitary pattern with late venous drainage without evidence of abnormal veins (Fig 15), the second is a spongy RG f Volume 21 ● Number 6 Dubois et al 1529 Figure 16. Venous malformation of the right thigh. Direct phlebogram demonstrates a venous malformation with a spongy pattern. Figure 18. Venous malformation of the anterior portion of the elbow. Peripheral phlebogram demonstrates a malformation and its venous drainage. pattern with small “honeycomb” cavities and late venous drainage (Fig 16), and the third is rapid opacification of dysmorphic veins (Fig 17). Peripheral Phlebography In most cases, peripheral limb phlebography is not helpful in the diagnosis of venous malformations of the upper or lower limbs because most of these malformations will not demonstrate opacification. In cases of venous malformations composed of dysmorphic veins, peripheral phlebography is helpful in demonstrating the venous drainage of the malformation (Fig 18). Arteriography Arteriography is usually not required for the diagnosis of venous malformations. Findings can be normal or demonstrate dysmorphic veins in the late venous opacification phase. Arteriography may be useful in cases of complex malformations such as capillary-venous malformations or in Figure 17. Venous malformation of the hand. Direct phlebogram demonstrates a venous malformation with dysmorphic veins and early drainage. 1530 November-December 2001 RG f Volume 21 ● Number 6 Figure 19. Complex venous malformation of the temporal area. (a) External carotid angiogram demonstrates progressive filling of venous structures. (b) Delayed-phase angiogram shows stagnation of the contrast material in the venous lakes. Because no washout of the dysmorphic veins was observed, the term microfistula is probably not appropriate. This malformation demonstrated high venous flow at Doppler US. Arterial embolization was performed to decrease the flow, followed by direct embolization with alcohol. demonstrating microfistulas (Fig 19). The pathophysiology and clinical significance of these microfistulas are unclear. Treatment Medical Treatment Lower-extremity venous malformations should first be treated with elastic stockings. Low doses of aspirin seem to minimize phlebothromboses. Preoperative control of intravascular coagulopathy with heparin should be considered before the resection of large venous malformations (3). Sclerotherapy Treatment of venous malformations is indicated when they cause aesthetic problems, pain, or functional problems. Absolute ethanol is the most commonly used agent (9). Alcoholic solution of zein (Ethibloc; Ethicon, Norderstedt, Germany), a mixture of zein (a corn protein), alcohol, and contrast medium, is commonly used in Europe (10). The main drawback of this agent is its propensity to induce cutaneous fistulization with extrusion of the agent. In cases involving very superficial cutaneous or oromucosal lesions, sodium tetradecyl sulfate is preferred to minimize the risk of superficial necrosis. Sclerotherapy should be performed under fluoroscopic control by a skilled interventional radiologist. The amount of sclerosing agent required is evaluated with percutaneous phlebography. It is important to avoid filling drainage veins with the sclerosing agent. A tourniquet or manual compression is useful in minimizing passage of the sclerosing agent into the systemic circulation. The main complications of sclerotherapy are cutaneous necrosis and neural toxicity, especially with alcohol. Systemic complications are rare and are related to the passage of alcohol into the systemic circulation. These include hemolysis with potential renal toxicity and cardiac arrest. Sclerotherapy induces an inflammatory reaction that will worsen the symptoms during the week following intervention. Analgesics and antiinflammatory agents (nonsteroidal anti-inflam- RG f Volume 21 ● Number 6 matory agents or corticoids) must be given to minimize the symptoms. There should be a time delay of 1–3 months between each sclerotherapy session. Venous anomalies have a propensity for recanalization and recurrence (11). We have observed better results with sclerotherapy in cases involving cavitary lesions and dysmorphic vein patterns, although the latter are more prone to recurrence. Spongy patterns, especially when they are intramuscular, are more difficult to treat. Because of the significant inflammatory reaction that follows sclerotherapy, it is recommended that a control MR imaging examination not be performed until 6 months after the last session. Surgical Resection Surgery is generally contemplated after sclerotherapy when treatment is incomplete or when an aesthetic prejudice requires correction. Laser Therapy Laser therapy can be useful in very superficial forms of venous malformations and in oromucosal lesions. Photocoagulation can be performed with argon, yellow dye, or a neodymium yttrium aluminum garnet laser. For deeper lesions, laser probes can be inserted subcutaneously. Satisfactory results with minimal scarring have been reported (12), but recurrences and repeated treatments are common. Summary Venous malformations are relatively easy to recognize. Radiologists play a key role in avoiding inappropriate treatment of these lesions. The first rule is to refer to a proper classification scheme for vascular anomalies and avoid the use of false generic terms such as hemangioma (which is not seen in adult patients). Absence of flow or lowvelocity venous flow is observed at Doppler US. MR imaging is very useful in assessing the extension of venous malformations. These lesions are usually hypointense on T1-weighted images and markedly hyperintense on T2-weighted images. Gadolinium enhancement is present but variable. Direct phlebography is useful in confirming the diagnosis and excluding other soft-tissue tumors. Dubois et al 1531 Three distinct phlebographic patterns (cavitary, spongy, dysmorphic) have been identified. Conservative treatment is recommended in most cases. In cases of functional impairment or significant aesthetic prejudice, sclerotherapy with or without surgery is useful even if recurrences are frequent. References 1. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982; 69:412– 422. 2. Enjolras O. Classification and management of the various superficial vascular anomalies: hemangiomas and vascular malformations. J Dermatol 1997; 24:701–710. 3. Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg 2000; 37: 517–584. 4. Boon LM, Mulliken JB, Vikkula M, et al. Assignment of a locus for dominantly inherited venous malformations to chromosome 9p. Hum Mol Genet 1994; 3:1583–1587. 5. Boon LM, Brouillard P, Irrthum A, et al. A gene for inherited cutaneous venous anomalies (“glomangiomas”) localizes to chromosome 1p21-22. Am J Hum Genet 1999; 65:125–133. 6. Trop I, Dubois J, Guibaud L, et al. Soft-tissue venous malformations in pediatric and young adult patients: diagnosis with Doppler US. Radiology 1999; 212:841– 845. 7. Paltiel HJ, Burrows PE, Kozakewich HP, Zurakowski D, Mulliken JB. Soft-tissue vascular anomalies: utility of US for diagnosis. Radiology 2000; 214:747–754. 8. Li W, David V, Kaplan R, Edelman RR. Threedimensional low dose gadolinium-enhanced peripheral MR venography. J Magn Reson Imaging 1998; 8:630 – 633. 9. Dubois JM, Sebag GH, De Prost Y, Teillac D, Chrétien B, Brunelle FO. Soft-tissue venous malformations in children: percutaneous sclerotherapy with Ethibloc. Radiology 1991; 180:195–198. 10. Berenguer B, Burrows PE, Zurakowski D, Mulliken JB. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg 1999; 104:1–11. 11. De Lorimier AA. Sclerotherapy for venous malformations. J Pediatr Surg 1995; 30:188 –193. 12. Derby LD, Low DW. Laser treatment of facial venous vascular malformations. Ann Plast Surg 1997; 38:371–378. This article meets the criteria for 1.0 credit hour in category 1 of the AMA Physician’s Recognition Award. To obtain credit, see www.rsna.org/education/rg_cme.html.