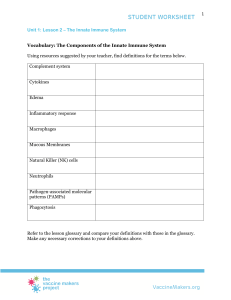
PATHOGENESIS OF PERIODONTITIS AND HOST RESPONSE I 1 Dr SC Manenzhe BDS 3 /2019 OBJECTIVES Discuss microbial plaque and host interaction Microbial Virulence factors Kornman pathogenesis of periodontitis model of 1997 From health=gingivitis=periodontitis Chappel model Periodontitis multifactorial disease Discuss Immuno-inflammatory response Innate and adaptive immunity interactive relationships/the difference? Cellular components of the immune system Major histocompatibility complex (MHC-I & II) Inflammatory mediators Pattern recognition receptors Toll like receptors & PAMPS Complement cascade Osteo-immunology (RANK/RANKL/OPG) 2 INTRODUCTION Pathogenesis =The development of a disease and the chain of events leading to that disease Process by which the aetiologic factor + other factors cause diseases Disease expression and progression reflects the interplay between: The microbial plaque (including complexes +AA), the host’s immuneinflammatory response and environmental factors Periodontitis is polymicrobial infection Gingivitis =precursor for periodontitis An understanding of the aetiology and pathogenesis of periodontitis provides a basis for treatment planning and future risk assessment 3 HOST AND DENTAL PLAQUE INTERACTION Microbial Attack vs. Defense Reactions by the Host The virulence of bacteria: their capability to invade into tissues their number and composition their metabolic products (enzymes & toxins) and “signal” substances that activate macrophages and T-cells Elicit reactions by the host (immune-inflammatory response). Whether periodontal disease will occur, and its severity, depends Upon the bacterial insult and host response 4 EVOLUTION: PATHOGENESIS OF PERIODONTAL DISEASE 1960’s model 1980’s model (Source: Kornman, K.S., 2008. Mapping the pathogenesis of periodontitis: a new look. Journal of periodontology, 79(8S), pp.1560-1568.) Pathogenesis of periodontitis Kornman, Page and Tonetti 1997: model of pathogenesis of periodontitis Critical !! 6 DEVELOPMENT OF COMPLEXES Bacteria no longer work as single entities: The biofilm acts and reacts as a stable “organism.” Pathway (A-G) leads to the “red complex,” Pathway (A-D) leads to Aa. Complex development Dependent upon host response, availability of nutritive substances, and interbacterial competition 7 VIRULENCE FACTORS OF (PG) 8 Pg is a strict anaerobe, and is therefore present in increased numbers in deep pockets VIRULENCE FACTORS OF (AA) 9 MICROBIAL CHALLENGE ROLE IN PERIODONTAL TISSUE DESTRUCTION In order to elicit periodontitis, microorganisms must: • Establish themselves near the host tissue • Avoid being eliminated by saliva or exudates • Avoid the defense mechanisms of the host and other microorganisms • Find appropriate nutrition • Be capable of destroying periodontal tissues. Progressive periodontitis is characterized not only by elevated levels of bacterial substances e.g LPS But also by pro-inflammatory mediators. 10 Microbial plaque biofilm=initiates and perpetuates the inflammatory response The nature of the immune-inflammatory response =major determinant of sucseptibility to periodontitis It is paradoxical that the defense mechanisms (has protective intent) result in majority of tissue destruction seen Susceptible host Excessive or dysregulated host response==increased tissue breakdown 11 MICROBIAL PLAQUE NECESSARY BUT NOT SUFFICIENT Aetiology of Periodontitis Interaction between: Dental Plaque + the susceptible Host Influence the existence and the clinical course of periodontitis Modify immune-inflammatory response. Time Influence plaque formation + host immune response Influence the systemic and psychic well being Influence the immune status. 12 13 HOST SUSCEPTIBILITY –HOST RESPONSE TO INSULT Maintaining periodontal health involves a complex immune response to the plaque biofilm. Surveillance by the immune system protects an individual by recognizing and responding to antigens, When the immune system is overwhelmed, clinical symptoms of disease become evident. Responsiveness of the immune system + the amount and type microorganisms/ various antigens • Defective immune responses • Hyperreactive immune BIOLOGICAL AND CLINICAL SIGNS OF INFLAMMATION Inflammation is a wellcoordinated process to plaque accumulation and includes: Increased vascular permeability Classical signs of inflammation: Red Swollen Secretion of inflammatory mediators and activation of complement system Painful Hot Migration of PMN; monocytes (macrophage) and lymphocytes into the tissues Possible loss of function HOST RESPONSE: MECHANISMS + COMPONENTS First Axis of the Host IMMUNE System consists of: • Phagocytes, NK cells and also diverse molecular effectors (complement, Creactive protein, etc.) • complement Second Axis of the IMMUNE System consists of: • Specific immunity • Lymphocytes (T- and B-cells) • Antigen-presenting cells (APC) e. g., macrophages/MΦ) • The various immunoglobulins. Each and every cell that is involved in maintenance of periodontal tissue integrity • Synthesizes a large spectrum of cytokines and other mediators. 16 • Even the resident (non-mobile) cells are active in the immunologic process. HEALTH Homeostasis PERIODONTITIS Plaque accumulation Non-specific 17 Shift in microbial flora Murakami et al., 2018 Clinical Flow Diagram: From Gingivitis to Periodontitis 18 THE TWO DISTINCT ARMS OF THE IMMUNE RESPONSE The innate immune response Not antigen specific (no memory) • Response the same with each exposure Physical barrier Adaptive immune response The distinction of the 2 has become blurred over the years • Responsiveness enhanced with the discovery that: Antigen specific with repeated antigen exposure • Recognition of the pathogens (immunologic memory) Delayed response time Immediate protection Antibodies, cytokines Cytokines, complements The innate immune response determines the nature of the subsequent adaptive response Aspects of the adaptive response control the effectiveness of the innate response stronger 19 IMMUNITY “Free of burdens” In medical terms it denotes Freedom from disease Resistance to infectious disease 20 HOST RESPONSE: COMPONENTS 21 Facilitates cell-cell relationships ,signal formation, antigen presentation 22 PATHOGENESIS OF PERIODONTITIS 23 INNATE IMMUNITY RESPONSE Components present before the onset of infection. Disease resistant mechanisms that are not specific to a particular pathogen Pathogens must first breach barriers that protect host Provides the first line defence right after exposure. Most micro-organisms are readily cleared within a few days by innate immune system before adaptive immune system is activated 24 INNATE DEFENSE SYSTEMS: 1ST LINE OF DEFENSE NONSPECIFIC IMMUNITY POSSESSES NO “MEMORY.” Vascular and cellular inflammatory responses Barrier mechanisms: physical & chemical Complement cascade Vascular Gingival crevicular inflammatory events fluid Cellular Saliva inflammatory events (PMN’s) Oral epithelium 25 SALIVA Saliva 26 CONSTITUTION OF GCF Cellular Elements • Bacteria, desquamated epithelial cells, and leukocytes (PMNs, lymphocytes, monocytes/macrophages) Electrolytes • Potassium, sodium, and calcium Organic Compounds • Carbohydrates and proteins Metabolic and bacterial products • Lactic acid, urea, hydrogen sulfide 27 GCF ROLE IN IMMUNITY JE allows movement of GCF and the cells molecules of innate immunity Flushing action Brings the blood components (e.g., neutrophils, antibodies, and complement components) of the host defenses into the sulcus. The flow of GCF increases in inflammation 28 Flushing effect 1. Flushing action 2. Brings blood components to the area 29 EPITHELIAL ROLE IN IMMUNE RESPONSE 1. Barrier Keratinization Shedding 2. Pattern recognition receptors 3. Microbial plaque recognition molecules Releases IL-1, IL-8 (Chemotactic for PMN) 30 LOSS OF EPITHELIAL INTEGRITY In the depth of the active pocket bacteria invade the connective tissue (red bars) via the ulcerated epithelium Tissue damage 31 Vascular and cellular immunoinflammatory responses Barrier mechanisms Vascular events Gingival crevicular fluid Complement cascade Cellular events (PMN’s, Macrophages, Saliva Natural killer cells) • Involves the mechanisms of pathogen recognition, phagocytosis Oral epithelium (killing and digesting of • Physical microorganisms) and acute barrier inflammation Epithelial cells Via Toll like receptors • Immunologic process 32 VASCULAR INFLAMMATORY RESPONSE Bradykinin: Increases vascular pearmeability (Source: https://www.slideshare.net/SimbaSyed/acute-inflammation-21504202) PATTERN RECOGNITION RECEPTORS Family – Toll like receptors (TLRs) Expressed predominantly in cells which mediate first-line defense. • e.g. neutrophils, monocytes/ macrophages, and dendritic cells, as well as epithelial cells • The activation of PRR in this cells activates innate immune response TLRs have the ability to recognize structures known as pathogen‐associated molecular patterns (PAMPs) across wide variety of pathogens • They bind microbial cell molecules, such as lipopolysaccharides, microbial fimbriae, and lipoteichoic acid (GRAM +VE) The activation of TLR e.g. TLR-4 (principal LPS receptor) & TLR-2 induces the expression of a variety of cytokines that are crucial in adaptive immune responses. 34 PATTERN RECOGNITION RECEPTORS (PRRS) The discovery of TLRs have prompted the “bar code” hypothesis of innate recognition of microbes. TLRs read a “bar code” on microbes and the interaction result in: Intracellularly tailored appropriate type of innate responseare to plaque biofilm Different TLR respond to different PAMPs 35 Recognition of PAMPs Interaction of PAMPs with TLRs 36 Connective tissue and bone destructionm Cells with first line of defense + epithelial cells PAMPs Tissue repair Activation of innate and adaptive immune system 37 TLR ACTIVATION LEADS TO Regulation of the innate immune response Regulation of the adaptive immune response Inflammation Tissue repair Toll-like receptors interact with pathogens and induce cytokines, which may aggravate disease 38 PAMPS AND PRR INTERACTION The activation of toll-like receptors with bacterial components triggers a cascade of intracellular signaling mechanisms Production of Inflammatory mediators Activation of Bcells Barros and Offenbacher, 2014 INNATE-IMMUNE RESPONSE ==MEDIATED MAINLY BY: Neutrophils Macrophages 40 Phagocytosis and degranulation PMN Protective cell Defective neutrophil function is associated with periodontal destruction=increased susceptibility to periodontitis include abnormalities in Adherence, Chemotaxis decrease of neutrophil migration in the presence of a chemotactic gradient Phagocytosis and bactericidal activity. Superoxide generation, Deficiencies in PMN function are associated with severe and rapidly progressive periodontitis 42 Cellular/molecular pathway signaling cytokine signaling and cell The stimulation of macrophages (MΦ) by LPS initiates the immune response and the inflammatory response 43 Vascular and Barrier INNATE DEFENSE SYSTEMS cellular mechanisms inflammatory responses Complement cascade Vascular Gingival crevicular inflammatory events fluid Soluble factors C-1 to tC-9 that circulate in the blood 7 tissue fluids Cellular Saliva inflammatory events (PMN’s) • Opsonization of pathogens • Recruitment of inflammatory cells • MAC=direct killing of pathogens (Bactricidal) Oral epithelium (pattern recognition receptors) 44 COMPLEMENT CASCADE Consists of plasma proteins Bind covalently to pathogens, opsonizing them for engulfment by phagocytes bearing receptors for complement. The most important action of complement is to facilitate the uptake and destruction of pathogens by phagocytic cells 45 Activated initially independent of antibodies via the alternative pathway (APW) later activation is dependent on antibodies via the classical pathway (CPW) Opsonization, chemotaxis, membrane destructive -MAC 46 Schematic overview of the complement cascade Activation of C3 MAC Macrophages and neutrophils phagocytosis 47 Cell/molecules Characteristics Functions/effects 48 CYTOKINES Cytokines are hormone-like soluble proteins that act as messengers that initiates / maintains an immune response • They are key inflammatory mediators • In combination with other mediators they build a large network responsible for normal tissue homeostasis & immune response. They regulate important biological processes: • Cell proliferation, cell growth, cell activation, inflammation, immunity and repair. Some cytokines e. g., IL-8 have a chemotactic effect on immune cells Members of the cytokine family include: • Interleukins (IL) • Cytotoxic factors (tumor necrosis factor (TNF) α and β) • Interferons (anti-viral IFNα and β, “immune-IFNγ”) • Colony stimulating factors (CSF) • Growth factors (GF) 49 CYTOKINES…… Most of the cytokines primarily act locally in tissues where they are produced, others have systemic effect e.g. TNF, IL-1, IL-6 etc. •They can induce their own expression in an autocrine or paracrine fashion •They pleitropic effects on different cells Bind to specific receptors on target cells •Initiate intracellular signaling cascades resulting in phenotypic changes The cytokine-producing cells and their target cells exchange signals continuously. •Supports primarily tissue homeostasis The host response to periodontal infection requires expression of proinflammatory (IL-1, IL-6IL-8,TNFα, IFNγ) and antiinflammatory cytokines,(IL-1 ra (receptor antagonist), IL-10, TGFβ) 50 Cytokines are not stored but are constantly produced , epithelial 51 52 Host-Microbial interaction NB determinant of whether disease will be established opr not 53 The host cellular activation as protective against microbial assault and the acquired immune activation with chronic inflammation and cytokine networks modulating the connective tissue response. 54 INNATE IMMUNE RESPONSE Does not require previous exposure to the offending organism Important for initiating the immune response to new exogenous microbial challenges. Mediate acute exacerbations of a chronic inflammatory state