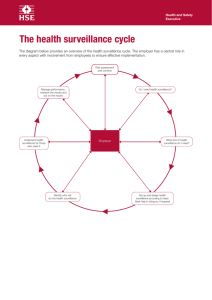
Surveillance & Notification Prince Naeem BSN-RN, M. Phil (EPI-PH) Control of Communicable Diseases: Tools • Isolation • Treatment • Disinfection & Barriers • Quarantine & Surveillance • Vaccination • Prophylaxis Could you drive without looking at the traffic? Can you make public health decisions in the absence of data? SURVEILLANCE • French word means watch over. • Close observation of a person or group, especially one under suspicion. “The continued watchfulness over the distribution & trends of incidence through the systematic collection, consolidation, & evaluation of morbidity/mortality reports & other relevant data, together with dissemination to those who need to know.” (LANGMUIR, 1963) ”A systematic ongoing collection, collation, analysis of data for public health purposes & timely dissemination of public health information for assessment & public health response as necessary.” (World Health Assembly 2005) Definitions of Surveillance “Surveillance serves as the brain & nervous system for programs to prevent & control disease.” (D.A. HENDERSON, 1976) “Ongoing systematic collection analysis, interpretation of health data, essential to planning, implementation, & evaluation of public health practice, closely integrated with timely dissemination of these data to those who need to know. ” (CDC-1986) “Continuous analysis, interpretation & feedback of systematically collected data, generally using methods distinguished by their practicality, uniformity & rapidity, rather than by accuracy & completeness”. (WJ Eylenbosch & ND Noah: Surveillance in Health & Disease. Oxford University Press 1988) Definitions of Surveillance Key Elements 1. Collection of health data expressly for use in health planning, disease control/ prevention, &/or health promotion 2. Ongoing collection of data 3. Timely analysis 4. Easily understood 5. Dissemination of results 6. Action based on results 7. Periodic evaluation of the system Historical Perspective First use for Public Health Action William Farr (1807 – 1883) • Superintendent, statistical department, General Register Office, UK • Collected, analyzed, interpreted vital statistics • Plotted rise & fall of epidemics of infectious diseases, identifying associations • Disseminated information weekly/quarterly/annually/medical journals public press Recognition by World Health Organization 21st World Health Assembly (1968) "Information for action" • Systematic collection of pertinent data • Orderly consolidation & evaluation of these data • Prompt dissemination of the results to those who need to know Surveillance System/ Loop Health care system & Surveillance centre Event Data Planning, Evaluation, Policy formulation Action Information Feedback, recommendations Analysis, interpretation Reporting Event & Population Under Surveillance •Event •Disease •Syndrome – Acute flaccid paralysis – Influenza-like illness – Diarrhoea •Infection •Public health issue – Antimicrobial resistance •Environment – Vector population – Water quality •Population & Time • Everyone in the country or region • Patients in hospitals • Employees in a factory • All children in the winter months Aims of Surveillance Process of doing something: examples • Manage contacts of a case • Detect outbreaks • Early warning • Design/change vaccination policy • Design policy re antimicrobial resistance • Evaluate interventions to improve them • Certify elimination / eradication Aims of Surveillance Public Health Aims Assess Public Health Status (Monitor Trends, Detect Outbreaks) - Prevent And Control Disease Define Public Health Priorities - Plan Considering Impact Of Hazard, Exposure, Disease Evaluate Public Health Programmes - Make Decisions Regarding Interventions Stimulate Or Inform Research - Generate Hypotheses, Inform Methodologie Principles of Surveillance • A key principle is to include only conditions for which surveillance can effectively lead to prevention. Another important principle is that surveillance systems should reflect the overall disease burden of the community. Other criteria for selecting diseases include: • The surveillance plan should include a detailed M & E plan • Incidence & Prevalence • Indices Of Severity (Case-fatality Ratio) • Mortality Rate & Premature Mortality • An Index Of Lost Productivity (Bed-disability Days) • Medical Costs • Preventability • Epidemic Potential • Information Gaps On New Diseases • Public Concern & News-worthiness Requirements for Surveillance Diagnostic Algorithm Costs Availability Of Data Staff Members Sampling Frame Access/Network Competent Laboratory Surveillance Vs. Screening & Research Surveillance: Data collection to measure magnitude, changes, & trends in populations The objective is intervention in defined populations Screening: Testing to identify individuals with infection or disease Measurement of prevalence in screened populations Research: Pursues new knowledge from which better control measures will result Systematic investigation, testing & evaluation, designed to develop or contribute to knowledge. Steps in Setting Up Surveillance System 1. Understand the problem 2. Identify opportunities for prevention & control - Interventions/Selection of Population 3. Set objectives 4. Specify requirements to meet objectives 5. Design - Case definitions & indicators/Data needed/Data sources/Data transfer 6. Translate information into action - Analyse/Interpret/Disseminate 7. Evaluate surveillance system Understand The Problem Exposure Transmission Environment Vector Direct Source Of Infection Infection Disease Death Disability Reservoir Recovery Identify Opportunities For Prevention & Control Exposure Transmission 6. Prevent transmission e.g. universal precautions 1. Vaccination 4. Isolation/Treatment Environment Vector Direct Source Of Infection Infection 2. Prophylaxis 5. Ecological Management Disease Reservoir 3. Treatment Death Disability Recovery Surveillance Systems Selecting the Population Defining the selection criteria Human populations Zoonotic populations Gaining access to target populations NGOs/support groups Obtaining & maintaining compliance Set Objectives Objectives should be SMART: • Specific • Measurable • Acceptable and Action oriented • Realistic • Time related Indistinct... • To estimate the prevalence of hepatitis C Specific, Measurable, Action-oriented & Timed • To assess the prevalence of hepatitis C in Lahore in order to allow planning of specific health care needs for the coming 20 years Surveillance Systems Selecting The Appropriate Strategy & The Reservoir Need for cultural sensitivity Understanding the implications & limitations of different strategies Selecting the appropriate surveillance strategy For surveillance, want a representative sample For finding the reservoir, or finding infected individuals Defining A Case (Case Definition) Establishing a functional case criteria Quickly & easily defined Selecting the right test or definition Easy, specific Clinical versus epidemiological diagnostic criteria Function over precision Disease versus infection AIDS & HIV infection Case Definition YES NO A case is an event A case is not a person An event is something that happens to: Events do not exist if you lack info: A person, In a given place, At a given time A case definition is a set of criteria that triggers reporting On the person On the place On the onset date A case definition is not a diagnosis made to decide treatment Surveillance Methods Key Data Items Collected – Numerators – Number of cases of disease – Antibody positive samples – Number of resistant strains – Descriptors – Characteristics of patients, strains etc – Denominators – Total population at risk (or sub-sample) in a given time frame – Total number of strains examined Surveillance Data Sources Common sources – Notifications of infectious Dx. & biological changes in agent/vectors/reservoirs – Microbiology laboratory reports & vaccine utilization – Hospital episode statistics and records – Primary care spotter practices – Blood banks & screening programmes (antenatal, blood donors) – Prescriptions/over the counter drug sales – Mortality and morbidity reports – Outbreak reports – Sickness absence records For example, Surveillance Systems Other Considerations Timely data processing Results and action Interpretation Facilitating appropriate action based on surveillance results Evaluation & Revisions Importance of ongoing evaluation Revising the surveillance program When & Why Surveillance Systems Surveillance Study Designs Cohort studies Cross-sectional studies/surveys Serial cross-sectional studies Mortality surveillance Sentinel surveillance Syndromic (early outbreak detection) Passive Surveillance • This form of data collection, in which health-care providers send reports to a health department on the basis of a known set of rules & regulations, is called Passive surveillance (provider-initiated). • Passive surveillance often gathers disease data from all potential reporting health care workers. Health authorities do not stimulate reporting by reminding health care workers to report disease nor providing feedback to individual health workers. • Most common type of surveillance in humanitarian emergencies. Most surveillance for communicable diseases is passive. Passive = reporting Hospitals, Laboratories, Clinics, Physicians Active Surveillance • Active surveillance (health department- initiated) is usually limited to specific diseases over a limited period of time, such as after a community exposure or during an outbreak. • Active surveillance requires significantly more time & resources & is therefore less commonly used in emergencies. • Community health workers may be asked to do active case finding in the community in order to detect those patients who may not come to health facilities for treatment. Active = searching Sentinel Surveillance Monitoring of rate of occurrence of specific conditions to assess the stability or change in health levels of a population. It is the study of disease rates in a specific cohort such as in a geographic area/population subgroup to estimate trends in larger population. (CDC) A sentinel surveillance system is used when high-quality data are needed about a particular disease that cannot be obtained through a passive system. Selected reporting units, with a high probability of seeing cases of disease in question, good lab facilities & experienced well-qualified staff, identify & notify on certain diseases. A sentinel system deliberately involves only a limited network of carefully selected reporting sites. (WHO) Sentinel Groups (HIV) Homosexual/bisexual Commercial sex workers Returning overseas workers Intravenous drug users Males at STD clinics Other groups Analysis Of Surveillance Data Descriptive use –Measure of disease frequency –Incidence (no. Cases/population at risk over given time period) e.g. 5 cases per 1000 person years; 0.3 cases per 1000 persons –Prevalence (no. Cases/population at risk at a set time) e.g. 15% patients sampled antibody +ve; 3% strains erythromycin resistant –Data described according to time-person-place Analytical use –Comparison between groups to gain a measure of increased risk e.g. Case fatality in males vs females e.g. Change in rate of infection over time Characteristics/Requirements & Evaluation of A Surveillance System Sensitivity Timeliness Representativeness Predictive value positive Acceptability Flexibility Simplicity Cost/benefit Dissemination of results Appropriate action taken Representativeness Do reported cases differ from unreported cases? Timeliness Is information disseminated rapidly enough to permit timely action based on the surveillance system? Predictive Value Positive What proportion of those identified actually have the disease or factor? Sensitivity What proportion of “cases” are identified? Does the system give an accurate picture of trends and magnitudes? Acceptability Does the system stimulate the cooperation of respondents? Does the process discourage participation? Flexibility Can changes be easily made in the system to reflect changes in trends, magnitude, and other relevant factors? Simplicity Can the system be simplified & still obtain the necessary information? Cost/Benefit Is the system worth the cost? Can costs be reduced without sacrificing the essential quality of the system (e.g., each 12 vs each 6 months)? Dissemination Of Results To decision-makers To data collectors To the general public Appropriate Action Taken Are appropriate actions taken in response to the surveillance data? Does surveillance lead to effective intervention? Uses of Surveillance • Recognize isolated or clustered cases/early epidemic detection & assess how big a problem is. i.e. Human disease Zoonotic diseases Food safety Drug-resistant organisms (e.g., MDR-TB) • Assess the Community health impact of events & assess trends/pattern of disease/health problems. Prevalence/incidence of disease and/or risk factors Emerging diseases Geographic distribution Risk group distribution • Good surveillance is vital for successful control of communicable diseases. • Measure the causal factors of disease & identify high risk groups. • Monitor effectiveness, evaluate the impact of prevention & control measures, intervention strategies & health policy changes • Plan, provide care & various interventions • Evaluate various hypotheses about disease occurrence • Help to identify epidemic outbreaks in order to investigate & control them • The facility-based health information system should be augmented with a community based surveillance that uses volunteers & Community health workers/health information teams to gather essential data through home visits & other means. In addition to estimating the magnitude of an epidemic & monitoring its trends, data can also be used to: • Strengthen commitment, • Mobilize communities, • Advocate for sufficient resources. Health Indicators • These are quantifiable characteristics of a population used by researchers as supporting evidence for describing the health of a population. Typically, researchers will use a survey methodology to gather information about certain people, use statistics in an attempt to generalize the information collected to the entire population, then use the statistical analysis to make a statement about the health of the population. • Health indicators are often used by governments to guide health care policy. Some of the basic health indicators are: – Crude Birth Rate, – Crude Death Rate, – Infant Mortality Rate, – Morbidity Rate, – Perinatal Mortality Rate, – Neonatal Mortality Rate, – Maternal Mortality Rate, – Incidence Rate, – Prevalence Rate, – Life Expectancy, – General Fertility Rate.