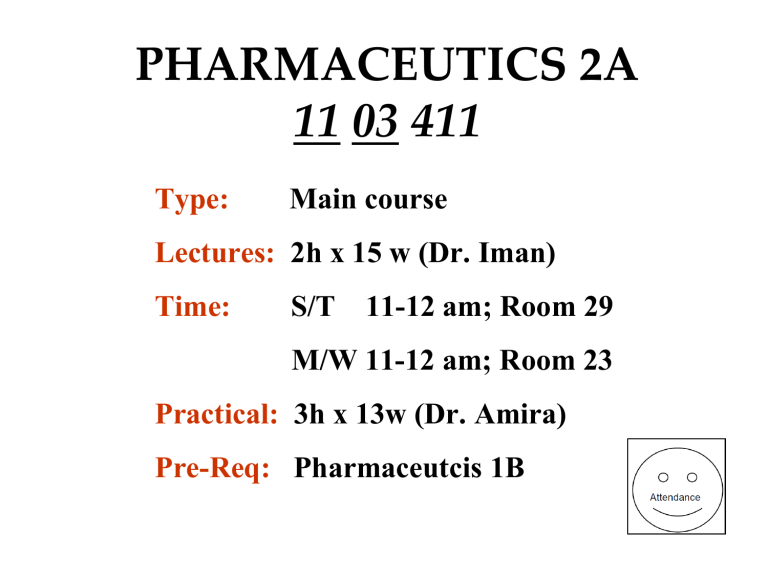
PHARMACEUTICS 2A 11 03 411 Type: Main course Lectures: 2h x 15 w (Dr. Iman) Time: S/T 11-12 am; Room 29 M/W 11-12 am; Room 23 Practical: 3h x 13w (Dr. Amira) Pre-Req: Pharmaceutcis 1B Reference Textbook Leon Shargel, Andrew B.C. Yu, Applied biopharmaceutics & pharmacokinetics, Seventh edition, McGraw-Hill Education, Inc. 2016. Where does Pharmaceutics 2A stand in the pharmacy program? Teaching/Learning Tools • • • • • Lecture-based instruction, Lab experiments Group assignments Problem solving Active learning PK and PD PK is the study of what the body does to a drug PD is the study of what a drug does to the body Question 1 Which of the following is a PK response? A. The change of sugar concentration in the blood B. The change of tetracycline concentration in the blood C. The change of insulin concentration in the blood D. All of the above E. B & C Readings Leon Shargel, Andrew B.C. Yu, Applied biopharmaceutics & pharmacokinetics, Seventh edition, McGraw-Hill Education, Inc. 2016. pp: 1-6. DRUG THERAPY Duration of Drug Therapy: Single Dose: such as to relieve a headache For the Rest of the Patient’s Life: such as in chronic diseases (epilepsy, diabetes) DOSAGE REGIMEN The manner in which a drug is taken is called a Dosage Regimen Duration of Drug Therapy and Dosage regimen will depend on the therapeutic objective. Objectives of taking a drug are : Cure, Mitigation, Prevention SUCCESSFUL DRUG THERAPY By optimally balancing the desirable and undesirable effects Accurate diagnosis is made Drug of choice Knowledge of clinical state of patient Understanding the pharmaco-therapeutic management of the disease Answer the questions How much? How often? and How long? Answers to Questions?????? How much? Recognizes that the magnitude of the therapeutic and toxic responses is a function of the dose given. How often? Recognizes the importance of time, in that the magnitude of the effect eventually declines with time following a single dose of drug. How long? Recognizes that a cost (in terms of side effects, toxicity, economics) is incurred with continuous drug administration. In the Past Questions were answered by trial and error, i.e. the dose, interval between doses, and route of administration were selected and the patient’s progress was followed. This empirical approach established many dosage regimens but left many questions unanswered!!!!!! This empirical approach did not contribute toward establishing a safe, effective dosage regimen of another drug, i.e. did not help us understand how drugs work? Empirically Derived Dosage Regimen DRUG Tetracycline INDICATED USE Treatment of infections ROUTE Oral Digoxin Amelioration of congestive cardiac failure Oral Oxytocin Induction and maintenance of labor Intravenous Morphine sulfate Relief of severe pain Intramuscular DOSAGE REGIMEN 250 mg every 6-8 hr 1.5-2 mg initially over 24hr, thereafter, 0.25-0.5 mg once a day 0.2-4 milliunits/min by infusion 10 mg when needed, not recommended orally Application of Pharmacokinetics • Rarely is a drug placed at its site of action, most drugs are given orally and yet they act in the brain, heart, or elsewhere!!!! • Which means a drug has to move from the site of administration to the site of action. • Therefore to administer drugs optimally, knowledge is needed not only of the mechanisms of drug absorption, distribution, and elimination but also the kinetics of these processes, that is PK Following Drug Administration 2 phases can be distinguished Pharmacokinetic Phase: in which the adjustable elements of dose, dosage form, frequency, and route of administration are related to drug level-time relationships in the body. Pharmacodynamic Phase: in which the conc of drug at the site of action(s) is related to the magnitude of the effect(s) produced. Advantages of PK and PD Knowing the PK and PD of drugs will: • Aid in designing a dosage regimen to achieve the therapeutic objective • Explain the manner of its use OPTIMIZE PATIENT DRUG THERAPY BY MONITORING PK&PD RESPONSES An Approach to the Design of a Dosage Regimen Pharmacokinetics Dosage Regimen Pharmacodynamics Plasma Concentration Site of Action Effects Where to measure Drug Concentration? • Rarely can the concentration of the drug at the site of action be measured directly; • Instead the concentration is measured at an alternative and more accessible site such as the plasma What is then an optimal dosage regimen? It is the one that maintains the plasma concentration of a drug within the therapeutic window and then maintaining this concentration by replacing the amount of drug lost with time. Initial and Maintenance Dose Plasma conc Regimen B 200 mg Drug Therapeutic Window Regimen A (100 mg Drug) Time Therapeutic Window (TW) • The size and frequency of the maintenance dose depends on the width of the therapeutic window and the speed of drug elimination. • When the window is narrow and the drug is eliminated rapidly, small doses must be given often to achieve therapeutic success. • Both cyclosporine and digoxin have a narrow TW, but because cyclosporine is eliminated much more rapidly than digoxin, it has to be given…?…?…?…? ( more frequently or less frequently????) Oxytocin • Oxytocin is an extreme example, it also has a • • narrow TW, but it is eliminated within minutes. The only means to ensure a therapeutic conc is to infuse it at a precise and constant rate directly into the blood (i.v. infusion). Oxytocin can not be given orally because it is destroyed in the GIT. Morphine can not also be given orally because it is extensively metabolized in the liver. PK in Clinical Trials • PK is incorporated in early Phase I studies, • usually in healthy volunteers together with assessment of any side effects produced to help choose candidate dosage forms and regimens for evaluation in Phase II studies conducted in a small number of patients (clinical PK). Phase II studies then help defining the most likely safe and efficacious dosage regimens for use in the subsequent larger Phase III trials often involving many thousands of patients. PROBLEM!!! Variability in Clinical Response Sources of variability: patient’s age, weight, degree of obesity, type and severity of disease, the patient’s genetic makeup, others drugs concurrently administered and environmental factors. Result: A standard dosage regimen of a drug may prove therapeutic in some patients, ineffective in others and toxic is still others. Dosage Regimen Adjustment The need is greatest for drugs with narrow TW: • Digoxin used to treat cardiac disorders. • Phenytoin used to prevent epileptic convulsions • Theophylline used to diminish chronic airway resistance in athmatics. • Cyclosporine used as immunosuppressant in organ transplantation. • Warfarin used as oral anti-coagulant. Drug-Drug Interaction Interactions that result in a change in PK of a drug could be due to: • Stimulation of drug metabolizing enzymes therefore increasing drug loss. • Inhibition of drug metabolizing enzymes therefore slowing drug elimination and increasing its concentration in the blood. • Interference with drug absorption. SOLUTION • A pragmatic approach to this problem would be to adjust the dosage until the desired objective is achieved. • Control on a dosage basis alone, however, has proved difficult. • Control is achieved more readily and accurately when plasma drug conc data and the PK of the drug are known. DRUG IS A VERY COMPLEX SYSTEM WHAT WE WILL DO IN THIS CLASS? • Although the details of drug kinetics are complicated, it is fortunate that we can often approximate drug kinetic processes using “SIMPLE MATHEMATICAL MODELS”. • The use of PK equations, rather than the derivation of the equations will be taught in this class.