Beneficial Effects of a High Protein Low Glycemic Load Hypocaloric Diet in Overweight and Obese Women with Polycystic Ovary Syndrome A Randomized
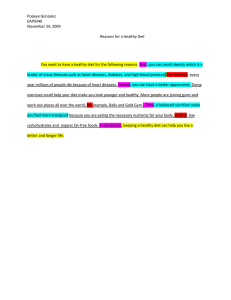
advertisement

Journal of the American College of Nutrition ISSN: 0731-5724 (Print) 1541-1087 (Online) Journal homepage: https://www.tandfonline.com/loi/uacn20 Beneficial Effects of a High-Protein, Low-GlycemicLoad Hypocaloric Diet in Overweight and Obese Women with Polycystic Ovary Syndrome: A Randomized Controlled Intervention Study Homeira Hamayeli Mehrabani, Saghar Salehpour, Zohreh Amiri, Sara Jalali Farahani, Barbara J Meyer & Farideh Tahbaz To cite this article: Homeira Hamayeli Mehrabani, Saghar Salehpour, Zohreh Amiri, Sara Jalali Farahani, Barbara J Meyer & Farideh Tahbaz (2012) Beneficial Effects of a High-Protein, Low-Glycemic-Load Hypocaloric Diet in Overweight and Obese Women with Polycystic Ovary Syndrome: A Randomized Controlled Intervention Study, Journal of the American College of Nutrition, 31:2, 117-125, DOI: 10.1080/07315724.2012.10720017 To link to this article: https://doi.org/10.1080/07315724.2012.10720017 Published online: 06 Jun 2013. Submit your article to this journal Article views: 603 Citing articles: 39 View citing articles Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=uacn20 Original Research Beneficial Effects of a High-Protein, Low-Glycemic-Load Hypocaloric Diet in Overweight and Obese Women with Polycystic Ovary Syndrome: A Randomized Controlled Intervention Study Homeira Hamayeli Mehrabani, PhD, Saghar Salehpour, MD, Zohreh Amiri, PhD, Sara Jalali Farahani, BS, Barbara J. Meyer, PhD, Farideh Tahbaz, PhD Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute (H.H.M., Z.A., F.T.), Faculty of Medicine (S.S.), Endocrine Research Center (S.J.F.), Shahid Beheshti University of Medical Sciences, Tehran, IRAN, School of Health Sciences (B.J.M.), University of Wollongong, Wollongong, New South Wales, AUSTRALIA Key words: PCOS, hypocaloric diet, hormones, inflammatory factors, blood lipids, glycemic load, dietary protein Objective: The recommended composition of a hypocaloric diet for obese women with polycystic ovary syndrome (PCOS) is unclear. The aim of this study was to investigate the effects of a high-protein, low-glycemicload diet compared with a conventional hypocaloric diet on reproductive hormones, inflammatory markers, lipids, glucose, and insulin levels in obese women with PCOS. Methods: A total of 60 overweight and obese women with PCOS who did not use insulin-sensitizing agents were recruited and randomly assigned to 1 of the 2 hypocaloric diet groups for a single-blind clinical trial. The groups included a conventional hypocaloric diet (CHCD) (15% of daily energy from protein) and a modified hypocaloric diet (MHCD) with a high-protein, low-glycemic load (30% of daily energy from protein plus lowglycemic-load foods selected from a list) that was prescribed via counseling visits weekly during 12 weeks of study. Anthropometric assessments and biochemical measurements including reproductive hormones, inflammatory factors, lipids, glucose, and insulin were performed on fasting blood samples at baseline and after 12 weeks of dietary intervention. Results: Weight loss was significant and similar in the 2 groups. Mean of testosterone in the MHCD and CHCD groups decreased from 1.78 6 0.32 to 1.31 6 0.26 ng/ml and from 1.51 6 0.12 to 1.15 6 0.11 ng/ml, respectively (p , 0.001). Follicle sensitizing hormone (FSH), luteinizing hormone (LH), and blood lipids concentrations were not changed except low-density lipoprotein cholesterol (LDL-C) was reduced by 24.5% 6 12.3% (p , 0.001 for both) after 12 weeks of intervention. MHCD resulted in a significant reduction in insulin level, homeostatic model assessment for insulin resistance (HOMA), and high-sensitivity C- reactive protein (hsCRP) concentration (p , 0.001). Conclusions: In this study both hypocaloric diets significantly led to reduced body weight and androgen levels in these two groups of women with PCOS. The combination of high-protein and low-glycemic-load foods in a modified diet caused a significant increase in insulin sensitivity and a decrease in hsCRP level when compared with a conventional diet. generally thought to affect approximately 1 out of 16 women INTRODUCTION [2]. The majority of these women are obese [2]. Obesity can exacerbate the metabolic and reproductive abnormalities that Polycystic ovary syndrome (PCOS) was first described more than 70 years ago [1]. It is a hormonal imbalance that is are associated with the disorder, mostly by increasing insulin Address reprint requests to: Farideh Tahbaz, PhD, Associate Professor, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, PO Box 19395/4741, Tehran, IRAN. E-mail: farideh.tahbaz@gmail.com Source of funding: National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Conflict of interest: There are no conflicts of interest between the authors and the source of funding. All coauthors accept responsibility for content of the manuscript. Journal of the American College of Nutrition, Vol. 31, No. 2, 117–125 (2012) Published by the American College of Nutrition 117 Effects of High-Protein, Low-GL Diet on PCOS Women resistance and hyperinsulinemia, so weight loss accompanied by an increase in insulin sensitivity was highly recommended for this population group [3]. The ideal hypocaloric diet should decrease body mass, improve cardiovascular risk factors, and decrease fat tissue while sparing lean tissue. Low-carbohydrate diets were traditionally thought to aid weight loss and improve metabolic and reproductive dysfunction [4]. An increasing interest in a high-protein/low-carbohydrate diet has been observed [5]. Stamets et al. [6] compared the short-term effect of a high-protein diet (30% protein and 40% carbohydrate) or a high-carbohydrate diet (15% protein and 55% carbohydrate) on weight loss in obese women with PCOS. Both groups lost body weight—approximately 3.6% (high-protein group) and 4.2% (high-carbohydrate group)—but there were no significant differences between the diets [6]. Douglas et al. [7] used eucaloric diets either with monounsaturated fatty acids (17% of energy) or low carbohydrate (43% of energy) relative to a standard diet (56% carbohydrate, 31% fat, and 16% protein) over 16 days, which resulted in lower fasting insulin and acute insulin response to glucose in a lowcarbohydrate diet compared with the standard and monounsaturated fatty acids diets, respectively. Moran et al. [8] studied high protein (30% of total calories) vs low protein (15% of total calories) plus exercise for 12 weeks followed by a 4-week weight maintenance in obese subjects with PCOS. Both groups lost approximately 7.7 kg of weight, and there was no effect of diet composition. Although a high-protein diet did not make any significant independent difference in comparison with other weight-loss diets, it seems that protein intake induces satiety and enhances a feeling of well-being and also self-esteem for obese women with PCOS who have tried to lose weight [9]. The concept of reducing glycemic index (GI) and glycemic load (GL) in the treatment of obese women with PCOS has received considerable interest. GI refers to a system for classifying the glycemic response of carbohydrate and measures the relative area under the postprandial glucose curve of 50 g of digestible carbohydrates compared with 50 g of a standard food, either glucose or white bread. The GL, which developed later, is calculated by multiplying the GI by the amount of carbohydrates in each food [10]. In 2008 Herriot et al. [11] performed a retrospective audit on a group of women with PCOS who had been advised to follow a low-calorie, low-GL diet over a 2-year period. They found that this type of diet with 40%–45% of daily energy intake from carbohydrate, 30% from protein, and about 10% from saturated fat together with insulin-sensitizing medications caused weight loss and better weight maintenance in overweight and obese patients with PCOS [11]. However, the impacts of the prescribed diets, like many similar studies, were limited to subjects’ self-reporting, and there was a lack of thorough investigation about the final biochemical and anthropometric results. 118 Thus, the aim of this controlled intervention study was to investigate and compare the effects of two kinds of diets including a conventional hypocaloric diet (CHCD) and a modified hypocaloric diet (MHCD) with low-GL and highprotein content on reproductive hormones, lipid profile, inflammatory factors, glucose, and insulin levels in overweight and obese women with PCOS who had not started taking any medications or changed their exercise habits since the diagnosis of their disease. MATERIALS AND METHODS A total of 60 women were recruited through newspaper advertisement, brochures, and referral of a gynecologist in outpatient nutrition clinic visits in the Taleghani infertility research center in Tehran, Iran. Subjects were included if they were aged between 20 and 40 years, had a body mass index (BMI) greater than 25 and less than 38 kg/m2, and no history of using an insulin-sensitizing agent such as metformin or oral contraceptives. Inclusion criteria were diagnosis of PCOS by menstrual irregularity (cycle length, ,21 days or .35 days), hirsutism, and biochemical hyperandrogenism. Volunteers were excluded if they were smokers, exercised heavily, and/or had any history of cardiovascular, renal, gastrointestinal disorders, liver or metabolic diseases. Women diagnosed with hyperprolactinemia, thyroid abnormalities, and/or nonclassic adrenal hyperplasia were also excluded from this study. The study protocol was approved by the ethics committee of the Institute of Nutrition Sciences and Food Technology of Iran, and all participants accepted the conditions of the study and gave their informed written consent. Study Design It was calculated that 23 subjects per group would provide 80% power to detect a difference of 7.7 nmol/L in the sex hormone-binding globulin (SHBG) levels in serum. Therefore 30 subjects were recruited for each group to cover the assumed withdrawal. Subjects were stratified to ensure equality of distribution in 2 groups for known confounding factors like age and BMI and then were randomized by an independent observer. The investigator was not blinded as to the kind of dietary intervention, but subjects were. Dietary intervention for the 2 groups were the CHCD and the MHCD each for 12 weeks. A dietitian initially instructed the subjects on quantification and recording of their daily food intakes. They were followed weekly and asked to prepare dietary records for 3 days every month during the intervention (weeks 0, 4, 8, and 12) to enhance compliance and to enable the dietitian to monitor the prescribed diet. Subjects were requested not to change their regular physical activities during the study period. In order to check that, they were asked to VOL. 31, NO. 2 Effects of High-Protein, Low-GL Diet on PCOS Women record all their daily physical activity and resting hours at the beginning and during the intervention. Description of the Diets For both groups energy content of the hypocaloric diet was calculated on the basis of subjects’ BMI of 21–22 kg/m2 and a deficit of 500-1000 kcal (2090–4180 kJ) per day. CHCD consisted of 55% of energy from carbohydrate, 15% of energy from protein, and 30% of energy from fat. MHCD included 40% of energy from low-and medium-GL carbohydrates, 30% of energy from protein, and 30% of energy from fat, with limitation of high-glycemic foods. The MHCD group refrained from consuming high-GL foods (GL 20). These foods in addition to the GL of the other foods were provided to them in a list [12]. In order to assist the subjects in meal planning some menu items including poultry, fish, legumes, egg white, fruits, and nonstarchy vegetables, which were similar to their regular dietary habits, were suggested by the researcher. In these meals the contents of macronutrients were close to the goals of the intervention. Furthermore, the subjects were instructed about exchanging food items, and to ensure their diet compliance they were followed by weekly counseling visits. Both groups of patients were precisely instructed about the foods they were or were not permitted to consume. Their eating habits were assessed using a food-frequency questionnaire [13]. Anthropometric Assessments All the anthropometric measurements were assessed in the fasting state. Body composition including total body fat and lean body mass were measured at the beginning and the end of the intervention using bioelectrical impedance (BioStat Co, 1500, UK). Skinfold thickness was measured at the suprailiac area using a skinfold caliper (Vogel, Germany) in order to determine abdominal fatness. Waist circumference was measured with a nonstretchable tape at the area demarcated by the umbilicus and hip circumference at the widest place over the buttocks. Subjects wore light clothes without shoes when they were weighed (Seca weighing scale, Model 709, Seca GmbH & Co KG, Germany) and their height was measured without shoes. Biochemical Measurements After an overnight fast, 10-ml blood samples were taken. The test was performed either at random in the amenorrheic women or 2–5 days after menstruation. Follicle stimulating hormone (FSH), luteinizing hormone (LH), and SHBG were measured by the immunoenzymometric assay method, and estradiol, total testosterone, dehydroepiandrosterone sulfate (DHEAS), and androstenedione were determined by enzyme immunoassay using a commercially available kit in a serum JOURNAL OF THE AMERICAN COLLEGE OF NUTRITION (Diagnostics Biochem Canada Inc, ON, Canada) [14]. The coefficients of variance (CVs) for these assays were as follows: 2.1% for FSH, 4.1% for LH, 3.1% for SHBG, 6.2% for DHEAS, 5% for total testosterone, and 5.2% for androstenedione. Fasting insulin and adiponectin were measured using an enzyme linked immunosorbent assay (ELISA; Mercodia, Uppsala, Sweden), and CVs were 7% and 5.1%, respectively. Serum glucose, triglyceride, total cholesterol, and high-density lipoprotein cholesterol (HDL-C) were measured by a colorimetric enzymatic assay, and the CV was lower than 2.5%. The Friedewald equation was used for low-density lipoprotein cholesterol (LDL-C) estimation [15]. Interleukin-6 (IL-6), tumor necrosis factor alpha (TNFa) were measured using ELISA (Diaclone, Besançon, France), and their CVs were 5.8% and 7.9%, respectively. High-sensitivity C-reactive protein (hsCRP) was measured by ELISA (DBC, ON, Canada) with CV 9.8%. The homeostatic model assessment for insulin resistance (HOMA) was used as a surrogate measure of insulin sensitivity and was calculated as fasting serum insulin (mU/L) 3 fasting serum glucose (mmol/L) / 22.5 [16]. The free androgen index (FAI) was calculated using the formula FAI ¼ T / SHBG 3 100 [17]. Statistical Analyses Data were analyzed using the Statistics Package for the Social Sciences 15 (SPSS Inc, Chicago, IL). Baseline parametric and nonparametric characteristics of subjects in the 2 groups and also the differences between the 2 groups (week 12 minus baseline) were compared by t test and Mann-Whitney test. Paired t tests were performed to evaluate the possible differences between baseline and week 12 for each group, separately. A p value of ,0.05 was considered significant. The results were analyzed in two ways. Firstly a paired t test was used to compare baseline and week 12 data. Second, the data of week 12 minus baseline were compared between the 2 groups. RESULTS In total, 49 out of 60 subjects completed the study: 26 in CHCD and 23 in MHCD. Three had difficulty with bloodsample draws, 2 could not tolerate any diet, 1 changed her mind and wanted to begin in vitro fertilization processing, 2 had family reasons, 1 moved out of the city without any forwarding address, and 2 did not provide any reason. No significant differences existed in subjects’ characteristics at baseline for the 2 treatment groups, except for hip circumference (Table 1). Both the MHCD and CHCD diets resulted in significant weight loss (p , 0.05). None of the subjects had weight gain during the study. The range in weight loss was 2 to 10 kg for MHCD and 1 to 9 kg for the 119 Effects of High-Protein, Low-GL Diet on PCOS Women Table 1. Baseline Measurements of the 2 Study Groups1 CHCD (n ¼ 26) Age (y) Weight (kg) BMI (kg/m2) Waist circumference (cm) Hip circumference (cm) Suprailiac skinfold (mm) Total fat mass (%) Total lean body mass (%) 28.5 78.9 31.1 102.3 112.1 40.0 39.9 59.9 6 6 6 6 6 6 6 6 5.2 12.4 4.6 9.9 11.3 9.4 7.1 7.2 MHCD (n ¼ 23) 30.5 83.0 31.9 108.2 120.2 44.1 40.4 58.8 6 6 6 6 6 6 6 6 6.4 11.7 4.0 8.1 17.1* 15.7 7.5 7.4 CHCD ¼ conventional hypocaloric diet, MHCD ¼ modified hypocaloric diet. 1 Values are means 6 SD. There were no baseline differences between the subjects in the 2 groups except for hip circumference (p , 0.05). CHCD group. It was estimated as 4.1% 6 0.58% and 3.3% 6 0.62% weight loss for MHCD and CHCD, respectively, in regard to initial weight, without any significant differences. Subjects in both groups did not change their physical activity during the study. Although there were not any significant changes in total body fat and lean body mass based on BIA (body impedance analysis) after 12 weeks of manipulation of the weight reduction diet, but in both groups fat mass was reduced at the end of the intervention (Fig. 1). The reduction of waist circumference in MHCD was significantly more than CHCD (p , 0.05). Dietary intakes at baseline and after intervention are shown in Table 2. There were no significant differences in dietary intakes of the 2 groups (zero time). During intervention, daily energy intakes decreased with no significant difference between the 2. As expected, protein as a percentage of energy intake was higher and carbohydrate was lower in MHCD, and these differed significantly in comparison with CHCD. Contribution of fat in total energy intake decreased in both groups. Carbohydrate and total fat intakes were decreased for MHCD and replaced by protein. Fiber intake increased by approximately 20% in the MHCD group (p , 0.05) but no difference was observed in fiber intake in the CHCD group. There was not any significant difference between the changes of fiber intake in the 2 groups at week 12 (0.3 6 1.4 g for CHCD vs 2.8 6 1.4 g for MHCD). There was no effect of energy reduction or diet composition on FSH, LH, and blood lipids except for LDL-C, which decreased significantly in both groups (Table 3). Reduction of LDL-C levels were 23.7% 6 13.8% for CHCD and 25.5% 6 10.5% for MHCD without any significant differences between the 2 groups. Mean 6 standard error (SE) of fasting glucose for CHCD vs MHCD, respectively, at baseline was 96.0 6 1.5 vs 97.4 6 1.4 mg/dl (p ¼ 0.49) and at week 12 was 98.3 6 1.7 vs 98.5 6 2.5 mg/dl (p ¼ 0.95). SHBG increased and testosterone and DHEAS decreased in both groups (Table 3). There were no significant differences between the 2 groups in regard to the changes of reproductive hormones (Table 3). In addition there were substantial decreases in fasting insulin level and HOMA after 12 weeks for both kinds of 120 Fig. 1. Percentage of anthropometric changes for women with PCOS after 12 weeks allocated to MHCD or CHCD. CHCD ¼ conventional hypocaloric diet, MHCD ¼ modified hypocaloric diet, WC ¼ waist circumference, HC ¼ hip circumference, SST ¼ suprailiac skinfold thickness, TBFM ¼ total body fat mass. All the anthropometric changes were significant for both groups, CHCD and MHCD (p , 0.05), except for TBFM. *p , 0.05 MHCD in comparison with CHCD. interventional diets: 25.3% and 23.2%, respectively, for MHCD (p , 0.001) vs 5.9% and 4.2% for CHCD (p , 0.001). However, this only remained significant after adjusting for BMI changes in MHCD and was found to be related directly to the type of diet. TNFa decreased and adiponectin increased significantly in both groups (Table 4), IL-6 did not change, and hsCRP decreased in MHCD, which was significant after adjusting for baseline hsCRP. DISCUSSION This study demonstrates that both kinds of hypocaloric diets with no medications and instructed physical exercise resulted in a significant weight loss, lowering of LDL-C, reduction of androgens, and an increase in SHBG, but consumption of the MHCD (a hypocaloric diet with low-GL carbohydrates and high-protein content) induced concomitant reductions of insulin and HOMA and, therefore, would be viewed as more favorable than the CHCD. The attrition rate in this study was about 20%, which was much lower than this rate in a recent clinical study investigating the effects of a low-GI diet on women with PCOS [18]. Perhaps prescribing the diets according to the patients’ regular dietary habits and without any medications might be a factor in this higher adherence of patients to their diets in this study. This is shown by these subjects who achieved the macronutrient goals that were set for them through their diets. Effects of Hypocaloric Diets on Weight Loss Even though the benefit of weight loss for women with PCOS is clear, the ideal diet composition for their management is not known. There is a paucity in the study of reduced-GL VOL. 31, NO. 2 Effects of High-Protein, Low-GL Diet on PCOS Women Table 2. Calculated Dietary Composition of MHCD and CHCD from 4 3 3 Days Food Record in Comparison with Baseline Dietary Intakes1 CHCD (n ¼ 26) Prescribed Diet Energy(kJ/d) (Kcal/d) Carbohydrate (% E) Fat (% E) Protein (% E) 5021–7113 1200–1700 55 30 15 Baseline 9117 2179 57.1 31.7 11.2 6 6 6 6 6 515 123 1.7 2.0 0.5 MHCD (n ¼ 23) Recalls p Value Prescribed Diet 6 6 6 6 6 0.000 5021–7113 1200–1700 40 30 30 6832 1633 55.2 30.2 14.6 414 99 4.9 4.6 2.3 0.125 0.362 0.000 Baseline 9472 2264 54.7 33.7 11.6 6 6 6 6 6 473 113 1.5 1.6 2.5 Recalls p Value 6 6 6 6 6 0.000 6590 1575 41.4 29.1 29.5 280 67 2.7 2.4 2.5 0.000 0.016 0.000 CHCD ¼ conventional hypocaloric diet, MHCD ¼ modified hypocaloric diet, % E ¼ percentage of total daily energy intake. 1 Values are means 6 SE. * p value for changes; Recalls Baseline. low-protein diets for the same duration was much higher than in this current study. It can be assumed that weekly exercise and the education class in their study were the key contributing factors for similar and higher degrees of weight loss in both groups. Few studies have addressed the effects of varying diet composition on the obese PCOS population; a hypocaloric diet supplemented with protein reduced fat mass and body weight more than diet supplemented with simple sugars [19]. It seems that the subjects receiving higher protein may have more successful weight loss due to the satiating effect of the diet [9,20], but there were no significant differences in hormonal changes attributed to the composition of the diet [6]. diets for obese PCOS women. In a retrospective study of normal-weight and obese women with PCOS by Herriot et al. [11], weight and fasting glucose were significantly reduced without changes in insulin concentrations for 13 patients by a low-GL-load diet: low-GL foods, reduced carbohydrate of approximately 40%–45% energy, 30% protein, reduced saturated fat of approximately 10%, and no snacking. The audit indicated that a low-GL diet may contribute to an improvement in symptom relief in patients with PCOS, such as carbohydrate craving and hypoglycemia [11]. In this study weight loss was similar in the 2 groups, and MHCD did not have any superior effect on weight loss compared with CHCD. But MHCD resulted in a higher decrease of waist and hip circumferences that might be due to the lower GL of carbohydrates or higher protein intakes, although at baseline the hip circumferences in MHCD had a significant difference with CHCD and could explain significant differences at week 12 between MHCD and CHCD. In the other studies the weight reduction was not different for highprotein (30%) and low-protein (15%) diets [8,9]. In the study performed by Moran et al. [8] weight loss on high-protein and Effects of Hypocaloric Diets on Reproductive Hormones and Insulin Levels The improvement of the abnormal reproductive hormones in this current study were consistent with some studies that had observed the effect of weight loss in improving abnormal reproductive and metabolic variables in women with PCOS Table 3. Serum Concentrations of Lipids and Reproductive Hormones at Baseline and after Intervention1 CHCD (n ¼ 26) Baseline T (ng/ml) A4 (ng/dl) DHEAS (ng/ml) SHBG (nmol/L) FSH (IU/L) LH (IU/L) FAI Triglyceride (mg/dl) Cholesterol (mg/dl) HDL-C (mg/dl) LDL-C (mg/dl) 1.5 1.9 330.1 26.9 5.2 2.9 6.6 132.9 197.1 62.4 158.5 6 6 6 6 6 6 6 6 6 6 6 0.2 0.1 30.6 3.8 0.6 0.4 0.7 7.8 5.3 1.6 6.9 MHCD (n ¼ 23) Week 12 1.1 1.8 298.1 37.6 4.5 2.3 4.2 124.4 191.6 61.3 120.0 6 6 6 6 6 6 6 6 6 6 6 change * 0.1 0.2 28.9** 4.6*** 0.5 0.4 0.5* 7.5 4.8 1.2 6.6* 0.4 0.1 32.0 10.6 0.7 0.6 2.4 8.6 5.5 1.1 38.5 6 6 6 6 6 6 6 6 6 6 6 0.04 0.1 8.9 4.1 0.5 0.4 0.5 5.4 3.2 0.8 4.9 Baseline 1.8 1.9 314.9 22.7 5.6 2.2 7.0 128.7 199.9 59.6 158.1 6 6 6 6 6 6 6 6 6 6 6 0.3 0.1 31.9 4.0 0.8 0.2 0.9 6.5 5.8 1.8 5.5 Week 12 1.3 1.8 272.8 31.4 4.9 2.6 5.1 122.4 191.5 59.2 116.7 6 6 6 6 6 6 6 6 6 6 6 Change ** 0.2 0.1 28.9** 4.4** 0.6 0.5 0.8** 5.7 5.5 1.6 4.3* 0.5 0.1 42.1 8.8 0.7 0.4 1.9 6.3 8.4 0.4 41.3 6 6 6 6 6 6 6 6 6 6 6 0.2 0.1 16.1 2.8 0.9 0.6 0.7 6.1 4.1 0.7 4.3 CHCD ¼ conventional hypocaloric diet, MHCD ¼ modified hypocaloric diet, T ¼ testosterone, A4 ¼ androstenedione, DHEAS ¼ dehydroepiandrosterone, SHBG ¼ sex hormone-binding globulin, FSH ¼ follicle stimulating hormone, LH ¼ luteinizing hormone, FAI ¼ free androgen index, HDL-C ¼ high-density lipoprotein cholesterol, LDL-C ¼ low-density lipoprotein cholesterol. 1 Data are mean 6 SE. * p , 0.001, ** p , 0.01, *** p , 0.05. JOURNAL OF THE AMERICAN COLLEGE OF NUTRITION 121 Effects of High-Protein, Low-GL Diet on PCOS Women Table 4. Serum Concentrations of Insulin and Inflammatory Factors at Baseline and after Intervention1 CHCD (n ¼ 26) Baseline Insulin (mU/ml) HOMA-IR TNFa (pg/ml) IL-6 (pg/ml) hsCRP (mg/L) Adiponectin (pg/ml) 12.2 2.9 6.3 1.1 2.7 59.6 6 6 6 6 6 6 6.0 1.6 0.9 0.06 0.6 4.4 Week 12 11.2 2.7 3.8 1.0 2.6 67.7 6 6 6 6 6 6 5.3 1.5 0.8** 0.06 0.6 4.6** MHCD (n ¼ 23) Change 1.0 0.3 2.5 0.1 0.1 8.1 6 6 6 6 6 6 0.7 0.2 1.1 0.07 0.2 3.9 Baseline 12.1 2.9 5.4 1.3 3.6 59.9 6 6 6 6 6 6 3.3 1.4 0.9 0.1 0.8 2.8 Week 12 8.4 2.0 3.3 1.3 2.7 68.6 6 6 6 6 6 6 Change * 3.6 0.8 2.1 0 0.9 8.7 3.7 0.9* 0.6** 0.3 0.6** 3.3* 6 6 6 6 6 6 0.7** 0.2** 0.8 0.2 0.4 2.0 CHCD ¼ conventional hypocaloric diet, MHCD ¼ modified hypocaloric diet. 1 Data are mean 6 SE. The difference between baseline and week 12 are shown in week 12 for each group. The difference between the changes of two groups are shown in the change of MHCD. * p , 0.001, ** p , 0.05. [6,8,18,21]. It is currently unclear why reproductive function is restored with energy restriction or weight loss, how long it would take for the hormonal changes to translate into improvements in reproductive functions, and what the key triggering hormonal factors are [21]. In this study it is hypothesized that a hypocaloric diet with increased protein content and reduced GL would decrease insulin concentration and this in turn results in lowering androgen concentrations. The levels of total testosterone and DHEAS decreased similarly in both groups after weight loss. In spite of significant decreases of insulin and HOMA in the MHCD group, there was no effect of reduced insulin on androgen levels. It seems that the changes in insulin concentration in this study were not enough to result in the reduction of androgens. Perhaps this was related to insulin resistance or lower insulin sensitivity in some of the studied subjects, but these were not measured directly. Similar to the current study, Moran et al. [8] found no significant effect of diet composition on testosterone or SHBG levels and showed that endocrine improvements caused maximal changes in insulin sensitivity, suggesting a relationship between the two. Decreases in the level of fasting insulin, increases in SHBG level, and decreases in testosterone were related to energy-restriction diets. It is possible that the family of insulinlike growth factors (IGFs) and their binding proteins may be involved [22]; in particular, IGF-binding protein-I increases during short-term energy restriction mediated by decreased insulin levels. Increased IGF-binding protein-I decreases free IGF-I, which down-regulates androgen synthesis through the cytochrome P450c17 system [23]. Free-testosterone concentrations are reported to decline significantly following weight loss and decrease of insulin concentration [24]. Previously Pasquali et al. [25] showed that moderate weight loss resulted in a reduction in insulin levels but did not alter androgen and DHEAS levels. There were no effects of weight loss or type of diet seen on LH and FSH. There were no changes of these hormones seen in other studies [8,26]. Guzick et al. [27] observed no effect of weight loss in obese hyperandrogenic women and suggested 122 that weight loss had no hypothalamic effect for secretion of LH. It is believed that LH concentration is not related to insulin concentration [27]. Moreover, this current study showed a significant effect of MHCD on insulin concentration and HOMA when compared with CHCD. This suggests that the lower GL in the MHCD group in combination with higher protein improved insulin resistance, given that low GL has been shown to improve insulin resistance [28,29]. In contrast, the Moran et al. study [8] showed improvements in insulin concentration and HOMA in both energy-restricted diets (high carbohydrate/low protein and high protein/low carbohydrate); however, in their study, both groups increased their exercise levels, and it has been shown that exercise improves insulin resistance in women with PCOS [30]. Taking these two studies together, one could speculate that to improve insulin levels and HOMA in women with PCOS, the women either go on an energy-restricted diet (irrespective of composition) so long as they also increase their exercise [8] or the women go on a MHCD diet without exercise as shown in this study. A limitation of the Moran et al. [8] study was the lack of an exercise-only arm, which would have definitively shown that exercise was responsible for the improvements in insulin levels and HOMA. Effects on Cardiovascular Risk Factors It has been proposed that excess fat accumulation alters the pattern of adipokines secretion, causing a low-grade inflammatory state that induces insulin resistance and endothelial dysfunction leading to diabetes and cardiovascular disease [31], and conversely, fat-mass loss or weight reduction induce decreases in cardiovascular risk factors. Some studies showed the relation between change of insulin resistance and decreases in these risk factors [32,33], but it has been assumed that the levels of blood lipids and inflammatory factor at baseline are important for observing a significant reduction. Noakes et al. [34] reported decrease of serum triacylglycerol after weight loss in obese women with high baseline triglycerides. Moran et al. [8] also showed reductions in VOL. 31, NO. 2 Effects of High-Protein, Low-GL Diet on PCOS Women plasma triacylglycerol after weight loss (due to energy restricted diets and increased exercise) on women with PCOS. In the current study there were no significant differences in plasma triacylglycerol, but this could be explained by the baseline plasma triacylglycerol levels being approximately 20% lower than those in the study by Moran et al. [8]. However, in the current study LDL-C decreased in both groups, and this could be due to its higher levels at the beginning of the study. Previously, dietary GL and carbohydrate has been associated with a number of cardiovascular risk factors, reduced HDL-C, and elevated triacylglycerol concentrations and also hsCRP level [35,36]. There are limited trials for inflammatory factors in obese women with PCOS after weight loss by hypocaloric diet. CRP was reduced significantly after consumption of an energyrestricted diet for 8 weeks [21]. But in comparison between women with and without PCOS, there was a significant interaction between PCOS status and CRP such that CRP did not decrease with about 4% weight loss in women with PCOS, and TNFa increased after weight loss, which was surprising because usually inflammatory factors decrease after weight loss. Esposito et al. [37] reported reduction of inflammatory factors by using a hypocaloric Mediterranean-style diet and regular physical activity in obese women. In the current study TNFa decreased for both groups, and IL-6 did not change and hsCRP decreased only in MHCD. In addition the decrease in waist circumference was higher in MHCD than in CHCD, so reduction of CRP may be related to this variable. Linear regression analysis revealed hsCRP baseline and waist difference parameter and individual variability has been suggested to have an important influence on the results [38]. The decrease in hsCRP concentration after weight reduction does not appear to be mediated by a decrease in circulating IL6 or adiponectin concentrations [39]. Adiponectin increased in both groups after weight loss, which had been observed in other studies [37], but it seems that the change in adiponectin level after weight loss did not happen regularly in obese women with PCOS [38,40]. It has been suggested to study the ratio of high-molecular-weight adiponectin to low-molecularweight adiponectin due to the varying appearance of the two adiponectin oligomers on fat and glucose metabolism [41]. In conclusion, the current study demonstrated that 2 kinds of low-calorie diets in women with PCOS who had not started taking any medications and without any prescribed exercise have significant effects on testosterone, androstenedione, dehydroepiandrosterone, SHBG, FAI, LDL-C, adiponectin, TNFa, and to our knowledge, this is the first interventional study to suggest that high-protein plus a low-GL hypocaloric diet without exercise has additional effects on lowering insulin level and HOMA. However, the limitation of this study was that it was a selfreported study in which the researchers relied on the study participants to follow their prescribed diets, and hence JOURNAL OF THE AMERICAN COLLEGE OF NUTRITION controlled-feeding programs for future studies is recommended. Recommendations for future studies include considering abdominal fat in addition to BMI as an inclusion criterion because it would ensure the subjects were metabolically much more similar. It is also recommended to follow up patients for another 6 months to see weight maintenance and the consequences of weight reduction on the reproduction of these groups of women. CONCLUSION Both hypocaloric diets without using any medications and instructed exercise were shown to significantly reduce body weight and androgen levels in 2 groups of women with PCOS. In addition, a high-protein, low-GL diet caused a significant increase in insulin sensitivity and a decrease in hsCRP level when compared with a conventional diet. However, a study to differentiate the effects of protein content and glycemic load in a hypocaloric diet for women with PCOS is needed. REFERENCES 1. Stein IF, Leventhal ML: Amenorrhoea associated with bilateral polycystic ovaries. Am J Obstet Gynecol 29:181–191, 1935. 2. Duniaf A, Thomas A: Current concepts in the polycystic ovary syndrome. Annu Rev Med 52:401–419, 2001. 3. Wild RA, Painter PC, Coulson PB, Carruth KB, Ranney GB: Lipoprotein lipid concentrations and cardiovascular risk in women with polycystic ovary syndrome. J Clin Endocrinol Metab 61:946– 951, 1985. 4. Raatz SK, Torkelson CJ, Redmon JB, Reck KP, Kwong CA, Swanson JE, Liu C, Thomas W, Bantle JP: Reduced glycemic index and glycemic load diets don’t increase the effects of energy restriction on weight loss and insulin sensitivity in obese men and women. J Nutr 135: 2387–2391, 2005. 5. Meckling KA, Sherfey R: A randomized trial of hypocaloric highprotein diet, with and without exercise, on weight loss, fitness, and markers of the metabolic syndrome in overweight and obese women. Appl Physiol Nutr Metab 32:743–752, 2007. 6. Stamets K, Taylor DS, Kunselman A, Demers LM, Pelkman CL, Legro RS: A randomized trial of the effects of two types of shortterm hypocaloric diets on weight loss in women with polycystic ovary syndrome. Fertil Steril 81:630–637, 2004. 7. Douglas CC, Gower BA, Darnell BE, Ovalle F, Oster RA, Azziz R: Role of diet in the treatment of polycystic ovary syndrome. Fertil Steril 85:679–688, 2006. 8. Moran LJ, Noakes M, Clifton PM, Tomlinson CL, Galletly C, Norman RJ: Dietary composition in restoring reproductive and metabolic physiology in overweight women with polycystic ovary syndrome. J Clin Endocrinol Metab 88:812–819, 2003. 9. Galletly C, Moran L, Noakes M, Clifton P, Tomlinson L, Norman R: Psychological benefits of a high-protein, low-carbohydrate diet in obese women with polycystic ovary syndrome—a pilot study. Appetite 49:590–593, 2007. 123 Effects of High-Protein, Low-GL Diet on PCOS Women 10. Gallagher ML: The nutrients and their metabolism. In EscottStump S, Mahan LK (eds): ‘‘Krause’s Food and Nutrition Therapy,’’ 12th ed. Philadelphia: Saunders, p 50, 2008. 11. Herriot AM, Whitcroft S, Jeanes Y: An retrospective audit of patients with polycystic ovary syndrome: the effects of a reduced glycaemic load diet. J Hum Nutr Diet 21:337–345, 2008. 12. Foster-Powell K, Holt SH, Brand-Miller JC: International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr 76:5–56, 2002. 13. Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F: Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr 13:654–662, 2010. 14. Edwards R: ‘‘Immunoassays.’’ New York: John Wiley & Sons, 1996. 15. Friedewald WT, Levy RI, Fredrickson DS: Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499– 502, 1972. 16. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC: Homeostasis model assessment: insulin resistance and beta cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419, 1985. 17. Vermeulen A, Verdonck L, Kaufman JM: A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84:3666–3672, 1999. 18. Marsh KA, Steinbeck KS, Atkinson FS, Petocz P, Brand-Miller JC: Effect of a low glycemic index compared with a conventional healthy diet on polycystic ovary syndrome. Am J Clin Nutr 92:83– 92, 2010. 19. Kasim-Karakas SE, Almario RU, Cunningham W: Effects of protein versus simple sugar intake on weight loss in polycystic ovary syndrome. Fertil Steril 92:262–270, 2009. 20. Pasquali R, Gambineri A, Biscotti D, Vicennati V, Gagliardi L, Colitta D, Fiorini S, Cognigni GE, Filicori M, Morselli-Labate AM: Effect of long-term treatment with metformin added to hypocaloric diet on body composition, fat distribution, and androgen and insulin levels in abdominally obese women with and without the polycystic ovary syndrome. J Clin Endocrinol Metab 85:2767–2774, 2000. 21. Moran LJ, Noakes M, Clifton PM, Wittert GA, Williams G, Norman RJ: Short-term meal replacements followed by dietary macronutrient restriction enhance weight loss in polycystic ovary syndrome. Am J Clin Nutr 84:77–87, 2006. 22. Hamilton-Fairley D, Kiddy D, Anyaoku V, Koistinen R, Seppala M, Franks S: Response of sex hormone binding globulin and insulin-like growth factor binding protein-1 to an oral glucose tolerance test in obese women with polycystic ovary syndrome before and after calorie restriction. Clin Endocrinol (Oxf ) 39:363–367, 1993. 23. Poretsky L, Cataldo NA, Rosenwaks Z, Giudice LC: The insulinrelated ovarian regulatory system in health and disease. Endocr Rev 20:535–582, 1999. 24. Kiddy DS, Hamilton-Fairley D, Bush A, Short F, Anyaoku V, Reed MJ, Franks S: Improvement in endocrine and ovarian function during dietary treatment of obese women with polycystic ovary syndrome. Clin Endocrinol (Oxf ) 36:105–111, 1992. 25. Pasquali R, Antenucci D, Casimirri F, Venturoli S, Paradisi R, Fabbri R, Balestra V, Melchionda N, Barbara L: Clinical and 124 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. hormonal characteristics of obese amenorrheic hyperandrogenic women before and after weight loss. J Clin Endocrinol Metab 68:173–179, 1989. Fulghesu AM, Cucinelli F, Pavone V, Murgia F, Guido M, Caruso A, Mancuso S, Lanzone A: Changes in luteinizing hormone and insulin secretion in polycystic ovarian syndrome. Hum Reprod 14:611–617, 1999. Guzick DS, Wing R, Smith D, Berga SL, Winters SJ: Endocrine consequences of weight loss in obese hyperandrogenic, anovulatory women. Fertil Steril 61:598–604, 1994. Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS: A reduced-glycemic load diet in the treatment of adolescent obesity. Arch Pediatr Adolesc Med 157:773–779, 2003. Kirwan JP, Barkoukis H, Brooks LM, Marchetti CM, Stetzer BP, Gonzalez F: Exercise training and dietary glycemic load may have synergistic effects on insulin resistance in older obese adults. Ann Nutr Metab 55:326–333, 2009. Hutchison SK, Stepto NK, Harrison CL, Moran LJ, Strauss BJ, Teede HJ: Effects of exercise on insulin resistance and body composition in overweight and obese women with and without polycystic ovary syndrome. J Clin Endocrinol Metab 96:E48–E56, 2011. Yudkin JS, Stehouwer CH, Emeis JJ, Coppack SW: C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 19:972–978, 1999. Florakis D, Diamanti–Kandarakis E, Katsikis I, Nassis GP, Karkanaki A, Georgopoulos N, Panidis D: Effect of hypocaloric diet plus sibutramine treatment on hormonal and metabolic features in overweight and obese women with polycystic ovary syndrome: a randomized, 24-week study. Int J Obes (Lond) 32:692–699, 2008. Bravata DM, Sanders L, Huang J, Krumholz HM, Olkin I, Gardner CD, Bravata DM: Efficacy and safety of low-carbohydrate diets: a systematic review. JAMA 289:1837–1850, 2003. Noakes M, Keogh JB, Foster PR, Clifton PM: Effect of an energyrestricted, high-protein, low-fat diet relative to a conventional highcarbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr 81:1298–1306, 2005. Liu S, Manson JE, Stampfer MJ, Holmes MD, Hu FB, Hankinson SE, Willett WC: Dietary glycemic load assessed by food-frequency questionnaire in relation to plasma high-density lipoprotein cholesterol and fasting plasma triacylglycerols in postmenopausal women. Am J Clin Nutr 73:560–566, 2001. Liu S, Manson JE, Buring JE, Stampfer MJ, Willett WC, Ridker PM: Relation between a diet with a high glycemic load and plasma concentrations of high-sensitivity C-reactive protein in middleaged women. Am J Clin Nutr 75:492–498, 2002. Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D: Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA 289:1799–1804, 2003. Moran LJ, Noakes M, Clifton PM, Wittert GA, Belobrajdic DP, Norman RJ: C-reactive protein before and after weight loss in overweight women with and without polycystic ovary syndrome. J Clin Endocrinol Metab 92:2944–2951, 2007. VOL. 31, NO. 2 Effects of High-Protein, Low-GL Diet on PCOS Women 39. Dvorakova-Lorenzova A, Suchanek P, Havel PJ, Stavek P, Karasova L, Valenta Z, Tintera J, Poledne R: The decrease in Creactive protein concentration after diet and physical activity induced weight reduction is associated with changes in plasma lipids, but not interleukin-6 or adiponectin. Metabolism 55:359– 365, 2006. 40. Kasim-Karakas SE, Almario RU, Gregory L, Wong R, Todd H, Lasley BL: Metabolic and endocrine effects of a polyunsaturated fatty acid-rich diet in polycystic ovary syndrome. J Clin Endocrinol Metab 89:615–620, 2004. JOURNAL OF THE AMERICAN COLLEGE OF NUTRITION 41. Bobbert T, Rochlitz H, Wegewitz U, Akpulat S, Mai K, Weickert MO, Mohlig M, Pfeiffer AF, Spranger J: Changes of adiponectin oligomer composition by moderate weight reduction. Diabetes 54:2712–2719, 2005. Received October 30, 2010; revision accepted December 14, 2011. 125