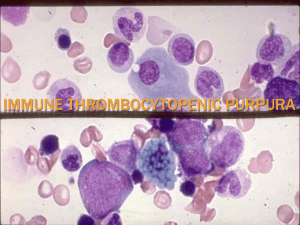
Immune (idiopathic) Thrombocytopenic Purpura Austin Rutledge, PGY2 Morning Report 7/30/19 Epidemiology The most common cause of acute onset of thrombocytopenia (usually <20K) in an otherwise healthy child A recent history of viral illness is described in 50-60% of cases of childhood ITP Typically 1-4 weeks after exposure Peak age 2-6y Slightly increased risk of developing ITP within 6 weeks of MMR vaccine (2.6 per 100,000 doses) Pathogenisis Autoantibody directed against platelet surface (glycoprotein complex IIb/IIIa) After binding, circulating antibody-coated platelets are destroyed by splenic macrophages In chronic ITP, T cell mediated cytotoxicity may cause platelet destruction Diagnosis ITP is a clinical diagnosis and diagnosis of exclusion PLT <100K Otherwise normal CBC including WBC, Hgb, reticulocyte counts No abnormalities on peripheral smear (no evidence of hemolysis or blasts) Negative DAT No findings on history or PE to suggest alternative dx (systemic symptoms, palpable lymph nodes, splenomegaly) Hemoglobin, WBC, and differential should all be normal Consider bone marrow aspiration if abnormal A DAT (Coombs) should be performed if unexplained anemia to rule out Evans syndrome (autoimmune hemolytic anemia w/ thrombocytopenia) before giving anti-D Diagnosis:2 criteria 1.Isolated thrombocytopenia,with otherwise normal blood counts and peripheral smear. 2.No clinically apparent associated conditions that may cause thrombocytopenia Exclude concurrent inf/autoimmune disorders/malignancy/drugs/genetic bleeding disorders/ marrow failure Differential Diagnosis Viral infection(IMN,Hepatitis,HIV- 1) Drug exposure(Heparin, Quinidine, Sulfonamide) Autoimmune Disorders(SLE) Leukemia (ALL) Acquired marrow failure syndrome (aplastic anemia) Inherited thrombocytopenic disorders(thrombocytopenia-absent radius syndrome, Wiskott-Aldrich syndrome,mutation of MYH 9 gene) Clinical Presentation Sudden appearance of bruising and/or bleeding in an otherwise healthy child Mild if bruising and petechiae Moderate if presence of mucosal lesions Severe if significant bleeding episodes (i.e. menorrhagia, epistaxis, melena In one large cohort study, mucosal bleeding was more common with PLT count <10K compared with >15K (51% vs 19%) Approximately 80% will have PLT <20K at presentation, and 45% will have PLT <10K History: No systemic symptoms Presence of systemic symptoms like fever ,anorexia, joint pain, bone pain or weight loss usually points to other diagnosis Drug induced (heparin, quinidine, sulfonamides) thrombocytopenia is uncommon in kids Disease course: 70% of children have the acute form of ITP, which is defined by recovery (platelet count >150,000/ micro L) in 6 months of presentation with or without treatment. Treatment do not affect the long term outcome,but minimize the risk of significant bleeding Treatment Ideal management still unclear: observation alone vs observation with pharmacologic intervention Initial approach includes no therapy other than education and counseling with minimal, mild, or moderate symptoms Restrict contact sports/physical activity Avoid medications with antiplatelet or anticoagulant activities Platelet transfusion is usually contraindicated unless there is life-threatening bleeding due to binding of antiplatelet antibodies to transfused platelets Presence of severe life threatening bleeding, risk of significant bleeding (planned procedures/count <10K, and cutaneous bleeding), comorbid conditions (hemophilia) requires intervention IV IG: Mechanism of action is multi-factorial,inhibition of antibody adsorption to platelets,prevention of RES uptake of auto ab coated platelets, interaction of auto abs with idiotype abs in IV IG. Works better than steroids but higher cost Dose: 400mg /kg/day x 5 days OR Single dose of 1g/kg IVIG induces rapid rise in platelet count in 95% of patients within 48hrs IVIG appears to induce a response by downregulating Fc-mediated phagocytosis of antibody-coated platelets IV IG – 500 mg /kg/day x 2 days ,and may be repeated if the symptoms recur Corticosteroids: DO NOT GIVE STEROIDS UNTILL OTHER DIAGNOSIS ARE EXCLUDED,AS THE STEROIDS CAN MASK EARLY LEUKEMIA. Reduce Ab production,RES phagocytosis of antibody coated platelets,improve vascular integrity, improve platelet production Prednisone 1-2 mg/kg/day(max 60 /day) in 3 divided doses x 2-4 wks, followed by a taper of 4mg / kg/day ,divided into 3 doses for 4 days OR Methylprednisolone( 30-50 mg /kg/day) for 3-7 days Some cases may need repeat courses CORTICOSTEROIDS-short course/pulse course Anti-D for Rh positive patients Anti-Rho(D) immune globulin: has been shown to be effective Platelet transfusion: used in case of life threatening bleeding(ICH) The therapy is targeted to increase count to >20,000.In risk of life threatening bleeding , IV IG could be repeated or combined with steroids Monitoring: the patients getting pharmacologic intervention the usual hospital stay is 2 days.In the ambulatory setting ,platelet count monitored 1-2 times /wk ,interval can increase as the platelet increase .monitoring is necessary until the count return to >150,000/microL(50% in 1 mont,70% in 3 months) Chronic ITP Approximately 10-20% of children who initially present with ITP will become chronic defined as PLT <100K for >12 months Risk factors include older age, higher presenting platelet count at diagnosis, insidious onset of symptoms, and lack of preceding infection or vaccination Chronic ITP: persistent thrombocytopenia(<150,000/microL) for > 6 months 20-30% will have chronic ITP 1/3 rd of the cases will have spontaneous remission in months to years In chronic ITP the platelet count ranges between 20,000-75,000/microL.usually do not require any treatment Management: decrease the risk for bleeding. Role of Splenectomy Older child >4yoa with severe ITP lasting >1 year (chronic ITP) Symptoms not easily controlled with therapy Life-threatening hemorrhage complicating acute ITP Platelet count cannot be corrected rapidly with transfusion of platelets and administration of IVIG and corticosteroids SPLENECTOMY- may be needed in patients needing repeated /continuous pharmacologic intervention even 12 months after diagnosis Prognosis Father asked question is it going to happen again Severe bleeding is rare (<3% of cases) ICH occurs in <1% of patients 70-80% will have spontaneous resolution in 6 months Approximately 20% who present with acute ITP will go on to have chronic ITP This increases to 50% in adolescents Take Away points References UpToDate D'Orazio JA, Neely J, Farhoudi N. ITP in children: pathophysiology and current treatment approaches. J Pediatr Hematol Oncol 2013; 35:1. Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood 2010; 115:168.