Aspiration Pneumonia: Pathophysiology, Prevention & Management
advertisement

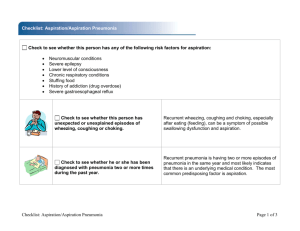
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/6585331 Aspiration pneumonia Pathophysiological aspects, prevention and management: A review Article in Panminerva medica · January 2007 Source: PubMed CITATIONS READS 11 910 4 authors, including: Angelo Petroianni Claudio Terzano Umberto I Policlinico di Roma Sapienza University of Rome 64 PUBLICATIONS 423 CITATIONS 179 PUBLICATIONS 1,108 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Smoking and COPD View project All content following this page was uploaded by Angelo Petroianni on 09 December 2016. The user has requested enhancement of the downloaded file. All in-text references underlined in blue are added to the original document and are linked to publications on ResearchGate, letting you access and read them immediately. PANMINERVA MED 2006;48:231-9 M C IN O E P R Y V R A IG M H E T ® DI C A Aspiration pneumonia Pathophysiological aspects, prevention and management A review A. PETROIANNI, D. CECCARELLI, V. CONTI, C. TERZANO Aspiration pneumonias occur more frequently than reported and, in many cases, the disease is not recognised. In hospitalised and institutionalised patients with predisposing diseases prompt diagnosis of this complication and correct preventive measures can drastically reduce the worsening of clinical conditions and the deaths due to aspiration pneumonia. Normal airway structure, effective defence mechanisms, and preventive measures are decisive in reducing aspiration episodes. An increased aspiration risk for food, fluids, medications, or secretions may lead to the development of pneumonia. Pneumonia is the most common respiratory complication in all stroke deaths and in mechanical ventilation patients. In addition, the increased incidence of aspiration pneumonia with aging may be a consequence of impairment of swallowing and the cough reflex. Dysphagia, compromised consciousness, invasive procedures, anaesthesia, insufficient oral care, sleep disorders, and vomiting are all risk factors. Aspiration pneumonia includes different characteristic syndromes based on the amount (massive, acute, chronic) and physical character of the aspirated material (acid, infected, lipoid), needing a different therapeutic approach. Chronic patients education and correct health care practices are the keys for preventing the events of aspiration. In patients at risk a clinical and instrumental assessment of dysphagia should be evaluated. Management includes the removal of etiologic factors (drugs, tubes, mobilisation, oral hygiene), supportive care, and in bacterial pneumonias a specific antibiotic therapy for community-acquired or nosocomial events. KEY WORDS: Pneumonia, aspiration - Dysphagia - Pneumonia, prevention and control – Pneumonia, therapy. A spiration is defined as the inhalation of fluid and secretions into the larynx and the lower res- Received on February 16, 2006. Accepted for publication on December 15, 2006 Address reprint requests to: Dr. A. Petroianni, Via Etruria 12, 00183 Roma, Italy. E-mail: angelo.petroianni@uniroma1.it Vol. 48 - No. 4 Unit of Respiratory Diseases Policlinico Umberto I Fondazione E. Lorillard Spencer Cenci University La Sapienza, Rome, Italy piratory tract, and aspiration pneumonia is the pathologic consequence of this abnormal intake. Several pulmonary syndromes may occur after aspiration, depending on the amount and nature of the aspirated material, its character (acid or neutral, infected or sterile), the frequency of aspiration episodes, and the host’s response.1 Some authors define as aspiration pneumonitis (Mendelson’s syndrome) the chemical injury caused by inhalation of sterile gastric contents, whereas aspiration pneumonia is the infectious process caused by the inhalation of oropharyngeal secretions that are colonized by pathogenic bacteria.2 In this review we define chemical inflammation and infection as pneumonia, classifying the different syndromes in chemical, bacterial, and lipoid pneumonias. Aspiration can be an acute or chronic process, and it can occur in the community or in a hospital setting. Even healthy subjects commonly aspirate, but normal defence mechanisms usually clear the inoculum, and these aspiration events rarely result in bacterial pneumonia.3 Aspiration pneumonia commonly occurs in those individuals who tend to aspirate, because of dysphagia due to neurological disease or oesophageal disorders, central nervous system disorders, and altered consciousness.4 Other risk factors for aspiration pneumonia include conditions in which the bacterial inoculum into the lung increases, such as periodontal disease, PANMINERVA MEDICA 231 PETROIANNI ASPIRATION PNEUMONIA TABLE I.—Predisposing factors for pulmonary aspiration. Compromised consciousness — alcohol intoxication — drug abuse — anaesthesia — neurological disorders — psychiatric diseases Dysphagia — neurological disorders (Parkinson’s disease, stroke, myasthenia gravis, amyotrophic lateral sclerosis, multiple sclerosis) — oesophageal disease (gastroesophageal reflux, achalasia, esophageal cancer, structural abnormalities of the pharynx and oesophagus) Invasive procedures of upper aerodigestive tract — nasogastric and percutaneous feeding tubes — endotracheal tubes — tracheostomy Vomiting Periodontal diseases Sleep disorders M C IN O E P R Y V R A IG M H E T ® DI C A dental or tonsillar abscess, the ingestion of sedative drugs, and any conditions that induce emesis.5 In addition, outside the hospital most cases are observed in alcoholics, the elderly, those who spend considerable time in the recumbent position, and the generally debilitated. The act of aspiration is usually not witnessed and the clinical presentation is often very similar to other pneumonias: cough, chest pain, dyspnoea and fever. However, symptoms tend to take days to weeks to evolve and aspiration can lead to the development of lobar or segmental pneumonia, weight loss, anaemia and lung abscess or empyema.6 In this review we discuss pathophysiological mechanisms and clinical features as well as management and preventive measures of aspiration pneumonia. An accurate anamnesis, direct or indirect, is essential to diagnose the disease and particularly to avoid relapses and worsening of complex patients. Epidemiology Although pulmonary aspiration is an important cause of serious illness and death, epidemiological data of aspiration pneumonia are poorly defined: in some papers7 its prevalence among all pneumonia was not determined. Nevertheless, several studies indicated that 5-15% of cases of community-acquired pneumonia are aspiration pneumonia.2 Aspiration pneumonia occurs most commonly in hospitalised and institutionalised patients, particularly those with pre-existing predisposing factors such as stroke, seizures and dysphagia due to several causes.1, 8 Aspiration pneumonia is the most common cause of death in patients with dysphagia due to neurological disease, developing in approximately 500 000 patients per year in the US.9 Marrie et al.10 indicated that the incidence of aspiration pneumonia in patients with nursing home acquired pneumonia was 18% and in control patients with community acquired pneumonia 5%. Aspiration pneumonia occurs in 10% of patients who are hospitalised after a drug overdose4, 11 and it is the cause of 10-30% of all death with anaesthesia.12, 13 The incidence of aspiration pneumonia is likely to rise, considering an increasing elderly population with factors predisposing to aspiration.1, 14 232 Pathophysiology The airway structure and the defence mechanisms are decisive in reducing aspiration episodes. An effective cough mechanism, mucociliary transport system, and normal function of the laryngeal tract allow good protection for this complication.15 Founded on a structural airway analysis, some papers reported a more frequent incidence for the right lung than the left. In fact anatomically the right main bronchus shows a vertical positioning more than the left main bronchus, and this could promote aspiration episodes preferentially in the right lung. Some pathological conditions, acute or chronic, can predispose for aspiration pneumonia (Table I). The predisposing factors for pulmonary aspiration are different in infants, in whom congenital airway defects or acute events prevail.5 There is a strong association between dysphagia and the development of aspiration pneumonia. This predisposing factor is the most frequent aetiology in chronic patients.9, 16 Swallowing is a complex and coordinately neuromuscular activity involving rapid coordination of structure in the oral cavity, pharynx, larynx and oesophagus. It is described as involving 3 anatomical and temporal phases: the oral, the pharyngeal and the oesophageal. The first is under voluntary control, whereas the second 2 stages are involuntary, being under reflexive control. The purpose of the first stage is to move food or liquid from the oral cavity to the anterior faucial arches, where reflexive swallowing is initiated; during the second stage, food is transported towards the oesoph- PANMINERVA MEDICA December 2006 ASPIRATION PNEUMONIA PETROIANNI to the onset of the swallowing action. The latent time (seconds) of swallowing was 1.2±0.1 in control subjects, 5.2±0.6 in patients with dementia, and 12.5±3 in patients with aspiration pneumonia. The cough threshold was determined using various concentrations of citric acid. The threshold concentration for citric acid was 2.6±4 mg/mL in control subjects, 37.1±16.7 mg/mL in patients with dementia, and > 360 mg/mL in patients with aspiration pneumonia.30 These results showed that the increased incidence of pneumonia with aging may be a consequence of impairment of swallowing and the cough reflex with senescence. Numerous studies have confirmed the effects of ageing on swallowing.28, 29 The major finding of these studies is that older people swallow more slowly, but the safety of oropharyngeal swallowing is not compromised. However, the incidence of cerebrovascular and degenerative neurological disease increases with aging and these disorders are closely associated with impaired swallowing and cough reflex and an increased risk of aspiration.31 A clinical assessment of dysphagia should observe parameters like oral control, lingual activity, oral residue, laryngeal excursion, voice quality and coughing after swallowing. Available evidence, although limited, suggests that a clinical assessment has approximately 80% sensitivity and 70% specificity for detecting aspiration in elderly adults.30 The instrumental assessment supplements the clinical assessment. The videofluoroscopic swallowing assessment (VFSS) is the most utilized instrumental tool for determining the nature and extent of swallowing disorders.32 It identifies the disorders in movement patterns of the oropharyngeal, laryngeal and oesophageal structures, that may result in aspiration or inefficient swallowing. Limitations are imposed by patient cooperation, timing of studies, and the ability to generalize to clinical settings. In addition fiberoptic endoscopic evaluation of swallowing (FEES) can give information on anatomy, the swallowing process, pharyngeal motility, and sensory deficits.33, 34 Although aspiration cannot be observed directly, it can be inferred from the residue left after swallowing or ejection of material out of the trachea after coughing. On comparison with VFSS in a small sample of dysphagic patients, FEES gave better sensitivity values.32 This assessment can also be conducted at the bedside, and it is safe and well tolerated. In recent years other clinically applicable methods M C IN O E P R Y V R A IG M H E T ® DI C A agus; there is the velopharyngeal closure to prevent the entry of food or liquid into the nasal cavity and airway aspiration is prevented through elevation and closure of the larynx. At the same time the cricopharyngeal region is open to allow bolus passage into the oesophagus. The upper oesophageal sphincter (UES) made up of cricopharyngeus attaches to the cricoid cartilage. At rest, the UES closes to prevent reflux from the oesophagus to the pharynx.17 One of the mechanisms that prevent aspiration during swallowing, such as vocal cord closure, aryepiglottic approximation, and laryngeal elevation, or during gastroesophageal reflux, such as contraction of the UES, may become impaired and this can lead to inhalation of food and to pneumonia. Swallowing abnormality are a common functional impairment of acute stroke, affecting as many as half of all patients,18 and its detection is an important part of acute stroke management.19 The literature suggests that swallowing difficulties can affect 22-65% of stroke patients, depending on the methods of assessment used,20, 21 and may persist in some patients for many months.22, 23 It is estimated that up to 38% of stroke victims die within the first month after stroke onset. Pneumonia contributes to 34% of all stroke deaths and represents the third cause of mortality in the first month after stroke.24 After a stroke or other neurological event, the laryngeal cough reflex may be weakened or absent. This increases the aspiration risk for food, medications, fluids, or secretions past the true vocal cords and may lead to the development of pneumonia.25 Loeb et al.26 investigated the risk factors for pneumonia in elderly residents of long-term care facilities. In this study multivariated analysis revealed that difficulty swallowing food and medication were the most important risk factors leading to pneumonia. Vergis et al.27 identified witnessed aspiration and sedative medications, which impair the cough reflex and swallowing, as the most important risk factors for pneumonia in a long-term facility. An assessment of swallowing reflex, cough reflex, and mucociliary transport system may determine the critical level of depression in the defence system that leads to aspiration pneumonia. Several methods to assess these mechanisms have been reported.28, 29 In one of these the swallowing reflex was induced by a bolus injection of 1 mL of distilled water into the pharynx. The swallowing action was evaluated by the latency of the response, which was timed from the injection Vol. 48 - No. 4 PANMINERVA MEDICA 233 PETROIANNI ASPIRATION PNEUMONIA The overall mortality rate associated with massive aspiration of gastric acid is approximately 30% and is greater than 50% in patients with initial shock, secondary infectious pneumonia, or adult respiratory distress syndrome (ARDS).36 M C IN O E P R Y V R A IG M H E T ® DI C A for the assessment of the risk of aspiration pneumonia in the elderly have been reported: the swallowing provocation test (SPT) and the simple SPT (S-SPT) proved very useful in differentiating patients with or without stroke who are predisposed to aspiration.35 Classification of aspiration pneumonia Aspiration pneumonia includes different characteristic syndromes based on the nature of the inoculum and the inflammatory reaction. The amount and physical character of the aspirated materials determines the different management. Chemical pneumonia Aspiration of gastric contents during vomiting may have significant consequences and may occur after sedation, anaesthetization,13 drug intoxication,11 gastrointestinal stasis or obstruction,36 autonomic dysfunction and other disorders.37 Vomiting with massive aspiration of gastric contents is a frequent phenomenon and is probably one of the most frequent causes of aspiration disease in healthy subjects. Chronic aspiration of gastric contents may result from primary disorders of the larynx or the oesophagus, such as achalasia, oesophageal stricture, scleroderma, oesophageal carcinoma, and gastroesophageal reflux. Several studies have demonstrated that the severity of lung injury increases directly with the volume of the aspirate and with decreasing pH.38 Aspiration of pure gastric acid (pH<2.5) causes an intense parenchymal inflammatory reaction, which results in extensive desquamation of the bronchial epithelium, bronchiolitis, pulmonary oedema, and haemorrhage, mediated by inflammatory cells and cytokines, including TNF-a, IL-8, and reactive oxygen products.39, 40 The content of the stomach is generally sterile, because the low pH of the gastric acid prevents the growth of micro-organisms. Bacterial infection may occur as a complication of the lung injury 2-3 days after aspiration, or when the pH of the gastric content is higher because of the use of antiacid, proton-pump inhibitors, or histamine H2-receptor antagonists.16, 41 Moreover, there may be a gastric colonization by gramnegative bacteria in patients who receive enteric feedings, or in patients with gastroparesis or small bowel obstruction.42 234 Bacterial pneumonia Upper airway secretions and colonizing microorganisms are frequent causes of bacterial community acquired and nosocomial aspiration pneumonias. It is widely believed that silent aspiration into the intrathoracic airways is a common occurrence in normal subjects, and approximately half of all healthy adults aspirate small amounts of oropharyngeal secretions during sleep.43 Pneumonia is usually prevented by mechanical and immunological defence mechanisms such as coughing, mucociliary clearance, airway and alveolar phagocytes. All these mechanisms, together with the low burden of virulent bacteria in normal pharyngeal secretions, allow a clearance of the infectious material without consequence. Therefore, aspiration pneumonia may follow if the aspirated inoculum is large enough, or if mechanical, humoral, or cellular defences are impaired. Huxley et al.3 injected small boluses of a solution of 111In chloride into the nose of 20 normal subjects and in 10 patients with coma or stupor, during nocturnal sleep. The results were that in 9 of the 20 normal subjects some 111In was found in lung parenchyma the day after. They also observed that sound sleep was a risk factor for aspiration of upper airway secretion. Other studies44 investigated whether oral care lowers the frequency of pneumonia in the institutionalised elderly. During follow-up, pneumonia was diagnosed in 19% of participants who didn’t receive oral care and in 11% of those who did. In aspiration pneumonias several pathogens can be isolated in the same patient. The predominant anaerobes include fusobacterium, clostridium species, and members of the bacteroides fragilis group. The major aerobic pathogens are Staphylococcus aureus, Klebsiella pneumoniae, and Pseudomonas aeruginosa.45 Lipoid pneumonia This syndrome is described separately because of its peculiarity in inflammatory response through a granulomatous reaction. Lipoid material glides down the PANMINERVA MEDICA December 2006 ASPIRATION PNEUMONIA PETROIANNI in a patient at risk, the diagnosis is usually based on findings of hypoxemia, pulmonary infiltrates, fever and leukocytosis. Rales, productive cough, wheezing, or cyanosis are present in the majority of patients. Anamnesis should investigate gastrointestinal conditions (vomiting, gastroesophageal reflux, achalasia, hiatal hernia), neurological disorders, psychiatric illness, medications, alcoholism, surgical operations, endoscopic procedures, sleep disorders, and periodontal diseases. Clinically chemical pneumonitis can represent the onset of respiratory distress, with cough, wheezing, fever, and tachypnea. Radiographic findings in acute gastric acid aspiration include bilateral perihilar, ill-defined, alveolar consolidations, multifocal patchy infiltrates, and segmental or lobar consolidation, which is usually localized to one or both lung bases.36 In bacterial pneumonias radiographic findings vary among the various species of bacteria. Aspiration of infected material results in a localized or lobar consolidation. Over a period of weeks after aspiration, cavitation, abscess, and empyema may occur. A prolonged clinical course or large aspirations may result in severe necrotizing bronchopneumonia.51 High resolution computed tomography (HRCT) showed a great capacity to establish the severity of the disease, especially for lipoid pneumonia (Figure 1). In this syndrome CT hypodense images are assessed by density measurement (Hounsfield Units, HU) or by visual comparison with subcutaneous adipose tissue or by the “angiogram sign” on parenchymal window setting. A negative density (between –150 and –30 HU) is highly suggestive of the presence of intrapulmonary fat.52 Lung function tests may reveal a normal or a restrictive ventilatory syndrome or a mixed syndrome; therefore, these parameters prove of less diagnostic value. The transfer factor for carbon monoxide was frequently abnormal. The appearance of bronchoalveolar lavage may be highly suggestive and the results of quantitative cultures of samples obtained with a protected specimen brush are particularly helpful for etiologic diagnosis. At differential cell count, various cytological profiles have been described: macrophage alveolitis, lymphocytic alveolitis and neutrophilic alveolitis.53 Microscopic and histological examination with specific stains (gram, sudan black, sudan red), and spectrophotometry or chromatography can be fundamental. Often the granulomatous form of the inflammato- M C IN O E P R Y V R A IG M H E T ® DI C A respiratory tract without stimulating cough and is not removed effectively by the cilia.46 The aspiration of a massive amount of liquid paraffin and petroleum may lead to an acute and fatal form of exogenous lipoid pneumonia. The prognosis of this entity is usually good if the disorder is quickly identified and the offending agent removed, unless the pneumonia is so widespread and severe, causing respiratory failure, or is associated with a superimposed infection. Lipoid pneumonia may be complicated by hypercalcaemia due to lipid granulomas, mycobacterial infection, progressive fibrosis or lung cancer.47 It is usually related to accidental poisoning in children, but it is also observed in fire-eaters. Repeated inhalation of mineral oil or a related substance into the distal lung can lead to chronic lipoid pneumonia. In adults it is related to the treatment of constipation with paraffin oil48 and the repeated use of oily nose drops for chronic rhinitis, mainly at bedtime. Animal fat, which can be hydrolysed to fatty acids, causes more inflammation than vegetable or mineral oils, but all types stimulate a chronic granulomatous inflammation, which tends to be located in the lower or middle lobes. A clinical diagnosis may be supported by bronchoalveolar lavage, transbronchial biopsy, and specific stains (sudan black, sudan red, oil red O).49 Diagnosis In patients with aspiration pneumonia the aspiration episode is generally not seen.2 In some cases, patients have no symptoms and the disease is an incidental finding. The diagnosis is, therefore, inferred when a patient at risk for aspiration has radiographic evidence of an infiltrate in a characteristic bronchopulmonary segment. Body position at the time of aspiration determines which lung zones are dependent. In patients who aspirate while in a recumbent position, the most common sites of involvement are the posterior segments of the upper lobes and the apical segments of the lower lobes, whereas in patients who aspirate in an upright or semirecumbent position, the basal segment of the lower lobes is usually affected.50 The process is similar to a typical community acquired pneumonia, but, if not treated, they have a higher incidence of complications such as cavitation and lung abscess.45 After an observed or suspected episode of aspiration Vol. 48 - No. 4 PANMINERVA MEDICA 235 ASPIRATION PNEUMONIA M C IN O E P R Y V R A IG M H E T ® DI C A PETROIANNI Figure 1.—High resolution computed tomography (HRCT) aspiration pneumonia. Ground-glass and reticulonodular infiltrates, and thick-walled cystic spaces in the right lung. ry cell reaction suggests a foreign body disease, and the frequency of fibrosis lesions explains the potential severity of the disease. Differential diagnosis has to consider a non-aspiration pneumonia, ARDS, pulmonary oedema, pulmonary haemorrhage, immunoallergic or neoplastic diseases.54 The diagnosis of aspiration pneumonia is difficult, because the disease and its complications can mingle. Relevant complications are acute respiratory failure, shock, ARDS, lung abscess, empyema, necrotizing pneumonia, fibrosis, and systemic spread of infection. Data about microbiological diagnosis of aspiration bacterial pneumonia are disparate. Several studies enrolled patients observed relatively late, when complications such as necroziting pneumonia, lung abscess or empyema had already occurred, and in these patients anaerobic organisms were found to be the predominant pathogens, from 62% to 100%, isolated alone or with aerobes.49, 51 Furthermore, in many cases, it is impossible to isolate the responsible pathogens. Mier et al.55 studied the bacteriology of early aspiration pneumonia with the use of protected brushing. Positive results were obtained for only 9 of 42 patients (47%). The recovered pathogens were S.pneumoniae (28.5%), other Streptococcus spp. (21.4%), S. aureus (14.3%), and gram-negative bacilli (35.7%). In another study the 236 cultures were positive in 60% of patients. The most common aerobic organisms were S. pneumoniae (23%), Staphylococcus spp. (29%), and gram-negative bacilli (40%). However, significant isolation of anaerobic bacteria in patients suffering from lower respiratory tract infection is difficult, because it requires specific sampling techniques, adequate transport conditions and specific growth media. Prevention and prognosis Aspiration pneumonia in many cases is a preventable disease requiring attention to patient care. A semirecumbent position, as opposed to supine, may prevent aspiration pneumonia by minimising gastroesophageal reflux and subsequent inhalation of gastric contents.56 Oral hygiene and dental prophylaxis may reduce the oral pathogenic bacilli load in subjects who have a high rate of aspiration and in elderly nursing home patients.14, 57 In these patients an assessment of swallowing, with a videofluoroscopic swallowing study and/or endoscopic evaluation, could also be necessary. There are contradictory aspects to the issue of feeding tubes and aspiration pneumonia. Feeding tubes have to be managed properly. The position of oral PANMINERVA MEDICA December 2006 ASPIRATION PNEUMONIA PETROIANNI First of all the disease (gastroesophageal, neurological, psychiatric) or the process (medications, alcoholism, feeding tubes) inducing aspiration pneumonia should be treated. Many nosocomial aspiration events represent chemical pneumonia and do not require antibiotic therapy. However, antibiotic therapy is commonly indicated in patients with aspiration pneumonia, because many patients are debilitated or immunocompromised, and so at increased risk for infectious pneumonia. The choice of the antibiotic should depend on the setting in which the aspiration occurs as well as the patient’s general health. In the case of community-acquired aspiration pneumonia, empiric treatment must principally cover anaerobic and streptococcal species. The usual oropharingeal flora is most likely involved in communityacquired cases, and treatment with penicillin is generally sufficient.45 Recommended antibiotic regimens include penicillin and beta-lactamase inhibitor combinations, such as ampicillin/sulbactam or amoxicillin/clavulanate, or clindamycin. Fluoroquinolones, such as levofloxacin and moxifloxacin, have reasonable anaerobic activity and achieve high concentrations in endobronchial secretions and lung tissue. Patients at risk for nosocomial pneumonia must be treated for gram-negative enteric bacilli and staphylococci, until culture results are available to guide therapy.36 Nosocomial aspiration pneumonia often occurs in very sick patients with modified oral flora, and abnormalities of the gastrointestinal tract, that favour the proliferation of gram-negative species.45 Possibly, it is wise to base the treatment on the results of quantitative cultures of samples obtained with a protected specimen brush.45 The risk of aggressive pathogens, such as Pseudomonas aeruginosa and Acinetobacter species, is highest in patients in intensive care units and those in mechanical ventilation. Patients with coma, diabetes mellitus, or end-stage renal disease are at high risk for staphylococcal pneumonia. Therefore, patients with nosocomial aspiration pneumonia may receive cephalosporin, such as cefepime or ceftazidime, and clindamycin or metronidazole. An effective alternative may be penicillin and beta-lactamase inhibitor combination, such as ampicillin/sulbactam,60 piperacillin/tazobactam, or ticarcillin/clavulanate. For patients allergic to penicillin, fluoroquinolones or a clindamycin and aztreonam combination may be considered. Vancomycin should be used for antistaphy- M C IN O E P R Y V R A IG M H E T ® DI C A feeding tubes should be monitored because they can easily become displaced over time.58 On the other hand, it is reasonable to believe that feeding tubes reduce the risk of aspiration pneumonia in some patients with swallowing difficulties, but they offer no protection from aspiration of oral secretions. Correct education of patients at risk and the sensitisation of health care personnel are the keys for preventing this serious complication. Guidelines for preventing health-care- associated pneumonia have been reported by the Center for Disease Control and Prevention of US (CDC).59 Prognosis of aspiration pneumonia varies considerably in the different studies because of the several confusing parameters involved in the mortality rate. In numerous series most deaths appeared to be attributable to the aspiration rather than to the disease leading to the aspiration.59 Nevertheless in Hickling’s study7 the mortality rate appears low (21%), and the deaths have been most often attributable to underlying illness than to an aspiration event. Another study16 has demonstrated a crude mortality of 22% and an attributable mortality linked to pneumonia of 11%, after excluding patients who died as a result of diseases leading to aspiration. The severity of the aspiration event is relevant for the mortality rate. Massive aspiration showed a mortality rate of 70%, whereas aspiration pneumonia complicated by empyema showed a mortality of 20%. For uncomplicated pneumonia the mortality rate was approximately 5%.7 Management All patients with aspiration pneumonia need supportive care as well as specific treatment. Oxygen supplementation and i.v. hydration may be necessary. The upper airway should be suctioned if feeding tube, foreign material, or secretions are still present in the oropharynx. Suctioning should be properly performed to avoid inducing gagging and emesis. Endotracheal intubation may be necessary in patients unable to protect their airways, with altered mental status, or persistent hypoxia. Positive pressure mechanical ventilatory support may be required in severe cases. The therapeutic approach for aspiration pneumonia is based on the knowledge of the presumable etiologic factor, through accurate anamnesis, clinical and instrumental data. Vol. 48 - No. 4 PANMINERVA MEDICA 237 PETROIANNI ASPIRATION PNEUMONIA 6. Marom EM, McAdams HP, Erasmus JJ, Goodman PC. The many faces of pulmonary aspiration. Am J Roentgenol 1999;172:121-8. 7. Hickling KG, Howard R. A retrospective survey of treatment and mortality in aspiration pneumonia. Int Care Med 1988;14:617-22. 8. Teixeira A, Cherin P, Demoule A, Levy-Soussan M, Straus C, Verin E et al. Diaphragmatic dysfunction in patients with idiopathic inflammatory myopathies. Neuromuscul Disord 2005;15:32-9. 9. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003;124:328-36. 10. Marrie TJ, Durant H, Kwan C. Nursing home-acquired pneumonia: a case-control study. J Am Geriatr Soc 1986;34:697-702. 11. Aldrich T, Morrison J, Cesario T. Aspiration after overdosage of sedative or hypnotic drugs. South Med J 1980;73:456-8. 12. Olsson GL, Hallen B, Hambraeus-Jonzon K. Aspiration during anaesthesia: a computer-aided study of 185,358 anaesthetics. Acta Anaesthesiol Scand 1986;30:84-92. 13. Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology 1993;78:56-62. 14. Watando A, Ebihara S, Ebihara T, Okazaki T, Takahashi H, Asada M et al. Daily oral care and cough reflex sensitivity in elderly nursing home patients. Chest 2004;126:1066-70. 15. Teramoto S, Ishii T, Yamamoto H, Yamaguchi Y, Namba R, Hanaoka Y et al. Significance of chronic cough as a defence mechanism or a symptom in elderly patients with aspiration and aspiration pneumonia. Eur Respir J 2005;25:210-1. 16. Davis LA, Thompson Stanton S. Characteristics of dysphagia in elderly patients requiring mechanical ventilation. Dysphagia 2004;19:714. 17. Aviv JE, Kaplan ST, Thomson JE, Spitzer J, Diamond B, Close LG et al. The safety of flexible endoscopic evaluation of swallowing with sensory testing (FEESST): an analysis of 500 consecutive evaluations. Dysphagia 2000;15:39-44. 18. Horner J, Massey EW. Silent aspiration following stroke. Neurology 1988;38:317-9. 19. Gordon C, Langton Hewer R, Wade DT. Dysphagia in acute stroke. BMJ 1987;295:411-4. 20. Kidd D, Lawson J, Nesbitt R, MacMahon J. Aspiration in acute stroke: a clinical study with videofluoroscopy. QJM 1993;86:825-9. 21. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil 1998;79:14-9. 22. Smithard DG, O'Neill PA, England RE, Park CL, Wyatt R, Martin DF et al. The natural history of dysphagia following a stroke. Dysphagia 1997;12:188-93. 23. Nilsson H, Ekberg O, Olsson R, Hindfelt B. Dysphagia in stroke: a prospective study of quantitative aspects of swallowing in dysphagic patients. Dysphagia 1998;13:32-8. 24. Heros RC. Stroke: early phatophysiology and treatment: summary of the fifth annual decade of the brain symposium. Stroke 1994;25:1877-81. 25. Roth EJ. Medical complications encountered in stroke rehabilitation. Phys Med Rehab Clin North Am 1991;2:563-78. 26. Loeb M, McGreer A, McArtur M, Walter S, Simor AE. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med 1999;159:2058-64. 27. Vergis EN, Brennen C, Wagener M, Muder RR. Pneumonia in a long term care: a prospective case-control study of risk factors and impact on survival. Arch Intern Med 2001;161:2378-81. 28. Nicosia MA, Hind JA, Roecker EB, Carnes M, Doyle J, Dengel GA et al. Age effects on the temporal evolution of isometric and swallowing pressure. J Geront A Biol Sci Med Sci 2000;55:M634-40. 29. Robbins J, Hamilton JW, Lof JL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology 1992;103:823-9. 30. Murray J. Manual of dysphagia assessment in adults. San Diego, CA: Singular Publishing Group; 1999. M C IN O E P R Y V R A IG M H E T ® DI C A lococcal coverage in hospitals with methicillin-resistant S. aureus. Treatment for 7-10 days appears adequate for patients who respond promptly. Therapy should be extended from 14 to 21 days if highly resistant pathogens, such as P. aeruginosa or Acinetobacter species, are isolated. Patients with lung abscess, cavitary pneumonia, or empyema require long-term treatment for 4-8 weeks or more.1 Corticosteroids have been used for decades in the management of aspiration pneumonia, but there are limited data to support this practice. Studies were generally unsuccessful and sometimes the outcomes were worse for those treated with corticosteroids. The patient’s clinical course should be monitored. Prompt clinical response over the first few days, including rapid clearing of pulmonary infiltrates, could suggest chemical pneumonitis rather than bacterial pneumonia. Conclusions Pulmonary involvement and symptoms in hospitalised and institutionalised patients with compromised consciousness, dysphagia, invasive procedures, vomiting, neurological or psychiatric disease, or treated with sedative drugs should make us suspicious of aspiration pneumonia. Management of these patients is complex because of severe concomitant diseases. Antimicrobial therapy for aspiration pneumonia is often empirical and should be based on patient characteristics. It is essential to know the setting in which aspiration occurred, the severity of pneumonia, and information regarding local pathogens and resistance patterns, and, last but not least, an accurate anamnesis for reducing the mortality rate and avoiding chronic and irreversible compromise of lung parenchyma. References 1. Johnson JL, Hirsch CS. Aspiration pneumonia. Postgrad Med 2003;113:99-112. 2. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001;344:665-71. 3. Huxley EJ, Viroslav J, Gray WR, Pierce AK. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am J Med 1978;64:564-8. 4. Roy TM, Ossorio MA, Cipolla LM, Fields CL, Snider HL, Anderson WH. Pulmonary complications after tricyclic antidepressant overdose. Chest 1989;96:852-6. 5. Bauer ML, Figueroa-Colon R, Georgeson K, Young DW. Chronic pulmonary aspiration in children. South Med J 1993;86:789-95. 238 PANMINERVA MEDICA December 2006 ASPIRATION PNEUMONIA PETROIANNI 47. Gondouin A, Manzoni P, Ranfaing E, Brun J, Cadranel J, Sadoun D et al. Exogenous lipid pneumonia: a retrospective multicentre study of 44 cases in France. Eur Respir J 1996;9:1463-9. 48. Terzano C, Ricci A, Petroianni A, Laurendi G, Mammarella A, Paoletti V et al. Lipoid pneumonia in multiple sclerosis: an insidious complication. Adv Ther 2003;20:138-42. 49. Franquet T, Giménez A, Bordes R, Rodríguez-Arias JM, Castella J. The crazy-paving pattern in exogenous lipoid pneumonia: CT-pathologic correlation. Am J Roentgenol 1997;170:315-7. 50. Terpenning M. Prevention of aspiration pneumonia in nursing home patients. Clin Infect Dis 2005;40:7-8. 51. Lorber B, Swenson RM. Bacteriology of aspiration pneumonia: a prospective study of community- and hospital-acquired cases. Ann Intern Med 1974;81:329-31. 52. Lee JS, Im JG, Song KS, Seo JB, Lim TH. Exogenous lipoid pneumonia: high-resolution CT findings. Eur Radiol 1999;9:287-91. 53. Midulla F, Strappini PM, Ascoli V, Villa MP, Indinnimeo L, Falasca C et al. Bronchoalveolar lavage cell analysis in a child with chronic lipid pneumonia. Eur Respir J 1998;11:239-42. 54. Talwar A, Mayerhoff R, London D, Shah R, Stanek A, Epstein M. False-positive PET scan in a patient with lipoid pneumonia simulating lung cancer. Clin Nucl Med 2004;29:426-8. 55. Mier L, Dreyfuss D, Darchy B, Lanore JJ, Djedaini K, Weber P et al. Is penicillin G an adequate initial treatment for aspiration pneumonia? Int Care Med 1993;19:279-84. 56. Orozco-Levi M, Torres A, Ferrer M, Piera C, el-Ebiary M, de la Bellacasa JP et al. Semirecumbent position protects from pulmonary aspiration but not completely from gastroesophageal reflux in mechanically ventilated patients. Am J Respir Crit Care Med 1995;152:138790. 57. Yoneyama T,Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K et al. Oral care reduces pneumonia in older patients in nursing homes. J Am Geriatr Soc 2002;50:430-3. 58. Kalinowski CP, Kirsch JR. Strategies for prophylaxis and treatment for aspiration. Best Pract Res Clin Anaesthesiol 2004;18:719-37. 59. Healthcare Infection Control Practices Advisory Committee; Centers for Disease Control and Prevention (U.S.). Guidelines for preventing health-care-associated pneumonia, 2003 recommendations of the CDC and the Healthcare Infection Control Practices Advisory Committee. Respir Care 2004;49:926-39. 60. Allewelt M, Schuler P, Bolcskei PL, Mauch H, Lode H; Study Group on Aspiration Pneumonia. Ampicillin + sulbactam vs clindamycin +/- cephalosporin for the treatment of aspiration pneumonia and primary lung abscess. Clin Microbiol Infect 2004;10:163-70. M C IN O E P R Y V R A IG M H E T ® DI C A 31. Sekizawa K, Ujiie Y, Itabashi S, Sasaki H, Takishima T. Lack of cough reflex in aspiration pneumonia. Lancet 1990;335:1228-9. 32. Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope 2000;110:563-74. 33. Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B et al. FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol 1998;107:37887. 34. Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 1991;100:678-81. 35. Teramoto S, Yamamoto H, Yamaguchi Y, Ouchi Y, Matsuse T. A novel diagnostic test for the risk of aspiration pneumonia in the elderly. Chest 2004;125:801-2. 36. Bynum LD, Pierce AK. Pulmonary aspiration of gastric contents. Am Rev Respir Dis 1976;114:1129-36. 37. Brown NW. Medical consequences of eating disorders. South Med J 1985;78:403-5. 38. James CF, Modell JH, Gibbs CP, Kuck EJ, Ruiz BC. Pulmonary aspiration - effects of volume and pH in the rat. Anesth Analg 1984;63:6658. 39. Nader-Djalal N, Knight PR 3rd, Thusu K, Davidson BA, Holm BA, Johnson KJ et al. Reactive oxygen species contribute to oxygen-related lung injury after acid aspiration. Anesth Analg 1998;87:127-33. 40. Folkesson HG, Matthay MA, Hebert CA, Broaddus VC. Acid aspiration-induced lung injury in rabbits is mediated by interleukin-8dependent mechanisms. J Clin Invest 1995;96:107-16. 41. Bonten MJ, Gaillard CA, van der Hulst R, de Leeuw PW, van der Geest S, Stobberingh EE et al. Intermittent enteral feeding: the influence on respiratory and digestive tract colonization in mechanically ventilated intensive-care-unit patients. Am J Respir Crit Care Med 1996;154:394-9. 42. Spilker CA, Hinthorn DR, Pingleton SK. Intermittent enteral feeding in mechanically ventilated patients: the effect on gastric pH and gastric cultures. Chest 1996;110:243-8. 43. Gleeson K, Eggli DF, Maxwell SL. Quantitative aspiration during sleep in normal subjects. Chest 1997;111:1266-72. 44. Yoneyama T, Yoshida M, Matsui T, Sasaki H. Oral care and pneumonia. Lancet 1999;354:515. 45. Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med 1974;56:202-7. 46. Spickard A, Hirschmann JV. Exogenous lipid pneumonia. Arch Intern Med 1994;154:686-92. Vol. 48 - No. 4 PANMINERVA MEDICA 239