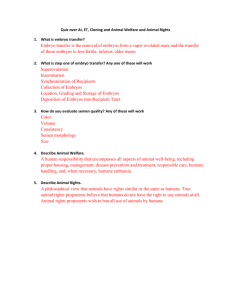
Fertility2013
advertisement

Human Fertility, 2013; 16(3): e1–e73 © 2013 The British Fertility Society ISSN 1464-7273 print/ISSN 1742-8149 online DOI: 10.3109/14647273.2013.810860 Fertility 2013 British Fertility Society Association of Clinical Embryologists Society for Reproduction and Fertility 3–5th January 2013, ACC, Liverpool ORAL PRESENTATIONS A1.1: The relationship between luteinising hormone in ovarian stimulation and subsequent embryo development and viability KIMBERLEY SWANN, JESSICA MEADOWS, KANNA MANNADIAR JAYAPRAKASAN, BRUCE CAMPBELL & WALID MAALOUF University of Nottingham, Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE], Division of Obstetrics and Gynaecology, School of Clinical Science, Nottingham, UK Aims: Ovarian stimulation is integral to most assisted reproductive treatments. Two recent systematic reviews demonstrated a significant increase in live birth rates in preparations containing LH activity compared to those containing FSH alone. Less attention however, has been focused on the effect of concentration and the duration of action of gonadotrophin preparations containing LH activity. In this study, we utilize the murine model to compare the effect of two different gonadotrophin preparations which contain FSH and LH activity at different ratios and half-lives, on embryo development and quality. Methods: Zygotes were collected from naturally mated female CBAB6F1 mice and after superovulation with either 0.5IU or 5IU human menopausal gonadotrophin (hMG) or Pergoveris. The number of embryos obtained and their subsequent development was monitored daily and the quality of the blastocysts, total cell number (TCN), ratio of ICM to TE allocation, and levels of apoptotic cells were recorded and appropriate statistical analyses employed. Results: The rate of cleavage to the 2-cell stage was comparable between hMG and unstimulated controls (P 0.05) but was significantly lower and more variable in the Pergoveris cohort (P 0.001). This delayed development persisted throughout pre-implantation culture where the median proportion of embryos achieving the blastocyst stage were significantly impaired by administration of hMG and Pergoveris vs. natural controls (P 0.05 and P 0.01). However, assessment of blastocyst quality demonstrated Pergoveris resulted in statistically more hatching blastocysts than control and hMG cohorts with greater average TCN counts (P 0.001) and a trend for reduced apoptosis (P 0.068). Conclusion: Ovarian stimulation with Pergoveris increases the number of hatching blastocysts, which appear to be of better quality to hMG counterparts. These differences highlight the potential drawback of using long-acting preparations of LH (hCG) on embryo quality and provides evidence in favour of a ceiling threshold of LH bioactivity. e1 e2 Abstracts A1.2: Accurate biopsy and ultrastructural morphological characterisation of decidua parietalis and basalis by a novel hysteroscopic technique: implications for early pregnancy trophoblast-decidua interactions VIKRAM SINAI TALAULIKAR, ISAAC MANYONDA & BRIDGET BAX Division of Clinical Sciences, St George’s University of London, London, UK Objective: An understanding of early events in human placentation might shed light on disorders such as miscarriage, intrauterine growth restriction and preeclampsia. The role of extracellular matrix in trophoblast invasion has gained wide attention in the recent times. Rigorous research is hampered in part by the poor accuracy of biopsy material used, and discrepancies in the results of studies of trophoblastic invasion have been acknowledged. We aimed to obtain accurate biopsies of decidua basalis and parietalis and describe their ultrastructural characteristics. Methods: The biopsy was performed in pregnancies undergoing first trimester surgical termination. Following cervical dilatation, a rigid hysteroscope was introduced into the cervical canal. The pressure of the saline distending medium sheared the membranes of the gestational sac away from decidua parietalis (DP), leaving the pregnancy suspended at the site of early placenta, the decidua basalis (DB). Under direct vision a biopsy forceps was used to sample DP, and then the forceps introduced beneath the gestational sac to sample DB. The biopsies were subjected to light and electron microscopy as well as immunohistochemistry. Results: Morphological and immunohistochemical studies confirmed the accuracy of the samples, with a high (40%) myometrial spiral artery presence, and presence of trophoblast in DB and its absence in DP. Prominent ultrastructural morphological differences were noted between the two types of decidua between 9–12 weeks of gestation such as 1) thicker (56.46/16.97 nm) collagen fibrils in DB versus DP (45.28/11.33 nm) (p value 0.0001) and 2) altered lengths and distribution of collagen fibres. Conclusion: We describe a simple, yet accurate novel technique of decidual biopsy under direct hysteroscopic vision. We have also reported the differences in the ultrastructure of the extracellular matrix between DB and DP which may play an important role in regulating the depth of trophoblast invasion. A1.3: Isolation and expression of the gametocyte-specific factor 1 gene (GTSF1) in human oocytes and preimplantation embryos JOHN HUNTRISS, JIANPING LU, MATTHEW COTTERILL, MATTHEW HINKINS, ROSEMARY BAYNE, ANDERSON RICHARD & ADAM BALEN Division of Reproduction and Early Development, Leeds Institute of Genetics, Health and Therapeutics, University of Leeds, Leeds, UK Aims: To isolate and sequence GTSF1 cDNA clones and to assess the expression of this gene in the human female germline. Content: Genes that are expressed specifically during gametogenesis are likely to be important for fertility. In mice, the Gametocyte-Specific Factor 1 gene (Gtsf1) is essential for spermatogenesis, however, the role of this gene in the female germline is not clear. Here we describe cloning and expression analysis of the human GTSF1 gene in human oocytes, preimplantation embryos, and foetal gonads. Relevance/Impact: Understanding the expression, localisation and function of human oocyte-specific genes is useful for determining their role in human reproduction. This report represents the first experimental cloning and expression profiling of the human GTSF1 gene on chromosome 12q13.2. Outcomes: GTSF1 cDNA clones were isolated from human oocytes containing the entire coding region that encodes a 167-amino acid protein with 91% identity to the murine Gtsf1 protein and exhibits two CHHC-type zinc finger domains. Reverse transcription-PCR revealed that transcripts of GTSF1 are detected in all adult oocyte stages from primordial follicles and onwards to metaphase II oocytes and are also present in preimplantation embryos. Real Time PCR revealed that GTSF1 expression was highest in GV stage oocytes, and expression increased again in blastocysts. In human adult somatic tissues, GTSF1 mRNA was highest in the testis. GTSF1 mRNA expression in human fetal ovary was observed to increase across the gestational range from 8 to 21 weeks, including the time at which primordial follicles are first formed. In human fetal testis GTSF1 expression increased from 8 to 19 weeks. Discussion: In humans, GTSF1 appears to be preferentially expressed in gametes and early embryos. This expression data, taken together with functional analysis of the gene from animal models will inform an understanding of the role of GTSF1 in human fertility. Human Fertility Abstracts e3 A1.4: Protection against perinatal loss by D6 receptor PEK JOO TEOH1, SM NELSON1, RJ NIBBS1 & GRAHAM BURTON2 1 Reproductive and Maternal Medicine, University of Glasgow; Glasgow, UK and 2School of the Biological Sciences, Department of Physiology, Development and Neuroscience, University of Cambridge, Cambridge, UK Aims: To assess the impact of chemokine receptor D6 deficiency on the outcome of pregnancy. Introduction: D6, a regulator of chemokine abundance highly expressed by the placenta, has been shown to protect against fetal death induced by bacterial endotoxin or anti-phospholipid antibodies from patients. Methods: We assessed the effect of D6 deletion on perinatal outcomes, postnatal growth, and placental stereology of naturally conceived syngeneic fetuses in unchallenged DBA/1 mice. Results: The lack of D6 caused a highly significant increase in the frequency of stillbirth (10.3% of wild-type pups (n 474) vs 21.3% of D6 deficient pups (n 418); p 0.0001 (χ2 test)) and neonatal death in first 3 wks after birth (16.7% of wild-type pups (n 400) vs 37.0% of D6 deficient pups (n 322); p 0.0001 (χ2 test)), leading to a substantial reduction in mean number of pups successfully weaned per litter (4.2/0.3 wild-type pups/litter (n 80 litters) vs 2.7/0.3 D6 deficient pups/litter (n 75 litters); p 0.0018 (Mann Whitney)). To examine whether the phenotype was related to abnormal placental development, time dated mice were assessed on day 14 and day 18 gestations. Fetal weight but not placental weight was significantly reduced in the D6 deficient mice on day14 (n 44 WT, n 24 D6deficient; p 0.003). Detailed placental stereology of 8 mice per group demonstrated that on day14 the Labyrinthine Zone volume % (LZ) was significantly reduced in the D6 deficient mice (p 0.03), with a concomitant increase in the Junctional Zone volume % (JZ) (p 0.03). LZ was positively associated with fetal weight (r 0.52, p 0.04), with the JZ negatively associated (r 0.5, p 0.05). These differences were not observed on day18. Conclusion: The D6 receptor is critical for normal LZ development and fetal growth, however, late compensatory mechanisms exist to ensure normal fetal weight at term. This initial abnormal placental development may underlie the observed increase in stillbirth and neonatal deaths. A1.5: The effects of gonadotropin stimulation and 2-cell embryo biopsy in mice on embryo quality and blastocyst development PRANAY GHOSH, KIMBERLEY SWANN, BRUCE CAMPBELL & WALID MAALOUF University of Nottingham, Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE] Division of Obstetrics and Gynaecology School of Clinical Science, Nottingham, UK Background: Embryo biopsy is a critical factor that determines success in a preimplantation genetic diagnosis program. The determination of the stage at which blastomeres lose totipotency is an important consideration. Embryonic biopsy at a stage after which the blastomeres exhibit a developmental bias is likely to have an adverse outcome if the blastomere destined to develop into inner cell mass is inadvertently removed. The stress conferred to the preimplantation embryo by the biopsy procedure is manifested in the form of a delay in morphokinetic development, reduction in total cell numbers, and an increased level of apoptotic indices in the blastocyst derived from biopsied embryo. Method: The effect of blastomere biopsy at 2-cell stage was assessed in terms of blastocyst yield, morphokinetic parameters, total cell numbers and the apoptotic cell count in the resulting blastocysts, from embryos obtained naturally or after gonadotropin stimulation. Results: Morphokinetic assessment revealed a significant delay in biopsied embryos reaching the 4-cell, 8-cell and morula stages, as compared to intact controls, but no delay in blastocoel appearance and latter stages. A comparison of morphokinetic characteristics in naturally mated and stimulated groups revealed no significant difference in time taken to reach various developmental checkpoints, and yield plus total cell number of blastocysts obtained were comparable. There was a significant reduction in total cell number following the biopsy at 2-cell stage. Dead cell index was significantly higher in blastocysts obtained from superovulated mice, but was comparable between intact and biopsied embryos in both groups. Conclusion: Embryo biopsy at 2-cell stage does not adversely affect the developmental capacity of the embryo in terms of blastocyst yield or apoptotic stress. This study advances evidence in favour of 2-cell embryonic stage as a possible time to conduct embryonic biopsy in mouse, and provides information that can be useful in future studies employing embryo biopsy for PGD. © 2013 The British Fertility Society e4 Abstracts A1.6: BMP4 induces terminal differentiation of primary trophoblast cells and increases chorionic gonadotrophin secretion AMANDA DE MESTRE, VICTORIA CABRERA-SHARP, STEPHANIE RICHARDSON, ALYCIA KOWALSKI, DOUGLAS ANTCZAK & ABIR MUKHERJEE The Royal Veterinary College, Department of Comparative Biomedical Sciences, University of London, London, UK Objective: Chorionic gonadotrophin (CG) is a hormone induced during terminal differentiation of trophoblast cells that significantly influences pregnancy outcome.The TGFβ superfamily SMAD2/3 pathway regulates placental function but the activity of the alternative pathway through SMAD1/5/8 in the placenta is unknown. This study investigated the role of BMP4 signalling through SMAD1/5 in terminal differentiation of primary chorionic gonadotrophin-secreting trophoblast cells. Methods: A novel equine animal model of trophoblast differentiation was used to gain pure populations of primary CG-secreting trophoblast cells and placental tissue. Chorionic girdle was isolated from day 30–35 equine conceptuses. A 44K gene probe equine expression array and RT-PCR was used to compare Type I and Type II serine/ threonine kinase and accessory receptor expression. Cultured chorionic girdle trophoblast cells were supplemented with 1–100 ng/ml human BMP4. Differentiation was determined following dual-labelling of the cells with CellTrace™ BODIPY® TR methyl ester and Hoeschst. The concentration of eCG was determined using ELISA. Total SMAD2, pSMAD1/5, total SMAD1/5, pSMAD3 and B-ACTIN expression in the placenta was determined using western blotting. Results: CG-secreting trophoblast preferentially expressed receptors ALK3, BMPR-II, Dragon and Bambi that bind the ligand BMP4. Stimulation of chorionic girdle trophoblast cells with 1–100 ng/ml BMP4 resulted in a dose dependent increase in total number and proportion of terminally differentiated binucleate cells (p 0.001) and induced eCG secretion (P 0.01) in a developmental dependent manner. Phospho-SMAD1/5 expression, but not pSMAD2 was tightly regulated during CG-secreting trophoblast differentiation in vivo, with peak expression of pSMAD1/ 5 noted at gestation day 31 corresponding to maximal trophoblast differentiation. Conclusion/relevance: Our findings support a role for TGFb signalling in regulation of differentiation of primary trophoblast cells via BMP4 dependent binding to BMPR-II and ALK3 and activation of SMAD1/5.The observation of BMP4 signalling in primary trophoblast provides a previously unreported mechanism of TGFb signalling in the placenta. A2.1: Levels and localization patterns of protamine 1 (P1) and 2 (P2), essential proteins for sperm head condensation and DNA stability, in fresh and cryopreserved mouse sperm SUSEELA YELUMALAI, CELINE JONES, JUNAID KASHIR, SU LIN OO, MARISA SCHUBERT & KEVIN COWARD Nuffield Department of Obstetrics & Gynaecology, University of Oxford, Level 3,Women’s Centre, John Radcliffe Hospital, Headington, Oxford, OX3 9DU, UK Infertility affects approximately 10% of couples worldwide. While Assisted Reproductive Technology (ART), a suite of sophisticated laboratory techniques, has accounted for the birth of over 8 million babies, success rates rarely exceed 30%. Evidence suggests that some routine ART techniques such as cryopreservation may induce detrimental effects upon critical sperm proteins thus compromising viability and function. Protamine 1 (P1) and 2 (P2) are arginine-rich proteins abundantly expressed in sperm nuclei and play a key role in DNA condensation and stabilization. During the latter stage of mammalian spermatogenesis, P1 and P2 are synthesized in order to replace histone protein during sperm nuclear chromatin packaging. In fertile human sperm, P1/P2 ratio is equivalent to 1.0 or falls between 0.8 and 1.2. Previous immunoblotting experiments have suggested that alterations in P1/P2 ratio may be implicated in male factor infertility. In the present study, a routine sperm swim-out technique was used to obtain the best quality sperm from the cauda epididymi of three age groups of mice (6, 16, and 32 weeks). Quantitative immunocytochemistry utilising monoclonal antibodies was used to investigate total levels and localization patterns of P1 and P2 in swim-out sperm. Findings indicate variation in the total levels of P1 and P2 in the sperm head across all age groups. However, the total level and proportion of sperm exhibiting P1 and P2 increased significantly (p 0.05) in cryopreserved sperm compared to fresh sperm. P1/P2 ratios were also elevated in cryopreserved sperm compared to fresh sperm in an age-dependent manner (6 weeks; 0.7–1.2, 16 weeks; 0.6–0.8, 32 weeks; 1.26–1.29). Collectively, current findings may enable assessment of the potential effect of sperm maturation and male age upon these key sperm proteins in a mouse model, which could later be extended to human sperm. Human Fertility Abstracts e5 A2.2: Chemotherapeutic drug sensitivity in mouse testis NORAH SPEARS, FEDERICA LOPES, HONG XIA BAI, ROD MITCHELL & RICHARD ANDERSON Centre for Integrative Physiology, University of Edinburgh, Edinburgh, United Kingdom; MRC Centre for Reproductive Health, Queens Medical Research Institute, University of Edinburgh, Edinburgh, UK Fertility preservation strategies for prepubertal boys undergoing potentially gonadotoxic cancer therapies remain highly experimental, with limited information available about the effects of chemotherapy agents on prepubertal testes. We have analysed the effects of exposing mouse testicular tissues, in vitro, to two different classes of chemotherapeutic drugs; cisplatin, an alkylating agent inducing cell death by DNA-crosslinking formation, and doxorubicin, an anthracycline DNA-intercalator inhibiting cell replication. Quartered neonatal testes were cultured for five days in αMEM medium with 10% knockout serum replacement, exposed to cisplatin (0.1, 0.5 or 1.0 μg/ml) and doxorubicin (0.02, 0.1 or 0.5 μg/ml) during Day 2 of culture only. Explants were processed histologically and analysed immunohistochemically for mouse vasa homologue (MVH) expression, to allow quantification of germ cells (GCs). At the lowest concentrations of both drugs tested, there was a marked decrease in GCs number despite preservation of normal overall testicular structure: there were (mean sem) 150 34 MVH-positive cells/mm2 tubule area in 0.1 μg/ ml cisplatin-treated testes and 130 30 MVH-positive cells/mm2 tubule area in 0.02 μg/ml doxorubicin-treated testes, compared with 880 94 MVH-positive cells/mm2 tubule area in Control tissues. In contrast, impairment of normal testicular morphology occurred only at the highest drug concentrations, with tissue structure substantially lost and widespread areas of cell death. Mouse ovaries exposed to cisplatin and doxorubicin in vitro displayed different effects, the former damaging primarily oocytes, while the latter damaged granulosa cells (Morgan et al., 2011, DFRO Conference abstract, Edinburgh, UK). The present work suggests that exposure of the pre-pubertal testis to even low doses of cisplatin or doxorubicin primarily affects GCs, probably because testes contains mitotically-active GCs, rendering them sensitive to both drugs, whilst the ovary contains only oocytes in meiotic arrest, thus not directly affected by doxorubicin-induced cell cycle perturbation. Work was supported by MRC grant G1002118. A2.3: Mesoporous silica nanoparticle (MSNP)-mediated delivery to mammalian sperm and oocytes: localisation, viability and loading studies NATALIA BARKALINA, JUNAID KASHIR, CAROLINE DAY, CELINE JONES, HELEN TOWNLEY & KEVIN COWARD Nuffield Department of Obstetrics and Gynaecology, University of Oxford, Level 3,Women’s Centre, John Radcliffe Hospital, Headington, Oxford, OX3 9DU, UK Nanoparticles (NPs) are being increasingly introduced into biomedicine as small-scale multipurpose biological delivery platforms with non-invasive internalisation profiles. Potential exists for the application of NPs as versatile research/ treatment tools to target localised physiological pathways in reproductive tissues and gametes. The aim of the current study was to evaluate the possibility and safety of mesoporous silica nanoparticle (MSNP)-mediated delivery into mammalian gametes. Fluorescent and non-fluorescent MSNPs were synthesised, optionally coated with polyethyleneimine (PEI) and loaded with lamin A/C siRNA. Firstly, fluorescent non-coated/PEI-coated and siRNA-bound MSNPs were applied to boar sperm in a range of concentrations (0.03–0.3 mg/ml) for various exposure times (2–4 hours). Secondly, mouse oocytes were exposed to various concentrations of fluorescent PEI-coated MSNPs (0.003– 0.3 mg/ml). Finally, oocytes were injected with fluorescent non-coated/PEI-coated MSNPs (0.3 mg/ml) alone or with boar sperm previously exposed to the same MSNPs. Imaging was performed using fluorescent and confocal microscopy. MSNPs did not exert any obvious detrimental effect upon boar sperm viability, regardless of surface chemistry, NP concentration, exposure time, and overall semen quality. However, MSNP-sperm association rate, but not the temporal dynamics of sperm-associated MSNP localisation, was highly dependent upon NP surface chemistry. Negative electrokinetic potential significantly increased MSNP-sperm association. Cargo loading onto MSNPs did not alter sperm association profiles, compared to unloaded vehicles. Oocyte exposure to MSNPs resulted in dose-independent attachment of particles to the zona pellucida. Microinjection experiments confirmed the possibility of assisted MSNP delivery through the zona pellucida, however technical modifications are necessary to further improve efficacy. In summary, our current data support the safety of MSNPs as delivery vehicles for reproductive application, and demonstrate highly distinctive MSNP-sperm association profiles that are dependent upon © 2013 The British Fertility Society e6 Abstracts surface chemistry. Future studies will focus upon toxicity, metabolic, and functional ramifications of MSNPmediated delivery. A2.4: CatSper and stored Ca21 control functionally different ‘behaviours’ in human sperm STEPHEN PUBLICOVER, WARDAH ALASMARI, SARAH COSTELLO, JOAO CORREIA, SENGA OXENHAM, LEONOR FERNANDES & JACKSON KIRKMAN-BROWN School of Biosciences and Birmingham Women’s Fertility Centre, University of Birmingham, Edgbaston, Birmingham,UK Within the female tract sperm must use functionally different behaviours at different times. Motility is controlled primarily by [Ca2]i, increased [Ca2]i apparently switching sperm from linear swimming to more complex motility types. CatSper, a pH-regulated channel that is the expressed only in the flagellum of sperm, is believed to be the principal sperm Ca2 channel. CatSper is essential for sperm motility regulation, but stored Ca2 in the sperm neck region may also be important. Using [Ca2]i imaging (Oregon Green BAPTA), fluorescent assessment of pHi (BCECF) and assessment of sperm motility (computer assisted semen analysis, penetration of viscous medium) we have investigated regulation of behavior in human sperm. Exposure to NH4Cl or trimethylamine to raise pHi (0.25– 0.5 units) or stimulation with progesterone (CatSper agonist) caused a sustained increase in [Ca2]i, confirming activation of CatSper. These treatments strongly enhanced penetration into viscous (methylcellulose) medium but had negligible effects on the motility parameters characteristic of hyperactivation. Methylcellulose penetration was inhibited by 10 mM NNC55–0396, which blocks CatSper currents in human sperm. 5 mM thimerosal, which mobilizes stored Ca2, also caused a sustained [Ca2]i rise in human sperm. Thimerosal had no effect on penetration of sperm into methylcellulose but induced robust hyperactivation which was insensitive to NNC55-0396. 2 mM 4-aminopyridine increased pHi by 0.25 units and also caused release of Ca2 from intracellular stores in sperm. 4-aminopyridine both stimulated robust hyperactivation and increased penetration of sperm into methylcellulose, but only methycellulose penetration was inhibited by NNC-0396. We conclude that release of stored Ca2 at the sperm neck is required for hyperactivation (crucial for zona penetration) whereas CatSper activation stimulates more subtle changes, probably in the distal flagellum, that enable penetration into viscous substrates such as mucus. These functionally different components of sperm behaviour may be differentially recruited by stimuli that ‘select’ a Ca2-signalling pathway. A2.5: Modulation of human sperm motility JOAO CORREIA & STEPHEN PUBLICOVER School of Biosciences, University of Birmingham, Edgbaston, Birmingham,UK Approximately 1 in 6 couples have difficulties in conceiving naturally, with male factor being the only cause of infertility in around 30% of these couples and a contributing factor in another 20–30%. Hyperactive motility, characterised by cells displaying very active thrusting, together with high amplitude, asymmetrical flagellar bending, is regarded as crucial for natural conception, but is also important in assisted reproduction. Hyperactivation enables spermatozoa to penetrate the egg vestments, and failure to hyperactivate has been associated with infertile phenotypes in rodents. Current understanding of the signaling events and mechanisms involved in regulating sperm’s transition to and from hyperactivated motility is still very limited, so progress in this area could prove significant in the development of potential pharmacological treatments for male motility-related infertility but also new approaches to contraception. To this effect we employ high-speed high-sensitivity ratiometric Ca2 imaging to monitor [Ca2]i and investigate the effects of motility modulators like 4-aminopyridine, thimerosal and [pH]i on human sperm, and how the neck/midpiece Ca2 store interacts with flagellar CatSper to develop hyperctivated motility. Similarly, we test the effects of rapid uncaging of Ca2 and InsP3 upon UV illumination in both free swimming and loosely-tethered spermatozoa and correlate the resulting changes in [Ca2]i with flagellar activity and different motility patterns. These experiments have revealed that, whereas activation has little effect, release of stored Ca2 is associated with a transition to hyperactivated motility. Localised Ca2 uncaging (using NP-EGTA AM) either in the head or mid-flagellum increased flagellar bending and beat frequency. The uncaging-induced [Ca2]i increase spread rapidly but the kinetics differed according to the uncaging site in a manner consistent with secondary release of stored Ca2 at the sperm neck by Ca2-induced-Ca2-release. Human Fertility Abstracts e7 A3.1: Development, implementation and clinical outcomes of a multiple birth minimisation strategy JENNY SPENCER, NICOLAS VULLIEMOZ, TIM CHILD, ENDA McVEIGH & KAREN TURNER Oxford Fertility, Institute of Reproductive Sciences, Oxford, UK Introduction: Multiple birth constitutes the greatest risk factor in ART. From 2009, in conjunction with HFEA guidelines, our clinic devised a Multiple Birth Minimisation Strategy (MBMS). The strategy has since been modified and the objective of this study was to review ART outcome for patients undergoing fresh embryo transfers. Materials and Methods: 905 fresh cycles from 2008, prior to strategy introduction, and 2563 fresh cycles from 2009 and 2010, during strategy implementation and modification were reviewed. ART outcome for patients undergoing elective single embryo transfer (eSET) and double embryo transfer (DET) were compared. Outcome measures included clinical pregnancy rate (CPR), multiple pregnancy rate (MPR) and live birth rate. Results: In 2009, the initial MBMS was a two-fold approach, with extended culture to blastocyst for all patients with more than 4 good quality embryos on day 3 and eSET for patients 35 years on day 5. Over the first two years this MBMS was successful in reducing MPR and thus MBR. However, in patients 35 to 38 years a significant rise (P 0.05) in MPR and MBR was seen within the first year to 38.3% (51/133) and 32.0% (43/133) respectively. Modification of the strategy to include this age group in selection criteria led to an overall decrease in 2010 of MPR to 16.1% (90/560), and MBR to 13% (74/560), below HFEA targets. CPR remained largely unaffected during strategy implementation. Pregnancy outcomes were also analysed over the three years, showing that reduced gestation length and birth weights and miscarriage (14–24 weeks) were more prevalent in multiple pregnancies. From 2008–2010 Singleton Pregnancy Multiple Pregnancy Miscarriage of 1 FH Gestation 37 weeks Low Birth Weight 2500 g 14 wks 14–19 wks 20–24 wks 90.6% (715/789)∗∗ 52.2% (117/224) 8.8% (70/789)∗∗ 54.9% (123/224) 12.4% (98/789) 12.9% (29/224) 0.5% (4/789) 2.7%∗ (6/224) 0.5% (4/789) 4.0%∗∗ (9/224) ∗P 0.05; ∗∗ P 0.0001. Conclusion: MBMS, combining eSET with blastocyst culture, is an effective method of reducing multiple pregnancies which pose risks of reduced gestation periods, low birth weight and late term miscarriages. Careful monitoring and development of the strategy is required to ensure CPR is maintained, whilst reducing MBR. A3.2: Female genital mutilation: are we meeting the standards of antenatal management MUNAWAR HUSSAIN, CHARLOTTE JONES & JANE BOOTH St Michael’s Hospital & Bristol Centre for Reproductive Medicine Bristol, Bristol University Medical School, Bristol, UK Introduction: In the UK, it is estimated that up to 24,000 girls under the age of 15 are at risk of illegal practice of female genital mutilation (FGM) and 66,000 women are living with its consequences.Antenatal booking is an important time to identify women who have undergone FGM and are properly managed. This audit aimed to determine whether current national and local guidelines for the management of pregnant women who are from high risk area or have undergone FGM are being adhered to. Material and Methods: Retrospective audit of 100 cases for antenatal management of women of Black/African origin over one year period from April 2010–April 2011. Out of these 100 patients, we further analysed the patient who had undergone FGM against and compared their management with national and local guidelines. Results: Out of 100 women from high risk background, 33% had undergone FGM and were interviewed and properly documented in notes. In the remaining 67% women who did not have FGM, only 7% were not interviewed while 60% were not asked about FGM. Majority (94%) of the women with FGM were referred for consultant led care. However, only 9% women with FGM were offered antenatal reversal of FGM while 24% women had already undergone reversal before the index pregnancy. 56% of the women with FGM gave birth to female child but only 39% of these women were advised on child protection issues. Only 40% of women from high risk areas were questioned and remaining 60% were not questioned about FGM at booking. Conclusion: Standards as set out from © 2013 The British Fertility Society e8 Abstracts the current guidelines were not met with. Patients from high risk countries should be identified and questioned about FGM at antenatal booking, referred to a consultant led antenatal clinic care for further assessment and management to minimize any anticipated problems. A3.3: Use of neonatal care (NICU) services after ART: a comparison of singleton and multiple births MUNAWAR HUSSAIN, KATE LIGHTLY, ERIK LENGUERRAND & PETER WARDLE Bristol Centre for Reproductive Medicine, St. Michael’s Hospital Bristol, Southmead Hospital Bristol, Bristol University, Bristol, UK Purpose: Multiple births are the single biggest avoidable health risk of fertility treatments, they deliver premature, have low birth weight and at more risk to be admitted in NICU. The purpose of this study was to compare the perinatal outcome (gestational age, birth weight), level of neonatal care (SCBU, HDU, and ITU) and days spent at different levels of care by babies born after singleton and multiple ART pregnancies. Methods: Retrospective analysis of perinatal and neonatal outcome of ART births in 2007–2008 from a large single HFEA-licensed unit prior to introduction of an elective single embryo transfer (eSET) policy. Data were collected from the ART, maternity and neonatal databases for all live births. Results: 683 babies were born: 415 singleton, 131 twins and 2 triplets. Multiple pregnancies were significantly more likely to be delivered by caesarean section (p 0.0001) than singletons. They were 4 times more likely to deliver at 32 weeks (RR 3.9, 95% CI 1.5–9.9) and 11 times more likely to deliver between 32–36 weeks (RR 11.1, 95% CI 6.1–14.9). Babies from multiple pregnancies were 926 g lighter (p 0.0001, 95% CI 1012– 840), 6 times more likely to deliver 1500 g than singletons. Multiples were admitted in NICU for significantly more days than singletons (median 8 vs. 2, p 0.0001). Even after adjusting for gestational age and birth weight, multiples were still more likely to be admitted in SCBU and ITU (p 0.05) however, unexpectedly singletons still had high rate of admission to NICU (14.2%).Conclusion: The risks of preterm delivery, low birth weight and NICU admission in ART multiple pregnancies confirms the findings of others. The unexpected high admission rate for singleton pregnancies suggests the impact of eSET on NICU resources may not be as great as anticipated. Further studies, after the full introduction of eSET, are planned. A3.4: Should we be freezing embryos? MOHAR GOSWAMI, ERICA HAIMES & ALISON MURDOCH Newcastle Fertility Centre At Life, Policy, Ethics and Life Sciences Research Centre, Newcastle University, Newcastle upon Tyne, UK Aim: Embryo freezing is standard clinical practice, despite sparse evidence of how couples make the decision to freeze their surplus embryos, or of their views at the time of freezing. This study explores this neglected area. The aim of the study is to provide information to both clinicians and patients to be used to provide better support for patients. Methods: This is a qualitative study of couples who have had / 1 IVF treatment. 16 couples were interviewed using a semi-structured questionnaire, followed by thematic analysis and category mapping. Results: Couples expressed ethical conflicts about freezing ‘babies’ and concerns about safety of the freezing process. However, the overwhelming desire to have a baby influenced their decision favouring embryo freezing; seeing it as a ‘part of a process’. Only on reflection were the issues fully considered.Funding issues also influenced their decision making, as the decision to freeze was almost automatic, when funded by the NHS. However when funded privately, the decision was more carefully thought out as the financial costs of freezing, storage and subsequent transfer versus a fresh IVF cycle had to be considered. Despite being given the relevant written information, couples were confused about the practical aspects of embryo freezing, namely: safety, success rates, duration of NHS funding, freezing fees. This confusion suggests that couples were preoccupied with the complexities of immediate treatment, and were less able to process extra information at that point. Nonetheless there was no regret expressed about the decision they made. Conclusion: Desperation for a baby is the dominant drive when considering freezing embryos but, on reflection, couples’ views were nuanced and complex. Although this study indicates that more detailed information may not have influenced their decision, it provides the basis for further study comparing the influence of more targeted information on freezing decisions. Human Fertility Abstracts e9 A3.5: The role of the ‘specialist’ Fertility Nurse in the establishment and maintenance of a service treating patients with known infectious disease SALLY WOOD, GRACE MARSDEN, BIJAL PATEL, STEVE TROUP, CHARLES KINGSLAND & ANDREW DRAKELEY Hewitt Fertility Centre, Liverpool Women’s NHS Foundation Trust, Liverpool, UK Introduction: In June 2009, a purpose-built Isolation Laboratory was opened within a large NHS-funded assisted conception unit enabling fertility treatment of viral-positive patients, whilst reducing risk of transmission to patients, partners and staff. We are situated within close proximity of a Virology Laboratory facilitating requisite and rapid viral testing. The aim of this study was to examine the role of the ‘specialist’ Fertility Nurse in the establishment and ongoing maintenance of this service. Tasks included developing SOPs, effective lines of communication with new and existing referral centres, patient and user information, and staff training. Methods: The tasks undertaken by ‘specialist’ Fertility Nurse(s) associated with this service, together with its activity and efficacy, were examined. Results: Continuity of patient care was facilitated by establishing SOP-driven effective lines of communication with referring centres. From feedback, information packs were greatly received, giving an insight to services provided and treatment pathways. 9, 42 and 91 cycles were performed in the 1st, 2nd and 3rd 12 months of operation, respectively. Referrals were received from 29 PCTs within a 100 mile radius including the Isle of Man and Yorkshire. 57, 49, and 18 couples in which HIV, HepB or HepC was present, respectively, were treated. Clinical pregnancy rates (per embryo transfer) for IVF and ICSI were 10/42(23.8%) and 9/37(24.3%), respectively. 19 IUI cycles resulted in two clinical pregnancies. Discussion: Demand for this rare and highly specialised service is demonstrably increasing; this study has demonstrated a pivotal and varied role for the ‘specialist’ Fertility Nurse(s) in its establishment, growth and maintenance. In addition to more conventional nursing tasks, need for straightforward patient pathways and supporting documentation is essential. It seems appropriate that further expansion of this service be via ‘satellite’ arrangements with ‘specialist’ Fertility Nurse(s) providing uncomplicated interface in a primarily nurse-lead service. A3.6: Supporting emotional well-being – Impacts on Assisted Reproductive Technology (ART) nursing practice JUDITH APPLEGARTH1, TRUDY DWYER2 & LORNA MOXHAM3 1 Monash IVF, Rockhampton, Queensland, Australia, 2Central Queensland University School of Nursing & Midwifery and Institute of Health & Social Science Research, Rockhampton, Queensland, Australia and 3University of Woolongong, School of Nursing, Midwifery and Indigenous Health,Wollongong, NSW, Australia Introduction: The Assisted Reproductive Technology (ART) patient journey has been likened to a roller coaster ride with both physical and emotional highs and lows. Given the key role that ART nurses play as they accompany patients on their journey, it is imperative to understand the issues that impact on practice and potentially contribute to clinical risk. The aim of this study was to explore and understand the clinical practice experiences of ART nurses in Australia. Methods: A qualitative, grounded theory (GT) approach was used. Purposive and later theoretical sampling facilitated recruitment of Registered Nurse (RN) participants. Semi-structured interviews were undertaken with RNs from metropolitan and regional ART units. The constant comparative approach was used in data analysis. Results: One key issue that arose in this study related to the role that ART nurses play in supporting the emotional wellbeing of patients. At times, this support posed a risk to the emotional wellbeing of the nurses. Access to specific education and training emerged as a factor that the ART nurses perceived were crucial to optimise their ability to provide support for the wellbeing of patients as well as themselves. Conclusion: Clinical risk management is a key consideration in all areas of health care. Given that ART nurses play a pivotal role in the co-ordination of the treatment journey it is imperative that strategies are in place to ensure that they have access to support and training to minimise risk to their own wellbeing and maximise patient safety and outcomes. This research contributes a unique perspective to the existing body of knowledge and highlights the complexity of the ART nurse role as well as potential areas of risk. Findings from this research can inform: practice development; quality assurance; and education for ART nurses and are translatable to the global context. © 2013 The British Fertility Society e10 Abstracts A4.1: Heparin treatment for unexplained recurrent implantation failure: empirical use or evidence based? NEELAM POTDAR, JANE BLOWER & TAREK GELBAYA Leicester Fertility Centre, University Hospitals of Leicester, Leicester, UK Introduction: Recurrent implantation failure (RIF) affects 10% of women undergoing assisted reproduction. In women with RIF and confirmed thrombophilia, heparin is used as an adjunct to ART because of its anti-thrombin effect. However, heparin has also been shown to be effective in improving implantation rates without thrombophilias. In this systematic review and meta-analysis we sought to investigate if heparin is effective for treatment of unexplained RIF. Methods: Online search of databases such as MEDLINE, EMBASE, OVID, Cochrane library, ISI Conference Proceedings and ISRCTN Register, from 1980–2012 was performed. The included studies were randomised or prospective non-randomised, where women with previous failed implantation had undergone intervention of heparin compared to the matched control group without use of heparin. Formal meta-analyses were performed using Review Manager 5.1 Software (The Cochrane Collaboration 2000). Random effects models (using the Peto modified Mantel-Haenszel method) were used and results expressed as risk ratio (RR) with 95% confidence interval (CI). Statistical heterogeneity was formally tested. Results: Hundred and five citations were identified, 30 selected initially and finally three were included in the meta-analysis. Total of 440 women participated, in the intervention arm there were 221 women and the pooled RR for clinical pregnancy was 1.26 (95% CI 0.83, 1.91, P 0.2). For the live birth rate the pooled RR was 1.32 (95% CI 0.97, 1.80, P 0.08). There was moderate statistical heterogeneity between the studies (I2 52%). Only one study reported implantation rate with RR of 3.42 (95% CI 1.62, 7.20, P 0.001). Conclusion: Although, RIF is associated with immense emotional and financial trauma, there is no significant evidence that heparin as an adjunct to ART, in absence of thrombophilia’s, will enhance implantation and subsequent live birth rates. There is emerging scientific evidence that heparin helps with decidualisation and implantation process and large multi-centered randomized studies are required to answer this important question. A4.2: Transforming growth factor-β family regulation of inhibitor of differentiation proteins in the peritoneal mesothelium: a potential explanation for the aetiology of endometriosis VICKY JANE YOUNG, JEREMY BROWN, CHRISTOPHER HARLOW, ALAN MCNEILLY, W. COLIN DUNCAN & ANDREW HORNE MRC Centre for Reproductive Health, The University of Edinburgh, The Queen’s Medical Research Institute, Edinburgh, UK Endometriosis is a major socioeconomic burden due to its association with pelvic pain and infertility. It is defined by the presence of endometrium outside the uterus, most commonly on the pelvic peritoneum. Its aetiology is uncertain but it is likely that the transforming growth factor-β (TGF-β) superfamily plays a major role. Indeed TGF-β1 is increased in the peritoneal fluid of women with endometriosis. Inhibitor of differentiation (Id) proteins are negative regulators of basic HLH transcription factors that regulate cell proliferation, cell invasion, cell differentiation and angiogenesis, all of which may have an aetiological role in endometriosis. Importantly they are transcriptional targets of some members of the TGF-β family through the smad pathway. We aimed to characterise TGFβ-superfamily and Id expression in the pelvic peritoneum of women with/without endometriosis and to measure the effect of TGFβsuperfamily signalling on downstream Id gene expression in peritoneal mesothelial cells. Peritoneal biopsies and peritoneal mesothelial cells were collected with informed consent from women with and without endometriosis at laparoscopy (LREC 11/AL/0376). TGF-β superfamily and Id 1–4 expression was measured in peritoneal biopsies from women with and without endometriosis by qRT-PCR (n 5) and immunohistochemistry (n 4). The effect of TGF-b1 on Id gene expression was assessed in the peritoneal mesothelial cells (n 6). Alk receptors, phospho-smad 1, 2/3, 5 and 7, and Ids 1–4 were all expressed in pelvic peritoneum from women with and without endometriosis. Exposure of primary peritoneal mesothelial cells to physiological concentrations of TGF-β1 increased Id1 and Id3 gene expression in 50% of samples (p 0.05). Our data suggest that TGF-β1 and the Id pathway are active in the peritoneal mesothelium. Further studies are required to determine whether they play a role in the modulation of cell proliferation, invasion and angiogenesis in the peritoneum, pathological events associated with the development of endometriosis. Human Fertility Abstracts e11 A4.3: Follicular fluid cytokine dynamics in natural cycles N. ELLISSA BASKIND, VINAY SHARMA, NICOLAS ORSI & NIGEL SIMPSON Leeds Centre for Reproductive Medicine, Leeds Teaching Hosptals NHS Trust; University of Leeds, Leeds, UK Aims: Oocyte to ovarian somatic cell bi-directional communication is mediated by multiple cytokines and growth factors. During the course of folliculo- and oogenesis, cytokines participate in regulating oocyte’s growth, vasculogenesis and steroid synthesis. This study aimed to characterise their dynamic changes in follicular fluid (FF) throughout the follicular phase of natural cycles and to ascertain whether these reflected oocyte maturity, fertilization potential and embryo viability. Methods: 10 women requiring IVF/IVF-ICSI for unexplained subfertility/male factor infertility aged 25–35 years with normal BMI and pelvis were recruited to undergo FF aspiration over two cycles. Blood sampling occurred in parallel. In the 1st cycle, dominant follicle was aspirated during the mid-follicular phase or after the LH surge. In the 2nd cycle, all patients underwent natural cycle IVF/IVF-ICSI after hCG administration at 17–18mm and clear catch FF was collected under ultrasound guidance. All FFs and plasma samples were analysed for cytokine profiles (vascular endothelial growth factor (VEGF), interleukin (IL)-1 receptor antagonist (ra), IL-6 and IL-8) by multiplex immunoassay. Data were analysed by paired t-test, Wilcoxon test and logistic regression analysis. Results: FF VEGF and IL-1ra levels were significantly higher in the mid-follicular than in the peri-ovulatory phase (P 0.05), a pattern reflected in plasma VEGF concentration. By contrast, IL-6 and IL-8 were significantly higher in the peri-ovulatory phase (P 0.05). Approximately 78% of oocytes retrieved were in metaphase II, fertilized successfully and embryos were transferred. Two women achieved viable pregnancies at 7 weeks’ gestation. We could not demonstrate a correlation between pre-ovulatory cytokine levels and oocyte developmental potential as measured by oocyte maturity, fertilization or implantation rate. Conclusions: The micro-environment of the dominant follicle accommodates the needs of the maturing oocyte in a very complex and dynamic manner. VEGF increases perifollicular vascularity and, in turn, oxygen, hormone and nutrient provision for the oocyte and its supporting somatic cells. IL-1ra may inhibit IL-1α/β in the mid-follicular phase, thereby permitting pre-ovulatory cytoplasmic maturation and preventing follicular wall degeneration. In this study however the pre-ovulatory cytokines did not correlate with oocyte quality. A4.4: The ex vivo effect of uterine fibroids on prostaglandins in menorrhagic women DEBBIE FISCHER1, JOANNE GARVIN2, DIANE FARRAR3, PETER O’DONOVAN3, DAVID WOODWARD2 & KAY MARSHALL2 1 School of Pharmacy and Pharmaceutical Sciences, University of Manchester; Manchester, UK, 2University of Bradford, Bradford, UK and 3Bradford Royal Infirmary, Bradford, UK Uterine fibroids have been associated with treatment failure and subfertility in women diagnosed with menorrhagia (excessive menstrual blood loss). To elucidate their pathology, prostaglandin (PG) profiles, PG receptor function and angiogenic processes were investigated in isolated myometrium from non-pregnant menorrhagic women with (n 8) or without (n 14) uterine fibroids. Approval for this study was granted by the Local Regional Ethics Committees. To quantify endogenous PGs, myometrial and endometrial biopsies were semi-purified and extracts were then analysed using liquid chromatography coupled with ionisation mass spectrometry (Nicolaou & Masoodi, 2006). For functional studies, myometrial strips were attached to isometric force transducers under physiological conditions. Following tissue equilibration, myogenic responses to vehicle (saline), PGE2 (10-10M to 10-5M) and PGF2α (10-9M to 10-5M) were measured. Treatment effects were also evaluated using the in vitro human umbilical vein endothelial cell (HUVEC) angiogenesis model (Rae et al., 2009). Results were expressed as means S.E.M and were analysed using the Mann-Whitney U or multivariate ANOVA with Bonferroni’s post hoc test. PGD2, 6-keto-PGF1α, PGE2, PGF2α and TXB2 production were attenuated in myometrial samples found to contain fibroids compared to those without (p 0.05). A similar trend was observed with the principal output of PGE2 and PGF2α in endometrial tissues. Compared to vehicle controls, PGE2 suppressed (p 0.001), whilst PGF2α enhanced (p 0.01) the amplitude and frequency of contractions; responsiveness to PGs was not influenced by underlying fibroids. Moreover, PGE2 and PGF2α had no effect on blood vessel formation. These findings show that when fibroids exist, PG metabolism was reduced. This may indicate why treatment with non-steroidal anti-inflammatory drugs (NSAIDs) is more effective in menorrhagic women without a secondary pathology (Makarainen & Ylikorkala, 1986). Since PGE2 and PGF2α did © 2013 The British Fertility Society e12 Abstracts not modulate myometrial function or the vasculature, targeting alternative pathways may improve the management of menorrhagia in women with fibroids. A4.5: Essure® for management of hydrosalpinges prior to IVF – A systematic review and pooled analysis PUNEET ARORA1 & DAVID CAHILL2 1 Department of Reproductive Medicine, St Mary’s Hospital, Manchester, UK and 2Department of Obstetrics and Gynaecology, St Michael’s Hospital, Bristol, UK Introduction: Hydrosalpinges in infertile women reduce the success of in-vitro fertilisation (IVF) by 50%. Surgical management of hydrosalpinges by laparoscopic salpingectomy and laparoscopic tubal clipping prior to IVF improves outcome but these procedures are contraindicated or more complex in women with dense pelvic adhesions. Tubal occlusion achieved by Essure® via hysteroscopy provides an alternative. We present a systematic review and pooled analysis of the use of Essure® in the management of hydrosalpinges prior to IVF. Methods: A search of published and grey literature was done. Based on defined criteria, the literature was screened for eligible studies. Data were extracted from the selected studies and pooled to give a summary statistic for each outcomes. Results: Ten studies (2 single case reports and 8 case series) were included. 110 women (median 10 women per study, range 1 to 26) received Essure®, mainly for management of hydrosalpinges because of prior pelvic adhesions. Outpatient setting with use of local anaesthesia by paracervical block and/or intravenous sedation was most commonly used. Successful placement of Essure® was achieved in 96% of women and tubal occlusion was confirmed in 98% of those where successful placement was achieved. IVF subsequent to Essure® resulted in pregnancy rate of 48.4%, live birth rate of 35.5% and a combined ongoing pregnancy and live birth rate of 37.6% per embryo transfer. Conclusions: This systematic review shows the potential for Essure® as an effective option for management of hydrosalpinx in women prior to IVF if other operative treatment options are limited by presence of pelvic adhesions. A controlled clinical trial, measuring IVF outcomes, adverse effects, patient experience and cost effectiveness would provide a more definitive answer to the role of Essure® in those with hydrosalpinx but without pelvic adhesions. A5.1: Anti-Mullerian hormone, polycystic ovarian morphology and polycystic ovary syndrome: A prospective cohort study ROY HOMBURG, ARPITA RAY, PRIYA BHIDE, AMIT SHAH, ANIL GUDI, PETER TIMMS & KATE GRAYSON Homerton Fertility Centre, Homerton University Hospital, London, UK The number of small follicles in the polycystic ovary may play a key role in the pathophysiology of polycystic ovary syndrome (PCOS) and determine severity of symptoms. Whereas 20% of the female population of fertile age have polycystic ovarian morphology (PCOM) on ultrasound examination, only 5–8% suffer from symptoms. Serum antiMullerian hormone (AMH) concentrations reflect the number of small antral follicles in the ovaries. The aims of this study, utilising the measurement of AMH, were 1. To define the place of PCOM alone in the hierarchy of the syndrome, 2. To investigate the relationship of AMH and gonadotrophin concentrations and 3. To clarify the role of AMH as a diagnostic aid. AMH was determined in 234 women; 96 with PCOS (Rotterdamcriteria), 35 with PCOM alone and 103 with normal ovaries using the Beckman Coulter Gen II assay. AMH values clearly distinguished between PCOS (mean 77.6 pmol/l, 95% CI 64.8–90.3), PCOM (52.5 pmol/l, [40.1–64.2]) and controls (22.8 pmol/l, [19.2– 26.4]). Analysis of covariance controlling for age confirmed that all groups were significantly differentiated from each other (P 0.001). LH concentrations were significantly lower in controls and PCOM than in PCOS and FSH was similar in PCOM and PCOS but significantly lower than in controls. Employing an ROC curve (AUC 0.81), an AMH of 48 pmol/l had a sensitivity of 60% and specificity of 98.2% for the diagnosis of PCOS. Adding LH 6IU/ l would predict 82.6% of the women with PCOS. In summary, AMH can distinguish between PCOM and PCOS strengthening the notion that PCOM is a precursor of PCOS and not merely a variation of normal ovarian morphology and illustrating that AMH levels reflect the severity of the syndrome. Whereas the place of AMH as a diagnostic aid for PCOS has yet to be settled, the role of AMH in the anovulation of PCOS may involve the inverse relationship found between AMH and FSH. Human Fertility Abstracts e13 A5.2: Stability and reproducibility of AMH measurements in blood and avoidance of proteolytic changes CRAIG FAIRBURN, CATHERINE BLANEY, DOROTHY LUCAS, MARCO GAUDOIN & RICHARD FLEMING Glasgow Centre for Reproductive Medicine, Glasgow, UK Aims & Objectives: Serum anti-Mullerian hormone (AMH) measurement is established as a predictor of response to ovarian stimulation and guide to appropriate controlled ovarian stimulation. Early assays suffered from sample instability, but the modern assay is stable in separated serum. The assay has not been tested for stability when the sample is stored as whole blood for appreciable amounts of time, as in a postal service. The aim of this study was to examine the effect of storage of blood samples under different conditions. Methods: Blood samples were collected in duplicate into red-topped Vacutainer tubes (clotted, whole blood samples) from women undergoing investigations for infertility treatment. Control samples were centrifuged within 5 hours of collection and assayed the following morning (T0) using the AMH Gen II ELISA assay [Beckman Coulter Ltd]. Study samples were assayed under varying storage conditions. Further samples were collected into gold-topped Vacutainers with a gel separator (clotted, serum samples). They were centrifuged simultaneously with controls, but were then stored at room temperature, with agitation for 5 days and then refrigerated for 2 days (to mimic a postal service). Results: Storage of whole blood at 4°C resulted in modest increases in AMH over 5 days ( 12%). Storage at 20°C resulted in increases that were time-dependent: 11% at 24 hours and 31% after 5 days (P 0.001). When samples were stored at 20°C in the gold-topped Vacutainers and centrifuged, there was no significant change in AMH at 7 days ( 1%). Discussion: The increase in AMH concentration was temperature- and time-dependent and required contact with blood cells, indicating an enzymatic (proteolytic) phenomenon. This has implications for postal assay services. Removal from contact with red cells within a few hours obviated this phenomenon. We recommend that clinics using AMH should handle the samples accordingly but, thereafter, the assay can be performed remotely with no additional storage requirements. A5.3: AMH – A Rationing Tool for Funded Assisted Conception Treatment? KIRSTY BRIGGS1 & ISHOLA AGBAJE2 1 Ulster Hospital, Upper Newtonards Road, Dundonal, Belfast, Northern Ireland and 2Regional Fertility Centre, Royal Victoria Hospital, Grosvenor Road, Belfast, Northern Ireland Background: The value of AMH is becoming increasingly established in assisted conception cycles. Whilst it has a clear role in identifying patients at risk of either an excessive or suboptimal response to controlled ovarian stimulation1, there is less evidence regarding a threshold below which patients should not be offered treatment. With the introduction of an AMH assay into our unit, we wished to explore whether an absolute cut-off value should be applied, below which patients should not be offered NHS funded treatment. Method: All women with an AMH 4 pmol/L were identified over a 12 month period from 1st April 2011 to 31st March 2012 in the Regional Fertility Centre, Belfast. Treatment outcomes were evaluated in those who had undergone IVF/ICSI treatment. Results: Forty-two patients had an AMH of 4 pmol/L. Median age was 37 yrs (IQR 34–39). Three patients elected not to pursue treatment. The median AMH was 2.5 pmol/L (IQR 1.6–3.2) with an FSH of 7.2 U/L (IQR 5.5–9.4). All patients underwent a conventional long agonist protocol. Median total gonadotrophin dosage was 2625IU (IQR 2231–3675). Seven patients (16.7%) had failed stimulation. The median number of eggs retrieved was 3 (IQR 1–4.5). Median fertilization rates were 50% (IQR 0–80). There were 5 biochemical pregnancies (11.9%) resulting in three clinical pregnancies and two miscarriages. Median AMH in those who got pregnant was 2.6 (IQR 1.9–4). Conclusion: The pregnancy rate in women with a low AMH is poor. However, caution should be exercised when using AMH estimation to decide if a patient should be offered NHS funded treatment. In our study, there is insufficient evidence to advocate its use as a rationing tool for NHS funded treatment. Reference Nelson S, Yates R, Fleming R. Serum anti-müllerian hormone and FSH:prediction of live birth abd extremes of response in stimulated cyclesimplications for individualisation of therapy. Human Reproduciton 2007;22(2414–2421). © 2013 The British Fertility Society e14 Abstracts A5.4: A comparison of Anti-Müllerian hormone (AMH) levels and treatment outcomes in South Asian and Caucasian women undergoing in vitro fertilization (IVF) SHIVA KUKREJA, VIRGINIA BECKETT & THOMAS TANG Reproductive Medicine Unit, Bradford Royal Infirmary, Smith Lane, Bradford, UK Aim: AMH has emerged as an effective tool in predicting ovarian response to controlled stimulation in assisted conception cycles. While many studies have suggested less favourable IVF outcomes in women of South Asian origin, little is known about variations in AMH levels in different ethnic groups. Our IVF Unit is based in a city with a diverse ethnicity. Approximately half of the women being treated are of South Asian origin, providing an ideal opportunity to assess differences in AMH levels and IVF outcomes. Method: A retrospective audit conducted in 2012. Information was obtained from the unit database and patient records. Results: In a 6 month period, 42 South Asian and 37 Caucasian women underwent a first cycle of IVF treatment. There were no differences in mean age (33.3 vs 31.5 years) and mean AMH levels (19.0 vs 14.8 pmol/l). All patients had a body mass index (BMI) less than 30 kg/m2. Despite a higher incidence of polycystic ovary syndrome in the South Asian population, the proportion of women with AMH levels over 30 pmol/l was not significantly different from Caucasian population. The mean oocyte retrieved was higher in the South Asian women (10.3 vs 7.9); however, the pregnancy rate was lower than the Caucasian population (23 vs 41%). Due to a low sample size, these findings were not statistically significant. Conclusion: In keeping with previous reports, IVF treatment success is lower among South Asian women compared with Caucasian women despite similar AMH concentrations and age range. We plan a prospective project to look at demographic details like consanguinity and ability to understand English. In addition, nutritional difference between the two populations warrants further research. A5.5: Are BMI, age, FSH and AMH good markers of spontaneous conception in infertile women? ORIANE CHAUSIAUX, RUTENDO GANYANI & SHARON MORRIS Cambridge Temperature Concepts Ltd, Cambridge Science Park, Cambridge, UK This is a prospective study looking at the pregnancy and live birth rates in a group of 200 infertile women. Women involved in this study were diagnosed as infertile, usually with mild infertility or unexplained infertility and they were trying to conceive naturally. In the UK, some markers are used to determine the likely success rate of an IVF/ICSI cycle for a given couple. These factors include the age of the woman, her ovarian reserve (assessed by FSH or AMH) and her BMI. Do any of these markers provide women looking at natural pregnancy additional information on their likelihood of a live birth? Using the woman’s age, it is possible to predict the pregnancy rate and live birth rate from natural conception. Our data suggest that BMI is not a marker which affect pregnancy or live birth rate for our group of patients. Additionally, the use of FSH as a marker of ovarian reserve does not improve either the predicted pregnancy or live birth rate. However the other marker of ovarian reserve, AMH, gives additional information on pregnancy and miscarriage rate above using just the woman’s age. A low AMH ( 7 pmol/L) appears to be linked with a 3% increase in miscarriage rate, and a high AMH ( 21 pmol/L) appears to be linked to an increased pregnancy (9%) and miscarriage rate resulting in an unchanged live birth rate. This study indicates that BMI and FSH are not useful markers for infertile women looking at natural conception. AMH on the other hand can provide additional information above the use of the woman’s age alone. The woman’s age is by far the most important factor when looking at pregnancy and live birth rate linked to spontaneous conception for infertile women. More data is needed, however our initial data suggest that the woman’s age alone is sufficient when counselling patients on their likely outcome with spontaneous conception. Human Fertility Abstracts e15 A5.6: The effect of age, AMH level and treatment type on early embryo development assessed using time-lapse imaging LAUREN WALLACE, A. BARRIE, K. SCHNAUFFER, C. KINGSLAND & S. TROUP The Hewitt Fertility Centre, Liverpool Women’s Hospital, Liverpool, UK Introduction: The introduction of time-lapse imaging into an embryology laboratory setting has facilitated the collection of accurate data regarding cell division timings, data which remains unknown for embryos cultured in standard incubators. As such it is now possible to examine factors which may influence early embryo development. The aim of this study was to examine the effects of maternal age, AMH level and treatment type on the timings of early embryo development. Method: Data were collected using the EmbryoScope™ for 185 embryos transferred (August 2011–August 2012). For each embryo the time spent at the two-cell, three-cell and four-cell stages was calculated. The corresponding treatment type (IVF or ICSI), maternal age, and the AMH value were compared with duration of time between cell divisions. Data regarding age/AMH and treatment type were analysed using a Kruskal-Wallis and Mann-Whitney U tests, respectively. Differences were considered significant when p 0.05. Results: With regard to maternal age, the duration of time spent transitioning between 4–5 cells was found to be significantly less (p 0.019) with reduced age, with embryos from younger patients spending 2.1 hrs less at the 4-cell stage than those from older patients. Embryos from patients who had undergone treatment by ICSI spent 1.6 hrs less (p 0.033) at the 4-cell stage than those from patients treated with IVF. No significant differences were observed in relation to the effect of AMH on early embryo development, although a trend reflecting the effect of patient age was observed. Conclusion: These data would suggest that the developmental pattern of early embryos varies according to age and treatment type, and these observations may be related to the inherent deterioration in egg quality with age and infertility cause. It may also be prudent to consider these findings when attempting to develop embryo selection algorithms using time-lapse imaging. B1.1: A non invasive time-lapse model to classify the risk of aneuploidy in embryos ALISON CAMPBELL1, CRISTINA FONTES LINDEMANN HICKMAN2, SAMANTHA DUFFY3, NATALIE BOWMAN3, MARK SEDLER3, & SIMON FISHEL1 1 Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK, 2Trinidad & Tobago IVF, Trinidad and Tobago and Care Fertility Manchester,Victoria Park, Manchester, UK 3 Ploidy screening of embryos during IVF provides opportunity for clinics to selectively transfer euploid embryo(s). Utilising the EmbryoScopeTM, we hypothesized that rates and patterns of development differed between aneuploid and euploid embryos. Ploidy (Euploid, Single and Multiple Aneuploid) of 98 blastocysts was determined either through whole genome amplification and comparative genomic hybridisation arrays (Genesis Genetics Europe, Nottingham, n 37) or single nucleotide polymorphism arrays with parental supportTM (Natera, California, n 61). Following ICSI, oocytes were cultured in the EmbryoScopeTM. Assessed variables included time, in hours post insemination (hpi), for pronulcer fading, cell divisions to two, three, five-cells, start of compaction (tSC), morula formation, start of blastulation (tSB), full blastocyst formation (tB), expansion and hatching, duration of the second and third cell cycles, synchrony of second and third cell cycles, duration of blastulation, incidence of multinucleation at two and four-cells and irregular cleavage from one to three and two to five cells. Significance was determined either by Mann-Whitney-Wilcoxon (morphokinetic variables) or Fishers (incidence of multinuclearity and irregular cleavage) test. Euploid and aneuploid embryos developed at similar rates until tSC, although multiple aneuploid embryos had significantly delayed tSC (Median 85.1 hpi, p 0.04) and tB (Median 110.4 hpi, p 0.03) compared to euploid embryos (tSC Median 79.2, tB Median 104.5 hpi). Single (Median 102.9 hpi, n 30, p 0.007) and multiple (Median 101.4 hpi, n 30, p 0.03) aneuploid embryos had significantly delayed tSB compared to euploid (Median 95.1 hpi, n 38) embryos. Other variables assessed were not significantly affected by ploidy.Our classification model (area under the ROC curve 0.72) for ploidy prediction (low, medium, high risk of aneuploidy) suggests that time-lapse monitoring may be used to exclude embryos with high risk and select embryos with a reduced risk of aneuploidy. Retrospective analysis of the model on non-PGS blastocysts will be presented with its proposed clinical application. © 2013 The British Fertility Society e16 Abstracts B1.2: Does the timing and degree of cleavage stage embryo fragmentation differ in Euploid and Aneuploid Embryos? SUE MONTGOMERY, SAM DUFFY, NATALIE BOWMAN, MARK SEDLER, ALISON CAMPBELL & SIMON FISHEL Care Fertility Manchester,Victoria Park, Manchester, UK The presence of embryo fragmentation has been shown to affect embryo development and ability to undergo blastocyst formation (Alikani et al, 2000). The introduction of time lapse technology into the IVF laboratory has facilitated the ability to study embryo development in greater detail and to retrospectively analyse and compare embryo development and fragmentation for embryos that reach blastocyst to those that do not. Using the EmbryoScopeTM (Unisense Fertilitech, Denmark) and array CGH it has been possible to compare the level and timing that fragmentation occurs in cleavage stage embryos that have continued to develop to the blastocyst stage, with ploidy outcome. In the 105 embryos studied, there was no significant difference found in the average percentage of fragmentation observed at the 4 and 8 cell stage in euploid (n 41) and aneuploid (n 64) blastocysts at 9.3% and 9.84% for 4 cells and 11.9% and 11.12% for 8 cells, respectively. There was also no significant difference in the average exact time that fragmentation first occurred at 26.87 and 28.82 hours post insemination, for those later tested as euploid and aneuploid. These results show that it is not possible to distinguish euploid and aneuploid embryos by timing and degree of early fragmentation alone, however, the EmbryoScope has also facilitated the study of whether the patterns of fragmentation I–IV first described by Alikani et al, differ according to ploidy status. To assess this, the pattern of fragmentation will be considered and videos of embryos categorized as type I–IV fragmentation (Alikani et al. 1999) blind to the ploidy status. These results will also be presented. References Alikani, M., Cohen, J., Tomkin, G., Garrisi, G.J., Mack, C. and Scott, R.T. (1999). Human embryo fragmentation in vitro and its implications for pregnancy and implantation. Fertil. Steril. 71 (5): 836–842. Alikani, M., Calderon, G., Tomkin, G., Garrisi, J., Kokot, M. and Cohen, J. (2000). Cleavage anomalies in early human embryos and survival after prolonged culture in vitro. Human Reprod. 15: 2634–2643. B1.3: Validation and clinical application of next generation sequencing for embryo screening: first pregnancy heralds a potential revolution in embryo selection DAGAN WELLS1,2, KULVINDER KAUR3, ALAIN RICO4, JAMIE GRIFO5, TYL TAYLOR & SANTIAGO MUNNE6 1 Nuffield Department of Obstetrics and Gynaecology, University of Oxford, Oxford, UK, 2Reprogenetics UK, Institute of Reproductive Sciences, Oxford, UK, 3The Wellcome Trust Centre for Human Genetics, Roosevelt Drive, Oxford, UK, 4 Life Technologies, Life Technologies France SAS, 25 av de la baltique, B. P. 96, 91943 Courtaboeuf Cedex 3, France, 5 NYU Fertility Center, NYU Langone Medical Center, New York, NY, USA and 6Reprogenetics, Livingston, NJ, USA Objective: Next generation sequencing (NGS), a class of methods involving the production of vast quantities of DNA sequence data, is revolutionising genetic diagnostics. However, NGS has not been applied to research or diagnostics involving human embryos due to technical obstacles that prevent analysis single cells. We aimed to create new methods overcoming these limitations, allowing clinical application of NGS technology for the identification of viable/ healthy embryos. Methods: Whole genome amplification and NGS (Ion Torrent) methods were optimised. Data was analysed with novel tools developed by our laboratory. Results: In pre-clinical work, NGS correctly diagnosed abnormalities in 100% of single cells isolated from aneuploid cell lines. Additionally, 45/45 aneuploid embryos donated for research were also successfully diagnosed (verified by blinded analysis using arrayCGH). NGS accurately detected single gene disorders, correctly diagnosing cystic fibrosis in single cells from an affected individual. Moreover, a mitochondrial DNA mutation was successfully detected and accurately quantified in single fibroblasts from a heteroplasmic patient with mitochondrial disease. Ultimately, NGS was employed clinically for the purpose of selecting chromosomally normal blastocysts for uterine transfer, resulting in a pregnancy. Conclusions: A powerful NGS technique applicable to single cells was successfully developed, allowing simultaneous testing for Human Fertility Abstracts e17 aneuploidy, single gene mutations and mitochondrial disease with exceptional accuracy. NGS also provided a DNA fingerprint for the sample, assisting embryo identification. It was possible to complete NGS analysis in a timescale compatible with a fresh embryo transfer. Furthermore, the cost was significantly less than existing methods for embryo testing, suggesting this approach may ultimately bring preimplantation diagnosis for serious genetic disorders within the reach of a much larger number of patients. Following rigorous pre-clinical validation, the novel protocol was applied clinically, resulting in a healthy ongoing pregnancy. This represents the first report detailing a pregnancy achieved after using an NGS-based embryo screening protocol. B1.4: The effect of aneuploidy on embryo morphology and preimplantation development from the cleavage to the blastocyst stage SAMER ALFARAWATI1,2, MAURIZIO POLI1, DAGAN WELLS1,2 & ELPIDA FRAGOULI1,2 1 Nuffield department of Obstetrics and Gynaecology, University of Oxford, UK and 2Reprogenetics UK, Institute of Reproductive Sciences, Oxford, UK Objective: Chromosome abnormality might have an adverse effect on various embryo characteristics including morphology. This study involved a detailed investigation of the impact of aneuploidy on embryo morphology at different developmental stages. The copy numbers of all 24 chromosomes were evaluated. Material and Methods: 1255 embryos generated from 229 patients (average maternal age 39 years) were investigated. Embryo morphology was assessed and recorded on days 3 and/or 5–6 post-fertilization and comprehensive chromosome analysis was carried out using microarray comparative genomic hybridisation (aCGH). Results: At the cleavage stage aneuploidy was common in better grade embryos typically chosen for transfer (grade 1–3) (80% affected) while an over-representation of aneuploidy was observed in embryos with worst quality which are rarely chosen for transfer (96% abnormal). The majority (51%) of the best quality blastocysts were euploid and the number of euploid embryos decreased with declined embryo quality. 19% of blastocysts affected by aneuploidies compatible with a clinical pregnancy had the best morphological quality (trisomy 13, 16, 18, 21, 22, X0, or XXY), whereas only 12% carrying errors non-compatible with pregnancies had the best quality. 59% of cleavage stage embryos and 51% of blastocysts were females and 41% and 49% were males. However, amongst the fastest growing cleavage-stage embryos ( 10 cells) 72% were female, while the opposite was noted for rapidly developing blastocysts (grade 5 or 6; 55% males). Conclusion: A weak association was observed between aneuploidy and morphology at the blastocyst stage, but not earlier in development. At the cleavage-stage complex abnormalities were observed in all grades, whereas this was only seen in ‘early’ blastocysts (P 0.0001). The morphology of abnormal blastocysts capable of implanting was similar to that of euploid embryos. This is in agreement with the fact that such aneuploid conceptions are capable of implanting and sometimes lead to clinical pregnancies and/or miscarriages. B1.5: The origin and impact of embryonic aneuploidy ELPIDA FRAGOULI1,2, SAMER ALFARAWATI1,2, KATHARINA SPATH2, SOURAYA JAROUDI1, JONAS SARASA1, MARIA ENCISO2 & DAGAN WELLS1,2 1 Reprogenetics UK, Institute of Reproductive Sciences, Oxford, UK and 2Nuffield department of Obstetrics and Gynaecology, University of Oxford, UK Objective: Chromosome abnormalities negatively affect natural conceptions, as well those derived from IVF cycles, in most cases leading to implantation failure or miscarriage. Despite the clinical importance of aneuploidy, little is known concerning its effects on preimplantation development. We aimed to shed light on the genesis, progression and survival of different chromosome errors during progression from zygote to blastocyst. The most appropriate stage for preimplantation genetic screening (PGS) was also considered. Methods: 2,204 embryos at three different preimplantation development stages (zygote, cleavage, blastocyst) were examined using comprehensive chromosome screening methodology. These embryos were generated by 396 couples (average female age: 40 years). Results: Progression from zygote to blastocyst was associated with a decline in aneuploidy (72% to 57.6%; P 0.0001), with embryos affected by multiple errors (complex abnormal) decreasing from 22% to 7% (P 0.0001). At the cleavage stage however, both the aneuploidy rate and the proportion of complex abnormal embryos increased (to 82% [P 0.001] and to 37% [P 0.0001] respectively). For all preimplantation stages examined, rates of simple and complex aneuploidy increased as female age advanced. Advancing age was also associated with a disproportionate increase in the frequency of © 2013 The British Fertility Society e18 Abstracts chromosome losses compared with gains at the cleavage and blastocyst stages. Conclusions: Aneuploidy had little effect upon development until after embryonic genome activation. A generalised decline in the fidelity of the chromosome segregation machinery was observed with advancing female age. The elevated frequency of anaphase lag with advancing female age noted post-zygotically is suggestive of a previously unrecognised affect of age on mitotic chromosome segregation, which may be clinically important. Most aneuploidies persisted to the blastocyst stage, although survival rates varied depending on the chromosome involved. We speculate that cytogenetic testing at the blastocyst stage provides the most accurate chromosome constitution prediction and should be the preferred PGS strategy. B1.6: The use of innovative, intelligent software and non-invasive embryo imaging to predict blastocyst formation by day 3 HANNAH MARSDEN1, JOE CONAGHAN2, KRISTEN IVANI3, R. GREGOIRE1, CHARLES KINGSLAND1 & STEPHEN TROUP1 1 Hewitt Fertility Centre, Liverpool Women’s NHS Foundation Trust, Liverpool, UK, 2Pacific Fertility Centre, San Francisco, California, USA and 3Reproductive Science Center of the Bay Area, San Francisco, California, USA Introduction: Early cell cycle timings have been previously correlated with blastocyst formation (BF) and gene expression. Using unique software alongside dark field microscopy, the Eeva™ (Early Embryo Viability Assessment) test (Auxogyn, Menlo Park, CA) tracks the division of each blastomere without requiring manual analysis. On the morning of day 3, Eeva gives a prediction of BF by utilising information regarding P2 (time between cytokinesis 1 and 2) and P3 (time between cytokinesis 2 and 3). This study aims to prospectively assess the performance of Eeva in multiple IVF laboratories. Methods: Eeva was utilised for IVF/ICSI cycles taking place between July and September 2012 at our centre and two further centres in the USA, and its performance assessed. Each centre followed its own stimulation protocols. BF predictions made by Eeva on day 3 were compared to morphological outcomes from day 5 embryos. Results: A total of 298 embryos from 30 patients were included for analysis. The Eeva test demonstrated a specificity (the ability of the test to identify negative results) of 79% and a positive predictive value (PPV, proportion of positive test results that are true positives) of 54%. This performance was not statistically different from what was previously reported for Eeva’s clinical validation (specificity 85%, p 0.19; PPV 59%, p 0.55). Among good quality blastocysts, the average P2 and P3 parameters measured by Eeva were also consistent with previously reported findings. Conclusions: Our results demonstrate Eeva software can predict BF by day 3 with a high degree of reliability, and the accuracy of the performance is consistent across diverse clinical practice styles, laboratory protocols and procedures. Follow up studies to link these findings with implantation are underway and may facilitate changes in practice, in particular a move away from blastocyst culture and the possible associated epigenetic risks. B2.1: Do IVF pregnancies grow differently to spontaneous conceptions SHYAMALY SUR1, JAMES HOPKISSON2, BRUCE CAMPBELL1,2 & NICHOLAS RAINE-FENNING1,2 1 School of Clinical Sciences, University of Nottingham, Nottingham, UK and 2Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE], Division of Obstetrics and Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK Aims: To investigate whether singleton pregnancies conceived following IVF show different growth patterns to spontaneously conceived pregnancies during the first trimester. We hypothesised there would be no significant difference in size between the two groups. Methods: A prospective study of women with live singleton pregnancies conceived after IVF treatment. Only pregnancies that ended in livebirth were included. Women were scanned transvaginally and the embryonic crown rump length (CRL) measured between 6 and 13 weeks gestation. A nomogram was devised, according to the principles of Chitty et al., and used to compare the IVF pregnancies to the current standard BMUS/NHSNSP first trimester CRL chart used in the UK for the dating of spontaneously conceived pregnancies. Limits of agreement (LoA) and the F-test were used to compare observed CRL measurements in the IVF pregnancies with those expected from the BMUS chart. Results: 1063 women recruited. 367 women excluded: 142 twin, 3 triplet, 7 ectopic pregnancies, 215 miscarriages. 696 women included in the final nomogram. LoA revealed a mean difference of 2.8% (95% CI 34.6 to 40.3) which, at 12 weeks equates to 1.5 mm (95% CI; 18.0–21.0 mm) with IVF pregnancies measuring greater than those in the BMUS chart. The F-test comparing the nomograms also revealed the Human Fertility Abstracts e19 curve for IVF pregnancies was significantly shifted to the left. This meant that for a CRL of 54mm whilst the BMUS chart calculated the gestational age to be 12 0 (11 2 to 12 5) weeks the mean gestational age of the IVF pregnancy was 11 6 (11 2 to 12 2). As such we rejected our hypothesis. Conclusions: IVF pregnancies are significantly larger than those conceived spontaneously during the first trimester. The difference is only one day at the end of the first trimester and could reflect measurement error therefore but was consistent. These findings need to be clarified in larger studies but could have implications for anomaly screening. B2.2: Assessment of birth weight and gestational period following in vitro fertilisation and intracytoplasmic sperm injection ELLA CLAPHAM, VANESSA WRIGHT, SAMANTHA BYERLEY, MARY HERBERT & JANE STEWART Newcastle Fertility Centre At Life, Newcastle University, Newcastle upon Tyne, UK Introduction: Low birth weight ( 2500 g) and premature birth ( 37 complete weeks) are two main determinants of neonatal mortality and morbidity and also pose a long-term threat to health with higher incidences of life-long conditions such as respiratory illnesses and learning disabilities documented. The aim of this study was to examine the obstetric outcomes of singleton births following in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI). Material & Methods: Retrospective data analysis was performed to compare the birth weights and gestational periods of all singleton births in a 32 month period following IVF treatment with those born following ICSI treatment. Information on 260 IVF singletons and 181 ICSI singletons was obtained from completed HFEA outcome registry forms. Statistical analysis was carried out using two sample independent t-test and Chi-square test. Results: The birth weight of IVF singletons was on average 91 g lighter than that of ICSI singletons (3159 g 629 and 3250 g 601 respectively) however this trend did not reach significance (p 0.13). There was no difference in the average gestational periods; 38.53 weeks for IVF pregnancies and 38.83 weeks for ICSI pregnancies (p 0.21). 11.9% of the IVF singletons had low birth weight, this was not significantly different from the 9.9% of ICSI singletons with low birth weight (p 0.52). Premature births accounted for 24.2% of all IVF births, this finding was greater than in the ICSI population which had a premature birth rate of 16.6% however significance was not quite met (p 0.053). Conclusions: Our findings indicate that the birth weight and gestational period of singletons born following IVF and ICSI do not differ significantly. This is in agreement with a number of published studies. Future work will continue to monitor obstetric outcomes to determine if the trends observed reach significance. B2.3: Reducing multiple births: single blastocyst replacement as a solution LAINA MURPHY, LOUISE KELLAM, LUCY JENNER & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: To compare clinical and multiple pregnancy rates (CPR and MPR) for patients having 3 good quality embryos on day 3 and having 2 of these transferred (D3 DET), compared to those having a single blastocyst transferred (D5 SET) following extended culture. Background: The HFEA has set a target of 10% maximum multiple birth rate for fertility clinics from 2012. Regular review of clinic multiple birth minimisation schemes are therefore essential and many new techniques are becoming available to do this. Results: Data analysis of ART cycles carried out at CARE Nottingham between 1st January 2008 and 30th November 2011 compared CPR and MPR for patients having D3 DET with good quality embryos, with those who had D5 SET, split into groups by age: 30 years (n 114), 35 years (n 319), 35 years (n 216) and all ages (n 535). CPR was maintained and not statistically significant for all age groups, including those 35 years (P 0.7481) having D5 SET at 52% (n 50), compared to D3 DET at 49% (n 166), however the MPR was significantly decreased (p 0.0108) to 0% from 21% in patients having D5 SET. CPR for patients with overall good quality embryos having D3 DET increased significantly (p 0.0001) compared to those with all embryo qualities at 42% (n 1204) but the MPR remained significantly higher in both groups at 36% and 30% respectively (p 0.1230). Conclusion: to reduce the MPR and associated risks significantly, patients of all ages, with 3 good quality embryos on day 3 could be encouraged to culture the embryos further and have a single blastocyst replaced, without compromising overall pregnancy chances. © 2013 The British Fertility Society e20 Abstracts B2.4: Live birth rates significantly improve following management of a PCT enforced “one for all” single embryo transfer policy SOPHIE JAQUES, JANE BLOWER, NEELAM POTDAR & TAREK GELBAYA Leicester Fertility Centre, University Hospitals of Leicester, Leicester, UK Background: Single embryo transfer (SET) is the main focus for reducing the risks associated with multiple pregnancies following IVF. To reduce these risks to mother and baby, in 2009 the HFEA introduced the “One at a time” initiative encouraging clinics and NHS commissioners to implement SET policies. Therefore, mandatory SET was enforced by our local primary care trust (PCT) for all NHS patients, irrelevant of patient age or embryo quality. Here, a retrospective analysis compares the effects of mandatory SET on clinical pregnancy, live birth and multiple pregnancy rates, before and after implementation of the ACE/BFS patient management algorithm. Methods: Clinical pregnancy, multiple pregnancy and live birth rates were compared for three embryo transfer periods: period 1, premandatory SET (both single and double embryo transfers) from 2007–2008 (n 307); period 2, mandatory SET (without using ACE/BFS algorithm) in 2009 (n 135); period 3, mandatory SET (using ACE/BFS algorithm) from 2010–2011 (n 317). Results: During the three periods, the SET rates were 10.7%, 100% and 100%, respectively (Chi-squared test P 0.000). There was no difference in clinical pregnancy rates (31.9%, 24.4% and 29.3%, respectively) (P 0.4034), but the multiple pregnancy rates was significantly reduced in second and third periods (24.9%, 3.3% and 1.1%, respectively) (P 0.000). The live birth rate was significantly improved in the third period (21.2%, 20% and 26.5%, respectively) (P 0.0019). Discussion: Following the introduction of the PCT enforced mandatory SET policy, the clinical pregnancy and live birth rates declined initially in period 2. As expected, a significant decrease in the multiple pregnancy rates was observed. The ACE/BFS patient management algorithm was implemented in period 3, which was met with a significantly improved the live birth rate. Implementation of the mandatory SET policy has positively affected the “take home baby” rate, which likely results from fewer, twin related miscarriages. B2.5: Predicting success of medical management of ectopic pregnancy: a retrospective cohort ALISON RICHARDSON Obstetrics and Gynaecology, Derriford Hospital, Plymouth, Devon,UK Introduction: Using current medical management of ectopic pregnancy protocols, the first indication of success is not obtained until day 7. Earlier indicators may permit timelier intervention, provide welcome reassurance and enable more individualized follow-up. Aims: To determine if the direction and magnitude of change in bhCG between days 0 and 4 after Methotrexate predicts success in medical management of ectopic pregnancy. Methods: A retrospective review of all medically treated ectopic pregnancies between 01/01/05 and 31/07/11 was undertaken. Women were treated using the regime developed by Stovall(1). bhCG levels on days 0, 4 and 7 were recorded in addition to whether a repeat dose of Methotrexate or surgery was required. Success was defined as the avoidance of surgery. Results: 232 women were identified. The overall success rate was 93.1%. Treatment was more successful when the ßhCG decreased between days 0 and 4 (97.6% versus 88%) and when the initial ßhCG was 3000 iu/l (96.6% versus 82.8%). Overall 15.9% had a repeat dose of Methotrexate which was successful for 86.5% of women. 6.9% of women underwent surgery. 31.3% of these had received 2 doses of Methotrexate. From the results, the probability of requiring a repeat dose of Methotrexate or surgery depending on the direction and magnitude of change in ßhCG between days 0 and 4 has been calculated. Conclusion: Success rates of medical management of ectopic pregnancy range from 73.5–98.0% depending on the initial ßhCG and whether it increases or decreases immediately after Methotrexate. This information could be used to develop new follow-up protocols which would have positive financial implications. It could also be used in combination with clinical findings when patients present with abdominal pain after Methotrexate to help determine the need for surgery. Reference 1. Stovall, T.G. Single dose methotrexate for management of ectopic pregnancy. Obstet Gynecol 1991; 77(5):754–7. Human Fertility Abstracts e21 B2.6: Effect of recipients’ Body Mass Index on pregnancy outcomes in oocyte donation cycles AMELIA RODRÍGUEZ, DÉSIRÉE GARCÍA, RITA VASSENA, ORIOL COLL & VALÉRIE VERNAEVE Clinica EUGIN, Fundació EUGIN, Barcelona, Spain Aims/Objectives: To evaluate the effect of Body Mass Index (BMI) of oocyte recipient in oocyte donation cycles on biochemical and clinical pregnancy rates. Content: This retrospective study investigates four BMI categories: underweight ( 18.5), normal ([18.5–25[, overweight ([25–30[ and obesity (class I [30–35[, class II-II I 35] on the chance to become pregnant with fresh donor oocytes. Data from 7339 cycles performed in a fertility clinic between February 2009 and May 2012 were analyzed. Relevance/Impact: High BMI is a risk factor for infertility and miscarriage, affecting both embryo quality and endometrial receptivity. In oocyte donation cycles, the endometrium of the recipient is prepared for embryo reception through an estrogenic treatment. However, because exogenous estradiol is metabolized and stored in the adipose tissue, the bioavailability of the treatment might diminish. Outcomes: Women recipients of oocytes were 41.0 4.80 (mean SD) years old, and had a BMI of 22.8 4.28 distributed in: 4% underweight, 66% normal, 21% overweight and 9% obese. Thirty percent were overweighed. Differences in biochemical pregnancy rates were observed for overweight (51%) and obesity (50%) when compared to normal (55%), although not statistically significant. However, when overweight was compared to not overweight, these differences became very significant (50% vs. 55%, p 0.001). Correspondingly, the differences in clinical pregnancy rates for overweight (47%) and obesity (47%) compared to normal (52%) turned into significant when overweight versus not overweight was analyzed (47% vs. 52%, p 0.001). Clinical pregnancy in obesity was not different either between classes of obesity (51% vs. 46%, p 0.29) or between short ( 20 days) and long ( 20 days) estrogenic treatment length (46% vs. 41%, p 0.39). Discussion: These results suggest a negative association between high BMI in oocyte recipients and pregnancy due to endometrial factors, independently of the length of estrogenic treatment. Longer administration of estrogens is not likely to improve pregnancy in obese patients. B3.1: Does donor age affect the final outcome in egg donation treatments? JAIME GUERRERO, JORGE TEN, JOAQUÍN LLÁCER, BELÉN MOLINER & RAFAEL BERNABEU Instituto Bernabeu, Alicante, Spain Introduction: The main goal of this study is to evaluate whether donor age is an independent predictor of pregnancy outcome in recipients. Materials and Methods: Retrospective study including 283 oocyte donation cycles performed in our clinic from January to June 2012. Donors were healthy women younger than 35 years, according to Spanish fertility act. All donors where estimulated with 150–300 UI of urofollitropin (Fostipur) depending on antral follicular count. When lead follicule reached 13–14 mm a GnRH antagonist (Cetrotide) was administered daily, and GnRH agonist (Triptorelin, 0.4 mg) was used for final oocyte maturation when at least 3 follicules were 18 mm in diameter. Recipients uterine endometrium was prepared using exogenous estrogen (Progynova) and progesterone (Cyclogest). To study the influence of donor age on clinical pregnancy we performed a multivariate logistic regression analysis with adjustment for recipient age, previous attempts, endometrial thickness, retrieved oocytes and embryo quality. Data were shown as mean SD. Results: Donor age ranged from 18 to 32, mean 24.8 3.9, recipient age 41.2 4.5, mean number of retrieved oocytes 18.5 7.5, endometrial thickness 8.7 1.8, and transferred embryos 1.9 0.4. The overall pregnancy rate was 69.6%, clinical pregnancy rate 54.1%, miscarriage rate 10.5%, and implantation rate 39%. The logistic regression analysis did not show statistically significant correlation between donor age and clinical pregnancy (OR: 0.99, 95% CI: 0.93, 1.07; p 0.91) with no other confounding factors affecting clinical pregnancy outcome. Conclusions: Often patients are particularly concerned about the age of the donor. However, we can conclude from our results that this factor doesn’t compromise the chance of pregnancy. © 2013 The British Fertility Society e22 Abstracts B3.2: Mechanical implantation, subendometrial embryo delivery (SEED), with egg donation MICHAEL KAMRAVA & MEI YIN West Coast IVF Clinic, Inc, Beverley Hills, Califormia, USA Introduction: Various techniques for embryo transfer (ET) have been advocated to increase pregnancy rates while reducing side effects from the procedure. We have hypothesized that the mechanical insertion of the blastocyst into the endometrium under direct visualization would increase the implantation and clinical pregnancy rate of IVF while minimizing side effects. The aim of this study was to re-investigate the potential of sub-endothelial ET, starting with quality eggs from young egg donors, and using a hysteroscopic direct implantation procedure. Materials and Methods: There were 21 consecutive patients between 34–50 years of age with a diagnosis of peri/postmenopause or premature ovarian failure with or without tubal disease. They underwent 24 fresh IVF cycles in this study. Controlled ovarian hyperstimulation and donor uterine preparation was done according to previously published protocols. Embryo transfer was done via a flexible minihysteroscope and implanting the embryo(s) directly into the endometrium. Results: There were sixteen positive βhCGs at levels greater than 5 IU/ml. There were five biochemical pregnancies, and eleven clinical pregnancies as evidenced by the presence of a gestational sac visualized by ultrasound examination at five weeks of gestation and heart beat at six weeks of gestation. There were 4 spotaneous abortions. Healthy babies were delivered by seven patients. No ectopic pregnancies (tubal, placenta previa, cervical) were seen. There were 4 twins from day five and none from day 6 implantations. Conclusion: We suggest that using a hysteroscopic subendometrial embryo delivery (SEED) allows for a targeted objective, reliable, and replicable method for embryo transfer. It will virtually eliminate ectopic pregnancies of all locations as well as occurrence of placenta previa and cervical pregnancies from IVF. Furthermore, it would greatly alleviate the anxiety, and cost to the patient as it would decrease the number of attempts at using IVF in achieving a successful singleton pregnancy. B3.3: Donor Oocyte Banking: A Three Year Perspective JOSH LIM1, MICHAEL TUCKER1,2, JAMES GRAHAM1, OLGA PILSHCHIKOVA & MICHAEL LEVY1 1 Shady Grove Fertility Reproductive Science Center, Rockville, MD, USA and 2Georgia Reproductive Specialists, Atlanta, GA, USA Introduction: Given the evolution of the donor oocyte industry, we have chosen to compare our cryopreserved and fresh donor oocyte outcomes to determine the efficacy of both approaches. Methods: Frozen oocyte cycles performed by a successful IVF laboratory from June 2009 to June 2012 were reviewed and analyzed. A proven oocyte vitrification protocol (7.5%EG DMSO, followed by 15%EG DMSO 0.5Msucrose) was employed with an ‘open’ vitrification carrier using commercially available media (Irvine Scientific); warming was undertaken in stepwise dilutions of sucrose. Results: Of 2053 oocytes banked in three years, 826 oocytes were thawed resulting in the survival of 736 (89%). These thawed oocytes were then distributed to 132 recipients. 567 oocytes were fertilized normally (2PN, 77%) following ICSI with 563 cleaving. Embryo transfer (ET) was performed in 130 cycles with cancellation of ET in two cycles due to inadequate embryo development. Transfers were performed either on day-3 (n 67, mean 1.95 embryos/ET), or as blastocysts (n 63, mean 1.42 embryos/ ET). From 130 ETs, 71 resulted in clinical pregnancies (55%), with 59 ongoing/delivered pregnancies (45%). This was in comparison with fresh oocyte cycles collected from Jan 2009 to Dec 2011, where 1160 clinical pregnancies arose from 1951 ETs (59%), which represented a live birth rate of 52%. Conclusions: This retrospective review of our donor oocyte banking program is very encouraging. While our sample sizes are somewhat unbalanced between the fresh and frozen oocyte population, pregnancy rates from either source were comparable. Donor oocyte banking utilizing vitrification is a feasible and clinically valuable adjunct to our fresh oocyte donation program, which ultimately may become a more important alternative. Additionally, the major advantage of a donor egg bank program is oocyte availability, which creates greater ease and convenience in the scheduling and co-ordination of donor and recipient cycles. Human Fertility Abstracts e23 B3.4: Is there a seasonal variation in conceptions by donor insemination? MADHAVI GUDIPATI, KIM PEARCE, DAVID CULLEN, GILLIAN REDHEAD, KEVIN MCELENY & JANE ALLISON STEWART Newcastle Fertility Centre At Life; Institute of Cellular Medicine, University of Newcastle, Newcastle, UK Objective: Seasonal variation in donor conceptions using frozen sperm, possibly due to the effect of photoperiod on female factors (egg quality/endometrial receptivity) has been reported, but this is controversial. We aimed to analyse the distribution of conceptions achieved by donor insemination (DI) treatments by the season of treatment. We further investigated seasonal variation in the cryo tolerance/sperm function by analysing the distribution of donor conceptions by the season of original sperm production of the thawed sperm used for treatment. Methods: We performed a retrospective review of all DI treatments performed at Newcastle fertility centre from 2005 to 2010. A total of 496 DI treatments were included in the study. DI treatment involved ultrasound monitored natural cycle intra cervical insemination of thawed sperm. The variables recorded were the season of treatment, treatment outcome, and donor sperm used which was tracked back to the season of original sperm production. A positive pregnancy test was taken as pregnant. Results: The age range of the women undergoing DI was 22 to 43 years with a median of 33 years. The pregnancy rate per DI cycle was 11.3%. Donor insemination treatment outcome by the season of treatment: The pregnancy rate per treatment cycle varied from 10.3% with treatments carried out in winter and summer to 13.8% in spring with 10.7% in autumn. There was no significant difference in the outcome of the DI treatment by the season of treatment (p 0.79). Distribution of DI conceptions by season of original sperm production: Only 480 DI cycles were included in this section as it was not possible to track down the season of original sperm production in 16 cycles. Most of the treatment cycles (42.2%) were carried out with semen samples produced in spring. The pregnancy rate per cycle varied from 9.3% when semen samples produced in winter were used for DI treatment to 15.1% by the semen samples from autumn, however there was no statistical difference in the outcome of DI treatment by the season of semen sample production (p 0.67). Conclusion: There was no significant difference in the outcome of the DI treatment by the season of treatment or the season of original sperm production. B3.5: Double donation of sperm and oocytes: patients’ characteristics and outcomes RITA VASSENA, JUAN JOSÉ GUILLÉN, FLAVIA RODRIGUEZ, ORIOL COLL & VALERIE VERNAEVE Clinica EUGIN, Barcelona, Spain Aims/Objectives: Although comparatively rare in the assisted reproduction landscape, double gamete donation, i.e. the gestation of an embryo produced by the fertilization of a donor oocyte with donor sperm, has become in the last few years the path to pregnancy for thousands of women worldwide. However, no studies so far have addressed the characteristics of the patient population undergoing this treatment. Our large retrospective study aims at identifying the characteristics of the cohort of patients receiving double gamete donation for fertility treatment, and monitoring their reproductive outcome. Content: Data from a cohort of 1131 fresh double donation cycles at a large fertility clinic in a ten year period between June 2000 and July 2010 were included. The unit of analysis is cycle of embryo transfer. Therefore, multiple procedures on the same patients, where present, are not linked to each other. Student’s t-test and Chi2 test were employed, as appropriate. Results: Women accessing double donation were on average 42.2 4.28 years old, their reported sterility time 3.2 3.99 years, and they reached double donation after 3 3.77 failed cycles, 1.38 0.7 of which previous double donation attempt. There was a clear difference between women in a heterosexual relationship, which were younger than average (40.37 4.7, p 0.001), with longer infertility history (5.2 4.24, p 0.001) and more failed ART cycles (4.33 4, p 0.001), and women without a male partner. Women without a male partner were older than average (43.59 3.24, p 0.001), with shorter sterility times (2.11 3.31, p 0.001) and less previous ART cycles (2.43 3.39, p 0.001). Biochemical pregnancy rates were comparable among groups (50–51%), as were spontaneous abortion (8.1–10.3%) and clinical pregnancy rates (39.9–41.6%). Conclusion: patients accessing double gamete donation present diverse socio-demographic typologies with variable reproductive histories and severity factors. Double gamete donation offers high biochemical and clinical pregnancy rates in all typologies analyzed, and is and effective fertility treatment option. © 2013 The British Fertility Society e24 Abstracts B3.6: Intermediate and normal sized CGG repeat on the FMR1 (fragile X) gene does not affect ovarian response in oocyte donor BELEN LLEDO, JAIME GUERRERO, JOSE A. ORTIZ, RUTH MORALES, JUAN GIMENEZ, JOAQUIN LLACER & RAFAEL BERNABEU Instituto Bernabeu, Alicante, Spain Objective: The goal of this study is investigated whether CGG repeats on the FMR1 gene have predictive value for ovarian response to gonadotropins, oocyte yield, days of stimulation and cycle outcome during an oocyte donors programme. We evaluate the ovarian response to gonadotropin in oocyte donors with different CGG repeats on the FMR1 gene in normal range. Materials and Methods: We include the results of X fragile genetic screening from 141 control and 63 study oocyte donors. The study population was divided into three groups: women with 35–39 repeats (n 34), 40–45 (n 12) and 45 (n 17). All the patients received a controlled ovarian stimulation protocol, combining rFSH (150 or 225) antagonist (Cetrorelix), and triggering the LH surge with agonist (Triptoreline). The test were performed in accordance with publish recommendations by commercial assay. Statistical analysis was performed using SPSS software. Results: No significance differences in cycle outcome were observed between control group and population subgroups. The ongoing pregnancy rate was 46.8% for control vs 54% for study group. According to ovarian stimulation, no differences were observed in donor age and number of oocyte yield between control and population groups. Women from control group used significantly more gonadotrophin (2212 IU) than study group (1850 IU) and regardless subgroup. Days of stimulation for women from control group were 11.40 vs 9.82 for women from study group. To subgroups only 35–39 (9.6) and 40–45 (9.8) showed significance difference. Conclusions: For the first time we present data showing the relation between normal and intermediated sized CGG repeats on FMR1 gene and ovarian stimulation using a non-confusion model as oocyte donor. Our data suggest that ovarian stimulation does not be affected by CGG repeats on normal and intermediated range. The number of oocyte yield and the cycle outcome are not influenced by the CGG repeats. B4.1: A retrospective study comparing implantation pregnancy rate to blastocyst grade in ART cycles from July 2010–May 2012 SAM DALE, ELLEN CATER, LUCY JENNER, LOUISE KELLAM & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: To investigate the significance of blastocyst ICM and trophectoderm grade, in relation to implantation grade (IR) in fresh ART cycles. Background: In recent years the application of blastocyst stage embryo transfer has increased to increase positive outcome and embryo selection to meet the MBMS targets set by the HFEA. Method: Data from 528 fresh cycles including all age groups from July 2010 to May 2012 were analysed. Those that achieved 100% implantation or where implantation failed were included. Blastocysts were graded on the morning of embryo transfer, scoring the quality of the ICM and the trophectoderm separately from 1 (highest) to 3 (lowest) using an in-house grading system. Results: A total of 747 blastocysts were transferred, in SET and DET cycles, of these 341 implanted (45.6%) as confirmed by a foetal heart per embryo. Where the ICM was graded 1 the IR was 56.1% (37/66), grade 2 43.8% (245/559) and grade 3 30.8% (4/13), where the trophectoderm grade was constant at 2. Embryos with a trophectoderm grade 1 IR was 65.2% (15/23), grade 2 43.8% (245/559) and grade 3 12.1% (4/33) ICM grade was constant at 2. Statistical analysis of these results, using a chi-squared test with 5 d of f, showed no significant difference for IR with respect to ICM grade (p 0.0987) and a highly significant difference for trophectoderm grade (p 0.0001). Blastocyst expansion rate was comparable in all groups (p 0.058 and p 0.077 respectively). Conclusion: The data suggests that the grade of the trophectoderm is a more significant predictor of IR than the grade of the ICM, supporting the findings by Honma et al (2012) but contradicts the findings by Van den Abbeel et al. (2012). Human Fertility Abstracts e25 B4.2: Pregnancy rates decrease after the fourth unsuccessful IVF/ICSI treatment cycle LUKASZ POLANSKI, LYNDSEY ZUJOVIC, MIRIAM BAUMGARTEN, JAMES HOPKISSON, KIRSTYN SEWELL, BRUCE CAMPBELL & NICK RAINE-FENNING Division of Obstetrics & Gynaecology, B Floor, East Block, NURTURE, QMC, School of Clinical Sciences, University of Nottingham, Nottingham, UK Aim: The aim of the study was to assess the chances of clinical pregnancy (CP) and the clinical pregnancy rates (CPR) in the index cycle in women undergoing repeated IVF and ICSI treatments. Materials and Methods: Women attending for IVF treatment were prospectively followed between Jan 2007 and June 2012. Only fresh cycles were included. Outcome was defined as a viable clinical pregnancy at 6 weeks on transvaginal ultrasound. Likelihood ratios and post-test probability analysis was used. Results: Data were normally distributed and presented as mean (/SD). Complete data was available for 2684 cycles. Mean age was 34.5 years (/4.4). The overall clinical pregnancy rate was 45.6%. 1740 women underwent first cycle with a probability of CP of 46.6%. 36 women underwent 6 or more cycles with a probability of 33.5% for successful pregnancy. Clinical pregnancy rates were noted to decrease significantly after the fourth treatment cycle, from 43.3% in the fourth cycle to 34.2% in the fifth cycle. Conclusions: This study demonstrates a relative stability of clinical pregnancy rates and probability of conception up to and including the fourth cycle, irrespective of previous treatment outcomes. This can be used to counsel couples when advising on the relative success of subsequent treatment cycles. The limitation of the current analysis is the lack of stratification for patients’ previous obstetric history and outcomes of IVF treatments preceding the index cycle. On-going data analysis aims to address this issue. B4.3: Outcomes of gonadotrophin-based spermatogenesis induction therapy in male hypogonadotrophic hypogonadism: 11-year, single-centre experience MEENAKSHI CHOUDHARY & RICHARD QUINTON Newcastle Fertility Centre At Life; Newcastle upon Tyne Hospitals NHS Trust, Newcastle, UK Introduction: Men with hypogonadotrophic hypogonadism (HH) are usually treated in non-fertility endocrinology clinics for initiation and monitoring of androgen replacement hypopituitarism. When they desire fertility they are generally referred to fertility centres. This study reflects on the outcome of gonadotrophin-based spermatogenesis induction in an adult endocrinology non-fertility setting in a tertiary referral unit. This study shows that awareness amongst adult endocrinologists of fertility induction for HH men can result in successful outcomes and greater continuity of care. Methods: A total of 15 men were treated with FSH and hCG combination therapy over an 11 year period (2000–2010) to induce spermatogenesis. Results: Of the total 15 men, 4 had Kallmann Syndrome, 5 had HH post transphenoidal pituitary surgery/ radiotherapy, 2 had combined pituitary hormone deficiency and rest had normo-osmic idiopathic HH (nIHH). Gene defect was identified in 4 of these 15 men. Spermatogenic induction was successful in all but one. Of the remaining 14 HH men, 3 men have sperms frozen but yet to undergo IVF treatment for female related subfertility and one is still having ongoing treatment with rising sperm count (15 million/ ml). This resulted in 16 pregnancies and 14 live births creating a total of 9 families for 10 men. 50% of these pregnancies required assisted conception. Total drug cost spent per live birth was £8000. Conclusions: Spermatogenesis can be successfully induced in male hypogonadotrophic hypogonadism in a non-fertility setting by dedicated adult endocrinology team. However, close liaison with fertility units is advised as around 50% of pregnancies achieved were IVF/ ICSI-assisted. © 2013 The British Fertility Society e26 Abstracts B4.4: The effect of thawing on tissue conservation in ovarian cryopreservation TOM MOREWOOD1, SAFAA NASSER EL DINE, GREG FITZHARRIS1, BARRY FULLER2 & PAUL HARDIMAN1 1 Institute for Women’s Health, University College London, London, UK and 2Division of Surgery and Interventional Science, Royal Free Hospital, University College London, London, UK Background: Approximately 1 in 640 adults is a childhood cancer survivor. Chemo- and radiotherapy often cause premature ovarian failure, especially with the use of alkylating agents. Currently the only fertility option for women diagnosed with malignant disease is emergency ovarian stimulation and freezing of ova or embryos, if a partner or donor gametes are available. This technique delays treatment and is not available to women with hormone-sensitive tumours or to pre-adolescents. Ovarian tissue cryopreservation is an experimental technique which aims to preserve the fertility of those women about to embark on a course of treatment for malignant disease. However, there remain many unresolved issues with this technique, for example there is no consensus regarding the optimum conditions for freezing and thawing the tissue. Our research group is attempting to maximise the proportion of tissue conservation by applying different slow freeze-thaw protocols to the ovarian tissue, which could be applied clinically prior to autologous transplantation. Methods: Ovarian tissue biopsies are collected during elective caesarean section operations, and then subjected to different cryopreservation and thawing protocols with unfrozen specimens used as controls. Viable follicle density is then determined by culturing tissue sections for four hours in a medium containing neutral red as a vital stain, followed by follicle visualisation using dark-field microscopy. Results: Results will be presented from our experiments attempting to optimise freeze-thaw protocols and the proportion of tissue conservation following cryopreservation. Pilot data reveal positive NR staining in approximately 68% of tissue slices and demonstrate follicle conservation rates between 19% and 33%. Conclusion: Optimisation of freeze-thaw protocols will increase the efficiency of ovarian tissue cryopreservation leading to improved outcomes for these disadvantaged patients. B4.5: Comparison of Cycle Outcome between Two Different Incubator Environments ALEXANDER GWYNN, AYSHA ITANI, TIM CHILD, ENDA MCVEIGH & KAREN TURNER Oxford Fertility Unit, Institute of Reproductive Sciences, Oxford Business Park North, Oxford, UK Purpose: Incubators are a core component of the IVF laboratory and so their ability to provide an optimal environment for embryo culture and development is critical. This study compared the cycle outcome (cleavage rate, incidence of Day 3 or Day 5 embryo transfer (ET), cryopreservation rate, incidence of elective single embryo transfer (eSET), clinical pregnancy rate and implantation rate) of patients cultured in two different types of low oxygen incubators; the top loading Cook K-Minc mini incubator and the front loading Sanyo MCO-18 large conventional incubator. Methods: A retrospective analysis of patients cultured in the two incubator types was performed using data from 2010 to 2012. This was limited to ICSI patients 38 years of age that had achieved between 4 and 12 fertilised oocytes. Surgical sperm retrieval (SSR) patients were excluded. This data set was chosen as the patients within this group were eligible for extended culture and eSET. Results: A total of 440 cycles were analysed, all of which resulted in embryo transfer. No statistical significance was evident for the mean patient age, the mean Mean Age (years) Mean No Fertilised Oocytes/Cycle Cleavage Rate: 1 to 2 cell (1 to 2 cell/No fertilised oocytes) Day 3 ET Rate (No/cycle) Day 5 ET Rate (No/cycle) Cryopreservation Rate (No/cycle) eSET Rate Clinical Pregnancy Rate Implantation Rate Cook K-Minc Sanyo MCO-18 33.0 6.5 99.1% (678/684) 46.2% (49/106) 53.8% (57/106) 25.5% (27/106) 28.3% (30/106) 40.6% (43/106) 29.7% (54/182) 33.4 7.0 98.7% (2290/2320) 35.9% (120/334) 64.1% (214/334) 38.6%∗ (129/334) 46.4%∗∗ (155/334) 42.2% (141/334) 33.9% (174/513) ∗p 0.05; ∗∗p 0.001. Human Fertility Abstracts e27 number of fertilised oocytes per cycle, the cleavage rate from 1 to 2 cells, the Day 3 and Day 5 ET rate, clinical pregnancy rate or implantation rate. However, embryos cultured in the Sanyo MCO-18 were more likely to achieve supernumerary cryopreservation and there was an increased incidence of eSET. Conclusion: Both types of incubator have a similar clinical outcome (pregnancy rate and implantation rate). However, the results of this study suggest that the Sanyo MCO-18 provides a more favourable environment for embryo culture to the blastocyst stage as embryos were more likely to be frozen and there was an increased incidence of eSET. B4.6: Retrospective analysis of “no result” rate and “no result rescue” by rebiopsy and reanalysis in PGD and PGS COLLEEN LYNCH, ELLEN CATER, LUCY JENNER, LOUISE KELLAM, KATHRYN BERRISFORD & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: To examine the percentage of samples with no result following PGD/PGS and the efficacy of retesting. Methods: PGD cycles from 2010–2012 were analysed in terms of number of embryos analysed, number returning no result, number rebiopsied, and subsequent outcome. PGS and chromosome rearrangement PGD cycles were similarly analysed for the period 2011–2012. Rebiopsied embryos are usually vitrified and used in subsequent cycles. Results: For PGD 702 samples were analysed, with a no result rate of 24%. Of the 169 embryos without diagnosis, 45 (27%) were rebiopsied and 35 (78%) returned a result. Of the reanalysed embryos, 26 (58%) were suitable for patient use. So far 18 of these embryos have been used over 15 cycles, resulting in a clinical pregnancy rate of 33% per cycle and 42% per transfer. For PGS 888 samples were analysed, with a no result rate of 13%. Of the 111 embryos without diagnosis, 14 (12%) were rebiopsied and 11 (79%) returned a result. Of the reanalysed embryos 6 (43%) were suitable for patient use. So far 3 of these embryos have been used over 3 cycles resulting in a clinical pregnancy rate of 67% per cycle and transfer. For chromosome rearrangement PGD 223 embryos were analysed with a no result rate of 19%. While 13 (30%) of the 43 embryos without diagnosis were rebiopsied, with 9 (69%) returning a result, no embryos were suitable for patient use. Conclusion: The percentage of embryos suitable for rebiopsy out of those with no result indicates that in the majority of cases this is due to factors related to the embryo rather than the testing. However, those that are suitable for rebiopsy have the potential to return a result and be suitable for patient use. These embryos have a good clinical pregnancy rate despite multiple biopsy and vitrification. B5.1: Establishment of androgen-induced mouse models for polycystic ovary syndrome KIRSTY WALTERS, LINDA MIDDLETON, CHARLES ALLAN & DAVID HANDELSMAN ANZAC Research Institute, Department of Andrology, Concord Hospital, University of Sydney, NSW 2139, Australia Polycystic ovary syndrome (PCOS) is an endocrine disorder affecting 5–10% of women of reproductive age, causing anovulation, infertility, hyperandrogenism, obesity, hyperinsulinism and increased risk of type 2 diabetes and cardiovascular disease. However, the etiology of PCOS is not well understood, and currently there is no consensus on the best experimental animal model to study the pathogenesis of PCOS. This project aims to develop a mouse model of PCOS that best emulates the disorder. We have investigated two strategies to replicate PCOS features by increasing androgen levels in vivo: 1) by inducing an increase in endogenous circulating androgens using letrozole, an aromatase inhibitor which prevents the aromatization of androgens to estrogens; and 2) administering exogenous DHT, a potent and non-aromatizable androgen. 21 day old mice were treated with 90 day sub-dermal implants of either letrozole, DHT or a placebo (controls). All DHT treated mice were acyclic (p 0.01) and exhibited a significant increase in body weight (p 0.05) compared to control mice. Ovaries exhibited many large antral follicles but had no corpora lutea present, indicating anovulation. Inguinal (p 0.01), parametrial (p 0.05) and retroperitoneal (p 0.01) fat pad weights were significantly increased in DHT treated mice compared to controls. Intraperitoneal insulin tolerance test revealed insulin resistance in DHT treated mice (p 0.05). 60% of letrozole treated females were acyclic (p 0.05), and ovaries contained no corpora lutea indicating anovulation. However, hemorrhagic cysts, which are not a true PCOS phenotype, were present in ovaries from letrozole treated females. Furthermore, there was no significant difference in body or fat pad weights between © 2013 The British Fertility Society e28 Abstracts letrozole treated and control mice, and no observed insulin resistance. In conclusion, current results support the treatment of mice with DHT over letrozole, as an effective approach to induce a useful mouse model to study pathogenic mechanisms in PCOS. B5.2: Cyclic guanosine monophosphate (cGMP) mediates regulation of vascular endothelial growth factor (VEGF)-A in ovine granulosa cells (GC) PETER MARSTERS, RANA ALHAMDAN & BRUCE K. CAMPBELL Division of Obstetrics and Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK VEGF is an important angiogenic factor which is up-regulated during hypoxia. Therefore levels naturally increase in the GC compartment as it becomes more densely populated. The functional significance of elevated levels of VEGF-A remains to be fully explained but the exceedingly high levels found in the follicular fluid of polycystic ovary syndrome (PCOS) follicles, suggests it is tightly regulated during normal folliculogenesis. VEGF-A is known to be an upregulator of Nitric oxide (NO) and stimulator of NO/cGMP signalling. Conversely, evidence suggests that NO mediates autocrine/paracrine suppression of VEGF via a cGMP pathway. It is intriguing to hypothesise that this may also be an important regulatory mechanism for the fine control of VEGF-A in the GCs of developing follicles. To test this hypothesis, ovine GCs were cultured over time under the specialised conditions necessary to allow cellular differentiation. Real-time qPCR was used to compare VEGF-A mRNA expression profiles from cells treated with either 8-Bromo-cGMP (a cGMP analogue), sodium nitroprusside (SNP, a Nitric oxide donor) or from untreated GCs. VEGF protein production in the different treatments was compared utilising Western blot analysis. Oestradiol (E2) and Progesterone (P4) production patterns were also determined over the same time course. The highest levels of VEGF mRNA expression, in the untreated GC, were noted at the earliest analysis time point (16 hrs), with levels declining until around 96 hours of culture and then remaining at this basal level for the remainder of time in culture. Both cGMP and NO addition accompanied a reduction of VEGF protein production, with mRNA expression at 16 hours of culture being suppressed to around basal levels (P 0.01). E2 and P4 were also down-regulated in the presence of 8-Bromo-cGMP and SNP. These results support the hypothesis that VEGF-A is auto-regulated in ovine GC utilising a NO/cGMP pathway. B5.3: Characterising natriuretic peptide ligand (NPs) and receptor (NPRs) associations in cultured ovine granulosa and theca cells (GC and TC) RANA ALHAMDAN1,2, PETER MARSTERS1 & BRUCE CAMPBELL1 1 Division of Obstetrics and Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK and King Faisal Specialist Hospital and Research Center, Riyadh-11211, Saudi Arabia 2 NPs mediate their actions through the activation of the second messenger cyclic guanosine monophosphate (cGMP) by interaction with membrane bound, guanylyl cyclase type receptors (NPRs). Cardiac natriuretic peptide (CNP) is reported to have a critical role in the maintenance of oocyte meiotic arrest and the atrial (ANP) and brain (BNP) forms are also thought to function in developing follicles. However, the mechanisms of action and signalling pathways of the NP system in ovarian somatic cells remain to be fully described. The objective of this study was therefore to characterise the presence of and associations between the NPs and the three main receptors (A, B and C) in cultured ovine granulosa (GC) and theca (TC) cells. GC and TC were cultured under specialised, serum-free conditions designed to induce cellular differentiation in response to gonadotrophic stimulation in 96 well plates or Labtek® slides. A proximity ligase assay (PLA), incorporating a novel signal amplification process, was utilised in situ for the accurate determination of specific interactions between NPs and NPRs in cultured cells. The effect of addition of NPs (10-5 M) to both cell types on steroid production was also determined. All NPRs were found to be expressed in both cell types. BNP and CNP were constitutively expressed in GCs and ANP in TCs. ANP seems to interact with both A and B-type receptors in GCs. Cell sensitivity to NP challenge appeared transient and ligand bound receptors were optimally detected around 17 minutes after treatment. ANP significantly reduced oestradiol production by GCs but conversely both ANP and CNP significantly up-regulated progesterone (P 0.001). These findings, showing the presence of the NPs and their receptors on ovarian somatic cells and the ability of NPs to modulate somatic cell differentiation in vitro, support the hypothesis that the NP system plays a local role modulating follicle development. Human Fertility Abstracts e29 B5.4: Anandamide levels are elevated in the peripheral blood of women with ectopic pregnancy and are mirrored by changes in their metabolising enzyme activity JUSTIN KONJE1, ALPHA GEBEH2 & JONATHON WILLETS1 1 Reproductive Sciences Section, Dept of Cancer Studies & Molecular Medicine, Robert Kilpatrick Clinical Sciences Building, Leicester Royal Infirmary, University of Leicester, Leicester, UK and 2Directorate of Womens, Perinatal & Sexual Health, Dept of Obstetrics & Gynaecology, University Hospitals of Leicester NHS Trust, Leicester Royal Infirmary, Infirmary Square, Leicester, UK Background:The endocannabinoid system (ECS),comprise of ligands (e.g.anandamide) synthesising (N-acylphosphaditylethanolamine-specific phospholipase D; NAPEPLD) and degradative (fatty acid amide hydrolase; FAAH) enzymes and cannabinoid receptors (CB1, CB2). The ECS is strongly linked to the regulation of early pregnancy success as elevated anandamide levels result in oviductal retention of embryos in knockout mice. Similar observations may occur in women with ectopic pregnancy as FAAH and NAPE-PLD have been localised in peripheral lymphocytes and Fallopian tubes. Aims: To (1) quantify the plasma levels of anandamide and (2) evaluate the blood anandamide metabolising enzyme activities FAAH and NAPE-PLD in ectopic pregnancy and normal pregnant controls and relate that to β-hCG levels. Methods: Whole blood collected from ectopic (n 38) and normal (n 38) pregnancies was used for quantification of plasma anandamide levels by UHPLC-ESI-MS/MS utilising isotope dilution and selective ion monitoring, FAAH and NAPE-PLD enzyme activities by radiometric assays and of β-hCG by immunoassay. Results: FAAH activity was significantly reduced in women with ectopic pregnancy compared to those with normal pregnancy (p 0.05). Mean SD FAAH activity (pmol/min/mg protein) was 132.0 11.91 (ectopic pregnancy) vs. 163.2 9.02 (normal pregnancy). Unlike FAAH activity, there was no significant difference in NAPEPLD activity between the groups (p 0.05). As expected from enzyme activity studies, anandamide levels were significantly higher in the ectopic pregnancy group with mean SEM (nM) levels of 0.78 0.04 (ectopic pregnancy) vs. 0.63 0.04 (normal pregnancy); p 0.05. There was no relationship between anandamide, enzyme activity and β-hCG levels. Conclusion: This is the first study to demonstrate elevated plasma anandamide levels and reduced blood FAAH activity in association with ectopic pregnancy suggesting abnormal function of the endocannabinoid system in peripheral blood. Further studies may be required to exploit these findings with a view to ascertaining their usefulness as discriminatory markers of ectopic pregnancy. B5.5: ‘Somatostatin receptors demonstrate cyclical expression in human endometrium and mid-secretory expression varies according to fertility outcome’ EMILY DICKERSON1, KAREN BEDFORD2, IAN RICHMOND2, STEVE MAGUINESS1,3, STEPHEN KILLICK1,3 & STEPHEN ATKIN1,3 1 Department of Obstetrics and Gynaecology, Hull Royal Infirmary, Kingston-upon-Hull, UK, 2Department of Pathology, Hull Royal Infirmary, Kingston-upon-Hull, UK and 3Hull IVF Unit, The Women and Children’s Hospital, Hull Royal Infirmary, Kingston-upon-Hull, UK Background: The actions of somatostatin, mediated through five somatostatin receptors (sst1–5), include inhibition of angiogenesis and cell proliferation and promotion of apoptosis; processes central to normal endometrial function. In an effort to confirm expression patterns which may suggest a functional role, the expression of sst1–5 in human endometrium from fertile and subfertile women was quantified. Methods: Histologically normal endometrium from the proliferative (n 11), secretory (n 8) and menstrual (n 7) phases of the cycle was analysed by semi-quantitative immunohistochemistry (IHC) to determine the cellular location and relative staining densities of sst1–5. Furthermore, mid-secretory endometrial samples were collected from infertile women prior to an IVF cycle and sst mRNA expression was assessed by quantitative PCR (qPCR). Results: Positive staining density demonstrated by IHC was significantly higher for sst2 (p 0.0001) and sst3 (p 0.0001) in endometrial epithelium during the proliferative phase, and for sst1 (p 0.001) in the epithelium of the early secretory phase. However, sst4 and sst5 were infrequently expressed. Expression of sst mRNA was demonstrated in mid-secretory endometrium by qPCR, and quantification appeared to vary according to diagnosis of infertility, as sst 1 and sst 3 mRNA were more frequently expressed in unexplained infertility. Sst1 expression was also higher in the endometrium from those with a positive pregnancy © 2013 The British Fertility Society e30 Abstracts following IVF (p 0.026). Conclusion: This study demonstrates that all five sst are expressed by human endometrium at gene and protein level, and furthermore the pattern of expression shows cyclical variation. In addition, the quantitative gene expression in mid-secretory endometrium relates to fertility outcomes. This suggests a possible role for somatostatin and its receptors in endometrial function which warrants functional validation. B5.6: Cycle scheduling with oral contraceptive pills vs. oral estradiol valerate: a randomized, controlled trial ERIK HAUZMAN, AZUCENA ZAPATA, ALFONSO BERMEJO, ANTONIO REQUENA, ANTONIO PELLICER & JUAN ANTONIO GARCÍA VELASCO Instituto Valenciano de Infertilidad (IVI), Madrid, Spain Introduction: Cycle scheduling can improve the organization of assisted reproduction units by equally distributing the workload along the week and avoiding its overload. Oral contraceptive pills (OCP) and oral estrogens have been used with good results in GnRH antagonist protocols, but there are no controlled trials comparing these options. Our objective was to compare the use of OCP versus oral estradiol (E2) valerate for cycle scheduling in IVF treatments performed with the GnRH antagonist protocol. Material and Methods: Regularly cycling women under 39 years, with BMI 30 kg/m2, basal FSH 10 IU/l, E2 60 pg/ml and 2 previous IVF attempts were enrolled. Patients with a history of low response to controlled ovarian hyperstimulation (COH), ovarian surgery, endometriosis or polycystic ovarian syndrome were excluded. Fifty patients received OCP (30 mcg ethinyl estradiol/150 mcg levonorgestrel) for 12–16 days, starting COH on post-pill day 5, whereas 50 patients received E2 valerate (4 mg p. o.) for 5–12 days, starting on day 20 of the previous spontaneous cycle and initiating COH the day after stopping E2. Patients were randomized at the time of cycle planning. Results: Groups were comparable in age (34.4 3.5 vs. 34.8 3.2 years, mean SD), BMI (22.3 3.7 vs. 20.9 2.7 kg/m2), and previous IVF attempts. As expected, more days of pre-treatment with OCP than with E2 (16.5 2.7 vs. 7.8 1.9 days, P 0.001) were necessary before starting stimulation. No significant differences were observed in cancellation rate (6.0% vs. 4.0%), fertilization rate (64.0% vs. 61.3%), number of top quality embryos (3.0 2.2 vs. 3.0 2.4), number of transferred embryos (1.6 0.7 vs. 1.4 0.8), implantation rate (34.4% vs. 36.6%), pregnancy rate per started cycle (58.3% vs. 54.8%) or miscarriage rate (3.1% vs. 16.0%). Conclusions: Comparable outcomes can be obtained using OCP or oral estradiol valerate to schedule GnRH antagonist cycles in IVF. POSTER PRESENTATIONS Sperm P001: Relevance of sperm DNA fragmentation index in a clinical setting MARIE-CHRISTINE DE TAVERNIER, SHARON CORCORAN, EVELYN COTTELL & MARY WINGFIELD Merrion Fertility Clinic, National Maternity Hospital, Dublin, Eire Background: Controversy exists as to the value of and indications for DNA fragmentation testing. Aim of study: To assess whether performance of a DNA fragmentation Index (DFI) influences clinical practice in an ART clinic. Methods: All patients had had at least one previous semen analysis (SA) and sperm preparation as per WHO 2010 recommendations. Those planned for IUI or IVF treatment (but not ICSI) had a DFI test using the SpermComet assay (normal and suitable for IUI 25%, abnormal but suitable for IVF 25–50%, require ICSI 50%). The number of cases changing from IUI to IVF or IVF to ICSI, based on DFI results was calculated. Other clinical criteria were correlated with DFI results. Results: A total of 107 men had DFI performed. 24 (22%) were classified as normal, 81 (76%) were abnormal but 50% and 2 (2%) were 50%. There was no significant difference in medical, smoking or alcohol history between the groups. The table shows the correlation between treatment recommendations based on initial SA and preparation and subsequent DFI. Human Fertility Abstracts e31 DFI Normal SA Sperm factor suitable IUI Sperm factor suitable IVF 25% n 24 25–50% n 81 50% n2 18 4 2 60 10 11 2 0 0 Based on a combination of female fertility factors (e.g. endometriosis, tubal disease) and initial SA, couples were planned for either IUI or IVF treatment. However, based on their DFI, 13/19 (68%) couples were transferred from IUI to IVF treatment and 2/88 (2.3%) from IVF to ICSI. Discussion: Our small pilot study indicates that a significant number 72/94 (77%) of those with a normal or mildly abnormal SA suitable for IUI will have a high DFI and may be better treated with IVF or ICSI. A smaller number of those listed for IVF will be switched to ICSI based on their DFI result. P002: Outcome of surgical sperm retrieval in correlation to FSH, testosterone levels and testicular volumes URMI SHUKLA, MONICA MITTAL, HAMODA HAITHAM, SAVVAS MIKE & NITISH NARVEKAR King’s College Assisted Conception Unit, King’s College Hospital, Denmark Hill, London, UK Background: Surgical sperm retrieval followed by intra cytoplasmic sperm injection (ICSI) has revolutionised the management of azoospermic men and allowed many of them to genetically father their offspring. The retrieval can be done electively to check for the presence of sperm or with egg retrieval to provide fresh sperm. The aim of this case series was to evaluate the success rates for surgical sperm retrieval, in correlation to FSH, testosterone levels and testicular volumes to establish indicators for successful retrieval. Materials and methods: We assessed 35 consecutive surgical sperm collections at our unit between December 2010 and January 2012. All azoospermic men had chromosomal analysis, serum follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone and testicular volume evaluated with an orchidometer. Data were retrieved from embryology databases and patients’ clinical notes. Results: 35 men underwent surgical sperm retrieval during. 14 men underwent percutaneous sperm extraction (PESA), 21 testicular sperm extraction (TESE) and 1 micro epididymal sperm aspiration (MESA). MESA was carried out under urology due to history of undescended testes and sperm was not retreived. All men who had PESA had sperm found that was suitable for ICSI. 3 of the remaining 18 men who had TESE did not have results available. Results for the remaining 15 are as follows: Table 1. Indicators of sperm retrieval in men under going TESE. FSH (IU/ml) 15 15–30 30 Sperm found Testosterone (IU/ml) Sperm found Testicular size Sperm found 7/10 (70%) 1/3 (33.3%) 0/2 (0%) 10 10–15 15 2/7 (28.6%) 3/4 (75.0%) 4/4 (100%) Small Normal 5/7 (71.4%) 5/8 (62.5%) Clinical pregnancy rates for PESA were 7/19 (36.8%). TESE sperm retrieval rates were 53.3% (8/15) and in cases where retrieved sperm was used clinical pregnancy rate was 50% (4/8). Conclusion: Significantly high FSH levels and low testosterone levels are associated with poor retrieval rates, while evaluation of testicular size, with an orchidometer does not seem to be a good predictor for retrieval. Our experience demonstrates that simple PESA procedures for men with obstructive azoospermia can be carried out with good retrieval rates. These findings, however, were retrospective and constitute a relatively small series, and this needs to be considered when interpreting the data. This information can be useful in counselling men undergoing the procedure and may help predict the likelihood of success. Our retrieval rates with TESE and clinical pregnancy rates are comparable to those from other studies and support TESE procedures being undertaken by gynaecologists in the fertility setting. © 2013 The British Fertility Society e32 Abstracts P003: Effective sperm preparation using migration-sedimentation: the Research Instruments MSC™ ERICA FOSTER Complete Fertility Centre Southampton, Princess Anne Hospital, Coxford Road, Southampton, UK Migration-sedimentation is a sperm preparation technique which harnesses both the ability of sperm to swim out from seminal plasma into culture medium and the property of sedimentation. Whereas sperm subjected to traditional swim-up methods are at risk of being returned to the semen layer due to gravity, migration-sedimentation exploits gravitational effects by allowing motile sperm to be collected in a separate compartment. Research Instruments’ Migration Sedimentation Chamber (RI MSC™) comprises a small well located within a larger, concentric plastic tube. Sperm which migrate from semen placed in the gallery eventually become harvested in the inner well. The RI MSC™ was trialled against the direct swim-up method on normozoospermic samples at Complete Fertility Centre Southampton. Equivalent volumes were used for both semen and media, and the incubation period was set at two hours. Preparation of semen in the RI MSC™ resulted in significantly higher motile sperm yields; 11 million versus 7 million for the direct swim-up (p 0.014). Whilst the RI MSC™ may not be ideal for use in the preparation of IUI samples, in which whole ejaculates are typically processed, or the preparation of ICSI samples, which benefit from being concentrated by selective washing processes such as density gradient centrifugation, it is appropriate for the recovery of sperm from good quality ejaculates for use in conventional IVF. Migration-sedimentation represents a means of achieving simple, quick and efficient sperm separation, and offers an alternative to the direct swim-up method. P004: Percutaneous or microsurgical epididymal sperm extraction as a diagnostic procedure for azoospermia: a comparative study STAMATIOS KARAVOLOS, JANANI IYER, LOUISE NEEDHAM, ELLA CLAPHAM & KEVIN MCELENY Newcastle Fertility Centre at Life, International Centre for Life, Times Square, Newcastle upon Tyne, UK Aims/Objectives: To compare sperm retrieval rates (SRR) in men with presumptive obstructive azoospermia undergoing diagnostic percutaneous or microsurgical epididymal sperm aspiration (PESA or MESA). To investigate the success of MESA to recover sperm after failed PESA, and to determine the chances of requiring testicular sperm extraction (TESE), if PESA or MESA failed to recover sperm suitable for storage. Content: We analysed SRR outcomes by PESA and MESA over a 2 year period in our unit. Men with a history of vasectomy were excluded. Relevance/Impact: MESA is more invasive and technically more difficult to perform, but may offer higher SSR. Outcomes: 20 men (mean age: 36 yrs, mean pre-operative FSH: 4.4 IU/L, mean testicular volume: 22.3 ml) underwent PESA (19 bilateral, 1 unilateral). The SRR was 55% (11/20) and the mean number of straws of sperm recovered was 3.72 3.13 (mean SD). TESE was performed in 45% (9/20) with an SSR of 44.4% (4/9). Diagnostic MESA (7 bilateral, 13 unilateral) was performed in 20 men (mean age: 35 yrs, mean preoperative FSH: 4.04I U/L, mean testicular volume of 22.7 ml). The SSR was 80% (16/20), and the mean number of straws of sperm recovered was 8.33 6.16 (mean SD). TESE was performed in 20% (4/20) and sperm recovered from 3 (75%). 9 out of 20 men undergoing MESA, had previously undergone failed PESA, and in 67% (6/9) of them, usable sperm was subsequently recovered from MESA without the need for testicular biopsy. Discussion: Although less invasive and more easily performed, PESA retrieved lower quantities of sperm than MESA (3.72 vs 8.33 straws, p 0.02) and patients undergoing PESA had a higher chance of requiring a testes biopsy (p 0.043). In our centre MESA has become the preferred method of sperm recovery in men with presumptive obstructive azoospermia. Human Fertility Abstracts e33 P005: An investigation into the effect of storing sperm in the dark between the time of preparation and insemination KATHRYN GARDNER1, SUE MONTGOMERY1, ALISON CAMPBELL1 & SIMON FISHEL2 1 Care Fertility Manchester,Victoria Park, Manchester, UK and 2Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Introduction: Current theories suggest wavelengths of light within the visible range enhance hyperactivated motility of sperm and capacitation. This is believed to occur through production of reactive oxygen species and nitric oxide; protein kinase A activation and Ca2 influx. Data at ESHRE 2012 demonstrated that storage of sperm in the dark may have contributed to the complete absence of failed fertilisation through the prevention of early capacitation (Ryder, 2012). A box was installed in our laboratory for the dark storage of prepared sperm samples prior to insemination, with the aim of improving the fertilisation rate and reducing failed fertilisation. Method: A retrospective analysis was performed of all IVF and ICSI cycles from 1 June–31 August 2012. The fertilisation and failed fertilisation rates were assessed 6 weeks before and after utilisation of the box, beginning on 16 July. Prior to 16 July, samples were stored in the laboratory with fluorescent background lighting with a diffuser and UV sleeve. Results: 20 IVF and 99 ICSI “light” cycles were performed from 1 June–16 July compared to 39 IVF and 108 ICSI “dark” cycles from 16 July–31 August. The IVF fertilisation rates for “light” and “dark” were 74.19% and 68.79%, whilst those for ICSI were 66.72% and 64.03%. The “light” failed fertilisation rates were 0% for IVF and 2.02% for ICSI compared to “dark” 2.56% (IVF) and 3.70% (ICSI). The light and dark differences in the fertilisation rates were found to be insignificant by chi squared analysis. Conclusion: In contrast to Ryder’s study, storage of sperm in the dark does not significantly affect the fertilisation rates, compared to storage of the samples in the light. P006: A retrospective study analysing outcome using fresh and frozen sperm ELLEN CATER, KATHRYN BERRISFORD, LUCY JENNER & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Aim: To assess and compare the fertilisation, embryo transfer and clinical outcome of fresh ejaculated sperm to thawed sperm and fresh SSR sperm to thawed SSR sperm. Relevance: It is widely reported that fresh and frozen thawed sperm used for ICSI have the same potential for pregnancy. This study aims to analyse data from a single clinic to more effectively advise patients clinically. Method: Data from 2386 cycles carried out between January 2009 and March 2012 were analysed. Cycles were divided based on the sperm source; fresh ejaculated sperm was compared to frozen thawed ejaculated sperm; fresh SSR sperm was compared to frozen thawed SSR sperm, and further division was performed based on SSR type. Fertilisation, number, achievement of an embryo transfer, positive βhCG and clinical pregnancy rate was analysed statistically using Chi square test with Yates correction. Results: Significant differences were found in 3 comparisons. The number of patients that achieved a transfer when using fresh ejaculated sperm was lower than when frozen was used (268/409 and 49/57 respectively p 0.05). Fertilisation rate of frozen thawed SSR sperm was found to be significantly lower (p 0.05) than fresh SSR sperm (619/1229 and 501/883 respectively). When analysing SSR sperm by type, this was found to be the case in PESA sperm (292/446 fresh, 310/592 frozen, p value 0.0001, but not in TESA or TESE. Conclusion: Our data suggests that on the whole, frozen and fresh sperm are comparable with the exceptions mentioned above. P007: Ultra rapid Freezing of seminal plasma free or density gradient prepared sperm testing sucrose as an alternative cryoprotectant FEDA ALJASER, TRACEY KOHUT, JAMES HOPKISSON, BRUCE CAMPBELL & MATHEW TOMLINSON University of Nottingham, Nottingham University Hospital, Nottingham, UK © 2013 The British Fertility Society e34 Abstracts Introduction: Sperm cryopreservation by slow freezing has changed little over the past 40 years, often resulting in poor survival rates whereas, in contrast, new methodologies of rapid freezing of oocytes and embryos have proved efficacious. The objectives of this study were to determine whether rapid sperm freezing is effective and whether it can be enhanced by sperm preparation or use of less toxic cryoprotectants. Methods: Initial experiments compared two methods of rapid freezing, liquid nitrogen (LN) or dry ice (DICE) using a standard glycerol cryoprotectant (12% v/v). This comparison between methods was then repeated for both semen and density gradient prepared (DGP) samples. The effect of seminal plasma removal prior freezing was tested and followed by a further series using sucrose as an alternative to glycerol (Isachenko et al. 2011). To ensure consistency of sperm assessment, endpoint analysis (postthaw motile concentration) was measured using computer assisted semen analysis (CASA) and the proportion of sperm remaining progressively motile post-thawing (yield%) was calculated. Results: Post thaw motility was preserved by LN (22.1%) and DICE (23.1%), but was enhanced further if samples were prepared by density gradients (51.9%, 42.53% respectively). Freezing by LN as opposed to DICE tended to result in higher progressive motility (n 20; 24.6 3.2% versus 20.2 2.5% mean SEM) and this observation, along with its technical simplicity, led us to adopt the LN method for following studies. Seminal plasma removal yielded poorer motility than DGP sperm (38.2% versus 51.9%) but was superior to unwashed sperm (35.1%). Samples frozen rapidly using glycerol yielded significantly increased survival compared to sucrose (n 23; 71.9 14.5% versus 26.6 7.8%; P 0.001). Conclusion: These pilot experiments have identified that ultra-rapid freezing is effective and could be a promising new development in sperm cryopreservation. Further work is required to optimize protocols and compare directly with slow freezing. P008: Evaluation of a new sperm selection medium LAURA WALKER, MARTYN BLAYNEY, PHIL SNELL, VAL SHAIKLY & GIDEON VERWOERD Bourn Hall Clinic, Bourn, Cambridge, UK Aims: Current practice within our clinic is to carry out intra-cytoplasmic sperm injection (ICSI) in fertilisation medium only. The aim of this study is to investigate the impact of using a new sperm selection medium, SpermSlow, to ascertain if any improvement is seen. Content: 126 patients having treatment with ICSI from 1st March–30th August 2010 were included in this data set. Oocyte injection was performed with or without SpermSlow™, and the results compared for oocyte viability, fertilisation, early pregnancy loss (EPL) and clinical pregnancy rates. Relevance/Impact: SpermSlow is a viscous medium containing hyaluronic acid, used for selecting mature, viable and morphologically normal spermatozoa during the ICSI procedure. It acts as a natural and biodegradable alternative to PVP, aiding the immobilisation of progressively motile spermatozoa. It may also confer an advantage during the injection technique, allowing for smoother manipulation. Outcomes: For oocytes injected using fertilisation medium only and those using SpermSlow, there was no difference observed in the fertilisation rate (66.4% vs. 64.4% respectively), nor the clinical pregnancy rate (42.6% vs. 40.5%). The post-ICSI damage rate was significantly reduced by the use of SpermSlow (8.8% vs. 14.5% without, p 0.01). The use of SpermSlow appears to lower the EPL rate (33.3% vs. 11.8%). Discussion: This study indicates the EPL rate is reduced by the use of SpermSlow, although the difference was not significant (p 0.05) due to the low number of patients. The post-ICSI damage rate is significantly reduced, and added to practitioner preference, SpermSlow is now used for all ICSI procedures within the clinic. P009: A laboratory audit to investigate the relationship between the total motile sperm count inseminated for intrauterine insemination and the clinical pregnancy rate URVASHI SARNA, SUZANNE CAWOOD, ALPESH DOSHI & PAUL SERHAL The Centre for Reproductive and Genetic Health, Eastman Dental Hospital, London, UK Objective: To determine the impact of the total motile sperm count (TMSC) on clinical pregnancy (CPR) rate after intrauterine insemination (IUI) using ejaculated partner sperm. Method and design: A retrospective analysis of 1,157 treatment cycles after stimulated and non stimulated IUI treatment using partner ejaculate sperm at the Centre for Reproductive and Genetic Health (CRGH) clinic, London between 01-01-2009 to 31-12-2010. Outcome measures: CPR is defined as the presence of foetal heart activity identified by ultrasound examination at 6 weeks gestation. Results: A total of 120 clinical pregnancies were achieved with a CPR/insemination of 10.4%. CPR for the TMSC groups 1 106, 1–2 106, 2–5 106, 5–10 106, 10–20 106 and 20 106 were 2.2%, 14.9%, 8.6%, 12.2%, Human Fertility Abstracts e35 9.9% and 10.6% respectively. Conclusion: There was no statistically significant relationship between the TMSC and the CPR when TMSC was 1×106. However, there was a statistically significant increase in the CPR for the subgroup of 1–2 106 in comparison to 1 106. We concluded that 1 106 was the minimum TMSC threshold post sample preparation for IUI treatment to be an efficient treatment option for selected patients. This supports our current in-house clinical protocols for offering IUI treatment. P010: Evaluation of the suitability of a Computer Assisted Semen Analysis (CASA) System for semen analysis LYNDSEY ZUJOVIC, SOPHIE BREARLEY, SHYAW AHMED, JAMES HOPKISSON & BRUCE CAMPBELL Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE], Division of Obstetrics and Gynaecology, School of Clinical Science, Nottingham, UK Aim: To assess the reliability, repeatability and cost effectiveness of a CASA system for routine semen analysis. Method: Repeatability of both CASA and manual methods of semen analysis were compared by performing 5 duplicate assessments of 10 different semen samples, assessing motility and concentration in each case. In order to compare the reliability, 55 semen samples were analysed for concentration & motility via both methods and the limits of agreement (LOA) were assessed. Finally the cost of performing manual and CASA were compared. Results: Duplicate concentration & motility assessments of the same samples showed a high level of correlation between the manual method and CASA, intra-class correlation (ICC) 0.962 (CI 0.85–0.99) and ICC 0.929 (CI 0.71–0.98) respectively. Coefficients of variation (CV) for the concentration of the 10 samples analysed showed that for the manual method the mean CV was 5.1% (range 3.5–8.9%) and for CASA the mean CV was 5.4% (range 1.6–8.1%). For motility the mean CV with the manual method was 6.6% (range 1.4–14.3) and for CASA was 8.7% (range 2.1–14%). Of the 55 separate semen samples assessed the mean concentrations obtained with the CASA and manual method were 48.6 M/ml and 50.2 M/ml respectively (p 0.433). There was however a significant difference between the average motility measures, p 0.009 and Bland and Altman LOA showed a mean difference between the two methods of 2.730. From a cost analysis perspective, the average cost of CASA test was £32.22 and £40.25 for a manual semen analysis. Discussion: No significant difference was observed between the concentration assessments obtained via CASA or the manual method. Comparisons between motility assessments were subject to greater variation between the two methods, with the greatest difference being seen at levels of motility 50%. From a cost perspective, CASA provides a more cost effective method of SA than the standard manual method P011: Validation of a new computer aided semen analysis (CASA) system for routine clinical use; a prospective comparative study STACY WHEAT, KATIE VAUGHAN & STEPHEN HARBOTTLE Cambridge IVF, Trumpington, Cambridge, UK Introduction: The precision and accuracy of manual semen analysis (MSA) is highly operator and laboratory dependant. In theory, CASA should allow a cost-effective semen analysis which is reproducible and reliable. We compared sperm concentration and motility using ‘The Sperminator’ with the World Health Organisation 2010 (WHO, 2010) gold standard method. Materials and Methods: Our CASA system was calibrated against a validated system using an Accubead suspension of pre-determined concentration. The same suspension was used to validate CASA against MSA in the laboratory. Once validation had been confirmed, CASA was performed alongside MSA for 50 semen analyses and is ongoing. Concentration was assessed for all samples (group 1) and those containing 80 mill/ml (group 2) and 80 mill/ml (group 3). Sperm motility was assessed in four categories: rapid progressive (A), forward progressive (B), non-progressive (C) and immotile (D). Comparisons between CASA and MSA were performed using the Wilcoxon Signed Rank test. Results: Mean concentration differed significantly when comparing CASA and MSA in group 1 (69.2 Mml-1 50.0 vs. 54.7 Mml-1 34.4 p 0.0001) and group 3 (123.8 Mml-1 34.9 vs. 87.9 Mml-1 24.6 p 0.0001); however in group 2 no significant difference was observed (37.4 Mml-1 21.8 vs. 35.4 Mml-1 22.3 p 0.28). Mean motility differed significantly when comparing CASA and MSA in categories A (37.1% 17.2 vs. 32.7% 14.9 p 0.05) and B (12.9% 8.1 vs. 16.8% 6.5 p 0.05); however when combined progressive motility (A B) was compared, no significant difference was observed (50.0% 15.1 vs. 49.6 18.2 © 2013 The British Fertility Society e36 Abstracts p 0.75). Similarly, mean motility in categories C (11.4% 5.8 vs. 11.5% 4.1 p 0.66) and D (38.1% 12.9 vs. 39.0% 18.9 p 0.81) were comparable for CASA and MSA. Conclusion: Our data demonstrate that samples containing a concentration of 80m/ml sperm benefit from dilution when using CASA; this finding is consistent with the manufacturers recommendations. The results highlight that human operators have difficulty distinguishing between A and B grade motility in MSA. Our results suggest that ‘The Sperminator’ can assess sperm concentration and motility to a standard comparable with WHO 2010. P012: The effects of Ginger on rat spermatogenesis and sperm parameters of rat SAMAN AYOUBI1, AMIR AFSHIN KHAKI1 & ARASH KHAKI2 1 Department of Anatomical Sciences, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran and Department of Veterinary Pathology, Islamic Azad University,Tabriz Branch,Tabriz, Iran 2 Background: Ginger rhizome (Zingiber officinale R., family: Zingiberaceae) is used medicinally and as a culinary spice. Objective: Medicinal use of ginger dates back to ancient China and India. Ginger and its constituents are stated to have antiemetic, antithrombotic, antihepatotoxic, anti-infl ammatory, stimulant, cholagogue and antioxidant. It has been used since ancient time as a medicinal and food produce since it contain antioxidative and androgenic activities and may have a useful effect on spermatogenesis and sperm parameters. Materials and Methods: Wistar male rat (n 30) were allocated into three groups, control (n 10) and test groups (n 20), that were subdivided into groups of 2 that received ginger rhizome powder (50 and 100 mg/kg/day) for 20 consecutive days. Animals were kept in standard conditions. On day 20 the testes tissue was removed, sperm collected from the epididymis and prepared for analysis. Results: Serum total testosterones was significantly increased in experimental group that had received 100 mg/kg/day Ginger (p 0.05). In addition the percentage of sperm viability and motility in both test groups significantly increased (p 0.05) in comparison to controls, whereas, LH, FSH hormones, sperm concentration, morphology and testes weights in both experimental and control group were similar. Conclusion: Administration of 100 mg/kg/day of ginger significantly increased sperm percentage, viability, motility and serum total testosterones. This suggests that ginger may hold promise in enhancing sperm viability. P013: MicroTESE outcomes at a tertiary referral centre JANANI IYER, STAMATIOS KARAVOLOS, ELLA CLAPHAM, LOUISE NEEDHAM, MEENAKSHI CHOUDHARY & KEVIN MCELENY Newcastle Fertility Centre at Life, International Centre for Life, Times Square, Newcastle upon Tyne, UK Background: Whilst widely performed in North America and elsewhere in Western Europe, MicroTESE (microsurgical testicular sperm extraction) is not currently widely available in theUK. Aims: To evaluate the outcomes of microTESE procedures performed at our unit, thereby enabling couples to make a more informed choice regarding sperm retrieval, fertilization and clinical pregnancy rates. Methods: 30 microTESE procedures were performed by a single surgeon between Jan 2010 to July 2012. Data was collected from departmental databases and analyzed on an excel spreadsheet. Results: The average age of patients was 33 yrs and the mean female partner age was 30 yrs. Mean pre-operative FSH and testicular volumes were 19.1 11.5 u/l and 15 7.5 mls (mean SD) respectively. The complication rate and the post operative admission rate was 0%. The surgical sperm retrieval rate was 43% of which, 84% had sperms that were suitable for treatment. Although 50% of mature oocytes injected with retrieved sperms were fertilized, all couples undergoing ICSI (intracytospasmic sperm injection) treatment obtained embryos for transfer. The clinical pregnancy rate was 23%. Following counseling, 70% of couples had opted for donor back-up in the eventuality of no sperm being recovered. 47% of those needed donor treatment due to poor quality of sperm or failure to retrieve sperm. 55% of couples who declined donor back-up stopped treatment due to lack of retrieved partner sperm. Conclusion: Sperm was recovered in nearly half of the men undergoing microTESE. Our data shows that if sperm is found, there is a high likelihood of undergoing ICSI treatment. Our clinical pregnancy rate of 23% would be acceptable to most couples who are looking to conceive through assisted production techniques. MicroTESE remains Human Fertility Abstracts e37 a useful and safe intervention in men with non-obstructive azoospermia. The expectations of couples undergoing microTESE treatment warrant further research. P014: Impact of sperm morphology, motility and concentration on fertilisation rates and outcomes in IVF cycles CATHERINE TURNER, JACQUELINE CRITCHLOW, KATHY CUMMING, DANIEL BRISON & GREGORY HORNE Central Manchester University Hospitals NHS Foundation Trust, Department of Reproductive Medicine, Old St Mary’s Hospital, Manchester, UK Whether to recommend IVF or ICSI treatment is a common conundrum for clinics especially where semen parameters are borderline. With ICSI being more expensive, demanding more expertise, laboratory time and involving greater risk than conventional IVF it is important to ensure patients are not offered ICSI “just in case”. Following an increasing proportion of ICSI cycles at our unit leading to increased laboratory workload, we decided to re-evaluate our IVF/ICSI selection criteria with particular reference to sperm morphology, previously absent from routine selection criteria. With the aim of helping to assess the requirement of morphology analysis prior to and during treatment, and allow re-evaluation of our selection criteria, a retrospective study was undertaken to evaluate correlations between sperm concentration, motility and morphology on fertilisation rates and outcomes in conventional IVF cycles. Data were collated from couples undergoing their first IVF cycle in 2010 (281 couples, 180 with all data available). Strict morphology, concentration and motility were assessed in a referral semen analysis and concentration and motility assessed pre and post preparation at time of treatment. Data were analysed to evaluate correlation and significance of single semen parameters with fertilisation rate and cycle outcome. Initial findings showed no correlation or significant difference between motility or concentration on fertilisation rate or cycle outcome for the pre and post prepared treatment sample. A slight positive correlation was observed between morphology and fertilisation rate (p 0.055), without effect on cycle outcome. Concentration and motility of referral and treatment samples were well correlated (p 2.2 10–16, 0.0044). Analysis is ongoing to assess the interaction of multiple variables but provisional data indicate that morphology should be considered and the concentration and motility cut-off values could be relaxed to the revised WHO 2010 values in our IVF/ICSI selection criteria. P015: A case study reporting Schistosoma haematobium miracidia detected in semen and the outcome on treatment decision CLAIRE SHEARER, SIMON FISHEL, ALISON CAMPBELL, ADEL SHAKER, RACHEL SMITH, CATH DREZET, ABIGAIL BURCHILL, CLAIRE BARTON & SARAH FOLEY Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK The couple first presented with four years primary infertility. The male partner was Normozoospermic. After several unsuccessful IVF attempts the couple presented for a donor oocyte cycle. On the day of treatment the embryologist discovered three living monocellular organisms on the Makler counting chamber. Treatment was postponed and six mature oocytes were vitrified to allow investigation into the nature of the infection and related implications for the patients, their treatment and any resulting pregnancy. The male patient was later confirmed to have a Schistosoma haematobium infection. This was thought to have been acquired some years earlier while wading barefoot in an infested lake (Milawi). This chance finding was extremely unusual as the organism is not thought to reside in the male reproductive tract but was more likely to be in the bladder and therefore the ovae and miracidia were probably flushed from the urethra upon ejaculation. Ovae may be passed intermittently or in small amounts, perhaps the reason this had not been observed in previous treatment cycles. He was treated and cleared of the infection by antiparasitic medication. The couple subsequently attended for their frozen oocyte ICSI cycle using a fresh semen sample. Five oocytes survived the warming process and all fertilised. Two day 3 embryos were replaced but sadly did not result in a pregnancy and none of the surplus embryos were frozen. This chance finding on the day of oocyte recovery resulted in the patients having an unscheduled oocyte © 2013 The British Fertility Society e38 Abstracts vitrification leading to subsequent ICSI, rather than a fresh IVF treatment. However, the patient was consequently cured of urinary schistomiasis which is often chronic, can cause pain, secondary infections and even kidney damage and cancer. P016: Quantitative immunofluorescent analysis of fertile human sperm suggests that levels of the oocyte activation factor, phospholipase C zeta (PLCζ), may be linked to male age WALAA RAMADAN1, CELINE JONES1, JUNAID KASHIR1, CARMEN NAVARRO2, JUAN DIAZ2, LUCY COLEMAN2 & KEVIN COWARD1 1 Nuffield Department of Obstetrics and Gynaecology, University of Oxford, Oxford, UK and 2Ferti-Aguerrevere, Caracas, Venezuela The fundamental process of oocyte activation in mammals is widely believed to be regulated by the spermspecific protein, phospholipase C zeta (PLCζ). When introduced into the oocyte at gamete fusion, PLCζ triggers a series of signalling mechanisms, controlled by oscillations in intracellular calcium, which initiate oocyte activation and early embryogenesis. Absence, reduced levels, or abnormal localisation patterns of PLCζ in human sperm have been linked to certain types of infertility. Previous studies have identified PLCζ in acrosomal, equatorial, and post-acrosomal regions of fertile human sperm, and discussed the possibility of differential functionality for such patterning. Previous work from our laboratory revealed notable variability in the total level and localisation pattern of PLCζ in human fertile controls, but whether this variance is associated with male age remains to be ascertained. Defining this relationship may provide important clues as to whether oocyte activation capacity also varies with age. In the present study, quantitative immunofluorescent microscopy was used to determine the total level and localisation pattern of PLCζ in human sperm samples acquired from fertile donors with informed written consent. Analysis involved 100 sperm cells per subject and data was categorised into four age groups [20–25, 26–30, 31–35 and 36 years of age]. Preliminary analyses indicated a significant reduction (p 0.05) in the total level of PLCζ in human sperm with advancing age, with no apparent relationship with localisation pattern. It would be desirable to increase the number of human donors recruited and to incorporate physiological tests of oocyte activation ability in order to confirm whether the observed reduction in total PLCζ with age is associated with impaired oocyte activation potential. Vitrification P017: A comparison of two closed vitrification devices SAMANTHA BURLEY-JACKSON, CLAIRE KAY, ALAN BIRKS & DEBORAH FALCONER Manchester Fertility Services, Bridgewater Hospital, Manchester, UK Objective: The survival rates of vitrified embryos have been widely reported to be better than conventional slowfreezing. This retrospective study aimed to compare the blastocyst survival, clinical pregnancy and implantation rate using two different closed vitrification devices, Cryopette® (Origio) and Rapid-iTM (Vitrolife). The choice of using a closed device instead of an open system was to reduce the risk of cross contamination during storage in liquid nitrogen. Materials and Methods: 162 patients undergoing blastocyst frozen cycles from April 2010 to August 2012 were included in the study. All blastocysts were vitrified and warmed in Irvine Vitrification and Warming media. Post thaw survival was confirmed by re-expansion of the blastocyst after 2 hours in culture. Survival, clinical pregnancy and implantation rate for patients vitrified in Cryopettes (n 99) and Rapid-i (n 63) were compared. Results: A significantly higher embryo survival rate was found using the Rapid-i (90%) compared to the Cryopette (70%), (p 0.0031). The lower survival rate with the Cryopette can be attributed to failure to retrieve the embryo from the device, a longer delay in exposure to the first warming solution, and embryos adhering to bubbles. No significant difference was found in clinical pregnancy rate with Rapid-i (31%) or Cryopette (25%). And the implantation rate per embryo transferred was identical for both devices (23%). Conclusion: Blastocyst survival rate was significantly increased with the Rapid-i device. This could be attributable to the rapid exposure of the embryo to the first Human Fertility Abstracts e39 warming solution with this device, in comparison to the Cryopette, and the ease of use of the device. Once successfully warmed and transferred, there was no significant difference in clinical pregnancy or implantation rate between the two devices. P018: A comparison of the efficiency of two different approaches to cryopreservation for ‘freeze-all’ scenarios LOUISE KELLAM, LUCY JENNER, SIMON FISHEL, KATHRYN BERRISFORD & RACHEL SMITH Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: Comparison of average number of 2PNs required per foetal heart (FH) in 2PN slow-freeze protocols, with ‘culture first and then freeze’ model. Method: Data from 2PN ‘freeze-all’ thaw cycles 2008–2012, with culture on to either day 2, 3, or 5, was used to determine the average survival rate (SR) and implantation rate (IR); the average number of 2PNs thawed per FH was calculated. To establish a model of ‘culture first and then freeze’ protocol, the fate of embryos from fresh cycles 2011–2012, where blastocyst transfer was intended, was analysed to determine the total number of freezable embryos created. Using this, SR and IR rates from day 3/5/6 embryos thawed in 2011–2012, the average number of 2PNs required per FH was calculated and compared to the above. Females 40 years, with identical freeze/thawing/culture protocols. Results: An average of 11.7 2PNs were frozen in 114 ‘freeze all’ cycles. Of 1019 2PNs thawed, 76.3% 2PNs survived. 199 embryos transferred either on day 2 (IR 26.7%), day 3 (IR 23.0%) or day 5 (IR 44.6%) giving an overall 29.6% IR. 71 embryos were refrozen. Average number of 2PNs thawed per FH 17.3. In the alternative model, the fate of 1426 2PNs from 292 IVF/ICSI cycles (average 5.6 2PNs/cycle) showed 128 freezable embryos developed on day 3, 274 on day 5, and 99 on day 6. Thaw outcomes from 80 vitrified day 5, 36 day 6 blastocysts, and 47 day 3 embryos, showed 80.0%, 69.4%, 63.0% SR, with 39.1%, 44.0% and 34.6 IR respectively. Using the extended culture, thaw and IR data, the average number 2PNs required per FH 9.9, statistically less than the 2PN slow freeze protocol (p 0.0006). Conclusion: The ‘culture first and then freeze’ is a more efficient approach compared to a 2PN freeze, and as a result likely to achieve higher success rates as a result. P019: A comparison of evaporation rates from different dewars in an assisted conception cryobank BRYAN WOODWARD, ANNA STOREY, KAREN CAMPBELL, SARAH KIRTON & ARIANNA D’ANGELO IVF Wales, University Hospital of Wales, Cardiff, UK Introduction: Cryopreservation of reproductive tissue and cells in liquid nitrogen is common practice in assisted conception. Dewar performance is crucial, to ensure that the low temperature (196 degrees C) is maintained. Dewar age and condition may affect on performance, especially in cryobanks that have been established for several years. The aim of this study was to independently assess evaporation rates in a large cryobank of liquid nitrogen dewars to establish if there was any variation in dewar performance. Material & Methods: The liquid nitrogen levels in 10 dewars were measured weekly for a period of 190 weeks from December 2008–August 2012. Depth measurements were taken using a graduated black cryorule inserted vertically into each dewar, through the liquid nitrogen to the base. The evaporation rate was then calculated for each dewar. Inter-dewar variation was assessed, as well as differences with respect to dewar volume, age and condition. Results: Dewar age ranged from 5 to 15 years. There were no significant differences in evaporation rates between any of the dewars. The dewar with the largest volume (Taylor Wharton LS48) showed the greatest range in evaporation rate. Six dewars of the same type (MVE XC47), showed very similar evaporation rates despite having different ages and one dewar having a cracked upper rim. There was a trend © 2013 The British Fertility Society e40 Abstracts to an increased evaporation rate in the oldest dewar (MVE SX35) which also had a neck core of reduced length, although this was not significantly different to the other dewars (P 0.05). Conclusions: Many assisted conception units rely on low level alarms to monitor dewar performance. Regular independent monitoring of evaporation rates further minimises uncertainty and can be a useful validation tool for indicating trends in dewar performance, particularly where there are concerns due to dewar age and condition. P020: Outcome of embryos vitrified at different stages STEPHANIE GADD & SARAH BENNETT Bath Fertility Centre, Roman Way, Bath Business Park, Bath, UK Objective: To compare the survival rates and implantation potential of vitrified-warmed embryos according to the day of cryopreservation. Method: This study is a retrospective data analysis of all frozen embryo transfer (FET) cycles involving the use of vitrified-warmed embryos in our clinic from January 2008 to August 2012 (n 1173 embryos in 507 FET cycles; 839 vitrified on Days 1–4 and 334 vitrified as blastocysts). From September 2009 all embryos vitrified at the blastocyst stage were collapsed using an ICSI needle just prior to vitrification. Results: Survival rates for embryos did not differ significantly for embryos vitrified on Days 1, 2, 3 and 4 (ranging from 88.3% on Day 1 to 95.4% on Day 4). When blastocysts were not collapsed prior to vitrification the survival rates were significantly lower (81.9% Day 5, 80.0% Day 6) than for Day 1–Day 4 embryos, however collapsing blastocysts prior to vitrification significantly increased the survival rates to 93.3% and 91.1% for Days 5 and 6 respectively. Clinical pregnancy rates per FET were not significantly different between any of the groups (Days 1–4, 24.2%; non-collapsed blastocysts, Day 5 26.4% and Day 6 16.1%; collapsed blastocysts, Day 5 28.3% and Day 6 27.1%). Implantation rates for embryos vitrified on Days 1–4 (17.5%) did not differ significantly from vitrified non-collapsed blastocysts (Day 5 20.5%, Day 6 15.3%), however collapsed blastocysts showed a significantly higher implantation rate (Day 5 24.1%, Day 6 25.2%). Conclusions: Embryos can be vitrified successfully at any stage from Day 1 to blastocyst. Vitrified blastocysts, if collapsed prior to vitrification, show increased survival and implantation potential. Day 6 blastocysts in particular appear to benefit from collapsing prior to vitrification, achieving the same implantation potential as blastocysts vitrified on Day 5. P021: The effect of blastomere loss during the freeze, thaw process on clinical pregnancy rate ASHLEY PAYNE, LYNNE NICE & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: To discover if the loss of blastomeres during the freeze, thaw process has a direct effect on clinical pregnancy rates. Methods: A retrospect analysis of 511 frozen embryo transfers undertaken at CARE fertility in 2011 was carried out. Comparisons were made between the clinical pregnancy rates for patients with fully intact embryos compared to patients with embryos which had lost up to 50% of blastomeres after thawing. Chi-squared tests were used to assess significance. Results: 511 Frozen embryo replacement cycles were analysed, 238 patients had a single embryo transfer, 273 patients had two embryos replaced. Patients who had a single embryo transfer had a clinical pregnancy rate of 19% with intact embryos and 18% for partially intact embryos (p 1.0000). A larger difference was observed between the two groups when 2 embryos were transferred. The clinical pregnancy rate with 2 embryos fully intact was 34% compared to 21% when both embryos had lost blastomeres (p 0.7510). There was no significant difference between clinical pregnancy rates with intact verses partially intact embryos transferred irrespective of whether a single or two embryos were replaced. Conclusion: Previous studies have found the loss of blastomeres to significantly decrease clinical pregnancy rates. This is not supported by the data in this study. The expected trends were not observed. No significant difference in clinical pregnancy rate was found between patients who had intact embryos replaced compared to the patients who had embryos transferred which had lost blastomeres. Our policy is to replace embryos with more than 50% of cells surviving. This is supported by the present study. Human Fertility Abstracts e41 P022: Determining the optimum post thaw culture period required to confirm the viability of slow-frozen blastocysts ELAINE TAYLOR & VIRGINIA BOLTON Assisted Conception Unit, Guy’s and St Thomas’ NHS Trust, London, UK It is common practice when assessing the viability of frozen-thawed blastocysts first to estimate the percentage of cells surviving the procedure, and second to evaluate re-expansion of the blastocoel during post-thaw culture. This study examines the relationship between commencement of re-expansion during post-thaw culture and implantation of transferred blastocysts. Blastocysts were thawed in 185 frozen embryo transfer (FET) cycles between October 2011 and June 2012. Thawing took place on the morning of the scheduled FET and blastocysts were assessed for re-expansion 60 and 120 minutes post-thaw. Endometrial preparation was carried out prior to transfer of 1 or 2 blastocysts. Where 2 blastocysts were transferred only those where both showed re-expansion at the same interval were included in the analysis. Implantation was defined as observation of fetal heart activity using ultrasound at 6 weeks following FET. Of 260 thawed blastocysts, 233 (89.6%) survived with 50% intact cells and were transferred. Of these 210 (90%) commenced re-expansion within 120 minutes of thawing. There was no difference in implantation rate (IR) between blastocysts that had already commenced re-expansion by 60 minutes (34/116, 29.3%) and those that commenced re-expansion after 60 minutes but before 120 minutes post-thaw (23/94, 24.5%, p 0.5) However the IR was significantly lower for blastocysts that showed no evidence of re-expansion up to 120 minutes post-thaw (1/23, 4.3%) compared with those that showed re-expansion, whether before 60 minutes or between 60–120 minutes post-thaw (p 0.008 and 0.04 respectively). These findings indicate that implantation potential for frozen-thawed blastocysts is associated with blastocoel re-expansion within 120 minutes of thawing. Analysis of these data has led to a change of practice in our unit. We now advise patients to agree to thaw additional embryo/s if thawed blastocysts with 50% cells intact post-thaw do not show commencement of re-expansion within 120 minutes of thawing. P023: Survival and viability of embryos using a closed vitrification device compared with controlled-rate freezing ZOE BRAME, LOUISE HYSLOP, SAMANTHA BYERLEY, EMMA DUNKLEY & MARY HERBERT Newcastle Fertility Centre At Life, Newcastle University, Newcastle upon Tyne, UK Introduction: Increasing evidence supports vitrification to cryopreserve embryos. However, most studies have been performed using open devices involving direct contact with liquid nitrogen, which may result in exposure of embryos to contaminants. We have addressed this problem by using a new closed system (Rapid-i, VitroLife). The aim of this study was to compare cleavage stage embryo survival and viability using this new closed vitrification device as opposed to conventional controlled-rate freezing. Methods: We performed a retrospective analysis of 99 frozen embryo transfer (FET) cycles comparing the cell survival of slow frozen (n 188) and vitrified (n 96) day 3 embryos. The implantation rate (IR), clinical pregnancy rate (CPR), and multiple pregnancy rate (MPR) were also compared. Statistical analysis was performed using the Chi-squared test. Results: No cellular damage (100% cell survival) was observed in 14.4% (27/188) of slow frozen compared with 67.7% (65/96) of vitrified embryos (P 0.001), and the proportion of embryos with 50% cell survival was 42.0% (79/188) and 93.8% (90/96), respectively (P 0.001). The IR of slow frozen embryos was 14.1% (9/64) compared with 19.3% (17/88) for vitrified embryos (P 0.20). The CPR/ET was 21.6% (8/37) and 28.3% (13/46) for slow frozen and vitrified embryos (P 0.25), respectively. The MPR was 12.5% (1/8) for slow frozen and 30.8% (4/13) for vitrified embryos (P 0.20). Discussion: Our results demonstrate that cellular damage is reduced in vitrified cleavage stage embryos compared with controlled-rate freezing. The significantly increased cell survival of embryos has led to improved embryo utilisation as the need for additional warming of embryos is obviated, thus maximising the number of potential cycles available to patients. Vitrified embryos also show a trend towards a higher IR and CPR. Our data add to the growing evidence in favour of vitrification and confirm that good cell survival can be achieved using a closed vitrification system. © 2013 The British Fertility Society e42 Abstracts Blastocysts P024: Blastocoel microsuction prior to vitrification significantly increases human blastocyst survival rate MAURIZIO POLI1, JENNY SPENCER2, KAREN TURNER2, TIM CHILD2 & DAGAN WELLS1 1 Nuffield Department of Obstetrics and Gynaecology, University of Oxford, Oxford, UK and 2Oxford Fertility Unit, Institute of Reproductive Sciences, Oxford Business Park North, Oxford, UK Introduction: The increasing implementation of elective single embryo transfer protocols has focused efforts on improving cryopreservation techniques in order to maximise fresh and frozen cumulative pregnancy rates. Vitrification, a common technique for the cryopreservation of surplus blastocyst stage embryos, results in a glassy, ice crystal-free state. Some authors argue that a large blastocoelic volume, due to its high water content, may interfere with the efficiency of vitrification. Aim: We set out to investigate whether emptying the blastocoelic cavity by microsuction before vitrification has an effect on the after-warming survival rate of Day 6 human blastocysts. Materials and Methods: Ten patients donated 27 surplus blastocysts to research. The embryos were graded on Day 6 with morphology 3Bc (Gardner’s criteria) and were not considered suitable for cryopreservation (low likelihood of survival/implantation post-thaw). All 27 embryos underwent blastocoel collapsing by microsuction using an ICSI needle. Collapsed embryos were vitrified following the media provider’s standard protocol, identical to that used for clinical samples. Vitrified blastocysts collapsed by microsuction were subsequently warmed and the survival rates compared to those of warmed clinical Day 6 embryos collapsed by manual pipetting at the time of vitrification. Results: Twenty-five out of 27 samples collapsed by microsuction (93%) survived the warming procedure showing full re-expansion within 18 hrs (21/27 within 1 hr, 23/27 within 2 hrs). Despite generally being of superior morphology, the samples vitrified for clinical purposes, with mechanical collapsing of the blastocoel, showed a significantly lower survival rate of 75% (136/181; p 0.05 Fisher’s exact test). Conclusions: Blastocoel microsuction allows full blastocyst collapse, improving survival rates when compared to embryos vitrified with mechanical collapsing. The extremely high survival rates achieved in poor quality embryos leads us to speculate that the application of blastocyst collapse to embryos of good morphology might be associated with even greater improvements in survival. P025: Blastocyst vitrification using a closed system: the St Mary’s experience HELEN HUNTER, J. DIANE CRITCHLOW, OLUTOPE ADENIYI, SIMONA SMUTNA, KEITH MCEVOY, CATHERINE TURNER, S. ROOMI AHMED, ELENA GISMANO, RUTH ARNESEN, ANNETTE LLOYD, YVONNE WILSON, GREGORY HORNE & DANIEL BRISON Department of Reproductive Medicine, St Mary’s Hospital, Manchester, UK Extended culture began at St Mary’s in August 2011. This audit was to assess the performance of our vitrification system by analysing recovery of viable embryos after warming and clinical pregnancy outcomes. Blastocysts were vitrified on day 5 or day 6 dependent on embryo growth, using Origio vitrification media and Vitrolife Rapid-iTM closed vitrification system. Patients were prepared for embryo replacement in a downregulated cycle. Results were compared to cleavage stage embryos slow frozen over the same time period (August 2011 to August 2012). A total of 60 patients underwent 64 thaw cycles. 37 patients had 39 blastocyst warming cycles. There were no failed thaws, and a mean of 1.1 embryos were thawed and 1.1 embryos replaced per cycle. 98% of warmed embryos were viable. 23 patients had 25 cleavage stage thaws, 8.7% of cycles were failed thaws. A mean of 1.8 embryos were thawed and 1.6 embryos replaced per cycle. 76% of thawed embryos were viable. Blastocyst warms gave positive hCG rate of 30.8% per cycle, compared to 20% for cleavage stage. The ongoing clinical pregnancy rate is 10% for blastocyst, 12% for cleavage stage (some outcomes outstanding). When results were analysed by IVF or ICSI, positive hCG rates were higher in the ICSI group following cleavage stage thaws (10% v 27%), but IVF embryos had better outcomes after blastocyst warming (35% v 26%). We have also found a high rate of biochemical pregnancy after ICSI blastocyst transfer. We found no difference in outcome between D5 and D6 blastocysts. We report an excellent recovery and Human Fertility Abstracts e43 viability rate after blastocyst vitrification using Origio Vitrification media and the Vitrolife Rapid-iTM closed storage system. Pregnancy rates are encouraging. The high rate of early miscarriage following ICSI blastocyst transfer needs further investigation. P026: Routine culture and cryopreservation of day 6 blastocysts – is it worthwhile? A National Survey AMY HATTON, VICTORIA GITTINS, SHARON BINNERSLEY, GEORGE HUGHES, ALISON LAVENDER & JASON KASRAIE The Shropshire and Mid-Wales Fertility Centre, Royal Shrewsbury Hospital, Mytton Oak Road, Shrewsbury, Shropshire, UK Introduction: Blastocyst culture is now routine, but national practice is not uniform. Extended culture to day 6 (D6) may be considered controversial due to possible associated epigenetic factors and a perceived decrease in viability of D6 blastocysts. Conversely, cryopreservation on D6 may reduce the number of fresh egg collections required, minimising risk to patients and cost to the healthcare economy, but do the benefits outweigh the potential risks? Method: National survey of practice, protocol and outcome. Results: 40 clinics responded 7.5% did not culture to blastocyst. 92.5% cultured to blastocyst in 5–80% of treatment cycles. 59.5% cultured to D6 if blastocysts were unavailable for transfer on day 5(D5) and between 0 and 90% of patients had fresh D6 transfers. Average clinical pregnancy rates (CPRs) for fresh D5 vs D6 transfers were 44.3% vs 25.7%. All clinics culturing to blastocyst cryopreserved. 89% cultured to D6 if no cryopreservation occurred on D5. 83.5% cultured remaining embryos to D6 whether or not cryopreservation occurred on D5. Average CPRs for cryopreserved D5 vs D6 blastocysts were 31% vs 28.3%. 89% believed culturing to D6 was worthwhile. Other data (e.g. culture system, cryopreservation method, carrier, media) were also collected and analysed. Conclusions: The majority of respondents cultured to, and cryopreserved, on D6. CPRs varied greatly between centres but were generally lower in fresh D6 vs D5 transfers. Nevertheless, results suggest that D6 transfer is worthwhile for patients without D5 blastocysts. Additionally, CPRs for cryopreserved D6 blastocysts were very similar to D5 and appeared slightly higher than fresh D6. Whilst it remains to be seen whether cryopreserved D6 blastocysts are more viable than fresh, it certainly appears that cryopreservation of D6 blastocysts is effective and beneficial to both patients and the healthcare economy by reducing risks from stimulation/ egg collections and overall costs whilst maximising cumulative success. P027: Is elective single blastocyst transfer the best option for all patients OMONIGHO OSEMEIKHIAN, CAITRIONA MEANEY, HELEN CLARKE, JANE SAXTON & RACHEL CUTTING Centre for Reproductive Medicine and Fertility (Jessop Fertility), Assisted Conception Unit, Jessop Wing, Level 1, Tree Root Walk, Sheffield S10 2SF, UK Introduction: Jessop Fertility’s Multiple Births Minimisation Strategy, involving blastocyst transfer and individual cryopreservation strategies, has enabled the HFEA’s 10% MBR target to be met. A contributing factor to this success is giving patients consistent and accurate information to strengthen the message that success rates can be maintained without exposing patients to the risks of multiple pregnancies. Methods: Data for fresh (n 452) and frozen (n 181) elective single blastocyst transfers (eSBT) and double blastocyst transfers (DBT) from January 2011 to June 2012 was retrospectively analysed. Fresh eSBT were divided into 3 age groups ( 37, 37–39 and 40–43 years). Frozen BTs were either rewarmed day 5 or 6 blastocysts or those cultured from thawed d3 embryos. Comparison between eSBT and DBT was performed using odds ratio (OR) with a 95% confidence interval. Significance was determined as P 0.05. Results: There was no significant difference in CPR between eSBT and DBT within any of the age groups having fresh BT. However, multiple pregnancy rates (MPR) for DBT were: 37 y, 46.3%; 37–39 y, 42.3%; 40–43 y, 11.8%. Although a higher CPR was observed in frozen DBT (43.3%) compared to frozen SBT (25.8%), this increase was not statistically significant at the 5% level. DBT was also associated with a MPR of 30.8%. Overall the monochorionic twinning rate was 1.4%. Conclusion: Based on our results, DBT does not significantly increase the chance of a pregnancy in a fresh or frozen cycle and, therefore, all patients having fresh blastocyst transfer are advised to have elective SBT. Patients having BT from frozen embryos are also encouraged to replace blastocysts one at time to eliminate the unacceptably high risk (approximately 1 in 3) of a multiple pregnancy. Patients are also able to vitrify supernumerary blastocysts derived from thawed d3 embryos. © 2013 The British Fertility Society e44 Abstracts P028: Blastocyst screening using Single Nucleotide Polymorphism (SNP) array with ‘Parental Support’ (Natera;California) technology to evaluate embryo ploidy status MARK SEDLER, ALISON CAMPBELL, KEITH JORDAN, LOUISE BEST, NATALIE BOWMAN & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Blastocyst screening using Single Nucleotide Polymorphism (SNP) array with ‘Parental Support’ (PS;Natera,California) technology to evaluate embryo ploidy status. Aneuploidy is the primary limiting factor to successful pregnancy outcome. Embryo chromosome abnormality rates range from 30% under 30 years of female age to 70% over 40 years. Day 5 and 6 blastocysts were biopsied using a laser assisted technique. Trophoblast cell were removed for analysis and cryopreserved. 24 chromosome assessment using Single Nucleotide Polymorphism (SNP) array with ‘Parental Support’ (PS) technology was employed. Blastocyts were vitrified pending results, with euploid embryos replaced in a subsequent frozen embryo replacement cycle. A total number of 26 cycles were started from 21 patients, with an average age of 36.6 years. In total, 110 blastocysts were biopsied. Of these, 36.4% (n 40) were euploid, 48.2% (n 53) aneuploid and 15.4% (n 17) showed a ‘no result’. 16 patients had transfer of euploid only embryos. An average of 1.1 embryos were replaced per embryo transfer. The initial pregnancy rate per embryo transfer was 68.75%, with a 50% ongoing clinical rate. 2 patients miscarried (12.5%) and 1 (6.25%) had a biochemical only pregnancy. PGS using SNP array with PS can accurately determine the ploidy status of blastocysts. Trophectoderm biopsy allows testing without compromising the Inner Cell Mass (ICM). This allows for the replacement of chromosomally euploid embryos, aiming to increase ongoing clinical pregnancy rates (CPRs) and decrease pregnancy loss. ‘Parental Support’ informs the parental origin of aneuploidy. This also allows for confidence level reporting of individual chromosome pairs. P029: Development of a rapid blastocyst comprehensive chromosome screening method using quantitative real-time PCR KATHARINA SPATH, ELPIDA FRAGOULI, MICHALIS KONSTANTINIDIS, MAURIZIO POLI & DAGAN WELLS Reprogenetics UK, Institute of Reproductive Sciences, University of Oxford,Oxford, UK Objective: Aneuploidy is common in preimplantation embryos leading to implantation failure, miscarriage or birth of handicapped children. Preimplantation genetic screening (PGS) techniques, such as array comparative genomic hybridisation (aCGH) assist in detecting chromosomally abnormal embryos generated by in vitro fertilisation (IVF). Considering that some aneuploidies are of paternal origin and the high prevalence of chromosomal mosaicism at the cleavage-stage, it can be argued that analysis of trophectoderm (TE) biopsies derived from blastocysts may represent the optimal strategy for predicting embryonic chromosomal status. However, current comprehensive aneuploidy screening methods require approximately 24 hours. Given that some blastocysts are not ready for biopsy until late on day-5 or even day-6, a 24-hour chromosome screening test may be incompatible with fresh embryo transfer, necessitating cryopreservation. Furthermore, application of conventional PGS techniques, significantly increases the costs of IVF treatment. For these reasons, we aimed to develop a rapid and less expensive blastocyst comprehensive chromosome screening method. Method/Results: The new approach is based on quantitative real-time polymerase chain reaction (real-time qPCR) and allows detection of aneuploidy by determining the relative copy number of 96 distinct target sequences spread across all 24 chromosomes. Initial work focused on lymphocytes derived from karyotypically normal males and females. After optimisation, the method was extended to the analysis of small numbers of cells from different cell lines with known aneuploidies (47,XY,13; 47,XY,18 and 47,XY,21). Finally, real-time qPCR was carried out on 50 TE biopsies derived from embryos previously shown to be aneuploid using aCGH, with results analysed blindly. Conclusion: This new methodology enables accurate detection of chromosome losses and/or gains in blastocysts within 4 hours, potentially allowing biopsy and transfer on the same day, avoiding the need for cryopreservation. Furthermore, the protocol has significant cost advantages over current PGS techniques. Human Fertility Abstracts e45 P030: Blastocysts: does size really matter? JO CRAIG, MUHAMMAD FATUM, TIM CHILD, ENDA McVEIGH & KAREN TURNER Oxford Fertility Unit, Institute of Reproductive Sciences, Oxford Business Park North, Oxford, UK Aim: Although it is known that blastocyst morphology affects pregnancy rates, it is unclear which factors are the most important i.e. degree of expansion, or inner cell mass (ICM) and trophectoderm grades. Methods: This study was based on retrospective analysis of 1070 single and 598 double blastocyst transfers in patients aged less than 38 years. The patients underwent ovarian stimulation followed by either conventional IVF or ICSI, and the blastocysts were graded immediately before transfer on day 5, according to Gardner & Schoolcraft 1999. The data was examined, changing only one morphological factor at a time, with double blastocyst transfers being included where both embryos were of the same grade. Grade 4Bb was used as the standard, as this was the most frequently seen grade. Chisquared was used to analyse the results. Results: Degree of expansion, when considered alone, was highly significant in predicting implantation∗. Although a trend can be seen, the quality of the ICM was only significant if the trophectoderm was poor (grade ‘c’). Morphology Expansion Morula 1 2 3Bb 4Bb 5Bb ICM 4Ab 4Bb 4Cb Trophectoderm 4Ba 4Bb 4Bc 4Cc Total Embryos Transferred Total Fetal Heartbeats Implantation Rate 23 92 163 123 421 19 2 27 64 55 235 15 8.7 29.3 39.3 44.7∗∗ 55.8 78.9 ∗p 0.001 (Chi2 50.1, df 5) 149 421 24 87 235 10 58.4 55.8 41.7 not significant 47 421 97 46 28 235 45 10 59.6 55.8 46.4 21.7∗∗ not significant Conclusion: An increase in blastocyst expansion correlates to increased implantation rate. However whilst the effects of the ICM and trophectoderm are more subtle, they do have a cumulative effect, such that a blastocyst in which both are poor will have a lower implantation rate than one with less expansion but otherwise better morphology (∗∗p 0.01). P031: Comparison of two different embryo grading systems for predicting blastocyst formation ESTEFANIA SEVILLANO, ORIOL OLIANA, PAUL WILSON, MARIA BONADA, STUART CAMPBELL, RI-CHENG CHIAN & GEETA NARGUND The Centre for Reproduction and Advanced Technology (Create Health Clinic), London, UK Background: The assessment of embryo viability is a key component in the IVF process. In order to assess embryo quality, several embryo grading systems have been developed. In this study we compared the predictive value of two different embryo grading systems. Purpose: To assess which D3 embryo grading system is more predictive of blastocyst formation. Methods: 874 embryos were evaluated on D3 using the inverted microscope. Two different grading systems were used to assess the morphology. System I assessed blastomere number and fragmentation grading embryos in four categories 1 (best) to 4 (worst). System II assessed the following parameters: cell number, rate of division, fragmentation, symmetry, multinucleation, compaction/adhesion, zona pellucida, blastomere shape, vacuoles, acytoplasmic ring. Embryos are classified in four categories according to these criteria from A (top quality) to D (poor quality). Results: Using System I, of 781 embryos classified as Grade 1 or 2, 357 (45.71%) reached blastocyst. Using System © 2013 The British Fertility Society e46 Abstracts II, of 333 embryos classified as Grade A or B, 213 (63.96%) reached blastocyst (95% CI, p 0.0). Using System I 189 (24.2%) embryos graded 1 or 2 developed into good quality blastocysts; whereas using System II 130/330 (39.04%) embryos graded as A or B formed good quality blastocysts (95% CI, p 0.000001). By assessing embryos with System II we can predict development of 2 good quality blastocysts from 5 A/B graded embryos on D3, whereas using System I we need 8 embryos graded 1/2 to obtain a similar number of good quality blastocysts. Conclusions: According to the data obtained using grading System II is superior in selecting embryos with higher blastocyst formation potential. This enables the team to make more accurate decisions regarding number of embryos to transfer and weather to extend the culture to obtain blastocysts. P032: A game of chance and influencing gender in single blastocyst transfer (SBT) KAREN DUEIGAN, G. EMERSON, C. HUGHES & E. MOCANU Human Assisted Reproduction Ireland, Rotunda Hospital, Dublin, Ireland Introduction: The aim was to examine whether culture conditions and the way an embryo is selected for transfer including methods of manipulation is affects the secondary sex ratio and influences gender ratio at birth in our eSBT embryo cohort. It was also intended to study associations of male and female deliveries with maternal and paternal age, sperm count and lifestyle factors-cigarette smoking and alcohol intake. Methods: A review was performed using patient charts and data collected via a Filemaker Pro based database and identified all patients who had in-vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) cycles and achieved a single blastocyst transfer between January 2008 and December 2010. The following parameters were measured: maternal and paternal age, blastocyst stage at transfer, laboratory procedure, reason for ART-male factor, female factor, combined male and female factor and unexplained, smoking status, and alcohol intake prior to treatment commencing. The number of male to female births was compared. The chi-squared test was used to analyse nominal variables. For the difference in live birth rates between male and female births, odds ratios and 95% confidence intervals were calculated. Results: There were significantly more males than females born to mothers in the under 30 and 30–34 age group (p-value 0.05). 19 female babies were born to mothers in the 38–40 age group compared to 10 male babies. This value was found to be significant (p-value 0.01). When the paternal age was under 30 the father to be, was three times more likely to have a male than a female (p value 0.005). When paternal age was greater than 40, more female babies were born than male babies in this age group (p value 0.003). The developmental stage of the blastocyst selected at transfer and the gender at birth were analysed. When cavitating morulas and early blastocysts were transferred more females than males were born (p-value 0.05). Transfer of a hatching blastocyst, the fastest growing embryo, was nine and a half times more likely to give rise to a male baby. The p-value had a level of statistical significance of 0.0002. Conclusion: Patients must be made aware that there exists a bias in the sex ratio after ART, however it is more likely due to patient profile, lifestyle factors at the time of conception and their individual embryo cohort characteristics. The hypothesis that blastocyst culturing is skewing the gender balance alone in either direction maybe premature. Embryology P033: Human embryo developmental dynamics in relation to maternal and paternal body mass index (BMI) CHRISTINE LEARY1,2, STEPHEN KILLICK1,2, HENRY LEESE2 & ROGER STURMEY2 1 The Hull IVF Unit, The Women and Children’s Hospital, Hull Royal Infirmary, Kingston-upon-Hull, UK and Hull York Medical School, Centre for Cardiovascular and Metabolic Research, University of Hull, Kingston-upon-Hull, UK 2 A key factor in successful IVF is the quality of the embryo selected for transfer. The relationship between BMI and embryo quality is relatively unknown, although lower pregnancy rates are frequently reported for overweight and obese couples. Subtle differences in embryo development could contribute to poorer outcomes. We have therefore compared the BMI of 89 patients at the time of IVF to blastocyst development (BD) in 518 embryos. In addition Human Fertility Abstracts e47 the developmental kinetics of 67 supernumerary embryos donated to research were analysed from time-lapse images captured at 5-minute intervals. A further 29 expanded blastocysts were fixed using chromatin-specific dyes to determine differential cell counts. Male obesity was associated with significantly higher rates of early embryo arrest compared to all other discordant pairings of male and female BMI (p 0.01); a finding which was independent of sperm quality. For those embryos capable of ongoing development the timelapse data showed no significant differences in the timings of blastulation and hatching (mean 159.4 17.4 hours post insemination) in relation to male or female BMI. However, blastocysts generated from obese parings had smaller diameters at the time of hatching (184 μm verses 244 μm p 0.05), increased zona thickness (6.9 μm verses 5.3 μm p 0.05) and an altered pattern of hatching, favouring projected escape over hydrostatic pressure. Total cell counts were significantly lower in embryos from obese pairings (101.1 verses 134.9 p 0.02), with a proportional decline in inner cell mass and trophectoderm cells. Male obesity contributed to reduced rates of BD, indicating a paternal effect on early embryo development. However the timing of blastulation or hatching was unrelated to male or female BMI. The reduced diameter of blastocysts from obese pairings may reflect the lower cell counts, possibly indicative of their lower viability. P034: ICSI training: The learning curve ANNE RICE Ninewells Hospital, Dundee, UK ICSI is now recognised as a routine technique and one of the most highly complex and demanding procedures to master. Success rates vary according to the skill and experience of practitioners, consequently applying pressure on trainee embryologists. Reasons for such variation include the technical difficulty associated with ICSI and the heterogeneity of cases such as the quality of the sperm and also the eggs, making the ICSI learning curve long and unpredictable. As it stands there is no official ICSI training programme and so experience is gained and performance is monitored in-house. Many factors affect the rate of attainment of competence, especially workload balance including the level of staffing and the level of activity in the lab. These factors may impact upon the time and the number of procedures it takes a trainee to learn the techniques, and then maintain the required level of performance. P035: A comparison of embryo culture in single step and sequential media CLAIRE KAY, ALAN BIRKS, SAMANTHA BURLEY-JACKSON & DEBBIE FALCONER Manchester Fertility Services, Bridgewater Hospital, Manchester, UK Objective: Use of a single step medium could reduce the time that the embryo is away from the incubator and streamline laboratory protocols. This study aimed to compare a single step medium (SSM) with a sequential media culture system already in use, with a view to implementing SSM if results were comparable or improved. Materials and Methods: Patients were randomly allocated for culture in either Irvine Single Step Media TM (n 71) or SAGE Quinn’s Advantage® sequential media (n 59), over a period of five months. Patients with 3 fertilised or aged 43 were excluded. Embryos were group cultured in 4-wells, and transfer occurred mainly on day 5 (77.6%). Embryos for replacement on day 3 or day 5 remained undisturbed in low oxygen culture until day 3. They were assessed and either replaced that day or cultured to day 5, dependant on stage and quality. Embryos cultured to day 5 in SSM were grouped according to quality on day 3 if necessary; embryos in sequential media were moved to a new dish with renewed pre-equilibrated media. All surplus embryos were cultured to day 5/6 and vitrified if good quality. Results: Mean age (SSM 36, sequential 35), fertilisation, cleavage and embryo utilisation rates (% of embryos transferred or vitrified) were comparable between the two groups. Clinical pregnancy rate in the sequential media group was increased (51.8%) compared to SSM (37.7%) but this was not statistically significant (p 0.14). Discussion: No statistically significant differences were identified in fertilisation rate, embryo utilisation rate or clinical pregnancy rate. Single step media allows for reduced time away from the incubator and less embryo manipulation if grouping is not required on day 3. Consumables and media costs are reduced and it is less labour intensive as it allows for a handling step to be removed on day 3. © 2013 The British Fertility Society e48 Abstracts P036: The formulation of a unit-specific embryo scoring algorithm using time-lapse imaging A. BARRIE1, R. GREGOIRE1, L. WALLACE2, K. SCHNAUFFER1, C. KINGSLAND1,2 & S. TROUP1,2 1 Association of Clinical Embryologists, Commerce Way, Colchester, UK and 2British Fertility Society, 22 Apex Court,Woodlands, Bradley Stoke, Bristol, UK Introduction: The advent of time-lapse imaging has necessitated the development of embryo scoring algorithms (ESAs) to facilitate embryo selection. In our centre, a published ESA has been used, however, very poor correlations between the ESA grade (A to D) and implantation rate (IR) were observed (A: 36%, D:40%). The aim of this study was to formulate a unit-specific ESA to identify those embryos with optimal implantation potential. Methods: Time-lapse imaging, using the EmbryoScope™, allowed observation of when two-cell (T2), three-cell (T3), four-cell (T4) and five-cell (T5) stages were reached and the intervals between these (T2-T3; T3-T4; T4-T5). 173 transferred embryos were assessed for each parameter and the IR determined. The range for each parameter was divided into centiles, and the IR calculated, providing a range of timings where IR was at its peak. Logistic regression analysis was performed to determine the importance of each parameter and a unit-specific ESA was generated assigning each embryo a new score (a to d). The IRs according to the published and unit-specific ESAs were then compared using Chi-square analysis. Results: Two parameters were found to be statistically significant as a result of the logistic regression analysis; T3-T4 (p 0.019), T4-T5 (p 0.043). T5 was included in the unit-specific algorithm although its influence was less important (p 0.239). Statistically significant differences in IR were observed between the two ESAs when considering the highest and lowest embryo classifications; A 36%(n 41) vs. a 68%(n 25)(p 0.0132) and D40%(n 10) vs. d-9%(n 22)(p 0.038). A comparison of the other classifications demonstrated a trend favouring the unit-specific ESA but did not reach statistical significance. Conclusion: These data demonstrate the importance of developing unit-specific ESAs when using morphokinetic parameters to make clinical decisions regarding an embryos fate. Although ESAs aid in determining implantation potential, pregnancies are still obtained from lower embryo classifications, and suggest that conventional grading should not be eliminated and a conjunctional approach should be taken. P037: Comparison of morphokinetic variables of implanted and non-implanted embryos: a search for exclusion criteria ALISON CAMPBELL1, CRISTINA FONTES, LINDEMANN HICKMAN2, SAMANTHA DUFFY1 & SIMON FISHEL1 1 Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK and 2Trinidad & Tobago IVF, Trinidad and Tobago Utilising the EmbryoScopeTM, we considered whether morphokinetics differed between embryos resulting in clinical pregnancy or failing to implant following ICSI to identify possible criteria for embyo selection/exclusion. Clinical pregncy was confirmed by foetal heart (FHB) at 7/1 week. 168 embryos were transferred before 96 hours post insemination (hpi), (early) and 161 after 96 hpi (late). We compared time (hpi) of divsion to two (t2), three, four, five and eight cells, duration of the second (cc2) and third (cc3) cell cycles, incidence of multinucleation at two and four cell stage and irregular cleavage (1 to 3 and 2 to 5 cells). Known Implantation Data value (KID) was defined per embryo from FHB. Where number of FHB was equal to or exceeded number of transferred embryos, KID was one. KID was zero if there was no FHB. Double embryo transfers resulting in one FHB were excluded. Mean implantation rate (IR) was number of embryos resulting in FHB over number of embryos transferred. Mean known implantation rate (KID-R) was number of embryos with implantation over number of known outcome transferred embryos. Where ET was 96 hpi, IR was 22% (n 191) and KID-R was 12% (n 135). Where ET was 96 hpi, IR was 30% (n 187) and KID-R was 24% (n 140). KID-R was compared by morphokinetic variables. Fishers test was used for significance of KID-R of embryos within and outside the group. Application of exclusion criteria; t2 32 hours, cc2 5 hours, cc3 5 hours increased KID rate from 12 to 22% for early and 24 to 31% for late transfer. For both early and late transfer groups there was a significant difference in KID rate between embryos excluded by the criteria and those not. The improvement potential from using these criteria may not be fully attainable in clinical practice due to lack of desirable embryos for some patients. Human Fertility Abstracts e49 P038: A retrospective data analysis of sequential versus non-sequential media in early embryo culture GERI EMERSON, C. HARRITY, C. HUGHES & E. MOCANU Human Assisted Reproduction Ireland, Rotunda Hospital, Dublin, Eire Introduction: Advances in the understanding of nutrient requirements of embryos, has led to the evolution of different chemical defined media into the assisted reproductive technology (ART) market. Over the last number of years the two approaches of 1. “Back to Nature” and 2. “Let the embryo choose” have been detailed and promoted by different commercial media companies. The aim of our study was to ascertain if there was a significant difference in outcome of embryos transferred on day 2/3, which were originally cultured in sequential, or non-sequential media. The main outcome were positive hCG/oocyte retrieval, (hCG/OR), Implantation Rate (IR) and Usage Rate (the total number of embryos transferred and frozen as a % of oocytes fertilised). Materials and Methods: We undertook a retrospective data base analysis of patients who attended for IVF or ICSI in the first 6 months of 2011 and 2012. We sub-grouped patients into 38 years of age and 38 years of age for both media used. Data were entered onto a Microsoft excel spreadsheet and analysed in SPSS v 18.0. Proportions were compared using Chi square test or Fishers exact test if an expected count was less than 5. Statistical significance was considered at p 0.05. Results: A total of 397 patients were analysed. 240 females were under the age of 38 yrs and 157 were over or equal to 38 yrs of age. In 2011 and 2012, for females under 38 years positive pregnancy test per oocyte retrieval was 47.6%, versus 49.1%, (p 0.897) implantation rate 32% versus 30%, (p 0.467) with a usage rate of 57% versus 53%, (p 0.563) respectively. For females over or equal to 38 years old, pregnancy per oocyte retrieval was 26.2% versus 29.3%, (p 0.713), Implantation rate of 13.6% versus 13.6%, (p 0.448) with a usage rate of 66.6% versus 59.1% (p 0.600), respectively. Conclusions: There was no significant difference observed between early embryo development in sequential or non-sequential media with regard to positive hCG/ oocyte retrieval, implantation rate and usage rate. P039: A retrospective comparison of polar body and blastomere biopsies in our PGS using aCGH program KATHRYN BERRISFORD, SIMON FISHEL, LUCY JENNER, ELLEN CATER, COLLEEN LYNCH & LOUISE KELLAM Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: The decision was made in 2011 to introduce blastomere biopsy into our PGS using aCGH program. This resulted in a move away from PB biopsy, based on the results presented in this comparison. Method: Retrospective data from all cycles in the PGS program were analysed. Cycles performed using PB and blastomere biopsy were compared. The blastomere biopsy group was split into two age ranges and the same data compared. Results: The average age of the patients in the PB (n 293) and blastomere (n 91) groups was 40.7 years and 39.4 years respectively. 18% (54) of patients did not achieve an embryo transfer in the PB group, compared to 29% (26) in the blastomere group. Clinical pregnancy rate (CPR) per embryo transfer (ET) and Oocyte retrieval (OR) was 19% and 14% respectively in the PB group, compared to 34% and 24% (22) in the blastomere group. Comparing age groups in the patients having blastomere biopsy: In the under 40s and 40s and over 17% (7) and 40% (20) respectively, did not achieve an embryo transfer. CPR per ET and OR was 24% and 20% (8) in the under 40s compared to 45% and 28% (13) in the 40s and over. Conclusion: Although, as we hypothesised, the percentage of patients that do not achieve an embryo transfer increases in the blastomere biopsy group, due to the additional sperm contributed aneuploidy and mitotic errors, the clinical pregnancy rate per OR is significantly increased. These trends are more pronounced in the patients 40 years and older. Discussion: The PGS using aCGH program has been improved with the introduction of blastomere biopsy, with the clinical pregnancy rates for the 40 and over age group comparable to patients not having CGH in lower age groups. © 2013 The British Fertility Society e50 Abstracts P040: Incubator power failure: how long do we really have to save the embryos? SHREENA TAILOR, MARIA VOURLIOTIS, STYLIANI ANDRONIKOU, JULIAN NORMAN-TAYLOR, GEMMA FRANCIS & PAULA ALMEIDA Chelsea and Westminster Assisted Conception Unit, Chelsea and Westminster Hospital, London, UK Introduction: Temperature and pH are fundamental factors which affect oocyte viability and subsequent embryo development. Incubators are critical to providing optimal culture conditions in vitro. Unforeseen circumstances such as power failure may be detrimental to the gametes/embryos if culture conditions are compromised. We therefore investigated the time taken for three different sized incubators to reach sub-optimal temperature and CO2 levels following power failure. Materials and Methods: Three incubators (a mixed-gas bench-top incubator, 150 L and 240 L CO2 incubators) were monitored for temperature and CO2 concentration after being switched off to mimic a power cut incident. Readings were taken every minute using an external monitoring system until atmospheric conditions were reached (approximately 25°C and 0.03% CO2). Main outcome measures were rate of heat and CO2 loss in the first three hours, time taken for temperature and CO2 to reach in-house limits ( 36.5°C and 5.5% CO2), and critical limits ( 33.0°C and 5.0% CO2). Results: The rate of heat loss in the first hour following the power cut for the 240 L, 150 L and bench-top incubator was 1.8°C/hr, 2°C/hr and 5.5°C/hr respectively; second hour 2.4°C/hr, 2.6°C/hr and 2.1°C/hr respectively; third hour 1.8°C/hr, 1.7°C/hr and 0.8°C/hr respectively. The time taken for the temperature to reach 36.5°C was 47 minutes (240 L), 44 minutes (150 L) and 8 minutes (bench-top) and to reach 33.0°C was 132 minutes (240 L), 123 minutes (150 L) and 42 minutes (bench-top). The rate of CO2 loss in the first hour following the power cut for the 240 L and 150L incubator was 0.14%/hr and 1.02%/ hr respectively; second hour 0.10%/hr and 0.69%/hr respectively; third hour 0.04%/hr and 0.51%/hr respectively. The time taken for the CO2 levels to reach 5.5% was 269 minutes (240 L) and 60 minutes (150 L) and to reach 5.0% was 598 minutes (240 L) and 86 minutes (150 L). Conclusion: The data demonstrate that in the event of power failure: i) incubators lose heat at a greater rate than CO2, ii) larger volume incubators retain heat and CO2 for longer. This has clinical implications with respect to determining which incubator to use for maximum safety and, in responding to out-of-hours equipment failure before gametes/embryos become compromised. P041: The impact of osteopontin on embryo implantation PEI-YU LIAO, SUI-HUI KAO, Y.C. CHEN, Y.C. WU & H.Y. CHANG School of Medical Laboratory Sciences and Biotechnology, College of Medical Science and Technology Successful implantation depends upon the implantation-competent blastocyst and the receptive uterus. This process is initiated via blastocyst-endometrium interaction and delicately regulated by multiple factors. Osteopontin (OPN) plays a role as a mediator of cell-cell, cell-extracellular matrix (ECM) communication and invasion. Studies have revealed that OPN is a major constituent of the uterine-placental microenvironment with influence as a component required for adhesion and signal transduction. Several evidence show that OPN binds to integrin αvβ3. In the implantation window, the increased αvβ3 was demonstrated in the endometrium that highly correlated with embryo implantation. The aim of this study is to realize the molecular signaling of OPN in embryo implantation. Fertility was assessed by mating 8-wk-old female mice with 16-wk-old male mice then determined the number and size of litters delivered. The results revealed that OPN enhanced the implantation rate to 1.7 fold. To gain insights into the molecular mechanisms, we used an oligo-microarray to identify the candidate genes involved in this implantation process including 177 up-regulated genes (NER 2) and 51 down-regulated genes (NER 0.5). The content of the regulator of G-protein signaling protein 2 (RGS2) mRNA was 44 folded increase by real-time quantitative PCR analysis. We established the in vitro matrigel assay to analyze the effect of OPN, αvβ3-integrin inhibitor or Ki16425 (RGS2 inhibitor) on embryo implantation in vitro and the developmental competency. The use of αvβ3-integrin inhibitor or Ki16425 attenuated implantation rates. Furthermore, the Jar cells were used as human trophoblasts to identify the molecular mechanism of OPN induced embryo implantation. OPN enhanced trophoblastic cells migration and the use of αvβ3-integrin inhibitor or Ki16524 reduced Jar migration. All the treated embryos stained with FITC-labeled phalloidin to observe the distribution of actin filament. These results indicate that through RGS2 signaling pathway, OPN-αvβ3 integrin may promote blastocyst implantation. Human Fertility Abstracts e51 P042: Split day (day 3 & day 5) embryo transfer: a case report JOANNA HAMMOND Homerton Fertility Centre, Homerton University Hospital, London, UK Embryo transfers usually take place on day-2, day-3 or day-5. The use of a ‘double’ day embryo transfer (one embryo on day-3 and & one day-5) may be beneficial in certain cases. A 31 year old female first presented to the Homerton Fertility Centre in June 2010 with primary infertility. A diagnosis of PCOS was established. The first treatment cycle resulted in 21 oocytes, 11 fertilised (IVF), 2 transferred on day-5 (2x1CC), Grade 1 Top quality; Grade 4 Poorest quality. No pregnancy occurred. The second cycle resulted in 2 oocytes (hCG taken at incorrect time), both fertilised and transferred on day 2 (6c1 & 4c2); no pregnancy occurred. The couple’s third cycle resulted in 36 oocytes, 18 fertilised (IVF). It was decided with the patient to transfer 1 embryo on day-3 & 1 on day-5. An 8c1 was transferred on day-3 and a 4AB on day 5. A viable single intrauterine pregnancy occurred. There seems to be an advantage for patients that either do not fit the blastocyst criteria and/or there is no clear selection of embryos on day-3. There is no way of knowing if a standard embryo transfer on either day-3 or day-5 would have resulted in pregnancy. P043: Is routine embryo culture to day 6 beneficial? KATHERINE NASH, VICTORIA GITTINS, AMY HATTON, SHARON BINNERSLEY, GEORGE HUGHES & JASON KASRAIE The Shropshire and Mid-Wales Fertility Centre, Royal Shrewsbury Hospital, Mytton Oak Road, Shrewsbury, Shropshire, UK Introduction: Following the HFEA’s ‘Multiple Birth, Single Embryo Transfer Policy’ in 2008, blastocyst culture has become routine practice in many clinics. In our clinic, patients unable to transfer on day 5 (D5) due to failed blastocyst development or poor quality, are cultured to day 6 (D6). Supernumerary embryos not suitable for freezing on D5 are cultured to D6 and frozen if viable. We compared biochemical and clinical pregnancy rates for D5 and D6 blastocyst transfers to determine whether routine culture to D6 is beneficial. Method: Biochemical (BPR) and Clinical (CPR) pregnancy rates were compared for D5 and D6 transfers between 01/01/09 and 31/05/12. Results were analysed using Fisher’s Exact test . We distinguished D6 blastocysts that were ‘true’ D6 from those that might have been later developing D5 blastocysts. Results: There was no significant difference in BPR (51.7%) and CPR (41.4%) for D5 (n 203) and D6 (43.5% and 30.4%, n 23) (BPR p 0.51, CPR p 0.37). One patient definitely had a ‘true’ D6 blastocyst. Conclusion: Culture to D6 appears beneficial as D5 and D6 pregnancy rates are similar. However, small numbers mean the D6 group results may be unreliable. One patient out of 23 had a definate D6 blastocyst making it possible that the other 22 developed late on D5. To truly distinguish D5 and 6 blastocysts we could perform transfers later on D5, but this may be impractical, particularly with blastocysts developing after 5 pm. Alternatively time-lapse technology would allow precise timing of blastulation. With these results in mind, it is likely that our policy of culturing to and freezing blastocysts on D6 regardless of the day of transfer is beneficial and will improve cumulative pregnancy rates. The number of fresh cycles a patient requires will also be reduced, ultimately benefiting the patient through reduced risk/cost, and the clinic/NHS healthcare economy. P044: Should embryos be cultured on to day 6 following embryo transfer if there are no embryos suitable for cryopreservation on the day of transfer? GEORGE HUGHES, SHARON BINNERSLEY, SARAH WALLBUTTON, VICTORIA GITTINS, STACY PARRY, AMY HATTON, ALISON LAVENDER & JASON KASRAIE The Shropshire and Mid-Wales Fertility Centre, Royal Shrewsbury Hospital, Mytton Oak Road, Shrewsbury, Shropshire, UK Introduction: Risks and costs associated with stimulation/egg collection mean that storage of excess viable embryos and maximisation of cumulative pregnancy rates from a single egg collection are a priority for clinics. Should we culture all embryos not suitable for cryopreservation on day 3 (D3) and day 5 (D5) onwards to allow us to assess their viability for cryopreservation over an extended period? Materials & Methods: Retrospective analysis of the development of © 2013 The British Fertility Society e52 Abstracts 457 embryos from 89 patients that were allocated for training from D3 (n 71) and D5 (n 18) transfer patients that did not meet cryopreservation criteria on D3 (6C 15% fragmentation, 70 hours post insemination/injection) or D5 ( 3BB (Gardner & Schoolcraft) 118 hours post insemination). The embryos allocated were cultured at 6% CO2 to D6 and graded each day. Results: Blastulation rates for D5 transfer patients were significantly greater than D3 transfer patients (43.04% vs 26.42%, p 0.0005). 1.88% of embryos from D3 patients with 0 frozen developed to 3BB on D5 vs 8.57% of embryos from D3 patients with 1 frozen (p 0.0142). 6.29% of embryos from D3 patients with 0 frozen developed 3BB on D6 vs 11.43% of embryos from D3 patients with 1 frozen (p 0.1498). 11.39% of embryos from D5 transfer patients developed to 3BB on D6. Conclusions: This small retrospective study, in suboptimal culture conditions, appears to show it may be beneficial to routinely culture embryos not meeting our cryopreservation criteria on D3 or D5 to D6. At present our biochemical success rates (53% vs 41%, p 0.3671) and clinical success rates for D5 vs D6 transfers (43% vs 32%, p 0.658) suggest that D6 blastocysts are as viable as D5 blastocysts. Practical and financial implications must be taken into account but this practice may reduce ‘fresh’ egg collections and maximise cumulative success, thereby reducing risk and cost to the healthcare economy. P045: A comparison analysis of clinical pregnancy rates following single embryo transfer of slow, normal and fast developing embryos on day 3 at time of embryo transfer REBECCA ROUGHTON, ELLEN CATER, KATHRYN BERRISFORD, LUCY JENNER & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK A comparison analysis of clinical pregnancy rates following single embryo transfer of slow, normal and fast developing embryos on day 3 at time of embryo transfer. Objective: A retrospective analysis of clinical pregnancy rates for all patients who underwent a single embryo transfer on day 3 at our clinic between January 2008 and April 2012. Data: The embryos transferred were categorised into 3 groups; slow (2–5 cells) normal (6–8 cells) and fast ( 9 cells) developing embryos on day 3 at the time of embryo transfer (ET), which was between 68–75 hours post insemination. Only single embryo transfers were included to provide accurate data on the implantation potential of the embryos. Clinical pregnancy data was analysed using Fisher’s exact test. Results: 608 single embryo transfers were analysed. Embryos ranged from 2–14 cells at the time of ET on day 3. 62 patients had slow developing embryos transferred and 6 patients achieved a clinical pregnancy (9.7% Clinical pregnancy rate (CPR). 489 patients had normal developing embryos transferred, and 153 achieved a clinical pregnancy (31.3% CPR). 57 patients had fast developing embryos transferred, and 16 achieved a clinical pregnancy (28.1% CPR). There is a significant difference between the CPR of the slow and normal embryos (P 0.0002). There is no significant difference between the CPR of the normal and fast embryos (P 0.6535). Conclusion: This study has shown there is no significant difference between the CPR of normal and fast embryos and therefore these ‘fast’ embryos should be considered for selection at embryo transfer. However slow developing embryos give significantly poorer clinical pregnancy rates compared with ‘normal’ embryos and therefore should not be considered for selection at embryo transfer and should only be transferred if there are no other embryos available. P046: Day 4 versus day 5 embryo transfer in an egg donation program JAIME GUERRERO, JORGE TEN, JOAQUÍN LLÁCER & RAFAEL BERNABEU Instituto Bernabeu, Alicante, Spain Introduction: Traditionally, the vast majority of embryo transfers are performed either at the cleavage stage or blastocyst stage, while transfer on day 4 remains an option that is practically overlooked. Few reports exist evaluating the effectiveness of day 4 embryo transfers. The main goal of this study was to analyze whether day 4 embryo transfer is as effective as day 5 in embryo selection capability in order to achieve pregnancy. Materials and Methods: During a six month period 228 fresh embryo transfers coming from our oocyte donation program were analysed, 67 of which were performed on day 4 and 161 on day 5. The procedure for recipients involved the use of oral estrogen (Progynova) in a step up protocol and vaginal micronized progesterone (Cyclogest). In cases of preserved ovarian activity, a LH-RH agonist depot was used in the luteal phase of the previous cycle. The main outcome measures were Human Fertility Abstracts e53 positive β-HCG, implantation, clinical pregnancy and miscarriage rate. Results were analyzed using t-student test and chi-square test. A P value of .05 was considered statistically significant. Results: There were no differences in terms of maternal and donor age (41.1 4.4 and 24.9 3.9 versus 41.9 4.4 and 24.1 3.8), endometrial thickness (8.6 1.8 versus 8.6 1.5), follicular phase length (19.0 3.6 versus 19.5 3.5), number of donated oocytes (12.4 3.8 versus 12.7 3.4) and embryos transferred (1.8 0.4 vs. 1.9 0.4) in day 5 and day 4 groups respectively. Positive pregnancy test (77.6% vs. 65.7%) , clinical pregnancy (57.8% vs. 55.2%), implantation rates (43.4% vs. 38.6%) and miscarriage rate (10.8% vs. 13.5%) did not achieve statistical significance. Conclusions: The clinical outcomes of transferring embryos on day 4 or day 5 were comparable, allowing major flexibility to schedule embryo transfer and, therefore, avoided inconveniences both for the patients and the clinic. Other P047: Main causes of rejection during egg donor selection process RAFAEL BERNABEU, JAIME GUERRERO, JORGE TEN, JUAN GIMÉNEZ & JOAQUÍN LLÁCER Instituto Bernabeu, Alicante, Spain Introduction: A careful evaluation of egg donors during the selection process is a determinant for the final outcome of treatment. Here we evaluate the main reasons for non-acceptance of candidates in our donation program. Materials and Methods: Study conducted from January 2011 through July 2012 including 560 potential egg donors. The selection protocol developed at the Instituto Bernabeu comprises of: – Personal interview with a clinical psychologist and application of our EMAE Psychological Assessment Questionnaire. – Evaluation of personal and family medical history, phenotype, clinical and gynecological examination, including vaginal smear and ultrasound scan performed by the gynecologist for follicle count and to rule out the presence of gynecological pathology. – Genetic studies: Karyotype (including chromosomal polymorphisms), Cystic Fibrosis, Fragile X syndrome and alpha-thalassemia. The DNA obtained is stored in a Biobank for 20 years. – Blood type and Rh factor, syphilis, Hepatitis B and C, HIV serology and coagulation tests. Results: Only 300 out of 560 candidates (53.6%) completed the selection process. 146 candidates (26.1%) were rejected after their personal and psychological evaluation due to inappropriate BMI (54), psychological assessment (32), age and phenotype (22), mental disorder (9) or medical reasons (19) in the donor or relatives, pharmacological treatment (7), lack of family history (2) or previous miscarriages (1). Of the remaining 414 candidates, 46 (11.1%) were not suitable after medical examination. 368 patients continued with the screening, resulting in 68 (18.5%) candidates excluded for their karyotype (36), cystic fibrosis mutation carriers (18), fragile X syndrome (3), alphathalassemia (8), and serology (3). Conclusions: Applying our protocol, only 53.6% of candidates were finally accepted into our program. Interestingly, 18.5% were rejected due to chromosomal or genetic causes. A donation program must have a strict selection process, including clinical, genetic and psychological evaluation to assure the best outcome with maximum clinical safety for recipients and clinicians. P048: Known versus Anonymous Oocyte Donation JOLLY JOY & GILLIAN WILLIAMSON Regional Fertility Centre (RFC), Royal Victoria Hospital, Belfast, Northern Ireland Introduction: Oocyte donation (OD) was first reported in 1983. An OD programme was established in Belfast in 1987. Aim: To compare known donor cycles (KDC) with anonymous donor cycles (ADC). Methods: Retrospective analysis of medical files from January 2006 to August 2012. Results: Of 119 OD cycles, 92(77.3%) were known donor cycles (KDC) and 27(22.7%) were anonymous donor cycles (ADC). There was no significant difference in KDC and ADC in the mean ages (years) of donors (32.8, 32.1, p 0.49) and recipients (37.7, 39.9, p 0.14). 29(24.4%) donors were 36 years of age [ADC 4(14.8%) v KDC 25(27.2%), p 0.22]. All cycles were long © 2013 The British Fertility Society e54 Abstracts agonist. Intracytoplasmic sperm injection rate, mean number of oocytes retrieved, cycles that did not have embryo transfer (ET) and ovarian hyperstimulation syndrome rates were not statistically different. There was no significant difference in Clinical Pregnancy Rate (CPR) per cycle started in ADC v KDC (38.5% v 28.5%, p 0.22) or in CPR per ET in ADC v KDC (41.7% v 28.2%, p 0.22). By contrast, the LBR was significantly higher in ADC (41.7% v 14.1%, p 0.007). There was a 50% miscarriage rate (MR) in KDC with 0 in ADC (p 0.001). The mean donor age for cycles that ended in a miscarriage and live birth was not significantly different (31.25 v 31.5, p 0.86). Conclusion: With the changes in donor anonymity laws in the UK there has been a trend towards decreased ADC. The LBR reported here is significantly higher in ADC compared to KDC. With no difference in treatment protocols and donor age of the pregnant recipients, the significantly higher MR and lower LBR in KDC merits further investigation. P049: Improving the patients experience of pain during egg collection CAROLYN CHESTER, EMILY WEST, ANNE MOWFORTH & RACHEL CUTTING Centre for Reproductive Medicine and Fertility (Jessop Fertility), Assisted Conception Unit, Jessop Wing, Level 1, Tree Root Walk, Sheffield S10 2SF, UK Introduction: NICE guidance (2004) recommends that women undergoing transvaginal retrieval of oocytes should be offered conscious sedation. However, patients frequently express anxiety regarding the degree of pain they are likely to experience. Therefore is it essential to manage the procedure effectively to reduce patient discomfort and anxiety. A nurse led quality improvement initiative commenced to assess and review current practice with the aim to introduce more effective pain management. This involved completing an audit, effecting change and re-audit. Methods: In 2009, 51 patients undergoing egg collection with a double lumen needle and Entonox and Fentanyl as their main pain relief were asked to participate. A further audit commenced in 2012 after changes were introduced. The audit questionnaire incorporated the use of an observational pain score which utilises a single 10cm continuum; the left end point signifies ‘no pain’ and the right endpoint signifies ‘worst possible pain’. Independently the clinician/nurse and the patient place an arrow on the line indicating their pain assessment. Results: Results from the initial audit showed that over 50% of patients experienced moderate to severe pain and the severity of the pain experienced correlated to the length of the procedure. The current audit is due for completion in November 2012 but early analysis show a reduction in the level of pain experienced. Conclusion: After discussing the 2009 audit at a team meeting modifications to the pain management protocol were agreed. Changes included the administration of IV Paracetamol prior to the procedure and the introduction of a tapered single lumen needle where appropriate. IV Paracetomol has been shown to reduce pain during and post procedure and tapered needles reduce pain, bleeding and procedure time. The current audit will be assessed after completion in November to assess how effective the changes have been. P050: Walking the path with Orthodox Jewish couples to achieve a family within Halachic law KEITH JORDAN1, SIMON FISHEL2, ALISON CAMPBELL1, NATALIE BOWMAN1, SAMANTHA DUFFY1, CAROLINE DREW1, KATHRYN GARDNER1, KAREN HARRISON1, LISA LEE1 & ELAINE POWER1 1 Care Fertility Manchester, Victoria Park, Manchester, UK and 2Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK “Be fruitful and multiply, fill the earth and subdue it”-Genesis 1:28 has been held to be so important to Judaism that the majority of Rabbi’s agree that it justifies the use of modern assisted reproduction technology for procreation within orthodox Jewish populations. However, critical issues still arise in order to ensure correct “Halachic” procedures are followed. The provenance of the gametes and embryos should be closely monitored by a Rabbi or suitable rabbinically trained observer, who would be present for all key procedures. It is also a requirement that there is no possibility of the gametes or embryos coming into close proximity to those of another patient, so must be cultured in a completely separate incubator. Having been approached by a number of orthodox couples for treatment, it was agreed that either a Rabbi, or trained members of a Jewish infertility charity named “Kivisi”, would have controlled access to the treatment areas and laboratories in order to witness and oversee the handling of gametes and embryos of orthodox couples. Monitors were required to sign privacy agreements and be aware of the HFEA Human Fertility Abstracts e55 restrictions regarding protection of data and privacy of all patients. Risk assessments regarding the presence of nonlaboratory staff were completed and training given regarding the restrictions and responsibilites of being present in a functioning ART laboratory. An incubator was purchased to be used solely by the couple for the duration of their cycle, being secured for when the were not present by using serially numbered anti-tamper seals, serial numbers being recorded by monitors and checked prior to opening for the next procedure. Monitors also witnessed patient labels and identification for each procedure in addition to the usual electronic and manual witnessing. P051: Pregnancy rate, abortion rate and contraceptive usage among street sex workers in Colombo, Sri Lanka ASANKA PATHIRATNE Base Hospital Panadura, Sri Lanka Objective: The objective of this study was to describe levels of pregnancy, abortion rate and contraceptive usage among a street-based female sex workers (FSWs) in Colombo. Method and Materials: The study sample was obtained from a community-based prospective study (2007–2009) of 96 women in street-based female sex workers. Individual self administered questionnaire was used. The FSWs were selected randomly. Information on contraceptive methods, number of abortions, and number of pregnancies was collected. Results: Mean age of these females was 29 years. The mean age of first sexual experience was 22.20 years. 69.2% of females were educated upto O/Ls. Others were educated up to year 5. Almost all (93.1%) complained of smelly vaginal discharge. Of these, 73.2% of whom had reported at least one prior pregnancy. Interestingly 61.2% of women had reported two pregnancies and of these 54% had undergone induced abortion during this study period. 81.2% did not use any contraceptive method. In the remainder ,oral contraceptives (7.5%), Depo provera injection (3.4%) use of condoms (1.9%), and intrauterine device insertion (1.2%), were the most common methods of contraception. Conclusions: These findings demonstrate high levels of unwanted pregnancy in this population of women leading to induced abortions due to low utilization of effective contraceptives and suggest a need to improve the accessibility and utilization of family planning methods, which are appropriately targeted and tailored for FSWs in Colombo. P052: Live birth rates after ART in Serodiscordant couples positive for Hepatitis B or C infection: A 10-year review VINETA CIPRIKE, CONOR HARRITY, G. EMERSON & E. MOCANU Royal College of Surgeons in Ireland, Dublin, Ireland Introduction: There is conflicting data that HCV and HBV may have a negative influence on gamete quality, however, there is no consensus on their impact on live birth rates after ART. This study was designed to compare outcomes of ART with IVF or ICSI in HCV or HBV positive serodiscordant couples with seronegative couples. Materials and Methods: A retrospective analysis of all fresh IVF and ICSI cycles undertaken at an academic tertiary referral ART centre in Dublin over a 10-year period (Jan 2001–Dec 2010) was performed. The study group included all HCV and HBV serodiscordant couples undergoing IVF or ICSI cycles. The control group consisted of couples negative for viral infections that had treatment over this period, and both groups were matched for female age, day 3 FSH, day and number of embryo transfer. Overall clinical pregnancy rates (CPR) and live birth rates (LBR) were compared between groups groups. Results: Of 8800 cycles undertaken during the 10-year period, 110 (1.25%) were performed on 59 couples that were discordant seropositive for HBV or HCV (61 IVF and 49 ICSI). The control group included 1852 IVF and 1021 ICSI cycles. Differences in CPRs were approaching statistical significance between the IVF study and control groups (24.5% vs. 36.8%, p 0.05) with a significant difference in LBR’s (18.0% vs. 34.3%, p 0.01). For ICSI treatment, the CPRs (25.0% vs. 35.9%, p 0.17) and LBRs (20.8% vs. 35.3%, p 0.06) were not significantly different between study and control groups respectively. Conclusions: The study demonstrated a trend towards lower clinical pregnancy and live birth rates in hepatitis serodiscordant couples undergoing ART compared to seronegative patients, but for ICSI treatments the differences were not statistically significant. These findings may aid practitioners in the counselling of serodiscordant couples prior to commencing ART treatment, and assist with the choice between IVF or ICSI to achieve fertilisation. © 2013 The British Fertility Society e56 Abstracts P053: Can chlamydia serology predict whether transcervical tubal catheterization at selective salpingography will be successful? DAVID CAHILL & MUNAWAR HUSSAIN School of Clinical Sciences, St Michael’s Hospital, Bristol, UK Purpose: Previously we reported the effectiveness of transcervical tubal catheterization at selective salpingography as a non invasive and relatively easy technique to treat and reverse proximal tubal blockage. In this study, we have analysed the data to examine whether a successful outcome can be predicted using results from Chlamydia serology estimation. Methods: From records collected over 11 years, follow up data were available for 97 women (and procedures). Data were analysed by Chlamydia serology as to whether the technique was successful (achieving unilateral or bilateral fill), whether pregnancy was likely to occur subsequently as a result and whether it did (or not). We used the cut-off of a Chlamydia antibody titre of more than or equal to 256 as being abnormal (as previously published). Results: We found that when Chlamydia antibody titres are considered, women with higher antibody titres ( or 1:256) did not show any significantly greater chance of success at the technique (31% vs. 42%, NS). However, they did have a lower opportunity to achieve a pregnancy (41% vs. 70%, p 0.019) though not of achieving a live birth (68% vs. 60%, NS). In the presence of excessively high Chlamydia titres (1:1024 or greater), pregnancy rates were not significantly reduced (15% vs. 34%). Conclusions: Women who have elevated Chlamydia antibody titres are less likely to be successful at selective salpingography and transcervical tubal catheterization, and should be counselled accordingly. P054: The implementation and evaluation of a nurse led Hysterosalpingogram service DAWN LITTLEHALES, NIKKI COTGREAVE-KEATES & JAMES HOPKISSON Fertility Unit, Nottingham University Hospital, Queens Campus, Nottingham, UK Introduction: In June 2009 the contrast media used during the HyCoSy procedure was withdrawn from production. With no suitable alternative media to replace Ecovist and no staff trained to perform HSG, the only option locally was for patients to undertake a Laparoscopy and Dye Test. This led to increased surgical waiting times and a less than satisfactory patient experience. Patient dissatisfaction was the driver for the search for a nurseled solution using the HSG (hysterosalpingogram) procedure, which had not been used in the trust for many years. The following describes a comparison of relative success between this service and the previous HyCoSy service with the aim of improving current practice and the patient journey. Methods: The outcome of both HyCoSy and and HSG clinics were reviewed over separate 2 year periods. Main measures included complications and the subsequent need for laparoscopy and dye testing. Patient questionnaires were provided to patients who have undertaken HSG in order to evaluate current patient satisfaction of the overall service, ranging from booking, information explanation, comfort during procedure and the professionalism of the staff. Results: Over a 2 year period 248 HyCoSy’s were performed with 50 patients requiring referral for laparoscopy and dye which equates to 20%. Over a separate 2 year period 392 HSG’s were performed with 17 patients requiring referral for laparoscopy and dye which equates to 4%. The failure rate for HSG is significantly lower when compared to the failure rate of HyCoSy (p 0.01). In general, patient satisfaction of the nurse led HSG service has been very high. Conclusion: The introduction of the nurse led HSG service has been a positive move for fertility service with increased efficiency and improved patient satisfaction P055: Hysterosalpingography audit VLADIMIR REVICKY, ARIANA SPUNGINA & HAMED AL-TAHER The Queen Elizabeth Hospital, Kings Lynn, Norfolk, UK Objectives: To measure our practice against the standards of NICE guidelines; specifically, in offering Chlamydia screening prior uterine instrumentation and the use of Hysterosalpingography (HSG) in favour of Laparoscopy for women who are not known to have co-morbidities such as pelvic inflammatory disease, previous ectopic pregnancy or endometriosis. Methods: This was a retrospective audit of 58 consecutive HSG cases identified from a Human Fertility Abstracts e57 radiological database. Results: Measured standards were achieved in all cases. Median of body mass index of patients was 26.4 with inter-quartile range (IQR) 23.3–32, median for age was 30.5 with IQR 26–33, primary infertility constituted for 52% of all cases of infertility, median for length of infertility was 2 years with IQR 1–2 and the most common cause of infertility was polycystic ovarian syndrome (31%). 84.5% (49/58) of all HCG examinations identified patent fallopian tubes. 19% (11/58) of all patients underwent Laparoscopy and Dye test.The most common identified pathology was endometriosis (46%). Conclusion: Our audit identified that our practice of offering Chlamydia screening and the use of HSG meets national standards. P056: A rare cause of unilateral neck swelling following ovarian hyperstimulation syndrome IRYNA KRYNYTSKA, JONATHAN LORD & SUSAN BATES The Cornwall Centre for Reproductive Medicine,Wheal Unity Clinic, Princess Alexandra Wing, Royal Cornwall Hospital, Truro, Cornwall, UK Ovarian hyperstimulation syndrome (OHSS) is a systematic disorder occurring as a result of excessive ovarian stimulation during assisted conceptions treatment. Thrombosis in OHSS may be the cause of serious morbidity and more rarely mortality. It is thought to develop due to hypercoagulable state of OHSS due to high serum level of oestrogen and haemoconcentration. Two cases of upper extremities deep vein venous thrombosis following OHSS. Both patients underwent ovarian stimulation with appropriate FSH dose and subsequent in-vitro fertilization procedure. In both cases women started displaying symptoms of moderate OHSS 11 days following embryo transfer. One of them required a short admission for observation and supportive treatment which included thromboprophylaxis. Otherwise they were managed in the out-patient settings. Both of them developed significant neck swelling four (first woman) and seven (second woman) weeks after having the embryo transfer procedure. First woman was diagnosed with superior vena cava thrombosis and the second one with subclavian and axillary venous thrombosis. They were treated conservatively with low molecular weight heparin and made complete recovery. Both women had successful pregnancies which resulted in livebirth (twins for the first patient). In future, they would be advised to commence prophylactic anticoagulation if any further ovarian stimulation required. Current national guidance limits thromboprophylaxis only to those cases that require admission to hospital. Severe OHSS is only accounted for 0.56–0.65% of all cases and it is estimated that 1 in 128 women with severe OHSS would develop thrombosis. These cases demonstrate possibility of serious complications during treatment involving ovarian stimulation. Awareness and early diagnosis are crucial for the management of those patients. Thromboprophylaxis should be considered for women with OHSS even if they do not require admission. The length of the treatment may need to be extended taking into the account late onset of complications. Hormones P057: Outcome of assisted reproduction treatment in women with extremely low antimullerian hormone (AMH) levels MUNAWAR HUSSAIN, UMA GORDON & VALENTINE AKANDE Bristol Centre for Reproductive Medicine, North Bristol NHS Trust, Southmead Hospital, Westbury on Trym, Bristol, UK Purpose: AMH is commonly being used as a specific ovarian reserve marker however; availability of different assays, pregnancies even at undetectable levels and intra-cycle variations has been reported for this test. The purpose of this study was to determine whether women with extremely low serum AMH levels ( 5 pmol/l) can achieve pregnancy and live birth with assisted reproduction treatment and whether this is age dependent. Methods: Retrospective analysis of 63 patients who underwent first cycle of IVF/ICSI from Sept 2010 to May 2012. Ovarian reserve was tested by menstrual cycle day 1 to 4 FSH and second generation AMH assays. Patients were divided in two groups according to their age (group 1 38 and group 2 38 years of age). Results: Results are outlined in Table 1. © 2013 The British Fertility Society e58 Abstracts Table 1. Demographic characteristics and pregnancy outcome. Total (n 63) AMH (pmol/L) FSH (mIU/ml)∗ Gonadotrophin dose (IU) Oocytes retrieved∗ Cycle cancellation∗∗ Clinical pregnancy∗∗ Live birth/ongoing pregnancy∗∗ Age 38 years (n 38) Age 38 years (n 25) P 2.1 (0.6–3.7) 9.3 (7–12) 4200 (3900–4500) 4 (3–6) 3 (4.8) 10 (15.9) 9 (14.3) 2.5 (0.7–3.7) 9.3 (7.7–11.5) 4200 (3000–4500) 5 (4–7) 1 (2.6) 7 (18.4) 7 (18.4) 1.5 (0.6–2.9) 9.3 (7–12) 4200 (3900–4800) 4 (3–5) 2 (8) 3 (12) 2 (8) 0.2188 0.7455 0.4669 0.0484 0.5574 0.7268 0.2977 ∗Median and interquartile range. ∗∗Number (%) Conclusions: Despite very low-serum AMH levels, our data shows a reasonable chance of pregnancy and live birth rates. A study with larger numbers is required to confirm whether the tendency towards lower pregnancy and live birth rates with increasing age is of any significance. P058: Discrepancies between anti-mullerian hormone (AMH) and follicle stimulating hormone (FSH) in assisted reproduction MUNAWAR HUSSAIN, UMA GORDON & VALENTINE AKANDE Bristol Centre for Reproductive Medicine, North Bristol NHS Trust, Southmead Hospital, Westbury on Trym, Bristol, UK Purpose: AMH and FSH are two commonly used ovarian reserve tests. Despite statistical congruity between these two hormones; many individual patients have discordant values. The purpose of this study was to determine the frequency of discordance between AMH and FSH tests and the clinical significance in terms of ovarian response, oocyte yield and cycle outcome in patients undergoing assisted reproduction. Methods: Retrospective analysis of 107 patients undergoing first IVF/ICSI cycle from Sept 2010 to May 2012. Data were analyzed in four groups; group 1 normal AMH/normal FSH, (NAMH/NFSH), group 2 normal AMH/high FSH (NAMH/HFSH), group 3 low AMH/normal FSH (LAMH/NFSH) and group 4 low AMH/high FSH (LAMH/HFSH). Results: Table 1 summarizes the cycle details. 57% patients showed concordant while 43% patients had discordant values of AMH and FSH. Conclusion: A significant proportion of patients had discordant AMH and FSH values. Women with normal AMH and FSH values showed the best oocyte yield while women with abnormal AMH needed a higher dose of gonadotrophins. There were no differences in clinical pregnancy and live birth/ongoing pregnancy rates. Table 1. Demographic characteristics and cycle outcome. NAMH/NFSH n 37 ∗AMH (pmol/L) ∗FSH (IU/L) ∗FSH dose (IU) ∗Oocytes retrieved ∗∗Cycles Cancellation Clinical pregnancy rate Live birth/ongoing pregnancy rate NAMH/HFSH n7 LAMH/NFSH n 39 LAMH/HFSH n 24 P value 13.1 (7.38–27.4) 7.1 (6–8.2) 3600 (2250–4200) 7 (5–10) 1 (2%) 9 (24) 9 (24) 8.8 (6.8–13.1) 12.54 (10.7–18) 3300 (2250–4299) 3 (2–7) 0 2 (28) 2 (28) 2.2 (0.7–3.9) 8 (6.4–10) 4200 (3000–4500) 4 (3–6) 2 (5%) 6 (15) 5 (12) 1.4 (0.4–3.1) 12 (11.2–32.9) 4500 (4200–4800) 4 (2–6) 1 (4%) 4 (16) 4 (16) 0.0001 0.0001 0.0008 0.0023 0.90 0.70 0.54 ∗Median (inter-quartile range) Kruskil-Wallis test, ∗∗Numbers (%) Fisher’s exact test. Human Fertility Abstracts e59 P059: Using AMH to individualise starting dose of gonadotrophin IRYNA KRYNYTSKA & SUSAN BATES The Cornwall Centre for Reproductive Medicine,Wheal Unity Clinic, Princess Alexandra Wing, Royal Cornwall Hospital, Truro, Cornwall, UK Serum anti-Mülerian hormone (AMH) is currently considered the best marker of ovarian reserve and of ovarian responsiveness to gonadotrophins in controlled ovarian stimulation for assisted conception. It allows clinician to categorise patients into those in whom poor response to the drugs may be anticipated or put at risk due to an excessive response. We performed retrospective case-based audit of the women undergoing controlled ovarian stimulation (COS). The objective was to assess whether the starting gonadotrophin dose was adjusted to the AMH level. Although it is clear that individualising treatment strategies according to circulating AMH may reduce clinical risks, no standardised protocol has been developed yet. To date only one prospective cohort study has been published looking at individualising FSH dosage in IVF cycles. Therefore, the treatment dosages for our criteria were mainly based on previous experience. The criteria were defined as follows: 1) women with low or very low level of AMH should have starting dose of gonadotrophins 300 using short protocol; 2) women with high AMH should have starting dose of gonadotrophins 150 using long protocol. We limited our audit to the women who were undergoing their first COS (N 51). There were 21 women in the short protocol group and 30 in the long one. Choice of protocol was mainly defined by the patient’s age with mean age 37 and 30 in short and long protocol respectively. The results showed that 93% of women in the short protocol arm and 78% in the long protocol had FSH dose 300. Total 37% women with low AMH level underwent COS using long protocol. There was only one patient with high AMH level who had COS using long protocol with starting FSH dose of 150. This complied with our audit criteria. This audit has identified some inconsistencies in the care we provided to the patients undergoing controlled ovarian stimulation and triggered development of the local protocol to standardise the starting dose of gonadotrophins in controlled ovarian stimulation. P060: AMH Gen II assay - can we believe the measurements? OYBEK RUSTAMOV, ALEXANDER SMITH, STEPHEN ROBERTS, ALLEN YATES, CHERYL FITZGERALD, MONICA KRISHNAN, LUCIANO NARDO & PHILIP PEMBERTON Department of Reproductive Medicine, St Mary’s Hospital, Central Manchester University Hospitals NHS Foundation Trust, Manchester, UK Introduction: In view of discrepancies in AMH results in our clinical samples we decided to investigate the performance of the Gen II AMH assay using following dataset-based and laboratory studies. Assay method comparison: Contrary to data from the manufacturer and subsequent validation study, our age-adjusted regression model for comparison of AMH concentrations between 3934 DSL (Active MIS/AMH ELISA; Diagnostic Systems Laboratories, Texas, USA) and 1934 Gen II (AMH Gen II ELISA, Beckman Coulter, CA, USA) samples showed that Gen II provides in average 33.5% lower results. Similarly, age adjusted comparison of assay methods in women who had initial measurement using DSL (n 330) and subsequently with Gen II (n 330) found that using Gen II results in obtaining, in average, 20% lower AMH concentration. Variability: In contrast with current belief, we found that there is significant variability between repeated samples of the same patient. Age adjusted analysis of AMH concentration in women (n 87) who had repeated measurements (n 177) provided a within-patient sample-to-sample CV of 59%. Linearity of dilution: The study found that the proportionality with two-fold dilution did not hold. There was, ion average, 57.4 12.3% increase in AMH concentration in dilution, compared to neat samples (n 9). Stability at room temperature: Storage of samples (n-47) at room temperature resulted in a progressive increase in AMH concentration; after 7-day storage there was 158.4 7.6% increase compared to the baseline. Stability during storage: AMH concentration appeared to increase in average 22.5 11.1% when samples (n 8) were stored at 20°C over a 5 day period. However storage of samples (n 8) at 80°C demonstrated an insignificant increase at 1.8 3.1%. Discussion: Our study indicates that AMH may not be stable under the storage and processing conditions recommended by the manufacturer. Use of Gen II assay samples may therefore result in erroneous measurements with possible subsequent clinical implications. © 2013 The British Fertility Society e60 Abstracts P061: Random AMH measurement is not reproducible OYBEK RUSTAMOV, ALEXANDER SMITH, STEPHEN ROBERTS, ALLEN YATES, CHERYL FITZGERALD, MONICA KRISHNAN, LUCIANO NARDO & PHILIP PEMBERTON Department of Reproductive Medicine, St Mary’s Hospital, Central Manchester University Hospitals NHS Foundation Trust, Manchester, UK Background: It is believed that serum AMH levels are highly reproducible within and across menstrual cycles. Hence single blood sampling for AMH measurement has been accepted as routine practice. However, we recently noted that repeated AMH measurements provided significantly different results in most of our patients and therefore, decided to investigate the reproducibility of random AMH measurements in women who had AMH measurements during investigation of their infertility. Methods: All women from age of 20 to 46 who had repeated AMH measurements using the same type of assay during one-year period were included. During the study period, 313 women had repeated AMH measurements (n 646 samples) using the DSL assay (Active MIS/AMH ELISA; Diagnostic Systems Laboratories, Webster). The median time between samples was 5.1 months. Eighty-seven women (n 177 samples) had repeated AMH using the Gen II assay (AMH Gen II ELISA, Beckman Coulter, Inc., CA). The median interval between samples was of 3.2 months. A mixed effects model in log scale was used to calculate the sample-to-sample (within-subject) variation of AMH levels with adjustment for age. Results: The sample-to-sample coefficient of variability (CV) in women who had repeated AMH measurements using DSL assay was 32%. In women who had repeated AMH measurements using Gen II assay, the sample-to-sample CV was 59%. Discussion: Many studies have reported that there is insignificant variation between repeated AMH measurements, suggesting that a single AMH measurement is representative of ovarian reserve. However our data suggests there is significant variability in AMH levels between random samples from women. Sampling variability is significantly higher in women who had repeated AMH using currently available Gen II assay. Conclusion: There is substantial variation in AMH levels between repeated samples. This sample-to-sample variation is significantly higher in women who had repeated AMH measurements using Gen II assay when compared to that of DSL assay. P062: Old and new AMH assays: Can we rely on current conversion factor? OYBEK RUSTAMOV, ALEXANDER SMITH, STEPHEN ROBERTS, ALLEN YATES, CHERYL FITZGERALD, MONICA KRISHNAN, LUCIANO NARDO & PHILIP PEMBERTON Department of Reproductive Medicine, St Mary’s Hospital, Central Manchester University Hospitals NHS Foundation Trust, Manchester, UK Background: According to recommendations of the manufacturer and subsequent validation study recently introduced the Beckman Coulter Gen II ELISA (Gen II) gives AMH values that are 40% higher than the Active® MIS/AMH ELISA by Diagnostic Systems Lab (DSL) assay. However, we noted that some patients had lower AMH levels when compared to their previously measured hormone levels using the DSL kit and therefore decided to investigate reliability of the conversion factor. Methods: Serum samples (n 5868) from a heterogeneous infertile female population (n 5007) assayed with either DSL (n 3934) or the Gen II (n 1934) assay were analyzed. Further subgroup analysis in a selected population was conducted by comparing AMH levels in 1783 women with no history of PCOS (DSL n 1839 samples and Gen II n 420 samples). In order to rule out population-related factors within-patient comparison of AMH levels was conducted in the group of women (n 330) who had had a first sample measured using DSL assay with later sample measured using Gen II assay. The values were compared using regression model in log(AMH) with adjustment for age. Results: After adjustment for age, the total cohorts showed Gen II gave AMH values 34% lower than those for DSL. Comparing patients with determinations using both assays the difference was 21%, whilst the non-PCOS series showed a larger difference with Gen II being 58% lower. Conclusions: The results of the laboratory validation studies for the Gen II AMH assay are not reproducible in a routine clinical setting. Consequently, observed AMH level were 21–58% lower than previously reported while the corrected reference range has increased by factor of 40%. This could lead to patients being treated assuming much lower ovarian reserve than is actually the case which can lead to increased risk of OHSS and cycle cancellations due to administration of significantly higher dose of gonadotrophins in IVF/ICSI cycles. Human Fertility Abstracts e61 P063: Low serum AMH and AFC values predict a low clinical pregnancy rate but only in women over 38 years of age LUKASZ POLANSKI, LYNSEY ZUJOVIC, MIRIAM BAUMGARTEN, JAMES HOPKISSON, KIRSTYN SEWELL, BRUCE CAMPBELL & NICK RAINE-FENNING Division of Obstetrics & Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK Aim: The aim of this study was to identify age-related anti-Müllerian hormone (AMH) and antral follicle count (AFC) cut-off values for prediction of poor IVF treatment outcome defined as clinical pregnancy rate (CPR) of 10%. Materials and Methods: This was a prospective study. AFC was performed and blood taken for serum AMH on day 1–5 of menstrual cycle immediately preceding IVF treatment between Jan. 07 and Jun. 12. Outcome was defined as viable clinical pregnancy at 6 weeks on transvaginal ultrasound. Post-test probability analysis was performed. Results: Data were normally distributed and presented as mean (/SD). AFC was available for 1028 women. Mean age was 34 (/4.3) years with mean AFC of 18.8 (/11.05). 476 (46.3%) of these patients had a viable pregnancy at 6 weeks. Patients with low AFC ( 5) had an overall CPR of 14.3%. Age stratification revealed lower CPR in women with a low AFC aged 39 years compared to younger women with the same AFC (14.6% vs. 45%; p 0.05). AMH levels were available for 585 women. Mean age was 34.6 (/4.7) years with mean AMH of 16.13 (/18.37) pmol/L. 256 (43.8%) of these women had viable pregnancy at 6 weeks. Patients with low AMH ( 3.08 pmol/l) had a CPR of 24.1%. Stratification of patients with low AMH for age, revealed a 33.8% chance of clinical pregnancy in women 39 compared to patients aged 39 who had 12.6% chance (p 0.05). Conclusions: Impaired ovarian reserve, defined as an AMH of 3.08 pmol/L or AFC 5, is predictive of lower chance of pregnancy, but only in women aged 39 who have an approximately 12% chance of pregnancy. The two tests offer equivalent predictive value and could be used interchangeably to counsel patients regarding chances of IVF success. Interpretation of these results needs to be cautious and repeated in larger multicentre studies. P064: Anti-Müllerian hormone can be considered to be a quantitative marker of oocyte yield rather than a qualitative indicator of oocyte or embryo developmental potential ANNABEL RATTOS, CHRISTINE LEARY, STEPHEN KILLICK, STEVE MAGUINESS & JOHN ROBINSON The Hull IVF Unit, The Women and Children’s Hospital, Hull Royal Infirmary, Kingston-upon-Hull, UK Pre-treatment Anti-Müllerian Hormone (AMH) levels correlate with oocyte yield, but poorly predicts pregnancy outcome. The relationship of AMH to oocyte developmental potential remains unclear. This study sought to determine the relationship between AMH and embryo development. AMH was recorded (TDL, DSL assay) for 353 IVF patients treated over a 12 month period. Patients were categorised into those with low AMH values; (lowAMH 3.08–21.97 pmoles/litre) versus satisfactory AMH values (satAMH 21.98–40.03 pmoles/litre). Based on these AMH levels, female age and previous cycle information, patients were prescribed appropriate doses of exogenous FSH in order to evoke an appropriate ovarian response prior to IVF. Embryo development was compared for the two groupings. Higher follicle and oocyte numbers were observed in the satAMH group (n 91). Oocyte maturity, fertilisation and embryo cleavage rates were comparable for the groupings. The proportion of high quality embryos was significantly higher for those with satAMH (60% verses 37% p 0.05), however, this group were found to be significantly younger. Interestingly, this did not translate into higher rates of blastocyst formation (34.9% and 32.7% for lowAMH and satAMH respectively). Female age has been widely shown to correlate with reduced oocyte competence and embryo quality. Increased blastocyst development was recorded for younger women (37.8% 35years versus 30.1% 35 years p 0.01) but, critically, this was independent of AMH (r 0.002, p 0.96). In younger women with lowAMH, 37.4% of embryos formed blastocysts versus 38.5% of embryos in patients with satAMH. Likewise there was no significant relationship in the older age group ( 35 years 30.3% lowAMH versus 29.8% satAMH). Clinical pregnancy and miscarriage rates did not correlate with AMH. Although a lower number of oocytes are recovered from women with lowAMH, the quality of these oocytes and resulting embryos does not appear to be inferior to those retrieved from women with satAMH levels. Embryos generated are of comparable quality, developmental and implantation potential. © 2013 The British Fertility Society e62 Abstracts Ovary P065: A clinician’s view on ovarian hyperstimulation syndrome (OHSS): preliminary results of the national survey MIRIAM BAUMGARTEN, LUKASZ POLANSKI & NICK RAINE-FENNING Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE], Division of Obstetrics and Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK Cabergoline has become a routinely prescribed drug for the prevention of development and treatment of OHSS. There is still much unknown over the best protocol used. We describe two patients who were prescribed cabergoline as a preventive measurement, and who started experiencing symptoms after stopping the treatment. The first patient is a 26 year old women suffering from primary infertility. After ovarian stimulation using a long protocol and human gonadotropins 150 IU during 15 days, 18 oocytes were retrieved, of which 15 were mature and with IVF 14 fertilized. From the egg retrieval patient was stared on cabergoline once a day 0.5 mg for the duration of 8 days. A single blastocyst grade A was transferred on day 5, and 7 were suitable for cryopreservation. After stopping the cabergoline, patient developed symptoms of feeling unwell, nausea and vomiting with abdominal distension and shortness of breath. An transvaginal ultrasound revealed a moderate amount of free fluid in the abdomen with enlarges ovaries. Patient was admitted and treated conservatively. A positive pregnancy test was performed and a viable intra uterine singleton pregnancy was confirmed by ultrasound. The second patient was 32 years of age and treated for primary infertility based on male factor. After ovarian stimulation using a long protocol with recombinant gonadotrophins 300IU egg collections was performed retrieving 26 oocytes of which 15 were mature. Unfortunatly a failed fertilization occurred after ICSI with PESA sperm. This patient also developed symptoms after the course of cabergoline which was prescribed at egg collection had stopped. These two cases can be an illustration that a dopamine agonist like cabergoline may be of use for prevention of OHSS. But the optimal treatment protocol still needs to be established by future research. P066: Two patients developing ovarian hyperstimulation (OHSS) after stopping cabergoline MIRIAM BAUMGARTEN1, RAJ MATHUR2 & NICK RAINE-FENNING1 1 Nottingham University Research and Treatment Unit in Reproduction and Embryology [NURTURE], Division of Obstetrics and Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK and 2Addenbrooke’s Hospital NHS Trust, Cambridge University Hospitals NHS Foundation Trust, Cambridge Biomedical Campus, Cambridge, UK Objective: This survey aims to describe current practice regarding prevention and management of OHSS, with a view to identifying and prioritizing areas of practice that clinicians feel need to be addressed by clinical trials. Methods: The survey was conducted amongst all UK clinicians involved with ovarian stimulation and IVF. All IVF units were contacted by email, through the BFS news letter and forum, with the request to fill out an online questionnaire. Results: So far 32 questionnaires have been completed. The most accepted classification of OHSS (92%) is that used in the RCOG guideline. Pre- existing risk factors for the development of OHSS were identified as, in order of importance, previous OHSS, polycystic ovarian syndrome (PCOS), high anti-mullerian hormone, high antral follicle count, polycystic ovaries on ultrasound, young age and slim build. The three most used pretreatment preventive measurements are reducing the starting dose of gonadotrophins, GnRH-antagonist protocol and metformin in case of PCOS. For cycles assessed being at risk of OHSS during stimulation, interventions in order of most practiced, are reducing the dose of gonadotrophins, freezing all embryos and coasting. Indications for which admission is always advised (60%) include dyspnea, clinical ascites, poor urine output, abnormal liver/kidney function and signs of hemoconcentration. Most frequently used treatment of OHSS is dopamine agonist (62%). Protocols differ significantly between clinics. Conclusion: There appears to be consensus concerning classification and risk factors for OHSS, but not on preventive measurements or treatment. Future research should focus on this, addressing questions that are prioritized by practicing clinicians. Patient involvement in framing study questions and design is important. The survey is ongoing and a higher response rate will provide a more adequate representation of current UK practice. We urge all clinicians to express their opinion on this important challenge to delivering safe care for our patients. Human Fertility Abstracts e63 P067: Ovarian stimulation in women with malignant disease gives a higher oocyte yield compared to their healthy counterparts RAVNEET SIRHA, STUART LAVERY, ANNA CARBY & JOSEPH ELIAHOO IVF Hammersmith Hospital, Statistical Advisory service, Imperial College, London, UK Objective: To evaluate the response to standard local protocols for ovarian stimulation in cancer and non cancer patients in the context of fertility preservation. Design: Retrospective. Setting: Academic fertility unit. Patients: 89 women with a diagnosis of cancer underwent stimulation cycles for fertility preservation. Their results were compared to a control group of 176 healthy women undergoing stimulation for IVF/ISCI. They were matched for age/ year of treatment/ protocol used/ type of fertility treatment. All patients were treated using local unit protocols. Intervention: Controlled ovarian stimulation and oocyte retrieval. Main outcome measure: Number of oocytes retrieved, total FSH dose and days of stimulation. Relevance: Fertility preservation is a growing field as survival rates form cancer are on the rise. It is important to identify differences in response to ovarian stimulation in cancer patients to avoid subjecting these women to lengthy and repetitive cycles of induction, delaying life saving oncological treatment. If differences are identified stimulation cycles can be modified for this group of women to allow them the best possible chance at fertility. Results: No differences were found in the total FSH dose, days of stimulation required or number of oocytes/ unit FSH. There was statistically higher oocyte yield from cancer patients compared to non cancer controls (p 0.02). Discussion/Conclusions: In contrast to recent literature suggesting a reduced oocyte retrieval in women with malignant disease, our data has highlighted a higher oocyte yield in these women. This novel finding may give us the scope to use lower doses of stimulation drugs therefore minimising the side effects and discomfort experienced, for the same final oocyte count as non cancer patients. Whilst optimisation of ovarian stimulation protocols in all patients is important, oncology patients may only have one opportunity to retrieve oocytes, emphasising the critical nature of planning treatment protocols and stimulation doses. P068: Spontaneous ovarian hyperstimulation syndrome – pathophysiological classification and diagnostic algorithm NIKOLETTA PANAGIOTOPOULOU Royal Oldham Hospital, Pennine Acute Hospitals NHS Trust, Oldham, Lancashire, UK Background: Spontaneous Ovarian Hyperstimulation Syndrome (sOHSS) is an extremely rare condition that occurs in the absence of ovarian stimulation treatment. Its aetiology is not fully understood; suggested causative factors include hypersecretion of glycoprotein hormones (hCG, TSH, FSH and LH) and/ or mutation of FSH and LH receptors. Aims: To understand the origins of sOHSS and facilitate the communication among clinicians and patients. Methods: Literature review with particular regard to pathogenesis. Results: A comprehensive literature search of electronic databases, including MEDLINE, EMBASE, AMED, CINAHL, revealed 63 cases, with date of last check the 1st of September 2012. A diagnostic algorithm of bilateral enlarged multicystic ovaries in early pregnancy is proposed. A suggested pathophysiological classification system of sOHSS which entails four types: type I corresponds to the mutated FSHr cases with normal hCG, TSH and FSH levels; type II corresponds to cases secondary to high hCG levels; type III is related to hypothyroidism with high TSH levels; and type IV is related to gonadotrophin adenomas secreting FSH or LH. Conclusions: The proposed sOHSS pathophysiological classification could assist in reporting new cases and lead to better understanding of its origin. Moreover, it will improve communication between clinicians and help with the investigation, treatment and counseling of patients. P069: Perifollicular blood flow and its impact on follicular fluid cytokines N. ELLISSA BASKIND, VINAY SHARMA, NICOLAS ORSI & NIGEL SIMPSON Leeds Centre for Reproductive Medicine, Leeds Teaching Hospitals NHS Trust; University of Leeds, Leeds, UK Aims: The oocyte and somatic cells of the ovarian follicle communicate with each other via cytokines and growth factors in an inter-dependant manner and many of these have pro- and anti-angiogenic properties. The stromal © 2013 The British Fertility Society e64 Abstracts vascularity supports synthesis of precursors for oestrogen synthesis by granulosa cells (androstenedione and testosterone) whilst the vascularity surrounding the follicle also supplies the developing oocyte with oxygen, nutrients and hormones that are crucial in enabling normal maturation of the follicle–oocyte unit. This study aimed to examine the correlation between follicular fluid (FF) pro- and anti-angiogenic cytokines, their impact on the peri-follicular blood flow (PBF) and oocyte quality. Methods: The FF from individual follicles and plasma from patients undergoing IVF/ IVF-ICSI (n 25) was retrieved following controlled ovarian hyperstimulation. The PBF of each follicle aspirated was assessed using power Doppler prior to oocyte retrieval and the blood flow was graded according to the Chui classification (Grade A: 25%; Grade B: 25% to 50%; Grade C: 50% to 75%; Grade D: 75%). For the purpose of analysis, A or B were defined as low and C or D as high-grade vascularity. In our programme, oocyte/embryo culture in single droplets enabled longitudinal tracking of each oocyte to its natural developmental fate. The FF and plasma cytokine levels (interleukin (IL)-6, tumour necrosis factor (TNF)-α and interferon (IF)-γ) were determined by multiplex immunoassay. Data were analysed using mixed-model logistic regression analysis. Results: High-grade PBF positively predicted normal fertilization and clinical pregnancy following embryo transfer. Pro-angiogenic FF IL-6 combined with high grade PBF was predictive of greater oocyte maturity whilst, conversely, anti-angiogenic interferon-γ together with low grade PBF was negatively associated with oocyte maturity (P 0.05). Conclusions: Follicular vascularity relates to FF cytokine levels and these in turn, impact oocyte maturity and developmental potential. We found evidence for a correlation between PBF, oocyte fertilization rate and cycle outcome. This correlation suggests that the impact of increased stromal vascularity in predisposing conditions such as PCOS on the rate and quality of oocyte maturation needs to be studied. P070: MAGE-11 (Melanoma antigen gene protein 11) profiling in fertile, infertile PCOS and endometriosis human endometrium KINZA YOUNAS, DEYA GONZALEZ, LEWIS FRANCIS, JOHN WHITE, LISA JOELS & STEVE CONLAN Institute of Life Science, Swansea University, College of Medicine and Singleton Hospital, Swansea, UK Background: Implantation failure remains an unsolved problem inreproductive medicine. Around 1 in 7 couples are involuntarily childless and the averageimplantation rate in IVF is around 25%. Inadequate uterine receptivity is responsible for approximatelytwo-thirds of implantation failure. Factors affecting uterine receptivity include the hyper-androgenic condition PCOS, and endometriosis. MAGE-11 is an Androgen Receptor (AR) coregulator that modulates AR amino- and carboxyl-terminal interaction to increase AR transcriptional activity. MAGE-11 is expressed in tissues and cell lines of the human female reproductive tract in a manner that correlates with AR. In human endometrium highest levels of MAGE-11 mRNA and protein coincide with the window of uterine receptivity to embryo implantation. The role of MAGE-11 and AR in human endometrium is relatively ill-defined but chronic androgen stimulation is associated with adverse effects on reproductive function. The objective of our study is to define gene expression of MAGE-11 in human endometrium of fertile and infertile PCOS and endometriosis patients. Materials and Methods: Endometrial samples obtained from fertile, ovulatory PCOS; anovulatory PCOS and endometriosis women. Endometrial expression of AR and MAGE-11 was quantified by RT-PCR and immunohistochemistry (IHC). Results: Peak mRNA and protein for AR were observed during proliferative phase (p 0.001) and MAGE-11 during secretory phase (p 0.001) in normally cycling fertile endometrium. No difference was noted for protein and mRNA expression among fertile and endometriosis patients in proliferative or secretory phase of the menstrual cycle. In ovulatory and anovulatory PCOS loss of cyclical expression for AR and MAGE-11 was observed by IHC. When compared with fertile patients, high endometrial AR and MAGE-11 mRNA and protein expression was observed in PCOS patients, regardless of their ovulation status (p 0.001). Conclusion: MAGE-11 mRNA and protein expression is elevated through the menstrual cycle in infertile PCOS endometrium compared to fertile endometrium and eutopic endometrium from endometriosis patients. Human Fertility Abstracts e65 P071: Use of metformin for women with polycystic ovary syndrome to improve metabolic parameters THOMAS TANG1 & ADAM BALEN2 1 Regional Fertility Centre (RFC), Royal Victoria Hospital, Belfast, Northern Ireland and 2Division of Reproduction and Early Development, Leeds Institute of Genetics, Health and Therapeutics, University of Leeds, Leeds, UK Background: Polycystic ovary syndrome(PCOS) is a common endocrine. Increased insulin resistance and compensatory hyperinsulinaemia play a key role on the pathogenesis of PCOS. PCOS also shares with metabolic syndrome a lot of common clinical and abnormal metabolic manifestations. The prevalence of metabolic syndrome among women with PCOS was estimated to be nearly two-fold higher than in the general population (43% versus 24%). These findings suggest that increased insulin resistance not only commonly affects reproductive health but also poses potential significant, long-term health risks in women with PCOS. The aim of this systematic review is to ascertain the effectiveness of metformin in improving metabolic parameters in women with PCOS. Methods: The authors searched the Cochrane Library, MEDLINE, Cumulative Index to Nursing and Allied Health Literature and EMBASE up to October 2011 for randomised trials compared metformin with placebo or no treatment for women with PCOS. Results: Thirty-eight trials were included with total participants of 3495. Metformin significantly reduced fasting insulin concentrations in the non-obese group (MD-5.65 mIU/l, 95% CI -10.25 to -1.06) but not in obese women with PCOS (MD-2.72 mIU/L, 95% CI -6.50 to 1.05). The current review showed that metformin had no effect on serum cholesterol concentrations (MD-0.14 mmol/l, 95% CI -0.31 to 0.02) or serum triglycerides (MD0.14 mmol/l, 95% CI-0.05 to 0.32). Furthermore, there was no evidence of an effect of metformin on BMI (MD-0.05, 95% CI -0.31 to 0.20). Conclusion: There is yet to be any long-term data on the use of metformin for women with PCOS in reducing the risk of developing diabetes or metabolic syndrome. Our analysis did not show that metformin is of benefit in improving weight loss, insulin sensitivity or lipid profiles. Hence, a long-term prophylactic treatment with metformin is unlikely to reduce the risk of developing metabolic syndrome. Infertility P072: Systematic management of secondary amenorrhoea-A case report SHANKARALINGAIAH NETHRA, N. AHMAD & G. AHMED Royal Oldham Hospital, Pennine Acute Hospitals NHS Trust, Oldham, Lancashire, UK A 37 yr old woman presented to a gynaecology outpatient unit with history of secondary amenorrhoea over 12 months periods. She had a child 3 yrs ago by normal vaginal delivery and a miscarriage about 18 months ago for which she needed surgical evacuation. She has been trying to conceive and not using any form of contraception over the last two years. She is medically fit and exercises about 4–5 times a week. There was no excessive weight loss or weight gain and her BMI was 20 with good appetite. She gives no history of hirsutism or hair loss. There was no history of excessive blood loss after her delivery or after miscarriage. Her menstrual history prior to the miscarriage was regular. She never complained of hot flushes or night sweats or any other symptoms of menopause. After initial consultation certain investigations including FSH, LH, Prolactin, Testosterone, oestradiol, free androgen index, Thyroid function tests and Ultrasound scan of the pelvis were carried out. A progesterone challenge test was negative and there was no withdrawal bleed with the use of combined oral contraceptive pill. Hence the decision was made for hysteroscopic assessment to rule out intrauterine adhesions. Hysteroscopy revealed intrauterine adhesions which were divided and a copper coil was inserted. She was reviewed back in clinic in 3 months and by then she had had 2 cycles of regular periods. As she was already 37 years old and quite keen to become pregnant the coil was removed and she was advised to try for the next few months. If unsuccessful would require further hysteroscopic assessment for further evaluation of the uterine cavity. Once she is pregnant she will be managed as a high risk case due to increased risk of intrauterine growth restriction and placenta accreta. There is also increased risk of miscarriage. © 2013 The British Fertility Society e66 Abstracts P073: Investigating the role of kisspeptins in mouse pregnancy WILLIAM COLLEDGE, ALICE HERREBOUDT & XAVIER D’ANGLEMONT DE TASSIGNY Clinical Pharmacology Unit, University of Cambridge, Cambridge, UK Kisspeptin signalling has become of interest in reproductive physiology due to the discovery that mutations in the kisspeptin signalling pathway prevent normal pubertal maturation in humans and mice. Mutations in GPR54, the receptor of kisspeptin, have been found to cause infertility and hypogonadotrophic hypogonadism in humans. Aside from these central regulatory roles of kisspeptins and GPR54 in reproductive function it has been suggested that they have further crucial roles in reproductive physiology, for example in ovarian and corpus luteum function, prolactin production and placentation. Kiss1 and Gpr54 knock out mice are being used to focus on the peripheral role of kisspeptin signalling in mouse pregnancy. Expression of Kiss1 and Gpr54 in wild-type placentas have been confirmed by qPCR. It has been established that there is no statistical difference in birth weight according to genotype and that there is typical Mendelian inheritance, suggesting no gross abnormalities in mutant placentas. Stereology is being used to confirm these finding. Placental transfer assays will be used to assess facilitated diffusion and active transport in the placenta. Ovary transplants suggest that there are no intrinsic defects in mutant ovaries but initial results suggest that there is a defect in progesterone biosynthesis in the corpus luteum. To over come this hormonal deficit an exogenous hormonal regime has been used to maintain pregnancy in mutant mice. So far pregnancy in mutants has been maintained until E10.5 which is strong evidence that there is a hormonal cause for infertility in the mutants. The data suggest that infertility in the mutants is caused by a hormonal deficit. There appears to be no instrinsic defects in placental development and ovarian function. Assisted conception P074: A multipurpose IVF handling medium utilizing a combination of buffers maintains pH stability and supports fertilization following ICSI JASON SWAIN1 & NADIR CIRAY2 1 University of Michigan, Ann Arbor, MI, USA and 2Bahceci Health Group, Fulya IVF Clinic, Istanbul, Turkey Introduction: Use of media containing pH buffers HEPES or MOPS are useful for minimizing environmental stress during procedures performed outside the incubator However, a single buffer may not optimize pH buffering and stability, especially over the range of temperatures encountered in the IVF lab For example, the pKa value, or maximal buffering of HEPES at 37°C is 7 31, while the pKa of MOPS is 6.98 At 25°C, these pKa values are 7.55 and 7.20, respectively. Methods: A medium containing both HEPES and MOPS (MHMTM, Irvine Scientific), was compared against a HEPES-buffered medium. pKa values were estimated from acid/base titration curves. pH stability was assessed over 1 month, w/ and w/o protein (10% SSS). Denuded sibling oocytes from patients undergoing ICSI with 6 oocytes (n 23) were randomly divided between media and injected. Fertilization and embryo development were recorded. Differences were determined using Fisher’s Exact Test. Results: Use of a medium containing both HEPES and MOPS yields a different pKa value compared to HEPES alone (∼ 7.45 vs. ∼ 7.55 @ 23°C and ∼ 7.21 vs ∼ 7.31 @ 37°C). pH stability of media was similar over 1 month (Δ 0.03 vs. 0.02), and was not affected by addition of protein. ICSI of oocytes using the dual-buffered medium yielded similar rates of fertilization (2PN) compared to HEPES-only (79.3 vs. 74.0%). No differences in abnormal fertilization were observed. No differences were apparent in embryo development on D2. The number of embryos with 10% fragmentation on D3 was significantly higher in MHM (62.7 vs. 47.0%, p 0.02). There were no differences in number or quality of blastocysts formed between treatments on D5/6. Conclusion: A medium containing both HEPES and MOPS gives excellent buffering and maintains a stable pH while supporting normal fertilization following ICSI at rates comparable to a HEPES-only medium, also yielding significantly lower D3 embryo fragmentation. Human Fertility Abstracts e67 P075: Oocytes recipients receiving 3 or 4 oocytes have a comparable live birth rate to those receiving high numbers EFSTATHIOS THEODOROU & ROBERT FORMAN CRM London, Park Lorne, 111 Park Road, London, UK Aims: The primary aim of this study was to identify whether a low number (3–4) of oocytes donated in an oocyte sharing program, affects the live birth rate (LBR) of the oocyte recipient (OR). A secondary aim was to identify whether there is a correlation of the age of the oocyte sharer (OS) with the LBR of the ORs. Methods: In a single fertility unit from 2007–2011, 395 consecutive oocyte sharing cycles were studied retrospectively. All oocyte sharing cycles for surrogacy or with the intention to freeze the embryos were excluded. Inclusion criteria included presence of both ovaries, normal FSH or AMH and not more than one unsuccessful previous IVF attempt. Results: The 395 ORs with a mean age of 41.9 5.1 years old received a mean of 8.8 3.8 (range 3 to 24) oocytes. The overall LBR was 44.6% (176/395) and multiple birth rate was 29.5%. We divided the ORs in 4 categories based on the number of the oocytes received: Group 1: 3–4, Group 2: 5–7, Group 3: 8–10, Group 4: 10 oocytes, and the observed LBR were 57.5%, 38.1%, 50.0%, and 39.8% respectively (p 0.060). We have also divided the ORs in 3 groups based on the age of the OS: Group A: 20–24, Group B: 25–29 and Group C: 30–35 years old and the observed LBR were 40.6%, 43.5% and 43.8% respectively (p 0.552). Conclusions: This is the largest series to our knowledge reporting live birth rate in an egg sharing program. The live birth rate of oocytes recipients who receive a low number of oocytes (3–4) is comparable to that of ORs who receive 5 oocytes or more and is independent to the age of the oocyte provider. P076: The effect of ethnicity on In-vitro fertilisation (IVF) outcomes: a Systematic review and meta-analysis RIMA DHILLON, ROSAMUND GRIMSHAW & ARRI COOMARASAMY Department of Obstetrics & Gynaecology, Birmingham Womens Hospital, Birmingham Women’s NHS Foundation Trust, Mindelsohn Way, Edgbaston, Birmingham, UK Background: Race and ethnicity are one of the most investigated prognostic factors in medicine today, however few studies have evaluated the role of ethnicity specifically with regard to infertility. There is wide variation in success rates with assisted conception for women from different ethnic groups. The aim of this study was to determine whether there are significant differences between ethnic groups on IVF success rates. Method: MEDLINE (from 1950 to present) EMBASE (from 1980 to present) and CINAHL (from 1981 to present) databases were searched electronically. Studies were selected if primary outcomes were live birth and or clinical pregnancy rate and where IVF/ ICSI was the only treatment given. Both fresh and frozen cycles were included. Data was collected regarding; study design, population size and treatment protocol and outcome. Where possible, the data on age, BMI and infertility diagnosis was also collected for subgroup analyses. The meta-analysis was performed using Review Manager, (version 4.2 for Windows). Each ethnic group (Black, South Asian, African American, Asian, Hispanic and Chinese) was compared with a Caucasian control for the primary and secondary outcomes. Heterogeneity was assessed by examining the χ2 and I; statistics and where relevant a sensitivity analysis was performed. Results: Fourteen studies were included in the meta-analysis. Conclusions: We hypothersise that the evidence will show that ethnicity may affect the outcome of IVF. However it is possible that this may be influenced primarily by socioeconomic factors that manifest itself as lack of access to medical treatment. The potential impact of ethnic background on chance of IVF success is an important factor to be included in the counselling of patients prior to treatment. © 2013 The British Fertility Society e68 Abstracts P077: The effect of IVF treatment on the endometrium and the subendometrium: are these changes predictive of success? SHYAMALY SUR, BRUCE CAMPBELL & NICHOLAS RAINE-FENNING Division of Obstetrics & Gynaecology, School of Clinical Science, University of Nottingham, Nottingham, UK It has been suggested there is a cyclical pattern in endometrial morphometry and subendometrial vascularity in the menstrual cycle, reflecting the changing hormonal environment. IVF-related superovulation may affect this pattern and influence endometrial receptivity. Aims: To confirm the cyclicity of subendometrial vascularity in the menstrual cycle. Is IVF associated with more profound changes due to hyperoestrogenaemia? Do women who conceive after IVF exhibit different patterns of vascularity? Methods: Prospective study: women with regular menstrual cycles, planning IVF. Studied at late-follicular and mid-luteal phases of menstrual cycle; day of final follicular maturation (FFM) and embryo transfer (EMT) in IVF cycle. Serum oestradiol (E) and progesterone (P) measurements and transvaginal 3D ultrasound to measure endometrial thickness (ET), volume (EV) and subendometrial vascularity indices. Repeated measures ANOVA: compare menstrual with IVF cycle indices. Results: 128 women studied in both their menstrual and IVF cycles. Hormone levels in IVF cycle were significantly different (p 0.01) compared to menstrual cycle: E levels remained high (10–20 fold higher than menstrual cycle) throughout; P levels showed a tenfold greater rise at EMT. ET and EV were significantly thicker through the IVF cycle than the menstrual cycle (p 0.01). IVF cycle subendometrial vascularity indices also showed a different pattern (p 0.01): IVF exaggerated the difference between preovulatory and implantational timepoints, potentially resulting in the IVF subendometrium being relatively more hypoxic at implantation. Women who conceived following IVF showed a greater increase in subendometrial vascularity pre-HCG than women who did not. Conclusions: IVF has a profound effect on subendometrial vascularity and endometrial morphometry, characterised by greater pre-ovulatory and lower implantational vascularity indices. Oestradiol levels were found to be higher throughout the IVF cycle, resulting in greater ET, EV and higher subendometrial vascularity. Relatively higher pre-HCG subendometrial vascularity during the IVF cycle was associated with pregnancy. This may suggest exaggerated peri-implantational hypoxia is advantageous to conception. Outcomes P078: Obstetric outcomes following assisted reproductive technology in a district general hospital KELLY MCNAMEE, SARA BRIGHAM & SIMON WOOD Countess of Chester NHS Foundation Trust, Countess of Chester Health Park, Liverpool Road, Chester, UK Background: Assisted reproductive technology (ART) has been associated with an increased risk of adverse perinatal outcomes, including pre-eclampsia, increased rates of labour induction (IOL) and Caesarean section (CS). In theUK, one in four ART pregnancies results in multiple births.The obstetric and neonatal risks associated with multiple gestation include preeclampsia, gestational diabetes and preterm delivery. Aim: To review the effect of assisted reproductive technology (ART) on pregnancy outcomes in order to optimise obstetric management and patient counselling. Method: All new patients receiving ART between February 2006 and April 2011 were identified. ART methods included in vitro fertilisation (IVF), IVF with intra cytoplasmic sperm injection (ICSI), frozen embryo transfer (FET) and intrauterine insemination (IUI). Case notes of patients whose ART treatment resulted in a positive pregnancy test were then analysed for pregnancy outcome and obstetric complications. Outcomes: A total of 366 patients had a positive pregnancy test however only 52% (n 191) continued to have a positive viability scan. The most common cause for infertility was male factor (35%) followed by tubal disease (11%). The cause remained unknown in a third of patients. Twin pregnancy accounted for 17% (n 29) of all pregnancies. Most patients delivered after 37 weeks (90%). IOL occurred in 29% (n 46) of pregnancies most commonly for prolonged rupture of membranes (n 12). The most common mode of delivery was vaginal birth (38%) followed by emergency CS (22%). Over 95% of singleton babies were over 2500g compared to 35% of twins. Discussion: Following a positive viability scan, pregnancy outcomes are favourable for the ART population with 90% of patients completing a term pregnancy. This percentage is reduced for twin pregnancies (73%). The number of twin pregnancies has an undeniable impact on obstetric and neonatal outcome data. Pregnancy outcomes following oocyte donation would be a beneficial adjunct to this study. Human Fertility Abstracts e69 P079: Natural cycle in-vitro fertilization in the poor responder patients at CARE Fertility Nottingham MAHA RAGUNATH, IRFANA KOITA, SHILPI SHETTY, PHILLIP LOWE, KEN DOWELL & SIMON THORNTON Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Objective: A retrospective survey of natural cycle IVF as a treatment option in the poor responder/older patient. Content: Our series follows 6 months of using natural cycle IVF as an alternative in older women with history of failed treatment cycles and poor response to stimulated IVF. The survey looked at 28 patients with an average age of 38 yrs The clinical pregnancy rate in this group of women was 47%. The protocol involved a normal day 1 FSH and oestradiol level with a baseline scan, to allow the patient to proceed. Serial USS examinations with estimations of FSH and oestrogen levels were done from Day 6 until the leading follicle reached 15 mm mean diameter. Indomethacin was started to prevent premature LH surge until the hCG administration, and transvaginal egg collection scheduled 36 hrs later. Outcome: The outcome measures included the number of cycles started, cancellation rates, and pregnancy rates per cycle, per oocyte retrieval and per transfer. Data on natural cycle IVF in all cases started. No of patients who intended to start No of cycles abandoned∗ No of cycles cancelled∗∗ Pregnancy rate per cycle started Pregnancy rate/OR Pregnancy rate/ET Clinical Pregnancy Rate 28 25% (7) 14% (3) 38% 42% 47% 47% ∗The cycles were abandoned for FSH levels 15 and Oestradiol levels 300. ∗∗The 3 cancelled cycles included premature ovulation, immature egg and arrest of embryo. Data on the group that acheived pregnancy. Average Age FSH Levels Duration of sub fertility Indication for NIVF Average no of previous stimulated cycles 38.38 11 2.77 yrs Poor Reserves 2.42 cycles Impact: Though our series started with a sceptical prognosis of outcome the results obtained with a 47% clinical pregnancy rate in a group of women with poor prognosis not only in terms of their age but also their reserves, makes this a highly suitable treatment alternative in older poor responders. Discussion: Although Initially conceived as the method of choice for women going through IVF, natural cycle IVF was abandoned in favour of COH which allowed an increase not only in oocyte recruitment but in the favourable pregnancy rates that followed (Steptoe PG et al. 1978). Diminishing ovarian response especially in older patients has put natural cycle IVF as an important treatment option in this group of patients with good results (Bassil S et al. 1999, Morgia et al.2004, Ubaldi B et al. 2005). Cycle abandonment and cancellation rates are acceptable given the particular poor prognosis these group of patients start out with. © 2013 The British Fertility Society e70 Abstracts P080: Oleoylethanolamide reduces Fallopian tube cilia beat frequency: implications for women with ectopic pregnancy JUSTIN KONJE1, ALPHA GEBEH2, JONATHON WILLETS1 & ROBERT HIRST3 1 Reproductive Sciences Section, Dept of Cancer Studies & Molecular Medicine, Robert Kilpatrick Clinical Sciences Building, Leicester Royal Infirmary, University of Leicester, Leicester, UK, 2Directorate of Womens, Perinatal & Sexual Health, Dept of Obstetrics & Gynaecology, University Hospitals of Leicester NHS Trust, Leicester Royal Infirmary, Infirmary Square, Leicester, UK and 3Department of Infection, Immunity and Inflammation, University of Leicester, Leicester, UK Background: Studies from knockout mice suggest that perturbations in oviductal endocannabinoid levels, endocannabinoid receptors (CB1) or endocannabinoid degrading enzyme (fatty acid amide hydrolase, FAAH) expression result in infertility secondary to physical trapping of embryos in their oviducts. These observations led to the hypothesis that ectopic pregnancy is associated with a perturbation in levels of endocannabinoids, their metabolising enzyme expression and that such changes are associated with impaired tubal function. Aims: To (1) quantify plasma and tubal levels of the endocannabinoid oleoylethanolamide and relate that to β-hCG levels (2) evaluate expression of FAAH and the degrading enzyme N-acyl-phosphatidyl-ethanolamine phospholipase-D (NAPE-PLD) in ectopic pregnancy and suitable controls and (3) examine the effect of oleoylethanolamide on cilia beat frequency (CBF) in tubal epithelial cells. Methods: Whole blood collected from ectopic (n 38) and normal (n 38) pregnancies was used for quantification of oleoylethanolamide levels by UHPLC-MS/MS and β-hCG by immunoassay. Fallopian tubes from ectopic and non-pregnant women were used for FAAH and NAPE-PLD quantification by RT-qPCR, immunohistochemistry and immunoblotting. Tubal epithelial cells from healthy volunteers were exposed to oleoylethanolamide and CBF analysed using high-speed digital camera mounted on a microscope. Results: Plasma oleoylethanolamide levels were significantly higher in ectopic pregnancy than in normal controls (p 0.05). 10 μM oleoylethanolamide produced a 60% reduction in CBF in Fallopian tube epithelial cells ex-vivo (p 0.05) (videos available). Ectopic pregnant women had reduced tubal FAAH expression compared to controls (p 0.05). Tubal oleoylethanolamide levels showed a trend towards higher levels. There were no differences in NAPE-PLD expression between the groups and no observed correlation between oleoylethanolamide and β-hCG levels. Conclusion: Elevated oleoylethanolamide levels and reduced FAAH expression are associated with ectopic pregnancy and may modulate cilia beating. This is the first study implicating a role for oleoylethanolamide in embryo-tubal transport. P081: Obstetric outcomes in monozygotic twins following single blastocyst transfer AMY SHARPE, NEELAM POTDAR & JANE BLOWER Leicester Fertility Centre, University Hospitals of Leicester, Leicester, UK Introduction: Monozygotic twinning (MZT) is associated with increased maternal and perinatal adverse outcomes such as miscarriage, preterm birth, pre-eclampsia, fetal growth restriction and intrauterine fetal death. Although, single embryo transfer can help to reduce the incidence of multiple births, MZT following single blastocyst transfer (SBT) is unavoidable and its emotional and financial implications can be great. In this study, we reviewed the obstetric outcomes of MZT following SBT in our local population. Methods: Retrospective cohort study from January 2010– August 2012 of women undergoing SBT. MZT was confirmed at first trimester scan and the chorionicity and amnionicity were confirmed. Fertility and Maternity databases were accessed for obtaining cycle details and obstetric outcomes. Results: During the study period, 84 SBT were performed and 5 had MZT (5/84, 6.0%). All were confirmed as monochorionic diamniotic and none presented with twin-twin transfusion syndrome. Overall, 60% of pregnancies were associated with obstetric and perinatal complications. Patient 1: Caesarean section at 333 weeks due to preeclampsia, both neonates survived and discharged home. Patient 2: Preterm spontaneous rupture of membranes (PPROM) occurred at 221 weeks, delivered at 226 weeks, and died due to extreme prematurity. Patient 3: PPROM and delivery of twins at 206 weeks (non-viable gestation). Infection by Group B Streptococcus with acute chorioamnionitis and pneumonia was identified as cause of fetal death. Patient 4: Spontaneous labour at 38 weeks, both neonates delivered by Caesarean section and discharged home. Patient 5: Ongoing pregnancy at 16 weeks with no known complications. Conclusion: MZT following SBT is unavoidable and associated with increased maternal and perinatal adverse outcomes. Chorionicity and amnionicity can give an indication of the level of risk. Our data indicates the risk of PPROM and premature labour is prevalent, potentially resulting in loss of one or both babies. Women receiving SBT should be counselled that multiple birth can occur and should be made aware of the risks of MZT. Human Fertility Abstracts e71 P082: Monozygotic twinning following single embryo transfer and potential contributory factors AMY SHARPE, JANE BLOWER & NEELAM POTDAR Leicester Fertility Centre, University Hospitals of Leicester, Leicester, UK Introduction: Monozygotic twinning (MZT) is associated with increased peri-natal morbidity and mortality combined with great emotional and financial implications. Reports of higher incidence of MZT following assisted reproductive techniques have been published extensively with a variety of hypotheses as to why it occurs. In this study, we sought to investigate the incidence and factors influencing MZT following single embryo transfer (SET) in our local population. Methods: Retrospective cohort study from January 2010–August 2012 of women undergoing SET. Clinical pregnancy (CP) was confirmed at 6 week scan and the number of fetal hearts noted. Treatment type (IVF, ICSI), patient age, day of transfer and fresh/frozen cycle were reviewed for trends. Statistical analysis was performed using two-tailed Fishers exact test. Results: 1301 embryo transfers were performed from January 2010–August 2012, of which 813 had SET with a clinical pregnancy rate (CPR) of 24.5% (n 199). There were 5 (2.5%) MZT pregnancies noted (5/199). Occurrence of MZT based on patient age ( 35 and 35 years) and treatment cycle (IVF or ICSI) showed no statistically significant difference (P 0.17 and P 0.21 respectively). Interestingly, 84 patients had blastocyst SET which resulted in the 5 MZT (5/84, 6.0%) and none resulted from cleavage stage SET (n 115). This difference was statistically significant (P 0.015). On further comparison for fresh versus frozen SET, all MZT were from fresh transfers. Conclusion: Patient age, day of transfer & zonal manipulation are all suggested causes for increasing MZT rate. Our study has also shown that extended culture increases the risk of MZT. It is vital that patients undergoing ‘blastocyst transfer’ should be counselled appropriately about the increased risks of MZT and SET should be considered to prevent higher order pregnancies. Further studies are required to identify factors that can be altered to reduce occurrence of MZT with blastocyst transfers. P083: Standard incubation versus Embryoscope incubation: a retrospective analysis of pregnancy outcome LOUISE BEST, ALISON CAMPBELL, SUE MONTGOMERY, SAM DUFFY & SIMON FISHEL Care Fertility Nottingham, Nottingham Business Park, Nottingham, UK Aim: A retrospective analysis of 942 embryo transfers clinical outcome over 14 months to see if a difference was observed between embryos cultured in a GalaxyR incubator (Eppendorf) ‘standard incubation’ and an Embryoscope (Unisense, Fertilitech, Denmark). The gas mix in both was 5.5% CO2, 5% O2 and 89.5% N2. Standard incubated embryos had a maximum of 6 development observations over 5 days compared to the 20 minute interval imaging in the embryoscope. The hypothesis was that increased embryo observations and uninterrupted culture of the Embryoscope positively increased the successful outcome of treatments. Method: Only ICSI cases were included where at least 1 egg was injected and day 3 or 5 embryo transfer was performed. Frozen embryo replacements were excluded from the data as it was not easily determined which type of incubation they were cultured in. Variables that were considered: Type of incubation Type of cycle Day of transfer Oocyte source Number of mature oocytes microinjected Patient age for autologous cycles Number of transferred embryos Results: Of 1704 egg recovery’s from May 2011 to July 2012 1248 were ICSI cases. After removing the excluded cases the clinical outcome of 942 embryo transfers were analysed for each variable. The biochemical and clinical pregnancy rate were both increased by culture in the embryoscope (50.1% vs 44.5% and 42.4% vs 36.1%) and statistically significantly different in the over 36 age group (36.9% vs 25%) P 0.025. Conclusion: The increase in clinical pregnancy rate cycles cultured in the embryoscope may be as a result of the stable incubation conditions; the reduced light exposure and disturbance; the increased information gathered on embryo development and morphology at a larger number of time points; or the use of quantitative morphokinetic parameters for selecting viable embryos and deselecting less viable embryos. © 2013 The British Fertility Society e72 Abstracts P084: Vitrification of lower grade cleavage stage embryos and pregnancy outcome SHARON BINNERSLEY, GEORGE HUGHES, AMY HATTON, VICTORIA GITTINS & JASON KASRAIE The Shropshire and Mid-Wales Fertility Centre, Royal Shrewsbury Hospital, Mytton Oak Road, Shrewsbury, Shropshire, UK Introduction: Conservation of viable embryos minimises risk to patients from repeated stimulation/egg collection, reduces costs and maximises cumulative success rates, but national practice varies greatly. Many clinics only cryopreserve top quality embryos, potentially leading to the disposal of viable embryos and unnecessary further cycles of IVF. Our clinics experience of survival rates from traditional ‘slow’ freezing, where fragmentation may provide additional foci for ice crystal formation, meant that, when our clinic introduced Vitrification in 2008, we continued to cryopreserve only embryos with 5% fragmentation. However survival and pregnancy rates using vitrification were such that from May 2010, following validation of survival rates, criteria were relaxed to allow embryos with 15% fragmentation to be stored. Materials and Methods: Retrospective analysis of 156 frozen (vitrified) embryo transfer cycles. Embryos were classified as top ( 5% fragmentation) or non-top (5 to 15% fragmentation) quality. Two embryos were transferred in all cycles. Three groups were compared: 1 Two top quality (n 109), 2 One top and one non-top (n 20), 3 two non-top (n 27) quality transferred. Vitrification cooling/warming utilised Origio media and Cryo-Bio system sealed straws. Results: There was no significant difference for patient age (p 0.48), survival rates of blastomeres in each group (97.9% vs 96.7% and 98.1%, p 0.62), biochemical pregnancy rate (36.7% vs 30.0% vs 33.3%, p 0.62), clinical pregnancy rate (20.2% vs 10.0% vs 22.2%, p 0.36), or implantation rate (12.8% vs 5% vs 12.96%, p 0.19) in all groups. Conclusion: This small retrospective study appears to show that vitrication of lower grade embryos ( 15% fragmentation) results in similar pregnancy rates to the vitrification of only top quality embryos. The resultant increase in the number of stored embryos and frozen embryo transfers decreases risk to the patient and cost to the healthcare economy whilst increasing the cumulative pregnancy rate from single ‘fresh’ IVF cycles. P085: Optimising culture conditions in the laboratory – Does continuous culture of embryos from day 3–5 impact embryo development and treatment outcome? BROOKE WILSON, PHILLIP SNELL & VAL SHAIKLY Bourn Hall Clinic, Charter Court, Newcomen Way, Colchester, Essex, UK Aims/Objectives: A review of incubator allocation was carried out to optimise temperature and CO2 stability. A new incubator plan was introduced so that all the patients having egg collection on one day were allocated to a single incubator for the duration of their culture; in addition day 4 scoring was discontinued. Our hypothesis was that embryos of patients having blastocyst culture would benefit from uninterrupted culture after media renewal on the morning of day 3 until scoring on day 5. Content: Data was reviewed retrospectively to assess the impact of the uninterrupted culture (n 1786 embryos) on blastocyst formation, blastocyst utilisation rates and pregnancy rates compared to embryos culture prior to the new incubator plan (n 3501 embryos). Relevance/Impact: It is important that in vitro culture replicates the stable conditions an embryo would experience in vivo. Implementation of an incubator plan will allow embryo culture to occur in a more constant environment between day 3 and day 5. Outcomes: No significant difference was observed between the two groups for blastocyst formation (p 0.896), blastocyst utilisation rates (p 0.131) or pregnancy rates (p 0.714) in the data set analysed. Discussion: Discontinuation of day 4 scoring and uninterrupted culture of embryos from day 3–5 of development did not appear to affect blastocyst formation, utilisation or pregnancy rates in our laboratory. However, these findings are from a limited data set and trends may be observed when analysing the culture of a larger number of embryos or blastocyst quality. It was found that the allocation of all oocytes collected on one day to a single incubator was an efficient use of culture space and facilitated the identification of embryos in the laboratory. Further analysis to identify the productivity of each incubator is in progress. Human Fertility Abstracts e73 P086: Identifying human error in the IVF laboratory using electronic witnessing SOPHIE BIRD, ALAN THORNHILL, XAVIER BRUNETTI & SHAUN ROGERS The London Bridge Fertility, Gynaecology and Genetics Centre, The Bridge Centre, One St Thomas Street, London Bridge, London, UK Aim: Electronic witnessing was introduced in IVF laboratories to provide an automated solution to regulatory requirements for double witnessing and prevent catastrophic mistakes. Following validation involving manual witnessing in parallel, an electronic witnessing system (RI-WitnessTM) has been used continuously for 19 months in our laboratory. We investigated the incidence of errors and frequency of difficulties encountered while using the system. Method: RI-WitnessTM uses Radio Frequency Identification (RFID) technology to track individual patient samples at all predefined steps of the IVF process. Workstations equipped with RFID readers accompanied by touch screens record each action involving pre-tagged (assigned) items. Self-adhesive RFID tags placed on all cultureware destined to contain gametes or embryos enable readers to assign tagged cultureware in any workstation area, thereby monitoring patient identity throughout the laboratory. We assessed the (i) true mismatch rate (i.e. introducing preallocated tags to work area whilst mid-procedure involving another patient); (ii) distribution and duration of mismatches and (iii) incidence of additional interventions required as a consequence of using RI-WitnessTM. Results: The study period (12/2010–7/2012) involved 24777 witness steps and 28178 tags. The total mismatch rate was 62/24777 (0.25%). Excluding flow-chart related mismatches (including system failures related to initial configuration e.g. cycles involving donor and recipient) and pre-allocated tags within the frequency range of the reader but outside of the workstation, the true mismatch rate was 0.117% (29/24777). All true mismatches were rectified in 10 seconds and their distribution was not confined to specific procedures, times of day or practitioner. Excluding pre-determined double manual witnessing steps, only 1% of all electronic witness steps required additional intervention from a second human. Conclusion: RI-WitnessTM is reliable and accurately records and time-stamps all laboratory procedures, identifying a consistently low true mismatch rate (0.117%) which compares favourably with published error rates of 0.21–5% for similar laboratory activities. © 2013 The British Fertility Society