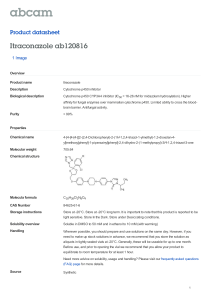
Antifungal Drugs Lorna G. Amoranto, RMT, RN, MD, DPPS Antifungal Drugs Fungal infectious occur due to : 1- Abuse of broad spectrum antibiotics 2- Decrease in the patient immunity Types of fungal infections 1. Superficial : Affect skin – mucous membrane Tinea versicolor Dermatophytes : Fungi that affect keratin layer of skin, hair, nail tinea pedis ring worm infection Candidiasis : Yeast-like oral thrush vulvo-vaginitis nail infections 2- Deep infections Affect internal organs lung – pneumonia heart – endocarditis brain - meningitis Classification of Antifungal Drugs 1- Antifungal Antibiotics : Griseofulvin Polyene macrolide : Amphotericin- B & Nystatin 2- Synthetic : Azoles : Imidazoles : Ketoconazole , Miconazole Triazoles : Fluconazole , Itraconazole Flucytosine Squalene epoxidase inhibitors Terbinafine & Naftifine Classification According to Route of Administration Systemic : Griseofulvin , Amphotericin- B , Ketoconazole , Fluconazole , Terbinafine Topical In candidiasis : Imidazoles : Ketoconazole , Miconazole. Triazoles : Terconazole Polyene macrolides : Nystatin , Amphotericin-B Gentian violet : Has antifungal & antibacterial Amphotericin B Produced by Streptomyces nodosus. Amphoteric polyene macrolide Pharmacological Effect: broad-spectrum Mechanism: binds to ergosterol in fungi (cholesterol in humans and bacteria) to form pores Pharmacokinetics: Poorly absorbed from the gastrointestinal tract More than 90% bound by serum proteins Metabolized in liver, excreted slowly in the urine Adverse Effects: Infusion-Related Toxicity: fever, chills, muscle spasms, vomiting, headache, hypotension Slower Toxicity: Renal toxicity K+↓, Mg2+↓ Anemia: erythropoietin ↓ Abnormalities of liver function Neurologic sequelae Liposomal Amphotericin B Lipid preparations reduce toxicity without sacrificing efficacy Lipid formulations distributes mostly in reticular endothelial tissue (liver, spleen, lung), but less in kidney Griseofulvin Derived from a species of penicillium Fungistatic drug Insoluble Administered in a microcrystalline form only using in the systemic treatment of dermatophytosis Deposited in newly forming skin where it binds to keratin, protecting the skin from new infection Azoles Synthetic compounds Classification: according to the number of nitrogen atoms in the five-membered azole ring Imidazoles: Ketoconazole, Miconazole, Econazole, Clotrimazole, Bifonazole Triazoles: Itraconazole, Fluconazol, Vorionazole → systemic treatment Mechanism of Action Reduction of ergosterol synthesis by inhibition of fungal cytochrome P450 enzymes Greater affinity for fungal than for human cytochrome P450 enzymes Imidazoles exhibit a lesser degree of specificity than the triazoles, accounting for their higher incidence of drug interactions and side effects Ketoconazole first oral azole introduced into clinical use Less selective for fungal P450 Inhibition of human P450 interferes with biosynthesis of adrenal and gonadal steroid hormones Alter the metabolism of other drugs Best absorbed at a low gastric pH Miconazole, Econazole, Clotrimazole Bioavailability is low by taking orally Used topically Itraconazole Its absorption is increased by food and by low gastric pH Treatment of dermatophytoses and onychomycosis The only agent with significant activity against aspergillus species Fluconazole Water soluble and good cerebrospinal fluid penetration The widest therapeutic index of the azoles Treatment and secondary prophylaxis of cryptococcal meningitis Voriconazole A broad spectrum antifungal agent Given orally or IV High oral bioavailability Penetrates tissues well including CSF Inhibit P450 Used for the treatment of invasive aspergillosis & serious infections. Reversible visual disturbances Acrylamide Include Naftifine and Terbinafine non-competitive and reversible inhibitor of Squalene epoxidase Terbinafine is synthetic, oral formulation Fungicidal Treatment of dermatophytoses, especially onychomycosis, more effective than griseofulvin or itraconazole Antituberculosis Drugs Therapeutic Goals: (1) Prevention or prophylaxis (2) Cure of clinical disease (3) Requirements: a) Prolonged therapy b)Combined therapy c) Compliance d) Prevention of development of drug resistance e) Cures, ideally, 95-100% Properties of Mycobacterium tuberculosis: a) Cell wall -- high lipid (60% dry weight) content b) Mycolic acid a major component c) Slow growth d) Survive within phagocytes Isoniazid (INH) General comments: (1) Prophylaxis as single agent (2) Cure -- ALWAYS in combination Slows development of resistance Isoniazid (INH) Antibacterial activity: Bacteriostatic at most concentrations (is bactericidal to actively growing organisms) Mechanism of action: Inhibits mycolic acid synthesis. Resistance: 1998 - 8-10% of isolates in US are resistant (10-20% in Caribbean and Southeast Asia). Organisms may be Multidrug-resistant. Adverse Effects: Allergic, Including fever, skin eruptions, hepatitis, and various kinds of rashes Hematological reactions, e.g., thrombocytopenia, agranulocytosis, eosinophilia, and anemia may occur Reversible vasculitis may occur and arthritic symptoms at various joints may be observed. Adverse Effects Most frequent -- Hepatitis 2 types a)minor increase in liver aminotransferases No need to stop drug, 10-20% of cases asymptomatic b) Clinical hepatitis in 1% can be fatal Stop drug Adverse Effects Most notable -- peripheral neuritis (including optic neuritis) in 10-20% if given > 5 mg/kg/d infrequent in standard dose of 300 mg/adult (Assuming 70 kg as standard, 300 is 4.3 mg/kg) Predisposing conditions slow acetylators Malnutrition Alcoholism Diabetes AIDS Uremia Supplement with pyridoxine (Vitamin B6) Rifampin Mechanism of Action: Binds to DNA-dependent RNA polymerase Inhibits initiation -- not elongation Antibacterial Spectrum: M. tuberculosis Bactericidal Broad spectrum of bacteria Many Gram– bacteria Chlamydia Pharmacokinetics Oral Well absorbed Broadly distributed -- even CSF Orange-red color stains tissues / secretions / urine Enterohepatic cycling and partially biotransformed in liver Drug and metabolites eliminated in feces Autoinduction of metabolism Half-life shortens 40% first 14 days of Rx Hepatic microsomal induction Clinical uses (1) Tuberculosis, Never used alone for Therapy of TB (2) Leprosy (3) Various bacterial infections, e.g., with a beta-lactam or vancomycin for staphylococcal endocarditis. Meningococcal and staphylococcal carrier states Adverse reactions Relatively safe, less than 4% in TB patients have significant reactions Drug interaction Hepatic microsomal induction Shortens half-life of many drugs Resistance Frequency of resistance is 1:106 organisms (M. tuberculosis) Develops quickly, due to changes in the beta subunit of DNA-dependent RNA polymerase Not use drug alone for TB or other bacteria Ethambutol Activity: No effect on bacteria other than mycobacteria Suppresses growth (static) of organisms resistant to streptomycin and isoniazid, i.e., no cross resistance Resistance to ethambutol develops Mechanism Not clear May interfereRNA synthesis inhibits synthesis of component of mycobacterial cell wall – arabinogalactan may increase penetration of other drugs into the organisms Clinical use Always used in combination. Adverse reactions Minimally toxic (<2%) at 15 mg/kg per day (usual dose) decreased visual acuity, rash, drug fever. Optic neuritis (reversible) -- most important adverse effect and dose related Occurs in 15% of patients receiving 50 mg/kg per day and 5% of those receiving 25 mg/kg per day and <1% 15 mg/day Decreased visual acuity and red/green color blindness Pyrazinamide Activity Bactericidal to tubercle bacilli within monocytes at 12.5 μg/ml requires slightly acidic pH Resistance develops rapidly when used alone. Mechanism: unknown Pharmacokinetics: Orally administered at 1 gram gives 45 μg/ml at 2 h and 10 μg/ml at 15 h Normal dose is 20-30 mg/kg po) Broadly distributed Eliminated primarily by glomerular filtration; also biotransformed Adverse reactions most common and serious side effect is liver injury. Other anti-tuberculosis dugs: Streptomycin Rifapentine Rifandin Para-aminosalicylic acid Ethionamide Amikacin Fluoroquinolones