!!!фонд тестовых заданий по базисной фармакологии №1 14B (Autosaved)
advertisement

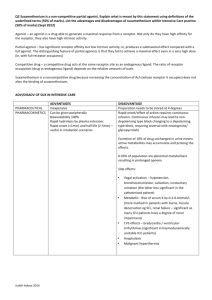
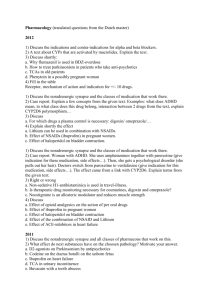
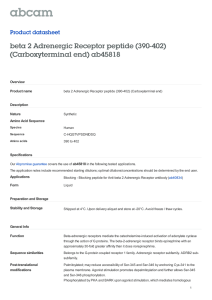
«Обсуждено»__________________ На заседании кафедры Протокол № ___от «___»____2017 зав.кафедрой д.м.н., проф. Белов Г.В. 1. What does “pharmacokinetics” include? a) Pharmacological effects of drugs b) Unwanted effects of drugs c) Chemical structure of a medicinal agent d) Distribution of drugs in the organism 2. What does “pharmacokinetics” include? a) Localization of drug action b) Mechanisms of drug action c) Excretion of substances 3. Route of administration when passage of drugs through liver is minimized: a) Oral b) Transdermal c) Rectal d) Intraduodenal 4. Route of drug administration is mostlikely to lead to the first-pass effect? a) Sublingual b) Oral c) Intravenous d) Intramuscular 5. Route of medicinal agent administration: a) Rectal b) Oral c) Sublingual d) Inhalation 6. Biotransformation of the drugs is to render them: a) Less ionized b) More pharmacologically active c) More lipid soluble d) Less lipid soluble 7. Tick the drug type for which microsomal oxidation is the most prominent: a) Lipid soluble b) Water soluble c) Low molecular weight d) High molecular weight 8. Biotransformation of a medicinal substance results in: a) Faster urinary excretion b) Slower urinary excretion c) Easier distribution in organism d) Higher binding to membranes 9. Which of the following processes proceeds in the second phase of biotransformation? a) Acetylation b) Reduction c) Oxidation d) Hydrolysis 10. Half life (t ½) doesn’t depend on: a) Biotransformation b) Time of drug absorption c) Concentration of a drug in plasma d) Rate of drug elimination 11. Elimination rate constant (Kelim) is defined by the following parameter: a) Rate of absorption b) Maximal concentration ofa substance in plasma c) Highest single dose d) Half life (t ½) 12. Stimulation of liver microsomal enzymes can: a) Require the dose increase of some drugs b) Require the dose decrease of some drugs c) Prolong the duration ofthe action of a drug d) Intensify the unwanted reaction of a drug 13. Pharmacodynamics involves the study of following? a) Mechanisms of drug action b) Biotransformation of drugs in the organism c) Distribution of drugs in the organism d) Excretion of drug from the organism 14. Pharmacodynamics involves the following? a) Information about main mechanisms of drug absorption b) Information about unwanted effects c) Information about biological barriers d) Information about excretion of a drug from the organism 15. If an agonist can produce maximal effects and has high efficacy it’s called: a) Partial agonist b) Antagonist c) Agonist-antagonist d) Full agonist 16. If an agonist can produce submaximal effects and has moderate efficacy it’s called: a) Partial agonist b) Antagonist c) Agonist-antagonist d) Full agonist 17. Tolerance and drug resistance can be a consequence of: a) Drug dependence b) Increased metabolic degradation c) Depressed renal drug excretion d) Activation of a drug after hepatic first-pass 18. The types of antagonism are: a) Summarized b) Potentiated c) Additive d) Competitive 19. Which isn’t related to a dose or to a pharmacodynamic property of a drug is called: a) Idiosyncrasy b) Hypersensitivity c) Tolerance d) Teratogenic action 20. Idiosyncratic reaction of a drug is: a) A type of hypersensitivity reaction b) A type of drug antagonism c) Unpredictable, inherent, qualitatively abnormal reaction to a drug d) Quantitatively exaggerated response 21. Tick the second messenger of G-protein-coupled (metabotropic) receptor: a) Adenylyl cyclase b) Sodium ions c) Phospholipase C d) cAMP 22. Tick the substance which change s the activity of an effector element but doesn’t belong to second messengers: a) cAMP b) cGMP c) G–protein d) Calcium ions 23. When a drug is taken continuously or repeatedly? a) Refractoriness b) Cumulative effect c) Tolerance d) Tachyphylaxis 24. What term is used to describe a decrease in responsiveness to a drug which develops in a few minutes? a) Refractoriness b) Cumulative effect c) Tolerance d) Tachyphylaxis 25. Serotonin reuptake inhibitors is: a-Imitryptaline b-Sertindole. c-Sertraline d-Buspirone 26. COMT inhibitor is: a-Enticapon b-Phenelizine c-Benzricide d-Acetazolamide 27. Non sedating antianxiety drug is: a-Propranolol b-Buspirone c-Oxizepam d-Primedone 28. Which of the following is side effect of carbamazipine except: a-Weight loss. b-Ototoxicity. c-Hypotermia d-Ataxia. 29. Which of the following drugs is not used in treatment of petit mal epilepsy: a-Ethosuxamide. b-Clonazipam c-Acetazolamide. d-Primidone 30. Which of the following is sigma receptor agonist: a-Bupropion b-Levalorphin c-Ketamine d-Nalbufin. 31. Addictive ,CNS depressant drug with profound psychological dependence and mild physical dependence is: a-Morphine b-Amphetamine c-Diazepam d-Cannabis 32. Long acting benzodiazepine is : a-Diazepam b-Oxizepam c-Medazolam d-Thiopental 33. Anoxiolytic , antiepileptic , addictive drug contraindicated in patients with porphyria is: a-Clonazepam. b-Phenobarbitone c-Carbamazepam. d-Valproic acid. 34. Non sedating, non addictive , hepatotoxic broad spectrum antiepileptic drug is: a-Ethintoin b-Carbamazipine c-Diazepam d- Valproic acid 35. Tardive dyskinesia is a side effect of which of the following drugs; a-Mepyridine b-Nortryptaline c-Isocarboxizide d-Droperidole 36. Pentazocin is used as analgesic in the treatment of: a-Headache b-Postoperative pain c-Gastritis pain d-Pain of myocardial infarction. 37. Hepatotoxic inhalation anesthetic with inadequate skeletal muscle relaxant effect is : a-Halothane b-Enflurane c-Sevoflurane d-Nitrous oxide 38. Which of the following anesthetic agents has the shortest recovery time: a-Thiopental sodium b-Ketamine c-Sufentanyl d-Propofol 39. Which one of the following has the least gastic irritant effect: a-Pyroxicam b-Meloxicam c-Ibuprofin d-Diclofenac sodium 40. Which of the followings is side effects of l-dopa: a-Abnormal movement b-Hypertension c-Constriction of muscles d-Gynecomastia. 41. To treat toxicity of acidic drugs, you must give a-Acidic substance. b-Basic substance c-Neutral substance d-Lipid soluble substance. 42. Effective dose 50 is a-The dose of the drug that produces the required response in half of the tested individuals. b-The dose of the drug that produces half maximal effect. c-The dose of the drug that produces half maximal plasma concentration. d- The dose of the drug that produces half minimal effect. 43. The drug which has rapid association and rapid dissociation with the receptors is called: a-Agonist. b-Antagonist c-Chelating agent d-Blocker 44. Drug toxicity of most drugs is exaggerated in : a-Renal patient b-Hepatic patient c-Tolerance d-Tachyphylaxis. 45. Placebo is a chemical substance which has a-Affinity and efficacy B-Affinity And no efficacy C-Efficacy and no affinity d-Neither affinity nor efficacy 46. Partial agonist has a-Partial affinity and efficacy B-Affinity And partial efficacy. C-Efficacy and partial affinity d-Neither affinity nor efficacy 47. A drug undergoing glomerular filtration: a- Highly bound to plasma proteins. b free and not bound to plasma protein. c-Has positively charged quaternary ammonium ion. d-Has low volume of distribution. 48. Using the Fick Law of Diffusion, how will flux change if membrane thickness is doubled? a) It will double b) It will quadruple c) It will halve d) It will quarter 49. To treat overdose toxicity of acidic drug ,you may perform gastric lavage with: a-Sodium bicarbonate. b-Ascorbic acid c-Saline d-Sodium chloride. 50. Drug disposition is : a-Absorption and distribution b-Distribution and metabolism c-Metabolsim and excretion d-Distribution + metabolism + excretion. 51. A decrease in renal and liver function, as seen in the elderly, would prolong drug half-life, ____ plasma protein binding, and ____ volume of distribution. a) Increase; Increase b) Decrease; Decrease c) Increase; Decrease d) Decrease; Increase 52. The lipid-soluble form of a base is ____ and the lipid-soluble form of an acid is ____. a) Protonated; Protonated b) Protonated; Unprotonated c) Unprotonated; Unprotonated d) Unprotonated; Protonated 53. The non ionized lipid soluble drug with low molecular weight is usually absorbed by: a-Pinocytosis. b-Passive diffusion c-Acitive transport d-Filtration 54. Which of the following describes an agonist? a) Any substance that brings about a change in biologic function through its chemical action b) A specific regulatory molecule in the biologic system where a drug interacts c) A drug that binds to a receptor and stimulates cellular activity d) A drug that binds to a receptor and inhibits or opposes cellular activity e) A drug directed at parasites infecting the patient 55. Half life of distribution is: a-The time required for the drug to increase its concentration to 50% of steady state concentration. b-Time required for the drug to decrease its concentration to 50% of steady state concentration. c-Time required for the drug to decrease its biological effect by 50%. d-Non of above 56. Subacute toxicity study is performed over: a-1-4 weeks. b-1-6 months. c-6-12 months d-1-2 years 57. Which of the following brain areas is outside blood brain barrier a-Choroid plexus. b-Vomiting center. c-Limbic system. c-Supraoptic nucleus of the hypothalamus. 58. What percentage of the steady-state drug concentration is achieved at 3.3 * t(1/2)? a) 10% b) 25% c) 50% d) 90%. 59. Damage at which of the following locations would most affect the goals of phase II biotransformation? a) Skin b) Kidneys c) Lungs d) Liver. 60. Acidic drugs, such bind primarily to which of the following plasma proteins? a) 1-fetoprotein . b) gamma Globulin c) Albumin. d) 1-acid glycoprotein . 61. What organ is responsible for metabolism in the “first pass effect”? a) Brain b) Heart c) Kidney d) Liver 62. Weak acids are excreted faster in ____ urine and weak bases are excreted faster in____ urine. a) Acidic; Alkaline b) Alkaline; Acidic c) Acidic; Neutral d) Neutral; Alkaline e) Alkaline; Neutral 63. To maintain a drug concentration at steady state, the dosing rate should equal the elimination rate. Which of the following is true? (CL = Drug Clearance) a) Dosing rate = CL + target concentration b) Dosing rate = CL - target concentration c) Dosing rate = CL * target concentration. d) Dosing rate = CL / target concentration 64. Which of the following metabolically active tissues is the principle organ for drug metabolism? a) Skin b) Kidneys c) Lungs d) Liver. e) GI Tract 65. What type of drugs can cross the blood-brain barrier (BBB)? a) Large and lipid-soluble b) Large and lipid-insoluble c) Small and lipid-soluble. d) Small and lipid-insoluble 66. Bioavailability is the fraction or percentage of administered drug that reaches the systemic circulation via a given route as compared to what route? a) Oral b) IV (intravenous) c) IO (intraosseous) d) CSF (cerebrospinal fluid) 67. When an inactive form of the drug is being activated in the body ,it is called a-Toxic metabolite. b-Pro-drug. c-Cleared part. d-Up regulation. 68. The cause of death in organophosphrus poisoning is: a-GIT bleeding b-Hypertension c-Respiratory failure b-Congestie heart failure 69. Psudocholinesterase inactivates: a-Succenylcholine. b-Methacholine c-Carbachol c-Curare. 70. A drug producing mydriasis without cycloplegia is: a-Homatropine. b-Pilocarpine. c-Isoprenaline d-Phenylephrine. 71. The central effect of anticholinesterase can be prevented by: a-Acetylcholine. b-Atropine. c-Methacholine d-Dopamine 72. Which of the following drugs is most likely to produce tachycardia a-Proparanolol b-Carbachol c-Neostigmine d-Trimetaphan. 73. Which of the following drugs is more likely to produce postural hypotension: a-Tolazoline. b-Metoprolol c-Ibobamine d-Bethanechol 74. Which of the following drugs stimulates nicotinic receptors a-Trimetaphane b-Carbachole. c-Phenoxybenzamine d-Atenolol. 75. Diastolic blood pressure is likely to be reduced by : a-Adrenaline b-Ibobmine c-Isoprenaline. d-Non of above 76. Which drug of the following can be used as a nasal decongestant a-Adrenaline b-Isoprnaline c-Dopamine d-Tetrahydrozoline. 77. Which of the following drugs blocks autonomic ganglia; a-Nicotine b-Hyosine c-Atropine d-D-tubocurarine. 78. which of the following does not cause bradycardia: a-Clonidine b-Reserpine c-Noradrenaline d-Prazocin. 79. Urinary retention in an elderly man is most likely to result from: a-Trimetaphan. b-Reserpine. c-Hyosine d-Atropine 80. Which of the following drugs inhibits uptake of norepinephrine by adrenergic neurons a-Tyramine . b-Amitryptayline c-Amphetamine . d-Yohimbine. General Pharmacology 81. Which of the following crosses the blood-brain barrier? A. GABA B. Propranolol C. Suxamethonium D. Edrophonium E. Dopamine 82. With regard to drug-receptor binding: A. A competitive antagonist has no intrinsic activity B. A partial agonist has less receptor affinity than a full agonist C. KD is maximal intrinsic efficacy D. KD is maximal intrinsic efficacy 83. A partial agonist: A. Always antagonises a full agonist B: Can never be used to antagonise a full agonist C: Has a dose response curve similar to that of a full agonist in the presence of a noncompetitive antagonist. D. Doesn’t have a dose response curve similar to that of a full agonist in the presence of a noncompetitive antagonist. 84. Placental transfer of drugs: A. Increases in late pregnancy B. Increases late because of decreased albumin C. Do not cross because > 600 daltons D. Decreases late because of decreased albumin 85. Therapeutic index: A. Easy to determine in humans B. Derived from HD50/ED50 C. Derived from LD50/HD50 D. Derived from LD50/ED50 General Anaesthetics - Inhalational 86. Regarding nitrous oxide at 70%: A. Synthetised from ? & N2 at 273C B. Decreases muscle blood flow by 30% C. Decreases cerebral autoregulation 24% D. Decreases muscle blood flow by 50% 87. The following drugs are (potent) triggers for malignant hyperthermia: A. Vitamin B6 B. Suxamethonium C. Bethanecol D. Pilocarpine E. Calcium F. NSAIDs 88. IPPV with Isoflurane at 1 MAC results in: A. Depresses cardiovascular reflexes more than halothane B. Causes decreased conduction velocity C. Maintains cerebral autoregulation D. Increased vasodilatation 89. The effect of increased cardiac output on Pa versus time for volatile agents is: A. Increase slope B. Decrease slope C. Decrease then increase slope D. Increase then decrease slope 90. Nitrous oxide: A. Supports combustion B. Is flammable C. Causes muscle rigidity D. In tissues is slower to reabsorb than oxygen 91. Nitrous oxide: A. Has MW of 42 B. Critical temperature 32 C C. Formed by using iron as a catalyst D. Does not support combustion 92. Sevoflurane: A. Is a methylethyl ether B. Is odourless C. Is stable in soda lime at 37 degrees D. Has a boiling point higher than enflurane 93. Sevoflurane: A. Molecular weight greater then enflurane B. MAC less than enflurane C. Contains Cl & F D. SVP > enflurane 94. Desflurane: A. Is non-irritant to the airways B. Is less potent than Sevoflurane C. Has a higher molecular weight than isoflurane D. Is a chlorinated methyl ethyl ether 95. Systemic vascular resistance is LEAST changed with: A. Isoflurane B. Sevoflurane C. Desflurane D. Halothane 96. Isoflurane & enflurane are: A. Structural isomers B. Enantiomers C. Diastereomer D. Optical isomers 97. Isoflurane: A. Is a halogenated methyl ethyl ether B. Higher boiling point than Sevoflurane C. No odour D. Enantiomer of enflurane 98. The washout of inhalational anaesthetics A. Increases with elimination by the liver B. Related considerably with the duration of anaesthesia C. Increases in the neonates compared to an adult D. Decreases in the neonates compared to an adult Anaesthetics - Intravenous 99. Thiopentone causes a decrease in BP by: A. Direct decrease in myocardial contractility B. Fall in systemic vascular resistance C. Decrease in venous tone D. Increase in venous tone Ketamine: A. Is a direct inotrope B. Causes bronchodilatation C. Less likely to see emergence delirium D. Reduces pharyngeal secretions 100. Benzodiazepine binding site on GABA receptor is: A. Near Cl- channel B. Inside the channel C. Outside the channel D. On the alpha subunit 101. The drug with the largest volume of distribution at steady state is: A. Propofol B. Midazolam C. Etomidate D. Thiopentone 102. Midazolam: A. Water soluble at physiological pH B. Undergoes oxidative metabolism C. More lipophilic than lorazepam D. Causes hypotension 103. Propofol clearance is significantly increased in: A. Elderly B. Metabolic acidosis C. Pregnancy D. Peptic ulcer 104. Ketamine: A. Direct acting negative isotope B. Indirectly acts on sympathetic nervous system peripherally C. Directly on the sympathetic ganglia D. Is a competitive antagonist at NMDA receptors 105. Propofol A. Causes decreased hepatic blood flow to influence its own clearance B. Relatively low clearance in Children C. Has a high rate of transfer from the peripheral to the central compartment on ceasing an infulsion D. Has clinically significant metabolites 106. Cocaine: A. Blocks reuptake of dopamine and noradrenaline B. Central effects are due to noradrenaline C. Crosses lipid soluble membranes because its pKa is 2.8 D. Is not metabolised by plasma pseudocholinesterase 107. Lignocaine works by: A. Altering Na+ permeability B. Altering membrane structure C. Reduced Ca++ permeability D. Increased K+ permeability 108. Regarding local anaesthetic plasma protein binding A. Is predominantly by albumin B. Is predominantly by alpha-1 acid glycoprotein C. Is greater for tetracaine than for bupivacaine D. Neonates have a greater number of binding sites 109. Hyperkalaemia with suxamethonium is associated with: A. Myotonic dystrophy B. Parkinson's disease C. Meningomyelocoele D. Cerebral palsy 110. The action of nondepolarising neuromuscular blocking agents is PROLONGED by: A. Respiratory acidosis B. Increased temperature C. Increased calcium D. Increased potassium E. Decreased magnesium 111. Which drugs (competitively) inhibit acetylcholinesterase? A. Neostigmine B. Pyridostigmine C. Physostigmine D. Edrophonium 112. Regarding vecuronium A. It accumulates in renal failure B. Is a benzylisoquinolinium C. Is a bisquaternary amine D. Is predominantly renally excreted 113. Succinylcholine can cause: A. Bradycardia B. Peptic ulcer C. ToothacheD. Hallucination) 114. Neostigmine's mechanism of action: A. Binds covalently to esteric site on AChEsterase B. Binds electrostatically to esteric site on AChEsterase C. Binds to anionic site D. Forms complex with AChEsterase with a shorter halflife than acetylcholine 115. Which of the following drugs is used for acute toxic effects of organophosphate cholinesterase inhibitors? a) Atropine b) Pilocarpine c) Pralidoxime d) Edrophonium 116. Acetylcholine is not a specific neurotransmitter at: a) Sympathetic ganglia b) Sympathetic postganglionic nerve endings c) Parasympathetic ganglia d) Parasympathetic postganglionic nerve endings 117. The mechanism of action of indirect-acting cholinomimetic agents is: a) Binding to and activation of muscarinic or nicotinic receptors b) Inhibition of the hydrolysis of endogenous acetylcholine c) Stimulation of the action of acetylcholinesterase d) Releasing acetylcholine from storage sites 118. Cholinomimetics is a drug of choice for reversing the effects of nondepolarizing neuromuscular relaxants? a) Echothiophate b) Physostigmine c) Edrophonium d) Pilocarpine 119. Stimulation of muscarinic receptors by pilocarpine and choline esters is blocked competitively by: a) Edrophonium b) Atropine c) Pralidoxime d) Echothiophate 120. Drugs is both a muscarinic and nicotinic blocker? a) Atropine b) Benztropine c) Hexamethonium d) Succinylcholine 121. Indicate a muscarinic receptor-blocking drug: a) Scopolamine b) Pipecuronium c) Trimethaphan d) Pilocarpine 122. Which of the following agents is a ganglion-blocking drug? a) Homatropine b) Hexamethonium c) Rapacuronium d) Edrophonium 123. Indicate the skeletal muscle relaxant, which is a depolarizing agent: a) Vencuronium b) Scopolamine c) Succinylcholine d) Hexamethonium 124. Which of the following drugs is a nondepolarizing muscle relaxant? a) Pancuronium b) Succinylcholine c) Hexamethonium d) Scopolamine 125. Which is rapidly and fully distributed into CNS and has a greater effect than most other antimuscarinic agents? a) Atropine b) Scopolamine c) Homatropine d) Ipratropium 126. The mechanism of atropine action is: a) Competitive ganglion blockade b) Competitive muscarinic blockade c) Competitive neuromuscular blockade d) Noncompetitive neuromuscular blockade 127. Indicate the alfa1-selective antagonist: a) Phentolamine b) Dihydroergotamine c) Prazosin d) Labetalol 128. Indicate the irreversible alfa receptor antagonist: a) Tolazoline b) Labetalol c) Prazosin d) Phenoxybenzamine 129. Which of the following drugs is an nonselective beta receptor antagonist? a) Metoprolol b) Atenolol c) Propranolol d) Acebutolol 130. Indicate the beta 1-selective antagonist: a) Propranolol b) Metoprolol c) Carvedilol d) Sotalol 131. Which of the following agents is a beta2–selective antagonist? a) Tolazolin b) Pindolol c) Ergotamin d) Butoxamine 132. Indicate the beta adrenoreceptor antagonist, which has partial beta–agonist activity: a) Propranolol b) Metoprolol c) Pindolol d) Betaxolol 133. Which of the following drugs is a reversible nonselective alfa, beta antagonist? a) Labetalol b) Phentolamine c) Metoprolol d) Propranolol 134. Indicate the indirect-acting adrenoreceptor blocking drug: a) Tolazoline b) Reserpine c) Carvedilol d) Prazosin 135. Nonselective alfa-receptor antagonists are most useful in the treatment of: a) Asthma b) Cardiac arrhythmias c) Pheochromocytoma d) Chronic hypertension 136. Which of the following drugs is useful in the treatment of pheochromocytoma? a) Phenylephrine b) Propranolol c) Phentolamine d) Epinephrine 137. Indicate adrenoreceptor antagonist agents, which are used for the management of pheochromocytoma: a) Selective beta2-receptor antagonists b) Nonselective beta-receptor antagonists c) Indirect-acting adrenoreceptor antagonist drugs d) Αlfa-receptor antagonists 138. Nonselective alfa-receptor antagonist, which is an ergot derivative: a) Ergotamine b) Prazosin c) Phenoxybenzamine d) Carvedilol 139. Which has great selectivity for alfa1a subtype: a) Prazosin b) Tamsulosin c) Phenoxybenzamine d) Phentolamine 140. Metoprolol and atenolol: a) Are members of the beta 1-selective group b) Are nonselective beta antagonists c) Have intrinsic sympathomimetic activity d) Have an anesthetic action 141. Indicate a beta receptor antagonist, which has very long duration of action: a) Metoprolol b) Propranolol c) Nadolol d) Pindolol 142. Indicate a beta receptor antagonist with intrinsic sympathomimetic activity: a) Propranolol b) Oxprenolol c) Metoprolol d) Carvedilol 143. Indicate the adrenoreceptor antagonist drug, which is a rauwolfia alkaloid: a) Prazosin b) Propranolol c) Reserpine d) Phentolamine 144. A beta-blocker, which is particularly efficacious in thyroid storm: a) Pindolol b) Sotalol c) Phentolamine d) Propranolol 145. Which of the following sympathomimetics acts indirectly? a) Epinephrine b) Norepinephrine c) Ephedrine d) Methoxamine 146. Epinephrine decreases intracellular camp levels by acting on: a) α1 receptor b) α2 receptor c) beta1 receptor d) beta2 receptor 147. Direct effects on the heart are determined largely by: a) Alfa1 receptor b) Alfa2 receptor c) Beta1 receptor d) Beta2 receptor 148. Which of the following effects is related to direct beta1-adrenoreceptor stimulation? a) Bronchodilation b) Vasodilatation c) Tachycardia d) Bradycardia 149. Alfa and beta1 adrenergic stimulation produces the same effect? a) Blood vessels b) Intestine c) Uterus d) Bronchial muscles 150. A bronchial smooth muscle contains: a) Αlfa1 receptor b) Αlfa2 receptor c) Beta 1 receptor d) Beta 2 receptor 151. Which is a direct-acting both alfa- and beta-receptor agonist: a) Norepinephrine b) Methoxamine c) Isoproterenol d) Ephedrine 152. Which of the following agents is an alfa1 alfa2 beta1 beta2 receptor agonist? a) Methoxamine b) Albuterol c) Epinephrine d) Norepinephrine 153. Indicate the direct-acting sympathomimetic, which is an alfa1 alfa2 beta1 receptor agonist: a) Isoproterenol b) Ephedrine c) Dobutamine d) Norepinephrine 154. Which of the following agents is an alfa1-selective agonist? a) Norepinephrine b) Methoxamine c) Ritodrine d) Ephedrine 155. Indicate the alfa 2-selective agonist: a) Xylometazoline b) Epinephrine c) Dobutamine d) Methoxamine 156. Nonselective beta receptor agonist? a) Norepinephrine b) Terbutaline c) Isoproterenol d) Dobutamine 157. Indicate the beta1-selective agonist: a) Isoproterenol b) Dobutamine c) Metaproterenol d) Epinephrine 158. Sympathomimetics is a beta2-selective agonist? a) Terbutaline b) Xylometazoline c) Isoproterenol d) Dobutamine 159. Indicate the indirect-acting sympathomimetic agent: a) Epinephrine b) Phenylephrine c) Ephedrine d) Isoproterenol 160. Norepinephrine produces: a) Vasoconstriction b) Vasodilatation c) Bronchodilation d) Decresed potassium concentration in the plasma 161. Isoproterenol is: a) Both an alfa- and beta-receptor agonist b) beta1-selective agonist c) beta2-selective agonist d) Nonselective beta receptor agonist 162. Ephedrine causes: a) Miosis b) Bronchodilation c) Hypotension d) Bradycardia 163. Treatment of chronic orthostatic hypotension? a) Epinephrine b) Norepinephrine c) Ephedrine d) Salmeterol 164. Which is used in a hypotensive emergency: a) Xylometazoline b) Ephedrine c) Terbutaline d) Phenylephrine 165. Sympathomimetics is preferable for the emergency therapy of cardiogenic shock? a) Epinephrine b) Dobutamine c) Isoproterenol d) Methoxamine 166. Sympathomimetics is used in the therapy of bronchial asthma? a) Formoterol b) Norepinephrine c) Methoxamine d) Dobutamine 167. The pathophysiologic basis for antiparkinsonism therapy is: a) A selective loss of dopaminergic neurons b) The loss of some cholinergic neurons c) The loss of the GABAergic cells d) The loss of glutamatergic neurons 168. Indicate the drug that induces parkinsonian syndromes: a) Chlorpromazine b) Diazepam c) Triazolam d) Carbamazepine 169. Drugs is used in the treatment of Parkinsonian disorders? a) Phenytoin b) Selegiline c) Haloperidol d) Fluoxetine 170. The treatment of the drug-induced form of parkinsonism: a) Levodopa b) Bromocriptine c) Benztropine d) Dopamine 171. Agents is the precursor of dopamine? a) Bromocriptine b) Levodopa c) Selegiline d) Amantadine 172. Indicate a peripheral dopa decarboxylase inhibitor: a) Tolcapone b) Clozapine c) Carbidopa d) Selegiline 173. The mechanism of carbidopa′s action is: a) Stimulating the synthesis, release b) Inhibition of dopa decarboxilase c) Stimulating dopamine receptors d) Selective inhibition of catecol-O-methyltransferase 174. Agents is the most helpful in counteracting the behavioral complications of levodopa? a) Tolkapone b) Clozapine c) Carbidopa d) Pergolide 175. Vitamins reduces the beneficial effects of levodopa by enhancing its extracerebral metabolism? a) Pyridoxine b) Thiamine c) Tocopherol d) Riboflavin 176. Indicate D2 receptor agonist with antiparkinsonian activity: a) Sinemet b) Levodopa c) Bromocriptine d) Selegiline 177. Antiparkinsonian drugs is an antiviral agent used in the prophylaxis of influenza A2(Antiviral) ? a) Selegiline b) Sinemet c) Pergolide d) Amantadine 178. Indicate a selective inhibitor of monoamine oxidase B: a) Levodopa b) Amantadine c) Tolcapone d) Selegiline 179. The mechanism of amantadine action is: a) Stimulating the glutamatergic neurotransmission b) Blocking the excitatory cholinergic system c) Inhibition of dopa decarboxilase d) Selective inhibition of catechol-O-methyltransferase 180. Which of the following antiparkinsonism drugs is an anticholinergic agent? a) Amantadine b) Selegilin c) Trihexyphenidyl d) Bromocriptine 181. Hypnotic drugs are used to treat: a) Psychosis b) Sleep disorders c) Narcolepsy d) Parkinsonian disorders 182. Select a hypnotic drug, which is a benzodiazepine derivative: a) Zolpidem b) Flurazepam c) Secobarbital d) Phenobarbitone 183. Tick a hypnotic agent – a barbituric acid derivative: a) Flurazepam b) Zaleplon c) Thyopental d) Triazolam 184. Select a hypnotic drug, which is an imidazopyridine derivative: a) Pentobarbital b) Temazepam c) Zolpidem d) Chloral hydrate 185. Which of the following hypnotic agents is absorbed slowly? a) Phenobarbital b) Flurazepam c) Triazolam d) Temazepam 186. Which of the following barbiturates is an ultra-short-acting drug? a) Secobarbital b) Amobarbital c) Thiopental d) Phenobarbital 187. Indicate the barbituric acid derivative, which has 4-5 days elimination half-life: a) Secobarbital b) Thiopental c) Phenobarbital d) Amobarbital 188. Hepatic microsomal drug-metabolizing enzyme induction leads to: a) Barbiturate tolerance b) Cumulative effects c) Development of physical dependence d) “hangover” effects 189. Hypnotics is preferred for elderly patients? a) Phenobarbital b) Flurozepam c) Temazepam d) Secobarbital 190. Indicate the competitive antagonist of BZ (Benzodiazepines) receptors: a) Flumazenil b) Picrotoxin c) Zolpidem d) Temazepam 191. Flumazenil blocks the actions of: a) Phenobarbital b) Morphine c) Zolpidem d) Ethanol 192. Which is an inhibitor of NMDA glutamate receptors: a) Thiopental b) Halothane c) Ketamine d) Sevoflurane 193. Which of the following general anesthetics belongs to inhalants? a) Thiopental b) Desfluran c) Ketamine d) Propofol 194. Indicate the anesthetic, which is used intravenously: a) Propofol b) Halothane c) Desflurane d) Nitrous oxide 195. Which of the following inhalants is a gas anesthetic? a) Halothane b) Isoflurane c) Nitrous oxide d) Desflurane 196. Which reduces arterial pressure and heart rate: a) Isoflurane b) Halothane c) Desflurane d) Nitrous oxide 197. Inhaled anesthetics causes centrally mediated sympathetic activation leading to a rise in blood pressure and heart rate? a) Desflurane b) Sevoflurane c) Nitrous oxide d) Isofurane 198. Which decreases the ventilatory response to hypoxia: a) Sevoflurane b) Nitrous oxide c) Desflurane d) Halothane 199. Which is an ultra-short-acting barbiturate: a) Fentanyl b) Thiopental c) Midazolam d) Ketamine 200. Indicate the intravenous anesthetic, which is a benzodiazepine derivative: a) Midazolam b) Thiopental c) Ketamin d) Propofol 201. Which of the following agents is used to accelerate recovery from the sedative actions of intravenous benzodiazepines? a) Naloxone b) Flumazenil c) Ketamine d) Fomepizole 202. Neuroleptics are used to treat: a) Neurosis b) Psychosis c) Narcolepsy d) Parkinsonian disorders 203. Most antipsychotic drugs: a) Strongly block postsynaptic d2receptor b) Stimulate postsynaptic D2 receptor c) Block NMDA receptor d) Stimulate 5-HT2 receptor 204. Hyperprolactinemia is caused by blockade of dopamine in: a) The chemoreceptor trigger zone of the medulla b) The pituitary c) The extrapiramidal system d) The mesolimbic and mesofrontal systems 205. Parkinsonian symptoms and tarditive dyskinesia are caused by blockade dopamine in: a) The nigrostriatal system b) The mesolimbic and mesofrontal systems c) The chemoreceptor trigger zone of the medulla d) The tuberoinfundibular system 206. Extrapyramidal reactions can be treated by: a) Levodopa b) Benztropine mesylate c) Bromocriptine d) Dopamine 207. Which of the following antipsychotic drugs is typical? a) Clozapine b) Quetiapine c) Haloperidol d) Olanzapine 208. Indicate the a typical antipsychotic drug: a) Haloperidol b) Clozapine c) Thioridazine d) Thiothixene 209. Antipsychotic drugs has high affinity for D4 and 5-HT2 receptors? a) Clozapine b) Fluphenazine c) Thioridazine d) Haloperidole 210. Which is a phenothiazine aliphatic derivative: a) Thiothixene b) Risperidone c) Chlorpromazine d) Clozapine 211. Indicate the antipsychotic drug, which is a butyrophenone derivative: a) Droperidol b) Thioridazine c) Sertindole d) Fluphenazine 212. Indicate the antipsychotic drug, which is a thioxanthene derivative: a) Haloperidol b) Clozapine c) Chlorpromazine d) Thiothixene 213. Drug having significant peripheral alpha-adrenergic blocking activity: a) Haloperidol b) Chlorpromazine c) Clozapine d) Risperidone 214. Indicate the antipsychotic drug having a muscarinic-cholinergic blocking activity: a) Chlorpromazine b) Clorprothixene c) Risperidone d) Haloperidol 215. Most antipsychotic drugs: a) Strongly block postsynaptic d2receptor b) Stimulate postsynaptic D2 receptor c) Block NMDA receptor d) Stimulate 5-HT2 receptor 216. Which of the following dopaminergic systems is most closely related to behavior? a) The hypothalamic-pituitary system b) The extrapyramidal system c) The mesolimbic and mesofrontal systems d) The chemoreceptor trigger zone of the medulla 217. Hyperprolactinemia is caused by blockade of dopamine in: a) The chemoreceptor trigger zone of the medulla b) The pituitary c) The extrapiramidal system d) The mesolimbic and mesofrontal systems 218. Parkinsonian symptoms and tarditive dyskinesia are caused by blockade dopamine in: a) The nigrostriatal system b) The mesolimbic and mesofrontal systems c) The chemoreceptor trigger zone of the medulla d) The tuberoinfundibular system 219. Extrapyramidal reactions can be treated by: a) Levodopa b) Benztropine mesylate c) Bromocriptine d) Dopamine 220. Which of the following antipsychotic drugs is typical? a) Clozapine b) Quetiapine c) Haloperidol d) Olanzapine 221. Indicate the atypical antipsychotic drug: a) Haloperidol b) Clozapine c) Thioridazine d) Thiothixene 222. Indicate the antipsychotic drug, which is a phenothiazine aliphatic derivative: a) Thiothixene b) Risperidone c) Chlorpromazine d) Clozapine Indicate the antipsychotic drug, which is a butyrophenone derivative: a) Droperidol b) Thioridazine c) Sertindole d) Fluphenazine 223. Indicate the antipsychotic drug, which is a thioxanthene derivative: a) Haloperidol b) Clozapine c) Chlorpromazine d) Thiothixene 224. Indicate the antipsychotic agent – a dibenzodiazepine derivative: a) Fluphenazine b) Clozapine c) Risperidone d) Droperidol 225. Antipsychotic drug having a muscarinic-cholinergic blocking activity: a) Chlorpromazine b) Clorprothixene c) Risperidone d) Haloperidol 226. Which of the following antipsychotic agents is preferable in patients with coronary and cerebrovascular disease? a) Chlorpromazine b) Fluphenazine c) Haloperidol d) Perphenazine 227. Which of the following antipsychotic agents is used in combination with an opioid drug fentanyl in neuroleptanalgesia? a) Haloperidol b) Droperidol c) Chlorpromazine d) Clozapine 228. Narcotics analgesics should: a) Relieve severe pain b) Induce loss of sensation c) Reduce anxiety and exert a calming effect d) Induce a stupor or somnolent state 229. Second-order pain is: a) Sharp, well-localized pain b) Dull, burning pain c) Associated with fine myelinated A-delta fibers d) Effectively reduced by non-narcotic analgesics 230. Which of the following mediators is found mainly in long descending pathways from the midbrain to the dorsal horn? a) Prostaglandin E b) Dynorphin c) Enkephalin d) Glutamate 231. Opioid receptor types is responsible for euphoria and respiratory depression? a) Kappa-receptors b) Delta-receptors c) Mu-receptors d) Beta receptops 232. Opioid receptor type, which is responsible for dysphoria and vasomotor stimulation: a) Kappa-receptors b) Delta-receptors c) Mu-receptors d) Beta receptors 233. which are located in the locus ceruleus or the lateral tegmental area of the reticular formation: a) Dopaminergic b) Serotoninergic c) Nonadrenergic d) Gabaergic 234. Which of the following analgesics is a phenanthrene derivative? a) Fentanyl b) Morphine c) Methadone d) Pentazocine 235. Tick narcotic analgesic, which is a phenylpiperidine derivative: a) Codeine b) Dezocine c) Fentanyl d) Buprenorphine 236. Which of the following opioid analgesics is a strong mu receptor agonist? a) Naloxone b) Morphine c) Pentazocine d) Buprenorphine 237. Indicate the narcotic analgesic, which is a natural agonist: a) Meperidine b) Fentanyl c) Morphine d) Naloxone 238. Which of the following opioid analgesics is a partial mu receptor agonist? a) Morphine b) Methadone c) Buprenorphine d) Sufentanyl 239. Partial agonists opioids are a. buprenorphine b. morphine c. fentanyl d. nalexene 240. Moderate agonists opioids are a. codeine b. morphine c. naloxone d. fentanyl 241. Strong agonists opioids are a.morphine b. codeine c. naloxone d. naltrexone 242. Naloxene has a half-life of a. 15-30mins b. 30-50mins c. 30-81.mins d. 30-95mins 243. Time to peak effect of morphine is a. 10 min b. 15 min c. 20 min d. 25 min 244. Morphine is conjugated with glucoronic acid in the… a. kidney b. brain c. liver d. stomach 245. Which of the following CNS stimulants are the agents of selective effect? a) Analeptics b) General tonics c) Psychostimulants d) Actoprotectors 246. Indicate CNC stimulating drugs, which are the agents of general action: a) Nootropic agents b) Analeptics c) Psychostimulants d) Antidepressants 247. Which of the following agents belongs to psychostimulants? a) Meridil b) Camphor c) Piracetam d) Pantocrin 248. Indicate the nootropic agent: a) Sydnocarb b) Eleuterococci extract c) Fluoxetine d) Piracetam 249. Which of the following agents is a respiratory analeptic? a) Piracetam b) Sydnocarb c) Bemegride d) Pantocrin 250. Indicate the CNC stimulating drug, which belongs to adaptogens: a) Amphetamine b) Eleuterococci extract c) Caffeine d) Sydnocarb 251. Actoprotectors are: a) Stimulators, improving physical efficiency b) Cognition enhancers, improving the highest integrative brain function c) Stimulants, raising non-specific resistance towards stresses d) Agents, stimulating the bulbar respiratory and vasomotor centers 252. Adaptogens cause: a) Improvment of efficiency using physical loads and acceleration of recovery after the load b) Stimulation of respiratory and vasomotor centers c) Temporary relief of the feeling of tiredness, facilitating the professional work and fighting somnolence d) Increased resistance towards stress situations and adaptation to extreme conditions 253. Indicate the CNS stimulants, which mitigate conditions of weakness or lack of tone within the entire organism or in particular organs? a) Psychostimulants b) Analeptics c) General tonics d) Antidepressants 254. Which of the following agents is a general tone-increasing drug of plant origin? a) Meridil b) Eleuterococci′s extract c) Pantocrin d) Caffeine 255. Indicate a general tone-increasing drug, which is an agent of animal origin? a) Pantocrin b) Amphetamine c) Sydnocarb d) Camphor 256. Indicate the CNS stimulant, which is a piperidine derivative: a) Meridil b) Amphetamine c) Caffeine d) Sydnophen 257. Which of the following CNS psychostimulants is a sydnonymine derivative? a) Caffeine b) Sydnocarb c) Meridil (methylphenidate hydrochloride) d) Amphetamine 258. Sydnocarb causes: a) Decreased sense of fatigue, it facilitates the professional work and fights somnolence b) The feeling of prosperity, relaxation and euphoria c) Influx of physical and mental forces, locomotive and speech excitation d) Peripheral sympathomimetic action 259. Indicate the psychostimulant, which is a methylxantine derivative: a) Caffeine b) Sydnocarb c) Amphetamine d) Meridil 260. Which of the following psychostimulants acts centrally mainly by blocking adenosine receptors? a) Meridil b) Caffeine c) Amphetamine d) Sydnophen 261. Bemegride: a) Stimulates the medullar respiratory center (central effect) b) Stimulates hemoreceptors of carotid sinus zone (reflector action) c) Is a mixed agent (both central and reflector effects) d) Is a spinal analeptic 262. Which of the following CNS stimulants belongs to nootropics? a) Camphor b) Pantocrin c) Sydnocarb d) Piracetam 263. Indicate the CNS stimulant, which is used in pediatric medicine, as it improves the communication with the child, increases the ability to study and communication with peers, improves school-performance? a) Meridil b) Piracetam c) Bemegride d) Amphetamine 264. Which of the following CNS stimulants is used for the cerebral stroke treatment? a) Pantocrin b) Sydnocarb c) Piracetam d) Caffeine 265. contrast to morphine, heroin is: a) Used clinically b) More addictive and fast-acting c) More effective orally d) Less potent and long-acting