Current Management of Hepatic Encephalopathy - J.Bajaj 2018
advertisement

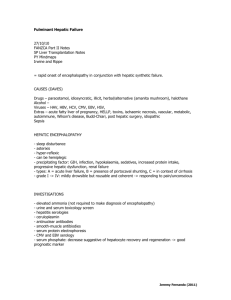
Review Article 1 Current Management of Hepatic Encephalopathy Chathur Acharya1 and Jasmohan S. Bajaj1 Hepatic encephalopathy is a state of brain dysfunction resulting from decompensation of cirrhosis. The mortality and morbidity associated with the overt form of hepatic encephalopathy are high, and even the covert form associates with poor outcomes and poor quality of life. We know that the dysfunction is not just an acute insult to the brain but rather results in long-standing cognitive issues that get worse with each episode of HE. Hence, there is an urgency to accurately diagnose these conditions, start appropriate therapy, and to maintain remission. Currently, we have two mainstay pharmacological treatment options (lactulose and rifaximin), but the narrative is evolving with new therapies under trial. Microbiome manipulation resulting in a favorable change to the gut microbiota seems to be a promising new area of therapy. Am J Gastroenterol https://doi.org/10.1038/s41395-018-0179-4 Introduction Hepatic encephalopathy (HE) is a serious complication of decompensated cirrhosis with a significantly high mortality if not managed appropriately and in a timely manner [1]. HE has a high prevalence affecting up to 20% of decompensated cirrhotic patients, and the first episode of overt HE (OHE) associates with a poor prognosis [1–3]. HE clinical manifestations range from a mild loss of cognitive abilities, to confusion and to coma. The AASLD and EASL have classified HE as a continuum with OHE and covert HE (CHE) as two distinct entities (Table 1) [4]. CHE is a new umbrella term introduced in 2012, covering both minimal HE (MHE) and grade 1 HE due to the unreliability of the diagnosis of grade 1, normal, and MHE on clinical examination [4–6]. In this review, CHE and MHE will be used interchangeably. Though phenotypically different, the underlying pathophysiology of CHE is like OHE and involves the neurotoxic effects of ammonia and other toxic metabolites on different regions of the brain in the setting of increased systemic inflammation [7]. Clinically OHE, as the nomenclature suggests, is noticeable to patients and caregivers, and involves significant psychosocial stresses [8]. Despite optimal treatment, the risk for recurrence of OHE is up to 40% within a month [9], making the need for efficient reliable treatment options more relevant. CHE on the other hand is not obvious but affects the patient’s health-related quality of life (HRQOL), behavior, cognition, and can adversely affect the driving skills [10, 11]. Hence, actively screening for HE during clinic visits and looking for potential precipitating factors should be the clinician’s prerogative. The treatment strategies, i.e., the pharmacological basis and clinical approach for these manifestations of cerebral dysfunction in cirrhosis will be discussed here (Tables 2 and 3). Basic Principles Underlying the Management of HE All decompensated cirrhosis patients are at risk for HE given the natural progression. MHE precedes OHE [12, 13], and hence in recognized patients, extra care should be taken to monitor them for preventable precipitants of OHE. Preventive strategies should ideally be initiated for all cirrhotic patients irrespective of the HE status. An important preventive aspect to HE is the nutritional management of patients with cirrhosis (see Special topics). The current recommendation is that patients with OHE should maintain the same diet as other cirrhosis patients, as there is no evidence that restricting dietary protein will prevent episodes of OHE [14]. Despite trying to maintain nutrition, certain patients with cirrhosis suffer from sarcopenia. There is mounting evidence to suggest that sarcopenia is associated with HE [15, 16] presenting another preventive opportunity in cirrhosis. Trying to improve nutritional status and muscle mass with a high-protein diet and a before-bedtime high-protein snack [17] will in theory help with prevention. Branched-chain amino acids (BCAA), which are not readily available in the United States have been studied as a therapeutic drug to alleviate sarcopenia in cirrhosis. BCAAs have also been studied as a treatment option for OHE, but success in management of sarcopenia and OHE has been limited [18–20]. Management of HE should begin with non-pharmacological strategies before an official diagnosis. Before labeling an episode as HE related, a thorough review of medications must be done to eliminate or reduce opioids, sedatives, sleep aids, psychoactive medications, and anticholinergic medications prescribed for unclear reasons. Discontinuation should be done in consultation with the prescribing provider to prevent rebound phenomena that could alter mentation. Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University and McGuire VA Medical Center, Richmond, VA, USA. Correspondence: J.S.B. (email: jasmohan.bajaj@vcuhealth.org) Received 20 December 2017; accepted 8 June 2018 1 © 2018 the american college of gastroenterology The American Journal of Gastroenterology Review Article see related editorial on page x 2 c. Acharya, J.S. Bajaj Review Article Table 1 Nomenclature of HE Based on underlying disease A Based on Severity Based on WHC severity scale MHE Grade 1 B C Based on ISHEN severity scale Covert Grade 4 Episodic Based on precipitating factors Spontaneous Recurrent Grade 2 Grade 3 Based on time course Overt Precipitated Persistent Based on disease- A: Acute liver failure, B-Bypass/shunts, C- Cirrhosis; Based on West Haven criteria (WHC)-MHE- minimal hepatic encephalopathy, not clinically noticeable, Grade 1: Mild cognitive changes with no asterixis not easily noticed in clinics, Grade 2: Confusion, disorientation to time, asterixis, Grade 3: Disoriented to place and person, altered response to questions, Grade 4: Comatose; Based on international society for hepatic encephalopathy and nitrogen metabolism (ISHEN)- Covert Hepatic Encephalopathy: Combination of MHE and Grade 1 OHE, OHE: All other clinically obvious grades of OHE on the WHC; Based on time course- Episodic: 1 in 6 months, Recurrent: ≥2 episodes in 6 months, Persistent: constant with no reprieve: Based on precipitating etiologyPrecipitated- obvious etiology such as infection, noncompliance, Spontaneousno clear etiology Despite our best efforts to understand its natural course, the clinical course of decompensated cirrhosis, i.e., onset of OHE, onset of ascites, development of variceal bleeding, etc. is often unpredictable. Pharmacological Approaches to HE Treatment options for OHE work broadly on the principle of systemic/gut ammonia reduction and intestinal microbial modulation. Treatments are outlined below based on the mechanism of action. Similar drugs are used for treatment of an acute episode and prevention of recurrence. Table 2 provides a list of pharmacological options and Table 3 lists the studies with combination therapies. Figure 1 shows the potential targets for the various treatment options available. This section will cover acute, episodic, and recurrent OHE and CHE in detail. Pharmacological therapies to modulate the gut milieu As ammonia is a direct by-product of nitrogen metabolism, drugs that help in reducing intestine luminal nitrogen by reducing production and/or increasing excretion are our mainstay of therapy. This is mainly due to easy availability and current evidence. Therapies used for OHE and CHE are largely the same. 1. a. Non-absorbable disaccharides (lactulose and lactitol): These drugs work by few mechanisms to improve outcomes. The mechanisms could be related to a reduction of intestinal pH by production of acetic and lactic acid (via bacterial degradation of lactulose) that converts ammonia to ammonium rendering it less absorbable, and then by an osmotic laxative effect that flushes the ammonium ion out. Another potential The American Journal of Gastroenterology mechanism espoused during the pre-culture-independent microbiota techniques era was a potential prebiotic action where lactulose use was noted to result in an increase in the fecal lactobacillus count [21]. However, recent evidence with the use of culture-independent microbiota techniques has not borne this out [22]. The most likely mechanism could be related to its laxative action which unfortunately is a major reason for noncompliance besides lactulose having an unpleasant taste. On the other hand, lactitol is more tolerated owing to less diarrhea and flatulence but it is not available in United States. Given the low cost of lactulose, it is the drug of choice for initiation of therapy for HE. 2. i. Non-absorbable disaccharides for OHE: Both drugs (lactulose and lactitol) were studied before adequately powered randomized trials were required. These two medications have been studied for acute episodes and for prevention of recurrence of OHE. Uribe et al. studied lactulose as a 20% enema vs. lactitol 20% enema vs. tap water enemas given 1 l three times a day for up to 5 days in a RCT and noted that there was similar improvement in mentation and ammonia levels for lactitol and lactulose but both drugs were superior to tap water enemas [23]. Morgan et al. compared oral lactitol (26 ± 5 g/day) to oral lactulose (21 ± 5 g/day) for a duration of 5 days in acute OHE and noted significantly better performance of lactitol for clinical improvement, psychometric tests (number connection test A (NCT-A) and EEG), and the portosystemic encephalopathy index (PSEI, P < 0.001) [24]. A randomized control trial (RCT) by Sharma et al. explored the administration of albumin (1.5 g/kg/day IV) with lactulose (30–60 ml oral/NG three times a day) vs. lactulose only for acute OHE episodes for up to 10 days. Significantly improved outcomes in terms of OHE recovery within 10 days (75% vs. 53.3%, P = 0.03), length of hospital stay (6.4 ± 3.4 vs. 8.6 ± 4.3 days, P = 0.01), and lower mortality (18.3% vs. 31.6%, P < 0.05) during hospitalization in the albumin with lactulose arm compared to lactulose-only arm were noted [25]. 3. ii. Non-absorbable disaccharides for CHE: As with OHE, multiple studies have been performed with lactulose, but primarily for improvement in HRQOL and cognitive impairment as measured by psychometric tests [26–28]. All these studies showed that oral lactulose (20–30 g oral/NG three times a day given for 8–12 weeks) was superior than placebo in reversing the cognitive impairment noted pretreatment. No studies specifically for lactitol have been done so far. Due to the laxative action of lactulose, these trials have been largely open-label in design. 4. a. Antibiotics (rifaximin, miscellaneous): Rifaximin is a non-absorbable oral compound that has a complex mechanism of action. Its functional impact is due to the effects that mitigate the potentially pathogenic microbial taxa relatively sparing the commensal bacteria. A recent review has summarized the various potential mechanisms of action [29]. Rifaximin, 550 mg www.nature.com/ajg Table 2 List of current pharmacological options for management of OHE Drug Dose Undesirable effects First-line therapy for acute episodic OHE in the United States Lactulose 20 g/30 ml—30 g/45 ml 3–4 per day titrated for 2–3 bowel movements a day orally. If unable to administer orally, use a similar dose via NG or 300 ml of enemas 3–4 per day till clinical improvement is noted. Diarrhea, flatulence, and bloating. Unpleasant taste Second-line therapy for acute episodic OHE in the United States (intolerant to lactulose) Rifaximin 400–550 mg PO twice daily indefinitely No major side effects Third-line (not approved by FDA) therapy for acute episodic OHE PEG 4 l of PO or via NG tube × 1 single dose (in lieu of lactulose) None clinically in short-term use First-line therapy for prevention of recurrent OHE in the United States Lactulose 20 g/30 ml—30 g/45 ml 3–4 per day titrated for 2–3 bowel movements a day orally for low grades or use 300 ml of 3–4 per day enemas till clinical improvement is noted. Diarrhea, flatulence, and bloating. Unpleasant taste Rifaximin 400–550 mg PO twice daily in conjunction with lactulose or as monotherapy for lactulose-intolerant patients. No major side effects Experimental (not approved by FDA) therapy for secondary prophylaxis of OHE Probiotics Dose dependent on the type of mixture used No major side effects FMT One small open-label randomized clinical trial Bloating and diarrhea PEG polyethylene glycol, LOLA L-Ornithine L-Aspartate, BCAA branched-chain amino acids, GPB glycerol phenylbutyrate, FMT fecal microbiota transplant oral twice daily is currently approved for use in conjunction with lactulose as a second-line therapy for the first episode of acute OHE or first-line therapy for OHE secondary prophylaxis in patients who cannot tolerate lactulose in the United States. 5. i. Rifaximin for OHE: Rifaximin can only be administered orally in the uncrushed form. Evidence for rifaximin is strong and evolving. Rifaximin (1200 mg/day) has been compared to lactulose (30 g/day oral/NG for 15 days) and lactitol (60 g/day oral for 5–10 days) and has been shown to be superior to lactulose and lactitol for improving mentation, ammonia levels, and OHE clinical scores such as the PSE in acute episodic OHE [30, 31]. Another RCT compared rifaximin with lactulose against lactulose alone for acute episodic OHE, and noted within a 10-day period significant improvement in OHE symptoms (76% vs. 50.8%, P < 0.004), reduced length of hospital stay (5.8 ± 3.4 vs. 8.2 ± 4.6 days, P = 0.001), and reduction in mortality (23.8% vs. 49.1%, P < 0.05) at © 2018 the american college of gastroenterology the end of the study [32], in the combination arm. Under investigation is a solid-state dispersible form of rifaximin for primary prophylaxis of OHE, and preliminary data have shown promising results for OHE prevention [33, 34]. 6. ii. Rifaximin for CHE: Only rifaximin has been studied (among the antibiotics). In an RCT, rifaximin (400 mg three times a day) for 2 months was superior for reversal of psychometric tests (number and figure connection tests A, critical flicker frequency, and digit symbol test) compared to placebo (P < 0.05) [30]. Other studies have shown rifaximin (400 mg three times daily for 8 weeks) to be superior to placebo (75.5% vs. 20%, P < 0.0001), and similar to lactulose (30–120 ml/day for 3 months (73.7% vs. 69.1%)) for improvement in psychometric tests such as number and figure connection tests, picture completion, digit symbol, block design tests, and critical flicker frequency. Rifaximin compared to placebo was superior in improving HRQOL (mean sickness impact profile (SIP) score) from baseline scores (11.67 vs. 6.45, P = 0.000 for rifaximin vs. 9.86 vs. 8.51, P = 0.82 for placebo) at the end of an 8-week trial [35]. A study looking at cognition, HRQOL, and specifically driving errors on a driving simulator, noted the superiority of rifaximin (550 mg twice daily for 8 weeks) for reversal of driving errors compared to placebo (76% vs. 31%, P = 0.013) [36]. 7. iii. Other antibiotics for OHE: Aminoglycosides, i.e., neomycin and ribostamycin, can be effective for acute OHE management but are seldom used due to their systemic toxicity (nephrotoxicity and ototoxicity) despite it being FDA-approved [37, 38]. Other oral antibiotics studied but not recommended for current use are vancomycin, paromomycin, and metronidazole [39–41]. 8. a. Miscellaneous laxatives (polyethylene glycol—PEG): PEG, another osmotic laxative can be used for management of acute OHE. Its postulated mechanism of action is a flushing-out effect of ammonia from the gut-like lactulose. A single RCT comparing PEG (4-l dose ×1 over 4 h orally/NG) to lactulose only (20–30 g/day via oral/NG or 200 g/day rectal) has proven it to be superior in terms of clinical improvement over a 24-h period, documented by the HE scoring algorithm (91% vs. 52%, P < 0.01), and by a shorter median time to resolution (1 day vs. 2 days, P = 0.002) [42]. PEG has not been FDA-approved for this indication but could be a viable alternative to lactulose. 9. b. Probiotics: Probiotics are mixtures of beneficial bacteria that are hypothesized to help HE by modulating the microbiome, which results in reduced systemic inflammation but not necessarily in reduced ammonia [43–45]. Multiple available mixtures have been explored, including VLS#3, Lactobacillus GG, etc., but commercially available probiotics may not have the recommended or claimed colony count that the ones used in trials have. Therefore, the major reason The American Journal of Gastroenterology 3 Review Article current Management of Hepatic encephalopathy 4 c. Acharya, J.S. Bajaj Review Article Table 3 Combination of drug studies done for OHE and CHE Combination of drugs Study aim Results Rifaximin+lactulose vs. lactulose [82] Reversal of OHE, mortality, and length of hospitalization Rifaximin+lactulose > lactulose for all Lactulose+BCAAs vs. lactulose+maltodextrin [113] Prevention of recurrence of OHE Lactulose+BCAAs = lactulose+maltodextrin with no decrease in recurrence Lactulose+rifaximin vs. rifaximin [84] Reversal of OHE and improvement in MELD score Lactulose+rifaximin > rifaximin for all Lactulose+GPB vs. lactulose+rifaximin+GPB vs. standard of care+placebo [58] Prevention of recurrence of OHE Lactulose+GPB and lactulose+rifaximin+GPB > standard of care+placebo Lactulose vs. lactulose+probiotics vs. probiotics [50] Reversal of CHE based on psychometric tests Lactulose+probiotic > lactulose > probiotics Lactulose+albumin vs. lactulose [25] Reversal of OHE and length of hospitalization Lactulose plus albumin > lactulose alone for OHE reversal Lactulose+IV LOLA vs. placebo [55] Reversal of OHE, venous ammonia, and length of hospitalization Lactulose+LOLA > placebo. Benefit is limited to days 1–4 for OHE reversal LOLA L-Ornithine L-Aspartate, GPB glycerol phenylbutyrate, BCAAs branch-chained amino acids for the poor uptake of probiotics for HE remains the lack of pharmacological quality medications as well as the use of different formulations. 10. i. Probiotics for OHE: There is no current evidence for probiotics use in acute OHE [46]. The two major studies for use of probiotics in OHE were for secondary prophylaxis and not for acute OHE treatment [44, 47]. In the RCT by Agrawal et al., use of probiotics (three capsules a day, each capsule containing 112.5 billion lyophilized bacterial mixture) was compared to lactulose alone (30–60 ml/day), and placebo for 12 months, and was associated with a lesser rate of re-admission for OHE for those on probiotics (34.4%) and lactulose (26.5%) compared to placebo (56.9%), but no difference was noted between lactulose and probiotics (P = 0.349). The other RCT by Dhiman et al. studied VLS#3 (9 × 1011 colonyforming units per sachet, a mixture of four lactobacillus species given once daily), compared to placebo (patients were taken off lactulose/rifaximin and were placed on alternative laxatives) and noted an improvement in the Child Turcotte Pugh (CTP) score and reduced breakthrough OHE (34.8% vs. 51.6%, P = 0.12) with reduced hospitalization risk (9.7% vs. 42.2%, P = 0.02). Both the studies clearly showed that probiotics delay future OHE episodes. A study for primary prophylaxis showed that a probiotic mixture (1 × 108 colony-forming units) three times daily for 3 months prevented OHE episodes [43] in those with and without CHE history. 11. ii. Probiotics for CHE: Studies in CHE have shown a reduction in serum ammonia, inflammatory markers, endotoxemia, and improvement in cognitive abilities (as evaluated by multiple validated tests) [43, 45, 48, 49]. The RCT by Mittal et al. randomized 120 cirrhosis patients diagnosed to have MHE by NCT-A and B (or figure connection tests A and B) The American Journal of Gastroenterology and/or neurophysiological test (P-300 auditory event-related potential), to either lactulose 30–60 ml/day or probiotic (four capsules of VSL#3; total of 450 billion CFU/day) for 2 months. The probiotic group and lactulose group were similar in terms of remission (69.7% vs. 62.5%, P = 0.07). The RCT by Bajaj et al. examined the effects of Lactobacillus GG (lactobacillus GG AT strain 53103, (LGG)) vs. placebo, given daily in 30 cirrhosis patients diagnosed to have MHE by PHES and the block design test, and noted significantly reduced serum inflammatory markers and endotoxemia in the LGG group at the end of 8 weeks. There have also been multiple studies that have compared probiotics to placebo, to lactulose, to LOLA, and even a combination of lactulose with probiotics that have shown benefit, i.e., superiority or equal efficacy in reversing CHE [48–50]. The RCT by Mittal et al. compared use of lactulose 30–60 ml two times a day, probiotics 110 billion colony-forming units two times a day, LOLA 6 g three times a day for 3 months, and no treatment in 120 cirrhosis patients with MHE, and noted significant improvement in all treatment arms (P = 0.006). They also assessed HRQOL via the SIP questionnaire and found improvement in all treatment groups compared to no treatment (P = 0.001). Pharmacological therapies to affect the nitrogen balance Ammonia is generated in the intestines and is transported via the portal vein to the liver for metabolism. The liver and skeletal muscle are the main detoxifiers of ammonia to urea via the urea cycle and to glutamine via glutamine synthetase/glutaminase, respectively. Glutamine produced in the skeletal muscles enters systemic circulation and gets converted back to ammonia in the kidneys for excretion. In cirrhosis, the urea cycle is altered, and the skeletal muscle mass can be reduced due to sarcopenia, effectively resulting in a reduced detoxification of urea and other nitrogen waste products. Hence, therapies focusing on rectifying www.nature.com/ajg current Management of Hepatic encephalopathy Glutamine NH3 enters the astrocyte and gets converted to glutamine by combining with glutamate. Glutamine results in astrocytic edema and HE changes Flumazenil NH3 + Indoles + Inflammatory mediators NH3 NH3 Glutamine Urea(Reduced in cirrhosis) OPA LOLA OPA, BCAAs LOLA Reduced in cirrhosis with sarcopenia NH3 NH3 + Indoles + Inflammatory mediators GPB,SPB and OPA Increased in cirrhosis due to dysbiosis NH3 Phenylacetylglutamine excreted Lactulose Rifaximin and antibiotics FMT Intestinal microbiome Fig. 1 Areas of action for different therapies in cirrhosis and HE. HE, Hepatic encephalopathy the abnormal ammonia/nitrogen waste metabolism pathways have been developed. None of the drugs in this section are approved for first-line therapy for acute or recurrent OHE prophylaxis yet in the United States. 12. a. L-Ornithine L-Aspartate (LOLA): Both the components of LOLA are substrates for the urea cycle and therefore act in the liver to help clear ammonia in HE and other hyperammonemic conditions. Peripherally, it acts on glutamine synthetase and increases glutamine levels. LOLA has a potential beneficial effect of alleviating sarcopenia by increasing muscle substrate, i.e., glutamine [51, 52], but stoppage has resulted in a mild rebound increase in ammonia. Though not available in the United States, it is manufactured in an oral and intravenous form. 13. i. LOLA for OHE: Most of the studies done thus far have looked at IV and oral forms only for chronic grade 2 OHE (not acute OHE or grade 3,4) and noted an improvement in mentation and venous ammonia [51, 53, 54]. The evidence for the IV form for acute HE episodes is new. A recent RCT by Sidhu et al. on 193 cirrhosis patients with OHE (grade 2–4) studied IV LOLA 30 g/day vs. placebo on top of con- © 2018 the american college of gastroenterology tinued standard-of-care therapy, i.e., lactulose till clinical improvement. The study showed a benefit of IV LOLA with lactulose over lactulose only, with improvement in mentation (early (day 1–4) but not at day 5), improved recovery time (1.9 ± 0.93 vs. 2.5 ± 1.03 days, P = 0.002), and length of stay. No difference in inflammatory markers was seen. All patients were administered IV cephalosporins regardless of infection [55] and none of the patients were on rifaximin. Therefore, this needs to be replicated in other centers without the use of broad-spectrum antibiotics. 14. ii. LOLA for CHE: Given its ammonia-reducing properties, LOLA has been examined in CHE in comparison with placebo, lactulose, rifaximin, and probiotics [48, 51, 56, 57] and has shown improvement in psychometric tests, ammonia, HRQOL, and in prevention of OHE. An RCT by Kircheis et al. showed reversal of certain psychometric tests in those with MHE when given LOLA 20 g once daily as a 4-h infusion IV compared to placebo. The RCT by Alvares-da-Silva showed that in 63 cirrhosis patients with MHE, compared to placebo, LOLA 5 g given three times a day for 60 days did not treat the cognitive deficits but prevented future OHE episodes at 6 months. The American Journal of Gastroenterology Review Article NH3 5 Review Article 6 c. Acharya, J.S. Bajaj 15. a. Glycerol phenylbutyrate (GPB): GPB enhances excretion of nitrogenous waste by binding with glutamine (formed in the skeletal muscles, gut, and liver) to form phenylacetylglutamine which gets excreted in the urine. 16. i. GPB for OHE: Given this unique property, it has found validity in preventing OHE recurrence in those already on lactulose or rifaximin or both [58]. In the large phase-II RCT by Rockey et al., 178 cirrhosis patients with a history of OHE in the last 6 months, who were already on standard-of-care lactulose/rifaximin were enrolled. GPB 6 ml twice daily for 16 weeks was given. The GPB group had a lower plasma ammonia level and lower HE episodes overall (21% vs. 36%; P = 0.02) compared to placebo. GPB is available only as an oral solution. It has not been studied for acute OHE management yet and due to regulatory and logistic issues it is not available for HE patients. 17. ii. There have been no studies of GPB for CHE yet. 18. a. Ornithine phenylacetate (OPA): This drug was developed for scavenging ammonia and glutamine to aid in excretion [59]. It enhances gut, skeletal muscle, and liver glutamine synthetase activity by providing a substrate to produce glutamine and then binds the glutamine with phenylacetate to form phenylacetylglutamine for easy urinary excretion. 19. i. OPA for OHE: OPA has been studied for acute OHE and in preventing OHE recurrence. In a preliminary analysis of a large randomized trial, there was a trend toward a reduction in hospital stay duration in patients randomized to therapy. In patients who were confirmed to be hyperammonemic via a central laboratory this reduction became significant. The duration of inpatient HE tended to reduce in the active treatment arm, not in the placebo infusion group. The trial did not meet its primary endpoint (www.clinicaltrials.gov—NCT01966419) even though ammonia levels were reduced significantly. Further evidence is awaited. 20. ii. There have been no studies of OPA for CHE yet. 21. a. Branched-chain amino acids (BCAAs): Patients with cirrhosis lack sufficient BCAAs such as valine, leucine, and isoleucine. These BCAAs are essential for detoxification of ammonia in skeletal muscles during the process of glutamine synthesis. BCAAs when compared to standard high-protein diet therapies in HE were noted to be similar in terms of nitrogen balance and safety for HE precipitation [60]. They are not available in the United States and evidence is largely from Asian countries. 22. i. BCAAs for OHE: Oral and IV formulations have been compared to lactulose/neomycin to treat OHE (clinical improvement, ammonia levels, mortality, and recurrence), but so far, only the oral formulations have shown limited The American Journal of Gastroenterology benefit for OHE symptoms and none for mortality and adverse events [20, 61]. 23. ii. BCAAS for CHE: Both formulations (oral/IV) have been studied looking primarily at improvement in psychometric scores and have not shown significant clinical improvement [20]. 24. a. Sodium benzoate: This drug binds ammonia to form hippurate for excretion and results in reduction in ammonia, and hence has been applied in acute HE and was found to be equally efficacious to lactulose for reducing ammonia [62], and for clinical symptoms resolution. It is available as an oral preparation (sodium benzoate and sodium phenylacetate 10%/10%) for use in patients with urea cycle disorders and hyperammonemia but is not licensed for cirrhosis/HE in the United States. Pharmacological therapies neurotransmitter chemicals to balance intracerebral Brain neurotransmitter imbalance has been proposed as a mechanism for HE. There is evidence for this in animal models that formed the basis for clinical trials. The drug in this category that has been evaluated most is flumazenil, but it is not used currently due to poor efficacy and predisposition to seizures [63, 64]. Pharmacological therapies to reduce systemic inflammation Systemic inflammation is a major contributor too and an upregulator of neuroinflammation, that is the main pathology in HE [7]. Probiotics and antibiotics act on the microbiome and help modulate this main driving force for inflammation. Studies have looked at suppressing inflammation by using nonsteroidal drugs in animal models [65, 66] but have not been looked at in humans. Albumin is an important prognostic marker in chronic liver disease [67, 68], has great anti-inflammatory properties and immunomodulatory properties apart from being a strong oncotic agent, and has been studied in acute OHE. Importantly, albumin infusions have shown mortality benefit in infection-driven complications in decompensated cirrhosis [69], and the evidence from the studies in this section further adds to this. 25. i. Albumin for OHE: In an RCT by Simon-Talero et al., albumin use in acute OHE did not show improvement in mentation but did show improvement in mortality at 90 days (69.2% vs. saline: 40.0%; P = 0.02) compared to placebo (IV normal saline). Albumin was given as IV 1.5 g/kg on day 1 and 1 g/kg on day 3, and patients were maintained on standard of care for acute OHE. Majority of the patients in the study had infections as precipitating etiology (53.8% in albumin vs. 36.7% in saline groups). The study however had an unequal distribution of patients in both groups in terms of other complications of portal hypertension [70]. A more recent study of the use of lactulose with albumin showed that the combination is more beneficial than lactulose only for OHE [25]. In this study as well, the most common etiology for HE precipitation was infec- www.nature.com/ajg current Management of Hepatic encephalopathy 26. ii. There have been no studies of albumin for CHE yet. Miscellaneous therapies a) Zinc sulfate: Cirrhotic patients with HE have been noted to have low serum zinc levels [72]. Zinc is required in the urea cycle and therefore for ammonia detoxification. Reding et al. randomized cirrhosis patients with chronic OHE (grade 1,2) to zinc acetate 600 mg/ day × 1 week vs. placebo and noted an improvement in NCT-A [73]. Brescri et al. in an RCT on OHE grade 1, 2 cirrhosis patients, using the same dose of zinc acetate vs. standard of care for 6 months, noted an improvement in NCT-A and the PSEI test at 6 months [74]. A Cochrane analysis noted that there is insufficient data to use zinc for improvement in OHE and for improvement of HRQOL [75]. In CHE, a single RCT comparing daily zinc gluconate with antioxidants to lactulose for 3 months noted more improvement in psychometric testing in zinc with the antioxidant arm [76]. b) l-Carnitine: This drug has interesting pharmacological properties and works to remove ammonia via ureagenesis. The RCT by Malaguarnera et al. showed a reduced ammonia level, improvement in NCT-A, and clinical improvement in patients with CHE and HE at the end of 90 days of l-carnitine (2 g twice daily) compared to the placebo group [77]. The same authors looked at acetyl-l-carnitine (ACL) and its role in improving physical and mental fatigue and noted an improvement in the treatment group compared to placebo [78, 79]. For MHE, the same authors compared ACL to placebo for 90 days and noted significant differences in improvement in the ACL group compared to placebo [80]. Secondary prophylaxis for OHE As after a single episode of OHE, the chance of having another OHE episode increases, i.e., recurrence [81], and there is a strong need for prophylaxis. Lactulose with rifaximin has been shown to be superior than just lactulose in this regard (22.1% vs. 45.9% over 6 months) [82, 83] and superior to just rifaximin monotherapy (13.9% vs. 24.8% over 6 months) [84]. Apart from HE medications, antibiotic prophylaxis with either norfloxacin or trimethoprim/sulfamethoxazole daily for SBP must be considered for prevention of recurrent SBP [85] which could precipitate OHE. As norfloxacin is not available in the United States, many centers use 250 mg of ciprofloxacin daily as first line and daily trimethoprim/sulfamethoxazole as second line due to the side effect profile being better in fluoroquinolones. Interestingly, rifaximin prophylaxis for OHE may have an added benefit for SBP prophylaxis [86] but using this in combination with another antibiotic for the purpose of prophylaxis is not recommended yet. Clinical Approach to HE (OHE and CHE) We shall now discuss the real-world clinical management of OHE and CHE by way of clinical cases. © 2018 the american college of gastroenterology Management of OHE Case 1—OHE: A 59-year-old Caucasian man with chronic hepatitis C cirrhosis presents to the emergency room for confusion. He was first seen in your clinic 2 years back for a new diagnosis of HCV cirrhosis based on abnormal low platelet counts that his primary care noticed. He at that time was found to be compensated. In the emergency room, the patient is not very conversant and appears confused. History is obtained primarily by his wife who attests to this not being the first episode, and that the patient has been on lactulose therapy with 3–4 bowel movements a day for the past year. Vital signs: Blood pressure––110/70, respiratory rate––14, heart rate––66, and temperature––99.1 °F. On examination, he has jaundice, anasarca, and considerable ascites with discomfort/rebound tenderness on palpation. He is not oriented to time, place, or person and is intermittently following commands. He has asterixis. Neurological exam otherwise seems nonfocal. There is a concern for OHE. Management recommendations, i.e., the initial four-pronged approach, continued management, and secondary prophylaxis (Figs. 2 and 3) are specific to case 1. Initiate care: Stabilization and triaging are the foremost. This patient’s vital signs seem stable and he seems appropriate for the general/step-down floor (based on institutional policy). The patient obtains IV access, liver functions, the basic metabolic profile, complete blood count, and venous ammonia levels on arrival. Evaluate for alternatives: Serum/urine drug screen should be obtained. The likelihood of this being an intracranial event is low given that this is his second episode and he does not have focal deficits; therefore, imaging may be lower down in the priority list. Identify precipitating factors: A thorough evaluation of the patient’s medication list, medication compliance, drug use including alcohol use, and other psychoactive medications should be discussed with the caregiver. Ascitic fluid for diagnosis of spontaneous bacterial peritonitis should be obtained. Given his tender abdomen, consider starting ceftriaxone/cefotaxime intravenously before culture data are back or if there is a delay in obtaining the paracentesis. Consider chest X-ray, urinalysis/urine cultures, and CT scan abdomen/pelvis for potential deep-seated infections, and draw cultures for management of sepsis/infections, i.e., do a broad workup for infectious etiologies. Screening the laboratory work for electrolyte abnormalities and for acute kidney injury that could manifest with altered mentation or precipitate OHE and correcting them as appropriate will be of high value. Patients should get blood work every 24 h or more frequently based on the underlying electrolyte abnormalities. Initiate empirical therapy: Empirical therapy with lactulose 30 g or 45 ml/4–6 hourly titrated for at least 3–4 bowel movements a day should be started via a nasogastric tube (NG) if there is any doubt regarding safety of swallowing. Given this being his second episode of OHE, he should be started on rifaximin 550 mg PO BID once he can take medications orally. Management past the four-pronged approach. Course: The patient’s blood laboratory work was found to be within normal The American Journal of Gastroenterology Review Article tions (35% vs. 32%). Apart from simple infusions, the Molecular Absorbent Recirculating System (MARS) with albumin has been effective in management of OHE grade 3 and 4 [71]. 7 8 c. Acharya, J.S. Bajaj Review Article Initiate general care Initiate treatment empirically for OHE Cirrhotic with AMS Is patient employed? Obvious cognitive disabilities noted by family or patient? Evaluate for alternative etiologies Identify precipitating factors Is patient a driver? Is patients QOL poor? If patient able to protect airway admit to floor. If not ICU level of care warranted. - Intubate patient if needed - If intubated, insert NG tube and start oral lactulose 30 g each hour until bowel movements and clinical improvement. - If not intubated, and patient cannot tolerate oral lactulose, start rectal lactulose, 300 ml in 1000 ml every 2-4 hours until clinical improvement. Switch to oral lactulose 20–30 gm every 2–4 hours once clinically improved Improves: Discharge on secondary prophylaxis Cirrhotic without AMS Consider evaluation for CHE based on institutional availability General floor - Start oral lactulose 20 g every 2–4 hours until BM or clinical improvement. - If patient cannot tolerate oral lactulose, start rectal lactulose, 300 ml in 1000 ml every 2-4 hours until clinical improvement. Does not improve: - Ensure correct diagnoses - Add rifxamin 550 mg po BID - Search for refractory etiologies - Consider experimental therapies. - Multi-center study: 2 testing strategies - One-center study: locally validated one strategy - Real-world: Stroop EncephalApp, SIP questionnaire Improves: Discharge on secondary prophylaxis Negative: Consider retesting in 6 months Positive: Consider a trial of treatment with lactulose 20 g/day and reevaluate in 8 weeks. Therapy for 6 months Fig. 2 Schematic of the approach to a cirrhotic patient with/without AMS. AMS altered mental status • Stabilize airway, vital signs • Triage appropriately • Lab work • IV fluids, NG tube, antibiotics empirically if indicated • Drug screen • Psychiatric disorder • Neurological disorders • Dementia • Obstructive sleep apnea Initiate general care Evaluate for alternatives Commence empirical therapy Identify precipitating factors and reverse • Lactulose either orally or via NG tube or via enemas depending on mentation • Other therapies • Infections • GI bleeding • Electrolyte disorder • Diuretic overdose • Unidentified Fig. 3 Four guiding principles to approach a cirrhotic patient with altered mentation The American Journal of Gastroenterology www.nature.com/ajg limits, except for an elevated white blood cell count of 18,000 cells/dl with a left shift. His ascitic fluid sample shows a nucleated count of 650 cells/mm3, and the cultures came back as positive for E. coli management: the patient should be continued on IV ceftriaxone till clinical improvement. Given the high nucleated cell count, he could undergo a repeat diagnostic paracentesis on day 3 of antibiotics to check for improvement. As he improves clinically to the baseline, he should be transitioned to PO ciprofloxacin and be discharged to complete a 7-day course of antibiotics. He should also get lactulose and rifaximin for secondary prophylaxis, and PO ciprofloxacin 250 mg daily as prophylaxis for SBP to prevent recurrent OHE after completion of his 7-day course of antibiotics. The patient this time suffered from type 2, episodic, grade 2 OHE, precipitated by SBP, and further details regarding this classification can be found in the AASLD/EASL guidelines [4] and Table 1. Management of MHE/CHE Given the current lack of routine clinical testing, the diagnosis of MHE/CHE is often missed. The best approach is to optimize general care in all patients, i.e., work on preventable causes of OHE precipitation and closely monitor patients who test positive. Diagnosis is achieved with tests that examine psychometric and neurophysiological properties of the brain. The commonly used tests are the psychometric HE score (PHES), EncephalApp Stroop test, inhibitory control test, and critical flicker frequency test [4]. Four questions of the Sickness Impact Profile (SIP), an HRQOL questionnaire, have been shown to be efficacious in diagnosis of CHE [87] as a potential “real-world” application. In a clinical singlecenter setting, only one locally valid test is required for a diagnosis, but in the research multicenter setting, two locally valid tests are recommended. The caveat is that psychometric testing diagnoses mild cognitive impairment from any etiology and hence the clinical context is relevant. Patients who are on multiple psychoactive medications for psychiatric conditions, were recently started on new psychoactive medications, are actively consuming psychoactive substances, or alcohol but then the results could be falsely positive. Hence, the results must be interpreted with caution. In situations of uncertainty, it is always good to seek the counseling of a psychologist if available. With regard to treatment of CHE, most studies so far have looked at outcomes such as improvement in psychometric tests, improvement in dysbiosis and inflammation, and HRQOL. Majority of the studies did not look at prevention of hospitalization and prevention of OHE as a primary endpoint in a double-blind manner. Open-label studies and meta-analysis have concluded that lactulose does prevent OHE development in CHE [88], and probiotics are effective in preventing OHE over a 3-month period [43]. Rifaximin has not been studied with the aim of preventing OHE in patients with CHE/MHE. Case 2/CHE: A 55-year-old African-American woman with chronic hepatitis C cirrhosis presents to a clinic for a follow-up visit. She was first seen in your clinic 2 years back for a new diagnosis of HCV cirrhosis, based on abnormal low platelet counts that her primary care physician noticed. She subsequently started © 2018 the american college of gastroenterology on DAA therapy and achieved SVR in 12 weeks. She continued to remain in SVR on follow-up visits, but over the last 1 year, she started complaining of fatigue and not being herself. Clinical exam and laboratory work that you obtain on the visit are normal. You obtain her annual liver US that shows cirrhosis but no other abnormalities. Management of case 2. The patient’s symptoms of fatigue and not being her usual self, after being treated for HCV should prompt further investigation. She should be questioned about any new medications, use of psychoactive medications, and symptoms of sleep apnea, i.e., other potential causes of fatigue/altered cognition. Another important aspect that needs to be kept in mind is the presence of chronic HCV and whether it is being treated as they associate with similar symptoms. The patient should be tested/referred for testing to a center with expertise, or alternatively, the EncephalApp Stroop can be used for a quick diagnosis. Upon confirming a diagnosis, a trial of lactulose should be initiated and appropriate follow-up scheduled (Fig. 2). Ideally, it may be important to screen every cirrhotic patient for CHE, but the groups to focus on are those with advanced liver disease, who are currently employed and driving, and those complaining of cognitive and quality-of-life issues. Screening for CHE should be done in a location away from the routine clinical areas by trained personnel. Real-world tests are the animal naming test [89], and four questions of the SIP [87] or EncephalApp Stroop [90], all of which can be point-of-care. EncephalApp results can be checked for CHE using http://www.encephalapp. com, which is based on normative US data. If a nearby center or a psychologist offers official testing, consider referring the patient for an official diagnosis. CHE treatment is not mandatory for those with positive official testing but is on a case-by-case basis and done in conjunction with patient discussion. First-line treatment could be a trial of lactulose 20 g/day with an interim follow-up at 8 weeks. If the interim check at 8 weeks shows no improvement, lactulose could probably be stopped. The acceptance of lactulose varies between cohorts in Eastern and Western countries [91] and this should be taken into consideration, when considering lactulose or rifaximin. Given the subtle nature of CHE, the significant implications, careful counseling of patients, and their companions/caregivers regarding the symptoms is important for early detection. Patients who test positive irrespective of their decision to try lactulose should be monitored closely as their risk for OHE is higher. Their caregivers should also be counseled about this since it will be the first OHE episode. Special Topics Nutrition in HE It is advised to have patients maintain a high-protein high-caloric diet of 1.2–1.5 g/kg ideal body weight/day and 35–40 kcal/kg ideal body weight/day, respectively [14]. This should be spaced out over 3–4 meals a day. Small frequent meals rather than large meals are preferred [92]. For those with weight loss/sarcopenia, advise a The American Journal of Gastroenterology 9 Review Article current Management of Hepatic encephalopathy Review Article 10 c. Acharya, J.S. Bajaj dietary supplement of a nightly high-protein snack. This could be a liquid protein meal. Patients can also use peanut butter/Greek yogurt etc. Although plant and dairy proteins are presumed to be better regarding ammoniagenesis compared to animal proteins, the primary goal is to design diets that the patients will follow. We should take care to avoid dehydration through diarrhea, excessive activity, and concurrent diuretic use and not avoid fluids along with salt, unless hyponatremic. In addition, patients should be encouraged to maintain their physical activity to prevent muscle mass loss. Moderate exercise in the gym (cycling and jogging) for 30–60 min three times a week could possibly help [93]. Liver transplantation (LT) for OHE OHE is reversed post LT, but cognitive changes present preLT can persist for up to 6 months post LT [94, 95]. A study by Ahluwalia et al. noted that cognition and HRQOL continued to improve 1 year post LT in all cirrhotic patients irrespective of the OHE history [96]. Another recent study evaluating cognitive flexibility based on the EncephalApp Stroop test noted the reversal of OHE-related learning disability post LT [97]. More importantly, studies have shown that having a pre-LT diagnosis of OHE does not always predict recovery of cognitive functions post LT, rather it is the presence of pre-LT cognitive impairment that is predictive [94]. Currently, OHE (recurrent or persistent) is not an indication for listing for LT unless associated with liver failure [4]. An interesting study looked at incorporating a history of OHE into the MELD score and noted that OHE-positive patients did have a higher 6-month post-LT mortality. However, the study also noted that adding points to the MELD score for OHE predicted the mortality, and by not considering OHE in the MELD score, up to 29% of patients were misclassified for LT [98]. Given the mounting evidence of reversibility of cognitive deficits and HRQOL post LT, there is a rise in the advocacy of considering pre-LT cognitive impairment and OHE status while listing for LT. Management of post TIPS OHE There is limited evidence for prophylaxis of post TIPS OHE. Preventive strategies of ensuring that the patient has no identifiable risk factors for post TIPS OHE are the first step. These risk factors include patients without prior OHE, lower MELD score, sarcopenia, pre-TIPS cognitive impairment, and hyponatremia as risk factors that are noted to predict post TIPS OHE [99–101]. Lactulose can be given if the patient develops OHE, but prophylaxis with lactulose or rifaximin is not recommended [102]. In refractory cases, the TIPS can be reversed or downsized but this can result in increased portosystemic gradients (PSG) [103, 104]. A potential preventive strategy or metric to guide and identify those at high risk for post TIPS HE would be a low post TIPS PSG (<5 mmHg), i.e., a post TIPS portosystemic gradient of >5 mmHg could possibly prevent HE [105]. Shunt closures for recurrent/persistent OHE Recurrent OHE always has an underlying precipitating etiology. A fervent search will often reveal a spontaneous portosystemic shunt The American Journal of Gastroenterology as the etiology in up to 70% of those with persistent OHE [106]. There are multiple options for shunt closure such as coil-assisted retrograde transvenous occlusion (CARTO), plug-assisted retrograde transvenous occlusion (PARTO), and balloon-occluded retrograde transvenous occlusion (BRTO). Shunt closure by any of these methods will prevent excessive gut-based products from reaching the systemic circulation, and studies have shown that despite closure and rise in portal hypertension complications are not clinically significant [107, 108]. Driving and HE Patients with CHE and OHE have a higher risk of road traffic accidents and adverse outcomes related to the accidents [10, 109]. Most CHE patients are safe drivers and the presence of CHE does not predict the inability to drive a motor vehicle [109]. Therefore, from a medicolegal standpoint, it is not mandatory in the United States (in any state) to report a driving impairment related to a diagnosis of CHE to the DMV. However, if patients with cognitive dysfunction purely related to CHE, have a higher rate of motor vehicle crashes as gathered in questioning, they could possibly have an official evaluation by the state’s department of motor vehicles. At the very least, these patients should avoid driving long distances, driving at night, and use GPS technology to prevent navigation errors. On the other hand, recent (<3 months) or current OHE, on the other hand, does qualify as a reportable “lapses in consciousness” diagnosis that requires reporting, and in some states requires mandatory reporting [110]. It would be best practice to counsel patients about the risks and to avoid driving in OHE if patients are symptomatic and have recurrent OHE. This should be discussed with patients and caregivers and documented in the chart. Future Therapies Fecal microbial transplant: Therapies focusing on modulation of the microbiome are gaining more interest due to the increased understanding of its role in HE. There have been a few studies conducted in this field. The smallest study was on a single OHE patient, and the intervention resulted in improved cognition and favorable microbiome changes [111]. A larger trial involving patients with recurrent OHE, showed that fecal enema transplants resulted in an improvement in cognition and the fecal microbiome profile with a reduced incidence of OHE post fecal transplant [112]. Given the success of the initial trial, a more robust trial for similar populations with oral fecal capsules is underway by the same group (NCT03152188). Other newer therapies: Therapies focusing on brain GABA receptors, altered E. coli, etc, are some of the newer modalities that are being actively investigated in HE but are not near clinical use now. Conclusion There are multiple factors that determine the risk and prognosis for HE. Early recognition and correction of these factors in clinics are essential to prevent morbidity. Acute OHE management is a www.nature.com/ajg complicated dynamic process where one needs to be cognizant of precipitating factors and of the long-term effects of untreated HE. In acute OHE, a wide net needs to be cast for recognizing precipitating factors and empirical therapy started immediately. Our conventional therapies are successful in the reversal of OHE but have their own limitations. Newer therapies being studied for nitrogen excretion and microbiome manipulation (fecal transplantation) may be the future of adjunct therapy for recurrent OHE. CHE testing and management are more controversial, but the consensus so far is to screen, test, and treat on a case-by-case basis. Conflicts of interest Guarantor of the article: Jasmohan Bajaj. Specific author contributions: CA and JSB wrote the paper. Financial support: VA Merit Review I0CX001076 and NIH R21TR020204. Potential competing interests: JSB has served on Advisory Boards for Norgine, Alfa-Sigma, Ocera, Synlogic, Kaleido, and Valeant Pharmaceuticals. The other author declares no conflict of interest. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Bustamante J, Rimola A, Ventura PJ, et al. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol. 1999;30:890–5. D’Amico G, Morabito A, Pagliaro L, et al. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468–75. Coltorti M, Del Vecchio-Blanco C, Caporaso N, et al. Liver cirrhosis in Italy. A multicentre study on presenting modalities and the impact on health care resources. National Project on Liver Cirrhosis Group. Ital J Gastroenterol. 1991;23:42–8. Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715–35. Bajaj JS, Cordoba J, Mullen KD, et al. Review article: the design of clinical trials in hepatic encephalopathy–an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther. 2011;33:739–47. Reuter B, Walter K, Bissonnette J, et al. Assessment of the spectrum of hepatic encephalopathy: a Multi-Center Study. Liver Transpl. 2018;24:587– 94. Shawcross D, Jalan R. The pathophysiologic basis of hepatic encephalopathy: central role for ammonia and inflammation. Cell Mol Life Sci. 2005;62:2295–304. Bajaj JS, Wade JB, Gibson DP, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol. 2011;106:1646–53. Prasad S, Dhiman RK, Duseja A, et al. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology. 2007;45:549–59. Bajaj JS. Minimal hepatic encephalopathy matters in daily life. World J Gastroenterol. 2008;14:3609–15. Bajaj JS, Saeian K, Schubert CM, et al. Minimal hepatic encephalopathy is associated with motor vehicle crashes: the reality beyond the driving test. Hepatology. 2009;50:1175–83. Das A, Dhiman RK, Saraswat VA, et al. Prevalence and natural history of subclinical hepatic encephalopathy in cirrhosis. J Gastroenterol Hepatol. 2001;16:531–5. Romero-Gomez M, Boza F, Garcia-Valdecasas MS, et al. Subclinical hepatic encephalopathy predicts the development of overt hepatic encephalopathy. Am J Gastroenterol. 2001;96:2718–23. Amodio P, Bemeur C, Butterworth R, et al. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology. 2013;58:325–36. © 2018 the american college of gastroenterology 15. Merli M, Giusto M, Lucidi C, et al. Muscle depletion increases the risk of overt and minimal hepatic encephalopathy: results of a prospective study. Metab Brain Dis. 2013;28:281–4. 16. Hanai T, Shiraki M, Watanabe S, et al. Sarcopenia predicts minimal hepatic encephalopathy in patients with liver cirrhosis. Hepatol Res. 2017;47:1359–67. 17. Plank LD, Gane EJ, Peng S, et al. Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology. 2008;48:557–66. 18. Kitajima Y, Takahashi H, Akiyama T, et al. Supplementation with branched-chain amino acids ameliorates hypoalbuminemia, prevents sarcopenia, and reduces fat accumulation in the skeletal muscles of patients with liver cirrhosis. J Gastroenterol. 2017;53:427–37. 19. Hiraoka A, Michitaka K, Kiguchi D, et al. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29:1416–23. 20. Gluud LL, Dam G, Les I, et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;5:CD001939. 21. Riggio O, Varriale M, Testore GP, et al. Effect of lactitol and lactulose administration on the fecal flora in cirrhotic patients. J Clin Gastroenterol. 1990;12:433–6. 22. Bajaj JS, Gillevet PM, Patel NR, et al. A longitudinal systems biology analysis of lactulose withdrawal in hepatic encephalopathy. Metab Brain Dis. 2012;27:205–15. 23. Uribe M, Campollo O, Vargas F, et al. Acidifying enemas (lactitol and lactose) vs. nonacidifying enemas (tap water) to treat acute portal-systemic encephalopathy: a double-blind, randomized clinical trial. Hepatology. 1987;7:639–43. 24. Morgan MY, Hawley KE. Lactitol vs. lactulose in the treatment of acute hepatic encephalopathy in cirrhotic patients: a double-blind, randomized trial. Hepatology. 1987;7:1278–84. 25. Sharma BC, Singh J, Srivastava S, et al. A Randomized Controlled Trial comparing lactulose plus albumin versus lactulose alone for treatment of hepatic encephalopathy. J Gastroenterol Hepatol. 2016;32:1234–9. 26. Watanabe A, Sakai T, Sato S, et al. Clinical efficacy of lactulose in cirrhotic patients with and without subclinical hepatic encephalopathy. Hepatology. 1997;26:1410–4. 27. Horsmans Y, Solbreux PM, Daenens C, et al. Lactulose improves psychometric testing in cirrhotic patients with subclinical encephalopathy. Aliment Pharmacol Ther. 1997;11:165–70. 28. Dhiman RK, Sawhney MS, Chawla YK, et al. Efficacy of lactulose in cirrhotic patients with subclinical hepatic encephalopathy. Dig Dis Sci. 2000;45:1549–52. 29. Bajaj JS. Review article: potential mechanisms of action of rifaximin in the management of hepatic encephalopathy and other complications of cirrhosis. Aliment Pharmacol Ther. 2016;43(Suppl 1):11–26. 30. Bucci L, Palmieri GC. Double-blind, double-dummy comparison between treatment with rifaximin and lactulose in patients with medium to severe degree hepatic encephalopathy. Curr Med Res Opin. 1993;13:109–18. 31. Mas A, Rodes J, Sunyer L, et al. Comparison of rifaximin and lactitol in the treatment of acute hepatic encephalopathy: results of a randomized, double-blind, double-dummy, controlled clinical trial. J Hepatol. 2003;38:51–8. 32. Sharma BC, Sharma P, Lunia MK, et al. A randomized, double-blind, controlled trial comparing rifaximin plus lactulose with lactulose alone in treatment of overt hepatic encephalopathy. Am J Gastroenterol. 2013;108:1458–63. 33. Bajaj JS, Zhou H, Joong Kang D, et al. Reply. Hepatology. 2016;63:1736–7. 34. Bajaj JS, Flamm SL, Chalasani N, et al. Oral rifaximin soluble solid dispersion immediate-release 40 mg prevents development of cirrhosis-related complications: a phase 2, randomized, multicenter, double-blind, placebocontrolled trial. Hoboken, NJ:Wiley-Blackwell; 2016. 35. Sidhu SS, Goyal O, Mishra BP, et al. Rifaximin improves psychometric performance and health-related quality of life in patients with minimal hepatic encephalopathy (the RIME Trial). Am J Gastroenterol. 2011;106:307–16. 36. Bajaj JS, Heuman DM, Wade JB, et al. Rifaximin improves driving simulator performance in a randomized trial of patients with minimal hepatic encephalopathy. Gastroenterology. 2011;140:478–87 e1. The American Journal of Gastroenterology 11 Review Article current Management of Hepatic encephalopathy Review Article 12 c. Acharya, J.S. Bajaj 37. Conn HO, Leevy CM, Vlahcevic ZR, et al. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977;72:573–83. 38. Strauss E, Tramote R, Silva EP, et al. Double-blind randomized clinical trial comparing neomycin and placebo in the treatment of exogenous hepatic encephalopathy. Hepatogastroenterology. 1992;39:542–5. 39. Tarao K, Ikeda T, Hayashi K, et al. Successful use of vancomycin hydrochloride in the treatment of lactulose resistant chronic hepatic encephalopathy. Gut. 1990;31:702–6. 40. Festi D, Mazzella G, Parini P, et al. Treatment of hepatic encephalopathy with non-absorbable antibiotics. Ital J Gastroenterol. 1992;24:14–6. 41. Morgan MH, Read AE, Speller DC. Treatment of hepatic encephalopathy with metronidazole. Gut. 1982;23:1–7. 42. Rahimi RS, Singal AG, Cuthbert JA, et al. Lactulose vs polyethylene glycol 3350–electrolyte solution for treatment of overt hepatic encephalopathy: the HELP randomized clinical trial. JAMA Intern Med. 2014;174:1727–33. 43. Lunia MK, Sharma BC, Sharma P, et al. Probiotics prevent hepatic encephalopathy in patients with cirrhosis: a randomized controlled trial. Clin Gastroenterol Hepatol. 2014;12:1003–8 e1. 44. Agrawal A, Sharma BC, Sharma P, et al. Secondary prophylaxis of hepatic encephalopathy in cirrhosis: an open-label, randomized controlled trial of lactulose, probiotics, and no therapy. Am J Gastroenterol. 2012;107:1043–50. 45. Bajaj JS, Heuman DM, Hylemon PB, et al. Randomised clinical trial: Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis. Aliment Pharmacol Ther. 2014;39:1113–25. 46. Dalal R, McGee RG, Riordan SM, et al. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;2:CD008716. 47. Dhiman RK, Rana B, Agrawal S, et al. Probiotic VSL#3 reduces liver disease severity and hospitalization in patients with cirrhosis: a randomized, controlled trial. Gastroenterology. 2014;147:1327–37 e3. 48. Mittal VV, Sharma BC, Sharma P, et al. A randomized controlled trial comparing lactulose, probiotics, and L-ornithine L-aspartate in treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2011;23:725–32. 49. Pratap Mouli V, Benjamin J, Bhushan Singh M, et al. Effect of probiotic VSL#3 in the treatment of minimal hepatic encephalopathy: A non-inferiority randomized controlled trial. Hepatol Res. 2015;45:880–9. 50. Sharma P, Sharma BC, Puri V, et al. An open-label randomized controlled trial of lactulose and probiotics in the treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2008;20:506–11. 51. Kircheis G, Nilius R, Held C, et al. Therapeutic efficacy of L-ornithineL-aspartate infusions in patients with cirrhosis and hepatic encephalopathy: results of a placebo-controlled, double-blind study. Hepatology. 1997;25:1351–60. 52. Pasha Y, Leech R, Violante IR, et al. The brain-muscle axis in minimal hepatic encephalopathy (MHE): a placebo-controlled, longitudinal double-blind trial With l-Ornithine l-Aspartate (LOLA) – preliminary results. J Clin Exp Hepatol. 2017;7:S5–6. 53. Poo JL, Gongora J, Sanchez-Avila F, et al. Efficacy of oral L-ornithine-Laspartate in cirrhotic patients with hyperammonemic hepatic encephalopathy. Results of a randomized, lactulose-controlled study. Ann Hepatol. 2006;5:281–8. 54. Stauch S, Kircheis G, Adler G, et al. Oral L-ornithine-L-aspartate therapy of chronic hepatic encephalopathy: results of a placebo-controlled doubleblind study. J Hepatol. 1998;28:856–64. 55. Sidhu SS, Sharma BC, Goyal O, et al. L-ornithine L-aspartate in bouts of overt hepatic encephalopathy. Hepatology. 2017. https://doi.org/10.1002/hep.29410. 56. Alvares-da-Silva MR, de Araujo A, Vicenzi JR, et al. Oral l-ornithine-l-aspartate in minimal hepatic encephalopathy: A randomized, double-blind, placebo-controlled trial. Hepatol Res. 2014;44:956–63. 57. Sharma K, Pant S, Misra S, et al. Effect of rifaximin, probiotics, and lornithine l-aspartate on minimal hepatic encephalopathy: a randomized controlled trial. Saudi J Gastroenterol. 2014;20:225–32. 58. Rockey DC, Vierling JM, Mantry P, et al. Randomized, double-blind, controlled study of glycerol phenylbutyrate in hepatic encephalopathy. Hepatology. 2014;59:1073–83. 59. Dadsetan S, Sorensen M, Bak LK, et al. Interorgan metabolism of ornithine phenylacetate (OP)–a novel strategy for treatment of hyperammonemia. Biochem Pharmacol. 2013;85:115–23. The American Journal of Gastroenterology 60. Christie ML, Sack DM, Pomposelli J, et al. Enriched branched-chain amino acid formula versus a casein-based supplement in the treatment of cirrhosis. JPEN J Parenter Enter Nutr. 1985;9:671–8. 61. Wahren J, Denis J, Desurmont P, et al. Is intravenous administration of branched chain amino acids effective in the treatment of hepatic encephalopathy? A multicenter study. Hepatology. 1983;3:475–780. 62. Sushma S, Dasarathy S, Tandon RK, et al. Sodium benzoate in the treatment of acute hepatic encephalopathy: a double-blind randomized trial. Hepatology. 1992;16:138–44. 63. Laccetti M, Manes G, Uomo G, et al. Flumazenil in the treatment of acute hepatic encephalopathy in cirrhotic patients: a double blind randomized placebo controlled study. Dig Liver Dis. 2000;32:335–8. 64. Goh ET, Andersen ML, Morgan MY, et al. Flumazenil versus placebo or no intervention for people with cirrhosis and hepatic encephalopathy. Cochrane Database Syst Rev. 2017;8:CD002798. 65. Cauli O, Rodrigo R, Piedrafita B, et al. Inflammation and hepatic encephalopathy: ibuprofen restores learning ability in rats with portacaval shunts. Hepatology. 2007;46:514–9. 66. Chung C, Gottstein J, Blei AT. Indomethacin prevents the development of experimental ammonia-induced brain edema in rats after portacaval anastomosis. Hepatology. 2001;34:249–54. 67. Serfaty L, Aumaitre H, Chazouilleres O, et al. Determinants of outcome of compensated hepatitis C virus-related cirrhosis. Hepatology. 1998;27:1435–40. 68. Alvarez MA, Cirera I, Sola R, et al. Long-term clinical course of decompensated alcoholic cirrhosis: a prospective study of 165 patients. J Clin Gastroenterol. 2011;45:906–11. 69. Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403–9. 70. Simon-Talero M, Garcia-Martinez R, Torrens M, et al. Effects of intravenous albumin in patients with cirrhosis and episodic hepatic encephalopathy: a randomized double-blind study. J Hepatol. 2013;59:1184–92. 71. Hassanein TI, Tofteng F, Brown RS Jr., et al. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology. 2007;46:1853–62. 72. Poo JL, Rosas-Romero R, Rodriguez F, et al. Serum zinc concentrations in two cohorts of 153 healthy subjects and 100 cirrhotic patients from Mexico City. Dig Dis. 1995;13:136–42. 73. Reding P, Duchateau J, Bataille C. Oral zinc supplementation improves hepatic encephalopathy. results of a randomised controlled trial. Lancet. 1984;2:493–5. 74. Bresci G, Parisi G, Banti S. Management of hepatic encephalopathy with oral zinc supplementation: a long-term treatment. Eur J Med. 1993;2:414–6. 75. Chavez-Tapia NC, Cesar-Arce A, Barrientos-Gutierrez T, et al. A systematic review and meta-analysis of the use of oral zinc in the treatment of hepatic encephalopathy. Nutr J. 2013;12:74. 76. Mousa N, Abdel-Razik A, Zaher A, et al. The role of antioxidants and zinc in minimal hepatic encephalopathy: a randomized trial. Ther Adv Gastroenterol. 2016;9:684–91. 77. Malaguarnera M, Pistone G, Elvira R, et al. Effects of L-carnitine in patients with hepatic encephalopathy. World J Gastroenterol. 2005;11:7197–202. 78. Malaguarnera M, Vacante M, Motta M, et al. Acetyl-L-carnitine improves cognitive functions in severe hepatic encephalopathy: a randomized and controlled clinical trial. Metab Brain Dis. 2011;26:281–9. 79. Malaguarnera M, Vacante M, Giordano M, et al. Oral acetyl-L-carnitine therapy reduces fatigue in overt hepatic encephalopathy: a randomized, double-blind, placebo-controlled study. Am J Clin Nutr. 2011;93:799–808. 80. Malaguarnera M, Gargante MP, Cristaldi E, et al. Acetyl-L-carnitine treatment in minimal hepatic encephalopathy. Dig Dis Sci. 2008;53:3018–25. 81. Sharma BC, Sharma P, Agrawal A, et al. Secondary prophylaxis of hepatic encephalopathy: an open-label randomized controlled trial of lactulose versus placebo. Gastroenterology. 2009;137:885–91. 891e1 82. Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071–81. 83. Mullen KD, Sanyal AJ, Bass NM, et al. Rifaximin is safe and well tolerated for long-term maintenance of remission from overt hepatic encephalopathy. Clin Gastroenterol Hepatol. 2014;12:1390–7 e2. 84. Sanyal AJ, Hassanein TI, Kayali, et al. Efficacy and Safety of Rifaximin Monotherapy Versus Lactulose Combination Therapy for the Prevention of Overt Hepatic Encephalopathy (HE) Recurrence. Hepatology. 2016;64 (S1): 248. www.nature.com/ajg 85. Runyon BA, Committee APG. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087–107. 86. Goel A, Rahim U, Nguyen LH, et al. Systematic review with meta-analysis: rifaximin for the prophylaxis of spontaneous bacterial peritonitis. Aliment Pharmacol Ther. 2017;46:1029–36. 87. Nabi E, Thacker LR, Wade JB, et al. Diagnosis of covert hepatic encephalopathy without specialized tests. Clin Gastroenterol Hepatol. 2014;12:1384–9 e2. 88. Luo M, Li L, Lu CZ, et al. Clinical efficacy and safety of lactulose for minimal hepatic encephalopathy: a meta-analysis. Eur J Gastroenterol Hepatol. 2011;23:1250–7. 89. Campagna F, Montagnese S, Ridola L, et al. The animal naming test: An easy tool for the assessment of hepatic encephalopathy. Hepatology. 2017;66:198–208. https://doi.org/10.1002/hep.29146. Epub 2017 May 27. 90. Allampati S, Duarte-Rojo A, Thacker LR, et al. Diagnosis of Minimal Hepatic Encephalopathy Using Stroop EncephalApp: A Multicenter US-Based, Norm-Based Study. Am J Gastroenterol. 2016;111:78–86. https://doi.org/10.1038/ajg.2015.377. Epub 2015 Dec 8. 91. Rathi S, Fagan A, Wade JB, et al. Bajaj JS Patient Acceptance of Lactulose Varies Between Indian and American Cohorts: Implications for Comparing and Designing Global Hepatic Encephalopathy Trials J Clin Exp Hepatol. 2018;8:109–15. https://doi.org/10.1016/j.jceh.2017.11.010. Epub 2017 Dec 2. 92. Hayashi F, Matsumoto Y, Momoki C, et al. Physical inactivity and insufficient dietary intake are associated with the frequency of sarcopenia in patients with compensated viral liver cirrhosis. Hepatol Res. 2013;43:1264–75. 93. Macias-Rodriguez RU, Ilarraza-Lomeli H, Ruiz-Margain A, et al. Changes in hepatic venous pressure gradient induced by physical exercise in cirrhosis: results of a pilot randomized open clinical trial. Clin Transl Gastroenterol. 2016;7:e180. 94. Ahluwalia V, Wade JB, White MB, et al. Liver transplantation significantly improves global functioning and cerebral processing. Liver Transpl. 2016;22:1379–90. 95. Garcia-Martinez R, Rovira A, Alonso J, et al. Hepatic encephalopathy is associated with posttransplant cognitive function and brain volume. Liver Transpl. 2011;17:38–46. 96. Ahluwalia V, Wade JB, White MB, et al. Brain integrity changes underlying cognitive and functional recovery postliver transplant continue to evolve over 1 year. Transplantation. 2017;102:461–70. 97. Acharya C, Wade JB, Fagan A, et al. Overt hepatic encephalopathy impairs learning on the EncephalApp stroop which is reversible after liver transplantation. Liver Transpl. 2017;23:1396–403. 98. Lucidi C, Ginanni Corradini S, Abraldes JG, et al. Hepatic encephalopathy expands the predictivity of model for end-stage liver disease in liver transplant setting: Evidence by means of 2 independent cohorts. Liver Transpl. 2016;22:1333–42. © 2018 the american college of gastroenterology 99. Nardelli S, Lattanzi B, Torrisi S, et al. Sarcopenia is risk factor for development of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt placement. Clin Gastroenterol Hepatol. 2017;15:934–6. 100. Nardelli S, Gioia S, Pasquale C, et al. Cognitive impairment predicts the occurrence of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 2016;111:523–8. 101. Merola J, Chaudhary N, Qian M, et al. Hyponatremia: a risk factor for early overt encephalopathy after transjugular intrahepatic portosystemic shunt creation. J Clin Med. 2014;3:359–72. 102. Riggio O, Masini A, Efrati C, et al. Pharmacological prophylaxis of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt: a randomized controlled study. J Hepatol. 2005;42:674–9. 103. Haskal ZJ, Middlebrook MR. Creation of a stenotic stent to reduce flow through a transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1994;5:827–9. discussion829-30 104. Kerlan RK Jr., LaBerge JM, Baker EL, et al. Successful reversal of hepatic encephalopathy with intentional occlusion of transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 1995;6:917–21. 105. Chung HH, Razavi MK, Sze DY, et al. Portosystemic pressure gradient during transjugular intrahepatic portosystemic shunt with Viatorr stent graft: what is the critical low threshold to avoid medically uncontrolled low pressure gradient related complications? J Gastroenterol Hepatol. 2008;23:95–101. 106. Riggio O, Efrati C, Catalano C, et al. High prevalence of spontaneous portal-systemic shunts in persistent hepatic encephalopathy: a case-control study. Hepatology. 2005;42:1158–65. 107. Laleman W, Simon-Talero M, Maleux G, et al. Embolization of large spontaneous portosystemic shunts for refractory hepatic encephalopathy: a multicenter survey on safety and efficacy. Hepatology. 2013;57:2448–57. 108. Marsala A, Lee EW. Coil-assisted retrograde transvenous obliteration: a valid treatment for gastric variceal hemorrhage and hepatic encephalopathy. Dig Dis Interv. 2017;01:302–5. 109. Kircheis G, Knoche A, Hilger N, et al. Hepatic encephalopathy and fitness to drive. Gastroenterology. 2009;137:1706–15. e1-9 110. Cohen SM, Kim A, Metropulos M, et al. Legal ramifications for physicians of patients who drive with hepatic encephalopathy. Clin Gastroenterol Hepatol. 2011;9:156–60. quize17 111. Kao D, Roach B, Park H, et al. Fecal microbiota transplantation in the management of hepatic encephalopathy. Hepatology. 2016;63:339–40. 112. Bajaj JS, Kassam Z, Fagan A, et al. Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: a randomized clinical trial. Hepatology. 2017;66:1727–38. 113. Les I, Doval E, Garcia-Martinez R, et al. Effects of branched-chain amino acids supplementation in patients with cirrhosis and a previous episode of hepatic encephalopathy: a randomized study. Am J Gastroenterol. 2011;106:1081–8. The American Journal of Gastroenterology 13 Review Article current Management of Hepatic encephalopathy GASTROENTEROLOGY ARTICLE OF THE WEEK September 6, 2018 Acharya C, Bajaj JS. Current management of hepatic encephalopathy. Am J Gastroenterol https://doi.org/10.1038/s41395‐018‐0179‐4 1. Lactulose for HE a. main mechanism of action is trapping ammonium in the gut b. lowering the colon lumen pH allows for the beneficial growth of bacteria such as lactobacillus c. Is the drug of choice for initiation of therapy for HE d. Is not effective in the treatment of minimal or covert hepatic encephalopathy 2. Main sites responsible for ammonia detoxification and excretion include a. skeletal muscle b. liver c. Kidneys d. intestinal epithelium True or False 3. Rifaximin is similar to lactulose and superior to placebo in the treatment of covert hepatic encephalopathy 4. Patients with recurrent HE should not consume more than 1.0g protein/kg/day 5. Sodium benzoate therapy has been found to be equally effective to lactulose for the treatment of acute HE 6. Rifaximin + lactulose has been found to be superior to lactulose alone in reversing OHE, and decreasing length of hospitalization 7. Metronidazole is recommended for OHE patients who cannot afford rifaximin 8. Patients admitted with OHE should undergo a comprehensive evaluation to exclude or diagnose infections 9. Sarcopenia (loss of skeletal muscle) is a risk factor for hepatic encephalopathy 10. Rifaximin is currently approved by the FDA as first line therapy for hepatic encephalopathy 11. Patients with cover hepatic encephalopathy should be reported to the department of motor vehicles and should not drive 12. Probiotics have not been studied in acute OHE, but may reduce or delay overt encephalopathy recurrence 13. Zinc sulfate theoretically could help encephalopathy by increasing urea cycle clearance of ammonia, data regarding its efficacy is lacking 14. Lactulose plus rifaximin has been found to be superior to rifaximin alone for the prevention of recurrent OHE 15. Based on open label studies, lactulose and probiotics prevent or delay onset of OHE in patients with CHE; there is no data regarding rifaximin efficacy 16. Patients undergoing TIPS for refractory ascites should receive HE prophylactic therapy with lactulose and/or rifaximin