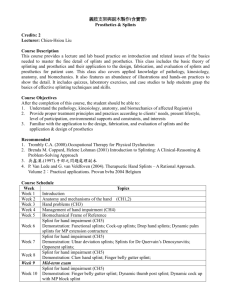
Orthosis and Splinting: OT Guide
advertisement

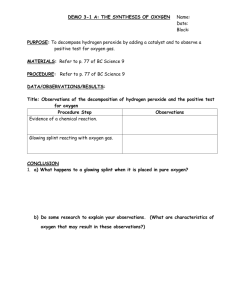
Orthosis and Splinting Radomski ch 16 and 17 OT 624 FOR for splinting and orthosis Biomechanical Uses principles of kinetics and forces acting on the body Sensory motor FOR- Used to inhibit or facilitate normal motor responses Rehabilitation Facilitates maximal function Defining terms Orthosis Any medical device applied to or around a body segment to address physical impairment or disability Brace and support are terms used for an orthosis a force system designed to control, correct, or compensate for a bone deformity, deforming forces, or forces absent from the body Refers to a permanent device to replace or substitute for loss of muscle function Wrist hinge orthosis Splint Device for immobilization, restraint, or support of any part of the body. Usually thought of as more temporary than and orthosis ASHT splint classification Static splint Serial Static splinting Static Progressive splints Dynamic Splints Health professionals who deal with splinting and orthotics OT’s/ COTA’s CHT’s (can be PT or OT) CO/ CPO Dentists Less common- nurses Orthotic selection What is the clinical or fxl problem? What are the indications for and goals of splint use? How will orthosis affect the problem and the client’s function? Benefits of splint/ orthosis? Limitations? Custom made vs. pre-fab vs. No device Splint related factors to consider: Type Design Purpose Fit Comfort Cosmetic appearance Weight Cost to purchase vs. fabricate Ease of care Durability Ease of donning and doffing Effect on unsplinted joints Effect on function Patient related factors Clinical status Functional status Attitude Lifestyle Preference Occupational roles Living envio Working envio Social support Issues related to safety and precautions Ability to understand and follow through Insurance and financial issues Purpose of orthosis Support a painful joint- slings, troughs, laptray and splints Immobilize for healing –dorsal block, buddy strap, figure 8, sh immobilizer Protect tissues, gun slinger, airplane spl, Provide stability and Restrict unwanted motion- resting pan splint, dorsal block Restore mobility-drop out cast,flexion glove, dynamic ext splint Substitute for weak or absent muscles- MAS, Deltoid aide, flexion assist spring, tenodesis splint, WDWHO, ratchet brace Prevent contractures or Modify tone- air splint, ball splint, neoprene thumb loop, wt. Bearing splint, Safety precautions for orthosis Impaired skin integrity Pain Swelling Stiffness Sensory disturbances Increased stress on unsplinted joints Functional limitations Purpose of splints Static Rest Prevention of further deformity Prevention of soft tissue contracture Substitution for lost motor function Dynamic Substitution for lost motor function Correction of a deformity Control of motion Aid in alignment and wound healing Types of Splints Static splint Drop-out Articulated splints Self adjusting or elastic components Static progressive Hinges, Serial velcro, turnbuckles static or casting Purpose of splints Static Rest Prevention of further deformity Prevention of soft tissue contracture Substitution for lost motor function Dynamic Substitution for lost motor function Correction of a deformity Control of motion Aid in alignment and wound healing Types of Splints Static splint Drop-out Articulated splints Self adjusting or elastic components Static progressive Hinges, Serial velcro, turnbuckles static or casting Other considerations for splinting Compliance Offer options Educate about benefits Provide easy application and removal Lightweight material Immobilize only joints being treated Cosmetically pleasing Collaborate w/pt. On wearing schedule Education Anatomical considerations Landmarks Distal IP creases DPC Proximal palmar crease Thenar crease Wrist crease Styloids, MP joints, IP joints, CMC, IP of Th Anatomy (continued) Arches of the hand Longitudinal Distal transverse Proximal transverse Fingers flex toward scaphoid Functional position of hand Position of safe immobilization- intrinsic plus position Influence of splinting on tissue Inflammatory phase- use splint to immobilize and protect Fibroplastic phase: use splints to mobilize healing tissues while protecting Maturation phase: low load force may be applied gradually increasing the stress tolerated Tissue Remodeling Ideal tissue remodeling occurs with gentle elongation of tissues (dynamic and serial splinting/casting) Total end range time suggests that the amount of increase in PROM of a stiff jt is proportional to the time joint is held at end range (serial static splinting/casting) Stress relaxation or static progressive stretch therapy Mechanical principles applied to splint design Increase the area of force application to disperse pressure Increase the mechanical advantage to reduce pressure and increase comfort Ensure three points of pressure Add strength through contouring Perpendicular traction for dynamic splinting Acceptable pressure for dynamic splinting High vs. low profile outriggers Other considerations for splinting Compliance Offer options Educate about benefits Provide easy application and removal Lightweight material Immobilize only joints being treated Cosmetically pleasing Collaborate w/pt. On wearing schedule Education Construction of Hand Splints Purposes: Protection Positioning for function Immobilization for healing Restriction of undesired motion Correction or prevention of deformity Substitution of absent or weak muscles Construction of a hand splint Design splint Select material Make pattern Cut splinting material Heat splinting material Form splint Finish edges Apply straps, padding and attachments Evaluate the splint for fit and comfort Materials and their properties Low temperature thermoplastic High temperature thermoplastics Metal braces and parts Soft splints Properties of materials Memory Drapability Elasticity Bonding Self-finishing edges Time to heat Performance characteristics of materials for splinting Conformability Flexibility Durability Rigidity Perforations Finish, colors, and thickness Pattern Making Tracing the hand Marking landmarks Cutting pattern Fitting pattern on client Forearm splint should go 2/3rds up forearm and trough should be ½ around the forearm. Should not restrict DPC if splint goes into hand, but doesn’t restrict fingers Adjusting pattern Refitting Tracing pattern onto material Cutting and molding a splint Cutting material Soften material Mold material on client Padding if needed prior to molding or after Adjusting Reheating vs. spot heating Strapping No tourniquet effect Wider distributes pressure better Dynamic Splinting Learning Objectives: After this session, the learner will: Explain the purposes of dynamic hand splinting Be able to identify the line of pull for muscles and joints in the UE List common pressure areas with dynamic splints Fabricate a dynamic flexion or extension splint Purposes of Dynamic Splinting: Definition- The application of a moving part of a force which remains approximately constant as the part moves. Purpose: To give MOBILITY to a joint, muscle, tendon, etc... (as opposed to static splinting, which is designed to give STABILITY). Joint MOBILITY can: Decrease adhesions maintain joint function promote tendon gliding Uses of Dynamic Splints: Skeletal Substitution Muscle Balance paralyzed muscles divided tendons or muscles (as in tendon transfers) Joint Motion aides in alignment supports bones and joints preserve or increase joint motion Rest: promote wound healing treat infection relieve pain Parts of Dynamic Splints Static Base Serves as the foundation for the splint, it: provides alignment provides the foundation for the outrigger provides the foundation for a hinge aides in relaxation of a spastic muscle allows tissues to adapt to new position protects a newly repaired structure provides proximal support aides in positioning and edema control Dynamic Component Can be slings, ratchet, springs, elastic bands, hinge These features give the splint its MOBILITY Benefits of Dynamic Splinting: Constant or longer duration of steady tension is more successful than vigorous passive exercise for 20 minutes (especially where contractures are present) Early motion=more effective healing increased circulation decreased edema due to increased pumping of stagnant fluids increased gliding of tendons increased flushing of synovial fluids decreased adhesions Can be used to introduce exercise more gradually and insure that the patient is doing exercise in good alignment Using Exercise in conjunction with Dynamic Splinting: Aides in : Joint excursion tone of skin increased circulation Increased patient confidence by seeing to what degree the hand can be moved safely Because part is supported proximally, patient can do exercise more independently and more safely Therapist should instruct patient not to go the the point of pain Where there is decreased sensation, one must be extremely careful to avoid pressure or push too rapidly Heat prior to exercise may promote increased movement Medical/ Biomechanical Principles: Moving muscles must be given an opposing, balance force in order to maintain joint mobility and tendon gliding Movement prevents joint/muscle atrophy and limits deformity Joints should never be immobilized needlessly Where the injury is on the flexor surface, wrist and fingers should be placed in flexion. Where the injury in on the extensor surface, wrist and fingers should be placed in neutral or resting position. Position of function should be maintained prior to application of any dynamic splint Edema should be decreased ASAP Strapping or construction of a splint should not constrict venous return Edema Has a high protein content which congeals around the hand structures, joint capsules, collateral ligaments, and other fibrous structures When these structures are surrounded by edematous fluid, the tissues swell, thicken, and shorten and become and unyielding fibrous tissue The best program for edema is motion and elevation Swollen fingers tend to go into hyperextension and the thumb into adduction Edema is more common in the dorsum of the hand where the skin allows more fluid to accumulate In the palmar surface of the hand, edema causes the arches to become flattened and hence clients have difficulty making a fist Splint strapping, when applied too tight, can worsen edema due to decreased blood flow Edema can also be aided by removal of a splint every two hours and allowing range to the unaffected joints Patient Education: Patients should be educated in: purpose of the splint accurate positioning of the splint what motion or range is being sought simple anatomy and mechanism of injury / surgical repair specific wearing instructions that include: wearing times placement of splint and strapping common pressure areas exercises allowed while in (or out of ) splint (if allowed) Hand Architecture Directional Pull of the fingers: All the fingers , excepting the middle finger (which may flex straight down) cross the palm obliquely from 10-30 degrees Anatomical center of the Hand: is located at the level of the head of the third metacarpal To find this point, converge all five fingers at one point with the fingers forming a cone Metacarpophalangeal joints Metacarpophalangeal joints are the most common site of joint limitations in the hand. Contributing factors might include: adhesions of the extensor tendons over the dorsum of the hand or of the extensor hood mechanism thickening of the dorsal capsule of the MP joint contracture of the collateral ligaments insufficient skin coverage over the dorsum of the hand a bony block within the joint Bones Radius Ulna Carpals Distal Row Proximal Row Thumb Metacarpals Interphalangeal joints The Mechanics of Splinting Principles Addition of forces Transmissibility of a force A force acting on a rigid body may be considered to have a point of application anywhere along its line of action Equilibrium two or more forces acting upon an object may be added and be replaced by a single force which is their sum If the forces and the torque applied to a body add up to zero the body will remain at rest Action and Reaction The interaction between two bodies in contact may be represented by two forces equal in magnitude and opposite in direction having the same line of action Friction the horizontal component of the force applied along the cuff of a dynamic splint when it pulls along the surface of the skin is called friction Friction is an unreliable force and splints should not be designed to depend upon friction for maintenance of a position. As patients move, slippage of cuffs and splints is bound to occur Therapists should attempt to reduce friction effects as much as possible One should assume that skin is essentially frictionless and it should not be depended on during splint design Tension and Compression Rubber bands, velcro strapping can have traction effects, the weight of the tension needs to match the weight of the extremity being placed in tension. For example, If a rubber band is too tight or too loose, it will not match the weight of the extremity and hence not have the desired effect Compression forces are those that squeezed together - A splint with a hinge on it might have this effect if it acts to hold two parts together, but still allows motion Balancing forces Equilibrium of a splint- all forces should balance out within a dynamic splint if the splint is not to cause problems (such as friction, shearing, pressure areas) Equilibrium of axial forces- Horizontal forces in a splint must = zero. If a hand presses against a splint and thus cancels out the horizontal force of a rubber band, the horizontal forces can be at equilibrium Wedging- changes the forces from small to large by changing the distribution of the force over a larger space. This increases the chance of pressure areas if the wedge is not widely Common pressure points MP joints IP joints Ulnar styloid Center of the palm Any surface on which a finger cuff or traction bar exerts a force Web space Dorsal-lateral aspect of the thumb Documentation about splinting Document why client needs splint Position that client was splinted in Instructions you gave client Follow up needed Splinting Lab