biomarkers
advertisement
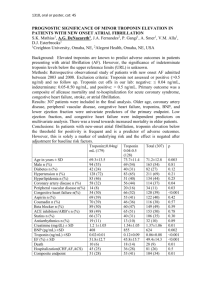
TROPONIN The preferred biomarker to detect myocardial injury. Troponin is a complex of three regulatory proteins (Troponin C, Troponin I and Troponin T) that is associated with muscle contraction in skeletal and cardiac muscle. Cardiac troponin is slightly different from skeletal troponin structurally hence serve as a potent and specific marker for cardiac disease. Individual subunits serve different functions: Troponin C binds to calcium ions Troponin T binds to tropomyosin, interlocking them to form a troponin-tropomyosin complex Troponin I binds to actin and inhibits actin myosin interaction. C-TNT It is extremely useful in patients who do not seek attention in the 2 to 3 days window with angina. Rise : can be detected approx 3 - 6 hrs of chest pain Peak : 2 days Returns normal : 10-14 days cTnT may show a biphasic release in some patients with a first peak occurring during first 24 hr of onset of symptom and second peak on appx. 4th day after admission. HIGH SENSITIVITY CARDIAC TROPONIN High-sensitivity assays deliver enhanced analytic performance, thus enabling more precise measurement of very low concentrations of cardiac-specific troponin . Experts recommend that the term high-sensitivity troponin (hsTn) be reserved for assays that can detect cardiac troponin in more than 50% of an apparently healthy population. In addition, high-sensitivity assays likely detect troponin release much earlier than older generation assays. hsTn assays facilitate the adoption of criteria for rapidly changing concentration of troponin over periods as short as 1 to 3 hours that aid in discriminating acute myocardial injury from chronically elevated values caused by underlying structural heart disease (e.g., left ventricular hypertrophy). Use of such “delta” criteria can improve the clinical specificity of diagnostic testing with cardiac troponin as well as permit rapid exclusion of MI in patients without changing values of hsTn - C TNI It is cardiac specific because it has additional amino acid residue on its N-terminal that are nonexistent in skeletal muscle. Rise : approx 3 - 6 hrs after onset of pain Peaks : 12-18 hrs Returns normal : 7 - 10 days Its measurement is advantageous over CK-MB as it is not found in detectable amount in serum of patients with multiple injuries, renal disease and in those with acute and chronic skeletal muscle disorders. . However, although troponin elevation in the presence of ischemic discomfort often signifies myocardial necrosis, there are numerous other mechanisms of troponin release, including apoptosis, cellular release of proteolytic degradation products of troponin, increased cellular wall permeability, and normal myocyte turnover. Furthermore, a wide variety of clinical conditions can be associated with troponin elevation that are not MI . Even with less sensitive troponin assays, 60% to 70% of persons with chest discomfort seen in the emergency department (ED) will have detectable cTn, but only a minority are diagnosed with acute MI. As high-sensitivity troponin (hsTn) assays that can detect ultralow concentrations of troponin in approximately 90% of healthy individuals become increasingly available, consideration of the clinical context of a troponin elevation will become even more important in avoiding misdiagnosis and improper triage in management of patients. Fourth-generation cTn assays used in the United States are less sensitive than hsTn assays available in european an few other countries. Thus, two negative cTn assays at least 6 hours apart are needed to exclude MI with these less sensitive assays. However, with newer hsTn assays (approved in the UnitedStates in 2017), it is possible with a single measurement at presentation of less than 5 ng/L to classify almost two thirds of patients presenting to the ED with suspected ACS as “very low risk” for MI or cardiac death in the next 30 days (negative predictive value [NPV], 99.6%). Absolute changes in hsTn greater than 9.2 ng/L are even more predictive of acute MI than a single measure or relative changes between two measurements. Use of absolute changes in hsTn allow for rapid protocols as brief as 1 hour to rule in or rule out MI in up to 77% of unselected patients presenting to the ED with acute chest pain, with results comparable to a 3-hour approach. In addition to their utility in early diagnosis and prognostication, cTn levels following ACS aid intermediate-term risk stratification over the subsequent 6 months