50 Lesions - For The Beginner
advertisement

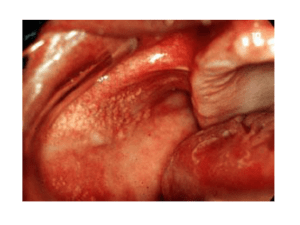
Fordyce Granules • A common condition in which small yellow dots are observed in the oral mucous membrane; these represent misplaced sebaceous glands; once properly diagnosed, no treatment is necessary Fissured Tongue • A condition of probable developmental etiology in which cracks are observed in the tongue dorsum; food debris and Candida albicans colonies may form in the fissures; once properly diagnosed, no treatment is necessary. Varix • A fairly-common condition of older people in which distended blood vessels are observed on the lingual tongue surface; once properly diagnosed, no treatment is necessary. Torus Palatinus • A hamartomatous overgrowth of bone from the midline of the maxilla. Torus Mandibularis • A hamartomatous overgrowth of bone bilaterally from the lingual surface of the mandible. Exostosis • Overgrowth of bone (like tori) from a site other than the maxillary midline or bilateral lingual mandible; commonly occur in the buccal maxilla adjacent to the bicuspid teeth. Nasopalatine duct cyst • A common true jaw cyst appearing as a radiolucency in the maxilla midline just lingual to the central incisor teeth (in the incisive canal); surgical removal will cure this cyst. Oral Lymphoepithelial Cyst • Uncommon lesion that develops in lymphoid tissue in the oral pharynx including the palatine tonsils, lingual tonsils, and pharyngeal adenoids. They may also arise within accessory lymphoid tissue on the floor of the mouth, ventral surface of the tongue, and soft palate. These small (rarely exceed 1cm) submucosal cysts have a yellow or white appearance and feel firm on palpation. They contain creamy or cheesy keratinous material and are usually asymptomatic except when they are traumatized of become infected. They may occur at any age but are most prevalent in young adults. Cysts rarely recur after surgical excision. Amelogenesis Imperfecta • The designation "amelogenesis imperfecta" refers to inherited defects in enamel formation. Several forms are recognized based on their pathogenesis and severity. • Clinically, affected enamel may be thinner than normal (generalized hypoplastic form), may be of normal thickness but lacks strength (hypocalcified form), or may be pitted (hypoplastic pitted form). Periapical Cyst • This cyst is a direct sequela of inflammation of the pulp which has extended into the adjacent periapical tissues. • Treatment consists of endodontic therapy or extraction of the associated tooth with curettage of the cyst. Acute Necrotizing Ulcerative Gingivitis • Poor oral hygiene combined with serious life stress and possibly nutritional deficiencies. Aka: trench mouth. It can be painful, and it is characterized by areas where the gum tissue has become so inflamed that it has become necrotic. These areas will be small ulcers, and will be grayish in color, and will tend to slough off. The tissue will be generally swollen, and where it isn't dead, it will bleed very easily. Wipes Off Pseudomembranous Candidiasis • A common fungal infestation of the oral cavity in the immunocompromised or antibiotictreated patient. Appears as milky white areas on the oral mucosa; lesions wipe-off leaving red (erythematous) base. Responds well to antifungal agents. Angular Cheilitis • Erythema, fissuring, and scaling at the angles of the mouth. • Often in an older person with reduced vertical dimension of occlusion • Caused by C. albicans, S. aureus (in kids – Rx: OTC triple antibiotic ointment), often both. Primary Herpetic Stomatitis • Effected mucosa develops numerous pinhead vesicles which collapse to form small, red lesions which enlarge and develop central areas of ulceration covered in yellow fibrin. • Adjacent ulcerations may coalesce to form larger, shallow, irregular-shaped ulcerations. • Distinctive punched-out erosions along the midfacial free gingival margins Recurrent Herpes Labialis • “cold sore” or “fever blister” • Most common site for recurrence – vermillion boarder and adjacent skin of the lips • Small, erythematous papules; clusters of fluid filled vesicles – rupture and crust within 2 days. Recurrent Intraoral Herpes Simplex • Multiple coalescing ulcerations on FIXED MUCOSA Herpes Zoster • Recurrent infection, often after several decades • Virus was latent in the dorsal spinal ganglia • Recurrent intraoral: – Unilateral, severe pain – Looks like recurrent herpes simplex Linea Alba • Normal variation in the buccal mucosa that appears as a white line beginning at the corners of the oral cavity and extending posteriorly at the level of the occlusal plane. It is composed of keratinized oral mucosa. Cheek Chewing • Hyperkeratosis caused by habitual chewing on the cheek Amalgam Tattoo • A bluish-black or gray macular lesion of the oral mucous membrane caused by accidental implantation of silver amalgam into the tissue during tooth restoration or extraction. Antral Pseudocyst • The antral pseudocyst is a common and welldocumented finding on a panoramic radiograph. Most are discovered during routine radiographic examination and have little clinical significance. The antral pseudocyst should not be confused with the mucocele of the sinus. The antral pseudocyst is believed to be caused by an inflammatory exudate that accumulates under the maxillary sinus mucosa and results in a sessile elevation. Aphthous Lesion • A very common self-limiting, episodic disease of unknown origin manifesting as one or several painful ulcers on the lining mucosa; the ulcers heal in 7-10 days with or without treatment. Major Aphthous Stomatitis • Major aphthae are more serious ulcerative disease of unknown etiology manifesting as large, deep, painful ulcers that leave scars; they recur more often and persist longer than minor aphthae; treatment consists of promoting healing and alleviating pain. Cinnamon Stomatitis • Contact stomatitis from artificial cinnamon flavoring (concentrations of the artificial flavoring are up to 100 times that in the natural spice). Most common in chewing gum, candy, toothpaste. Dentifrice Stomatitis • Superficial epithelial sloughing, no pain or bleeding, a reaction to detergent in toothpaste Squamous Papilloma • A common benign neoplasm arising from mucosal epithelium appearing as a raised, soft, pink lesion with a papillary surface texture; some are caused by viruses (HPV); surgical excision will cure squamous papillomas Seborrheic Keratosis • Extremely common skin lesion of older people and represents an acquired, benign proliferation of epidermal basal cells. There is a positive correlation with chronic sun exposure. Does NOT occur in the mouth. Does NOT wipe off. Idiopathic Leukoplakia • “a clinical white lesion that does NOT rub off and cannot be determined to be a specific disease.” Oral Melanotic Macule • Flat, brown mucosal discoloration produced by an increase in melanin deposition. The cause is unclear, but is not dependant on sun exposure. A solitary, well demarcated, uniformly colored, asymptomatic, round or oval macule. Vermillion zone of lower lip is the most common site. Can occur at any age. Stafne Defect • Asymptomatic radiolucency below the mandibular canal in the posterior mandible, between the molar teeth and the angle of the mandible. Typically well circumscribed and has a sclerotic border. • Developmental in nature, although not present at birth. Speckled Erythroplakia • Red and white, or reddish with white spots • Almost always carcinoma in situ or squamous cell carcinoma (not good) Smokeless Tobacco Keratosis • Characteristic white plaque produced on the mucosa in direct contact with the snuff or chewing tobacco. Typically thin, gray or graywhite, almost translucent plaque with a border that blends gradually into the surrounding mucosa. The usually stretched mucosa appears fissured or rippled. Actinic Cheilitis • A common condition caused by excessive exposure to sunlight manifesting as a crusting lesion of the lower lip; it may show evidence of dysplasia and superficial invasion; however, simple excision of actinic cheilosis usually cures this condition. Squamous Cell Carcinoma • A common epithelial malignancy of the oral mucosa appearing as a red, white, or ulcerated "sore" Basal Cell Carcinoma • A common malignancy of skin, usually of the upper face, that invades locally but rarely metastasizes. • “Classic" appearance of basal cell carcinoma is a central depression and a rolled peripheral border. Most basal cell carcinomas are located above an imaginary line drawn between the lower and upper lips. Mucocele • “Easy diagnosis”: lesion in area of minor salivary glands, goes up and down in size • Duct of salivary gland is severed, mucus leaks out into the tissue • Fast inflammatory reaction, macrophages come in to clean it up - Replacement by granulation tissue = fibroma Melanoma • A very serious malignancy of melaninproducing cells in the skin and occasionally of the oral mucosa; tends to invade and metastasize early Ranula • Large mucocele on floor of mouth (major salivary gland, usually caused by blockage) Minor Salivary Gland Tumor • Bump in the upper lip is NOT a mucocele – it is probably a minor salivary gland tumor • 50% are malignant! Fibroma • Most common tumor of oral cavity • Reactive hyperplasia of fibrous connective tissue in response to local irritation or trauma • Most common location = buccal mucosa along bite line (also: labial mucosa, tongue, gingival) • Smooth surfaced pink nodule, most sessile, asymptomatic, most <1.5cm • Rx: conservative surgical excision Four P’s • Pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, peripheral fibroma Hemangioma • A common benign neoplasm arising from blood vessels manifesting as flat or raised redpurple surface discoloration • Most common tumor of infancy (“strawberry hemangioma”) - rapid growth, but most resolve by age 5, almost all by age 9. Langerhans Cell Disease • Growing evidence indicates this is a neoplastic process of Langerhans cells. Intraosseous lesions may result in radiographic appearance of teeth with unsupported bone, often termed “teeth floating in space”. Florid Cemento-osseous Dysplasia • Multiple mixed radiopaque and radiolucent lesions of the mandible and maxilla Simple Bone Cyst • A benign, empty, or fluid containing cavity within bone that is devoid of an epithelial lining. Cause is uncertain, but one theory is a traumahemorrhage route that causes an intraosseous hematoma that may not undergo repair but instead may liquefy, resulting in a cystic defect. • Can be a well-delineated radiolucent lesion with projections between the roots of vital premolar teeth producing a scalloped appearance Periapical Cemento-osseous Dysplasia • It is a self-limiting fibro-osseous process where bone appears to react abnormally to some unknown stimulation. • Typical example is multiple radiolucencies at the apices of lower anterior teeth - It may be mistaken for inflammatory periapical disease. Determining tooth vitality will settle the issue (teeth are vital) Lateral Periodontal Cyst • An odontogenic cyst arising in the alveolar process appearing as a small radiolucency between the roots of the adjacent teeth (usually mandibular permanent bicuspids). • Generally quite small and well demarcated. Usually adjacent to vital teeth. Ameloblastoma • An uncommon benign jaw neoplasm of odontogenic epithelium appearing as an unilocular or multilocular radiolucency; because of its locally-infiltrative growth pattern, this neoplasm may be difficult to eradicate. • Should be suspected when ever a large multilocular radiolucent lesion is discovered. Most common in the posterior mandible. Lichen Planus • A fairly-common non-neoplastic dermatologic condition manifesting as flat, lacy, white, intersecting lines on the oral mucosa. Presumed autoimmune reaction to basal cells of oral mucosa and skin. • Intersecting white lines (Wickham's striae); may be irregular white plaques; may be ulceration and sloughing in erosive form. Bell’s Palsy • Facial nerve paralysis on one side of the face