mavrakanas2016

Serial versus single troponin measurements for the prediction of cardiovascular events and mortality in stable chronic haemodialysis patients
Short title: Serial versus single troponin measurement in haemodialysis
Thomas A. Mavrakanas, MD
1,2
, Allan D. Sniderman, MD
3
, Paul E. Barré, MD
1
, Ahsan
Alam, MD
1
1
Division of Nephrology, McGill University Health Center, Montreal, Canada
2
Division of General Internal Medicine, Geneva University Hospitals, Switzerland
3
Division of Cardiology, McGill University Health Center, Montreal, Canada
Corresponding author:
Ahsan Alam, MD
Division of Nephrology
McGill University Health Center
1001 Boulevard Décarie, Montréal, QC H4A 3J1, Canada
Telephone: (514) 934-1934
Fax: (514) 843-2815
E-mail: ahsan.alam@mcgill.ca
This study examined the variability of pre-dialysis troponin values to predict cardiovascular events in 128 HD patients. Most stable HD patients do not have elevated troponins at baseline. Howevery elevated or fluctuating levels are associated with a worse outcome. Serial troponin measurement has greater sensitivity and higher negative predictive power compared to a single troponin measurement.
This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/nep.12945
This article is protected by copyright. All rights reserved.
Abstract
Aim: This study aims to describe the variability of pre-dialysis troponin values in stable haemodialysis patients and compare the performance of single versus fluctuating or persistently elevated troponins in predicting a composite of mortality and cardiac arrest, myocardial infarction, or stroke.
Methods: 128 stable ambulatory chronic haemodialysis patients were enrolled. Pre-dialysis troponin I was measured for three consecutive months. The patients were followed for one year. A troponin elevation (>0.06 μg/L) was considered high risk, and patients were classified into 3 risk groups: 1) patients who had normal troponin levels on all three measurements; 2) patients with at least one elevated and one normal troponin value; 3) patients with elevated troponin values on all measurements.
Results: 81 patients had all three troponin values in the normal range; 29 had fluctuating values; 18 had all three values elevated. 27 deaths or composite events were observed: 8 in the first risk group, 10 in the second, and 9 in the third. Persistently elevated and fluctuating troponin values were associated with higher mortality and cardiovascular event rate. Serial troponin measurement had a higher sensitivity for the composite outcome than single troponin measurement when either fluctuating or persistently elevated values were considered to confer high risk.
Conclusion: Most haemodialysis patients do not have elevated troponin levels at baseline.
Troponin levels that remain elevated or fluctuate are associated with worse outcomes. A serial troponin measurement strategy is associated with better sensitivity and higher negative predictive value compared with single troponin measurement.
Keywords: haemodialysis, major adverse cardiovascular events, mortality, serial troponin measurement
This article is protected by copyright. All rights reserved.
Introduction
It has been demonstrated that elevated troponin T and I values are associated with higher risk of cardiovascular mortality, all-cause mortality, or major adverse cardiovascular events in haemodialysis (HD) patients.
1-2 Most of the studies evaluating the prognostic significance of high troponins were based on single pre-dialysis troponin measurements. However, troponin levels may fluctuate between sessions with certain patients having consistently elevated troponin levels and others having isolated elevations.
3
Although several studies have considered serial troponin measurement as a tool for risk stratification in asymptomatic HD patients, it has not been established whether this approach offers any prognostic advantage compared with a single mid-week troponin measurement.
4 It is also unclear how many elevated troponin values confer a higher risk for adverse outcomes.
The aim of this study was to describe the variability of pre-dialysis troponin values in clinically stable HD patients and compare the performance of single versus fluctuating or persistently elevated troponin levels in predicting a composite of mortality and cardiovascular outcomes.
Material and Methods
Study design
This was a prospective observational cohort study in HD patients at the dialysis unit of an urban, tertiary care hospital. The Ethics Committee of the McGill University Health Centre approved the study. The study was conducted according to the Helsinki declaration for medical research in humans.
All chronic HD patients aged 18 or more were enrolled in the study in February 2014.
Patients who were hospitalized, had an acute coronary event or were transferred to another
HD centre during the following three months were excluded (9 patients). We measured pre-
HD troponin I levels in 140 patients for three consecutive months (between February and
April 2014). Blood was collected with monthly bloods at the beginning of the HD session of the mid-week dialysis day (Wednesday or Thursday). The troponin I was measured by immunoassay (Beckman Coulter, Inc.) at the hospital’s central laboratory. Troponin I levels were considered to be elevated if they exceeded the 0.06 μg/L cutoff, which was the laboratory’s reference range. The coefficient of variation of the assay is 10% in the general
This article is protected by copyright. All rights reserved.
population.
5 We are not aware of any validated coefficient of variation specifically for dialysis patients.
Detailed data on demographic characteristics (age, sex), medical comorbidities (history of coronary artery disease (CAD) or diabetes mellitus), HD vintage, and routine monthly blood tests (complete blood count, serum electrolytes, pre-HD and post-HD urea, albumin, calcium, phosphate, parathyroid hormone) were collected at baseline (chart review).
Risk groups and outcomes
To assess the prognostic accuracy of troponin measurement in HD patients, we classified patients into 3 risk groups: Group 1: patients who had normal troponin levels on all three measurements; Group 2: patients who had at least one elevated and one normal troponin value; Group 3: patients with elevated troponin values on all three measurements. All the patients were followed for up to 12 months. During the last three months of the follow-up, pre-dialysis troponin values were measured again with the monthly bloods for all patients.
Our primary aim was to describe the variability and the prognostic accuracy of troponin levels. The primary outcome was a composite of all-cause mortality and major adverse cardiovascular events (MACEs). A MACE was defined as cardiac arrest, myocardial infarction, or stroke. The secondary outcome was all cause mortality. The secondary aim was to compare stability of troponin values for all patients between the beginning and the end of the study period.
Statistical analysis.
Results are presented as mean ± standard deviation or median, (interquartile range). To compare the baseline characteristics of the three different study groups, we used the chi square test for trend, the analysis of variance with polynomial linear contrast, and the
Jonckheere-Terpstra test for trend. The log-rank test was used to compare Kaplan-Meier survival curves. Time-dependent Cox proportional hazard analyses (non-adjusted and adjusted) were used to investigate whether mortality or MACE rate were higher in high-risk patients, as classified by troponin values, compared with low-risk patients. Factors with a univariate p-value < 0.1 were included in the multivariate model. To compare troponin values in the same individuals at the beginning and the end of the study period, the Wilcoxon signed ranks test was used. The SPSS software was used for all statistical analyses (version 20.0,
SPSS Inc., USA). The Stata software (version 14.1, StataCorp LP, USA) was used for the graphs.
This article is protected by copyright. All rights reserved.
Results
140 chronic HD patients in our centre fulfilled the inclusion criteria. Twelve patients had missing values and were excluded from the analysis. Of the remaining 128 patients, 81 patients had all three troponin values in the normal range; 29 patients had at least one elevated and one normal troponin value after three consecutive monthly measurements; 18 patients had all three troponin values elevated in the same time period. Table 1 shows the baseline characteristics of the patients in the three study groups. Patients with elevated troponin values had lower albumin levels and a trend toward higher prevalence of coronary artery disease and lower dialysis dose, as measured by urea reduction ratio.
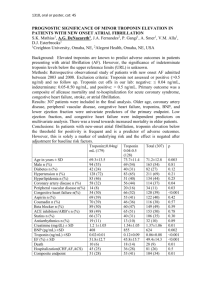
Twenty-seven deaths or composite events were observed at 12 months in our patients: 8 in patients with all three troponins in the normal range (10%), 10 in patients with fluctuating troponins (35%), and 9 in patients with three elevated troponins (50%). Most of the events in each of the three groups were deaths: 5 in the first one, 8 in the second, and 6 in the third group (Figure 1).
In a univariate analysis, age, risk group (based on troponin levels), and albumin levels, but not history of diabetes mellitus or CAD, were associated with MACE or increased mortality risk. In a multivariate model, persistently elevated troponin values as well as fluctuating troponin values were associated with higher mortality and MACE (Table 2). Survival analysis curves for composite events and mortality were significantly different between the three study groups (Figure 2): the log-rank p was < 0.001, and p = 0.001, respectively.
The level of troponin elevation did not have any significant prognostic impact (p= 0.14).
Table 3 shows the sensitivity, specificity, positive and negative predictive value, and accuracy for serial and single troponin measurements. For the single troponin measurement approach, only troponin values of the first month were analysed. Patients found to have elevated troponin levels were considered as high risk. For serial troponin measurement, two different approaches were used. First, patients were considered as high risk either if they had fluctuating or persistently elevated troponin values (any troponin elevation confers high risk).
Second, patients were considered as high risk if they had only persistently elevated troponin values (all troponin values had to be above the cutoff). Sensitivity was the highest with serial troponin measurement, 74% for mortality, when either fluctuating or persistently elevated values were considered to confer high risk. This approach also had a negative predictive value of 94% for mortality. Similar results were obtained for the composite of mortality and
MACEs. Serial troponin measurement with either fluctuating or persistently elevated
This article is protected by copyright. All rights reserved.
troponin values conferring high risk status had the lowest specificity (70% for mortality and
72% for the composite event), although in an acceptable range for a screening biomarker.
Therefore, a serial approach, considering any troponin elevation as high-risk, improves the sensitivity (and negative predictive value) of the assay for hard outcomes (mortality or
MACEs).
During the last three months of the follow-up, pre-dialysis troponin values were measured again with the monthly bloods for the 101 patients who were still alive and still receiving
HD. In the 68 patients of the first group, 60 had all three troponins in the normal range, 7 had fluctuating values, and 1 persistently elevated. In the 21 patients of the second group, 9 had normal values, 9 had fluctuating troponins, and 3 persistently elevated. In the 11 patients of the third group, 2 had all three troponins in the normal range, 3 had fluctuating and 6 persistently elevated troponin values. There was no statistically significant difference between the troponin values before and after the observation period (Wilcoxon signed ranks test -0.90, p=0.37). Although patients can still move from one group to the other over time, this result suggests that troponin measurements tend to be reproducible at 9 months in otherwise stable patients.
Discussion
This cohort study used serial troponin I measurements to stratify patients in different risk groups and followed them for 12 months. We report three major findings. First, most stable chronic HD patients do not have elevated troponin I levels. Only 37% of them had at least one elevated troponin value over three consecutive monthly measurements. Most patients with normal troponin levels in the first three months still had all three values in the normal range after 9 months. Second, troponin levels tend to fluctuate over time, at least in a subset of patients. This fluctuation is associated with a worse prognosis, thus justifying the utility of measuring serial troponins. Third, even an isolated elevated troponin value in this population is not meaningless and is associated with significantly higher mortality rates than those with consistently normal-range troponin levels. Those patients who have persistently elevated troponin levels have poorer outcomes, with a one year mortality exceeding 30%.
Mildly elevated troponin levels are often attributed to chronic kidney disease, especially in
HD patients. The concept of impaired troponin clearance in chronic kidney disease is prevailing among many physicians.
6 However, our results do not confirm this common assumption as most of our patients had all troponin values in the normal range. Few studies
This article is protected by copyright. All rights reserved.
have used serial measurements to assess troponin variability in HD patients. Roberts et al. prospectively followed 57 HD patients with weekly troponin measurements for eight weeks;
37 patients had all values in the normal range.
7 Hill et al. followed 61 stable HD patients with weekly troponin T values for 15 weeks. Twenty-nine patients had all values within the normal range, 15 patients had 1-9 elevated values, and 17 patients had 10-15 elevated values.
8 In another cohort of 81 HD patients, 28 had all five troponin T measurements over
12 months in the normal range.
9 In a cohort study of 59 HD patients, pre-dialysis troponin I was measured at the study onset, and then at 4 weeks, 3 months, 6 months, and 1 year. 88% of the values were above the upper reference limit.
10 Two of these studies used older assays with different cutoff values, 7,10 and the other two used troponin T instead of troponin I.
8,9
Therefore, these results are not directly comparable.
As demonstrated in this cohort, troponin levels do fluctuate, at least in some of the HD patients. Because of this fluctuation, a serial troponin measurement strategy is associated with better sensitivity and a higher negative predictive value compared with single troponin measurement. In the aforementioned study by Roberts et al., five of the twelve patients with elevated troponins on the first week had persistently elevated values over the eight weeks study period and six had fluctuating troponin values. Of the 45 patients with normal troponin values at baseline, 12 had at least one elevated value during the follow-up.
7 In a more recent study, Roberts et al. showed that 20 of 81 patients in a HD cohort had fluctuating troponin values over a 12-months period.
9 On the other hand, Hill et al. concluded that intra-individual troponin variability was minimal over 15 weeks in weekly measurements.
8 In a recent study, including 393 end-stage renal disease patients, high sensitivity troponin T levels were measured upon inclusion and after a one-year period. Changes in troponin T levels from baseline were minimal, even in patients who suffered a myocardial infarction.
11
Troponin has now been established to be a useful biomarker to identify the HD patients with the highest cardiovascular risk, even if the management of these patients has not yet been elucidated.
1 Long-term outcomes have already been evaluated in patients having at least one elevated troponin value over three serial monthly measurements.
12 Although that cohort included only 51 patients and the number of events was small, the MACE rate (but not allcause mortality) was associated with elevated baseline troponin I values. Fernández-Reyes et al. prospectively studied 58 HD patients with serial troponin measurements at 0, 6, and 18 months.
13 This study showed that patients with increasing troponin values over time have a higher propensity to develop de novo CAD. However, most of these patients had already elevated troponin values at baseline and would be qualified as high risk even with a single
This article is protected by copyright. All rights reserved.
measurement approach. Another study in 50 HD patients identified a subgroup of four asymptomatic patients with persistently elevated troponin values (more than 3 out of 6 monthly values). These patients had a history of CAD and were found to have lesions of variable severity in coronary angiography.
3 However, the number of enrolled patients was small and there were no data on hard clinical outcomes. Roberts et al. showed that mortality was higher in patients with fluctuating or persistently elevated troponin values, compared with patients who had all troponin values in the normal range.
9 In this study, patients with normal troponin values did not experience any major adverse cardiovascular events.
The underlying mechanism explaining troponin fluctuation and its association with adverse outcomes is still not clear. In our cohort, patients with fluctuating or persistently elevated troponin levels had a trend towards higher prevalence of underlying CAD. This may put these two groups at an increased risk of MACEs. However, fluctuation at longer intervals (9 months) reflects a dynamic and not a fixed state. How this injury is achieved in those patients remains to be elucidated. Besides underlying coronary disease, dialysis-related parameters, as excessive ultrafiltration or intradialytic hypotension, may also participate in the pathophysiology of myocardial injury.
14 Another potential mechanism underlying myocardial damage in HD is reperfusion injury. HD patients frequently have advanced coronary disease, left ventricular hypertrophy, and are vulnerable to recurrent ischemia. HD-related repetitive hypotensive episodes may be responsible for recurrent reperfusion injury.
15
Our study has several limitations. We used pre-HD troponin I levels as the screening biomarker in our cohort. Post-HD troponins, at a 6 to 9 hour intervals, could be more sensitive than pre-HD values to detect occult myocardial injury (if this is the underlying mechanism) and may improve prognostic accuracy. However, this approach would be limited by feasibility. Troponin T may have been more sensitive than troponin I.
7 We did not use high sensitivity troponin assays and our results might have been different with this test.
Cardiac failure, tachycardia or atrial fibrillation may all result in elevated troponin levels. Unfortunately, we did not have comprehensive clinical or echocardiographic data on the prevalence of these co-morbidities that could alone independently increase the risk of
MACE.
The number of patients enrolled in this observational study is small and the results may not be reproducible to a larger group. There are likely to be other confounders that are unaccounted for and may affect the cardiovascular risk of patients. For example, there may have been differences in medication that may reduce cardiovascular risk, or glycemic control that may account for the difference in risk between the 3 groups.
Eleven per cent of patients died and 11% were transferred to another centre during the 12-months observation period.
This article is protected by copyright. All rights reserved.
Therefore, our results concerning troponin variability at 12 months may be biased towards healthier patients with less significant underlying heart disease and more stable troponin levels.
Based on our results, we suggest three monthly troponin I measurements for all haemodialysis patients. Although evidence is lacking on interventions that might be considered to improve outcomes, high-risk patients could be further investigated with noninvasive cardiac imaging and referred for revascularization if deemed clinically appropriate.
Whether this approach can reduce morbidity or mortality remains to be demonstrated.
Conclusions
In conclusion, most stable HD patients do not have elevated baseline troponin levels and their intra-individual variability is not significant. Troponin values tend to fluctuate over time in a significant proportion of HD patients, justifying thus serial troponin measurement. Even a single elevated troponin value in this subgroup is associated with worse clinical outcomes and should not be overlooked in this high risk population. The role for further cardiac evaluation or optimization of therapy should be the focus of further study in this vulnerable patient population.
Acknowledgment s
Dr. Mavrakanas was supported by a grant from the Swiss National Science Foundation-
Schweizerischer Nationalfonds zur Förderung der Wissenschaftlichen Forschung
(P2GEP3_148806). The funding agency had no role in design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
The authors have no competing interests to disclose.
Previous presentation of the information reported in the manuscript: This work was presented in the form of a poster abstract at the 2015 Kidney Week of the American Society of
Nephrology in San Diego on 11/6/2015.
This article is protected by copyright. All rights reserved.
References
1.
Michos ED, Wilson LM, Yeh HC, et al. Prognostic value of cardiac troponin in patients with chronic kidney disease without suspected acute coronary syndrome: a systematic review and meta-analysis. Ann. Intern. Med.
2014; 161: 491-501.
2.
Alam A, Palumbo A, Mucsi I, Barré PE, Sniderman AD. Elevated troponin I levels but not low-grade chronic inflammation is associated with cardiac-specific mortality in stable HD patients. BMC. Nephrol.
2013; 14: 247.
3.
Katerinis I, Nguyen QV, Magnin JL, Descombes E. Cardiac findings in asymptomatic chronic HD patients with persistently elevated cardiac troponin I levels. Ren. Fail.
2008; 30:
357-62.
4.
Jacobs LH, van de Kerkhof J, Mingels AM, et al. Haemodialysis patients longitudinally assessed by highly sensitive cardiac troponin T and commercial cardiac troponin T and cardiac troponin I assays. Ann. Clin. Biochem.
2009; 46: 283-90.
5.
Beckman Coulter. Access immunoassay systems. AccuTnI. REF 33340. Available at https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwj
V96y7qvbOAhWKGR4KHUZPALMQFggcMAA&url=https%3A%2F%2Fwww.beckmanco
ulter.com%2Fwsrportal%2Fajax%2FdownloadDocument%2FA34077F.pdf%3FautonomyId
%3DTP_DOC_111223%26documentName%3DA34077F.pdf&usg=AFQjCNHaRLdMpaEFl4_sMEybQit8JiD8A&bvm=bv.131783435,d.dmo Accessed September 5, 2016.
6.
Parikh RH, Seliger SL, deFilippi CR. Use and interpretation of high sensitivity cardiac troponins in patients with chronic kidney disease with and without acute myocardial infarction. Clin. Biochem.
2015; 48: 247-53.
7.
Roberts MA, Fernando D, Macmillan N, et al. Single and serial measurements of cardiac troponin I in asymptomatic patients on chronic HD. Clin. Nephrol.
2004; 61: 40-6.
8.
Hill SA, Cleve R, Carlisle E, Young E, McQueen MJ. Intra-individual variability in troponin T concentration in dialysis patients. Clin. Biochem.
2009; 42: 991–5.
9.
Roberts MA, Hare DL, Macmillan N, Ratnaike S, Sikaris K, Ierino FL. Serial increased cardiac troponin T predicts mortality in asymptomatic patients treated with chronic haemodialysis. Ann. Clin. Biochem.
2009; 46: 291-5.
10.
Wayand D, Baum H, Schätzle G, Schärf J, Neumeier D. Cardiac troponin T and I in endstage renal failure. Clin. Chem.
2000; 46: 1345-50.
11.
Hassan HC, Howlin K, Jefferys A, et al. High-sensitivity troponin as a predictor of cardiac events and mortality in the stable dialysis population. Clin. Chem.
2014; 60: 389-98.
This article is protected by copyright. All rights reserved.
12.
Gaiki MR, DeVita MV, Michelis MF, Panagopoulos G, Rosenstock JL. Troponin I as a prognostic marker of cardiac events in asymptomatic HD patients using a sensitive troponin I assay. Int. Urol. Nephrol.
2012; 44: 1841-5.
13.
Fernández-Reyes MJ, Mon C, Heras M, et al. Predictive value of troponin T levels for ischemic heart disease and mortality in patients on HD. J. Nephrol.
2004; 17: 721-7.
14.
Mavrakanas TA, Sniderman AD, Barré PE, Vasilevsky M, Alam A. High ultrafiltration rates increase troponin levels in stable hemodialysis patients. Am J Nephrol.
2016; 43: 173–8.
15.
Sniderman AD, Solhpour A, Alam A, Williams K, Sloand JA. Cardiovascular death in dialysis patients: lessons we can learn from AURORA. Clin. J. Am. Soc. Nephrol.
2010; 5:
335-40.
This article is protected by copyright. All rights reserved.
Figure 1. Major adverse cardiovascular events and deaths in the three patients groups
Group 1: patients who had normal troponin levels on all three measurements; Group 2: patients who had at least one elevated and one normal troponin value; Group 3: patients with elevated troponin values on all three measurements.
This article is protected by copyright. All rights reserved.
Figure 2. A. All-cause mortality stratified by Troponin I Group. B. Major Adverse Cardiovascular
Events (MACEs) and All-cause Mortality Stratified by Troponin I Group
Group 1: patients who had normal troponin levels on all three measurements; Group 2: patients who had at least one elevated and one normal troponin value; Group 3: patients with elevated troponin values on all three measurements.
This article is protected by copyright. All rights reserved.
Table 1. Baseline characteristics of patients in different study groups
Characteristic
N
Group 1
81
0.02 (0.015-
Troponin (μg/L)
Age (years)
Male sex
0.03)
67 ± 16
44 (54%)
Dialysis vintage
31 (10-62)
(months)
Group 2
29
0.05 (0.03-0.07)
70 ± 15
17 (59%)
18 (9-43)
Group 3
18
0.11 (0.09-0.21)
68 ± 13
10 (56%)
47 (18-101) p
<0.001
0.65
0.82
0.59
History of diabetes 33 (41%) 13 (48%) 11 (61%)
0.11
History of CAD 19 (24%)
Hemoglobin (g/l) 105 ± 16
Albumin (g/L) 31 ± 4
Potassium
(mmol/l)
4.6 ± 0.6
Calcium (mmol/l) 2.14 ± 0.16
Phosphorus
(mmol/l)
PTH (pmol/l)
URR (%)
1.30 ± 0.41
35.8 (24.0-49.5)
79 (73-83)
11 (38%)
99 ± 19
28 ± 4
4.7 ± 0.6
2.05 ± 0.14
1.30 ± 0.46
34.2 (16.5-57.7)
77 (73-82)
8 (44%)
111 ± 15
30 ± 5
5.0 ± 0.9
2.13 ± 0.22
1.39 ± 0.30
46.3 (25.0-64.2)
75 (67-78)
0.08
0.70
0.04
0.11
0.26
0.51
0.86
0.06
Group 1: patients who had normal troponin levels on all three measurements; Group 2: patients who had at least one elevated and one normal troponin value; Group 3: patients with elevated troponin values on all three measurements. Results are presented as mean ± standard deviation, median (interquartile range), or number of patients (percentage). N, number of patients; CAD, coronary disease; PTH, parathyroid hormone; URR, urea reduction ratio. P values are for trend.
This article is protected by copyright. All rights reserved.
Table 2. Association of elevated troponin with MACE and mortality using time-dependent
Cox proportional hazard analyses
HR for all-cause mortality (95% CI) HR for mortality & MACEs (95% CI)
Parameter Unadjusted
Adjusted for age and albumin
Unadjusted
Adjusted for age and albumin
Fluctuating troponins (group 2) vs. Group 1
Persistently elevated
4.77 (1.56-14.59) 4.02 (1.28-12.63) 3.83 (1.51-9.71) 3.10 (1.17-8.16)
6.31 (1.92-20.70) 6.76 (1.90- 24.08) 5.95 (2.29-15.44) 6.45 (2.37-17.54) troponins (group 3) vs. Group 1
Fluctuating (group
2) vs. persistently elevated troponins
(group 3)
1.31 (0.45-3.77) 1.62 (0.51-5.12) 1.54 (0.63-3.80) 2.23 (0.83-5.95)
HR, hazard ratio; MACEs, major adverse cardiovascular events; CI, confidence interval;
CAD, coronary artery disease. Group 1: patients who had normal troponin levels on all three measurements; Group 2: patients who had at least one elevated and one normal troponin value; Group 3: patients with elevated troponin values on all three measurements.
This article is protected by copyright. All rights reserved.
Table 3. Comparison of single and serial troponin measurements for the screening of highrisk individuals for adverse clinical outcomes
Sensitivity
All-cause mortality
Single
Serial Serial fluctuating persistent
Mortality & MACEs
Single
Serial fluctuating
Serial persistent
57.9 % 73.7 % 31.6% 51.9 % 70.4 % 33.3%
Specificity 82.4 %
Positive predictive value
Negative predictive value
36.7 %
91.8 %
Accuracy 78.7 %
69.7 %
29.8 %
93.8 %
89.0%
33.3%
88.2%
84.0 %
46.7 %
86.6 %
72.3 %
40.4 %
90.1 %
91.1%
50.0%
83.6%
70.3 % 80.5% 77.2 % 71.9 % 78.9%
The number of samples tested in each group was 243, 85, and 54, respectively. MACEs, major adverse cardiovascular events
This article is protected by copyright. All rights reserved.