TOC for HIT in DVT
advertisement

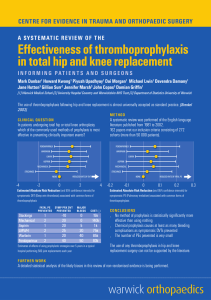
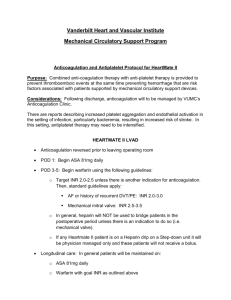
1/23/2019 InpharmD™ What is the drug of choice for DVT prophylaxis in a patient with a con rmed history of heparin induced thrombocytopenia (HIT)? Comment by InpharmD Researcher When selecting an agent for DVT prophylaxis in a patient with a history if heparin induced thrombocytopenia the only recommendation is to select a non-heparin agent. Based on the meta-analysis of non-heparin anticoagulant data, our primary literature focuses on fondaparinux and apixaban as the agents with most e cacy or e cacy and safety data respectively compared to low molecular weight heparin. Depending on individual patient factors (convenience, cost, compliance, renal and hepatic function, etc) and guidelines not recommending one medication over the other, either agent is a reasonable alternative. Search Strategy All Background Relevant Prescribing Information Literature Review Discus Background According to the American College of Chest Physician (ACCP) guidelines, the choice for DVT prophylaxis should include the following characteristics, ease of administration, e ectiveness, safety, and costhttps://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 1/9 1/23/2019 InpharmD™ e ectiveness. ACCP does not recommend a speci c agent but suggests selecting from the following pharmaceutical agents: low dose unfractionated heparin, low molecular weight (LMW) heparins, fondaparinux, and, where available, oral factor Xa or direct thrombin inhibitors. [1] In the case of heparin-induced thrombocytopenia, according to the America Society of Hematology (ASH) guideline panel, it is recommended that patients receive a non-heparin anticoagulant for VTE prophylaxis. One agent is not preferred over the other but ASH suggests choosing from the following, argatroban, bivalirudin, danaparoid, fondaparinux, direct oral anticoagulants. [2] Based on the American College of Chest Physician (ACCP) guidelines alternative anticoagulants for thromboprophylaxis, such as fondaparinux, danaparoid, warfarin, and the new oral anticoagulants, dabigatran and rivaroxaban, should be used. As there is limited studies evaluating fondaparinux and new oral anticoagulants in HIT, further studies would be bene cial. [1] When choosing an agent for DVT prophylaxis in HIT, the guidelines don’t recommend one non-heparin agent over another. We reviewed a meta-analysis comparing e cacy and safety of alternative choices for anticoagulants, in the prevention of venous thromboembolism after hip and knee arthroplasty, comparing all available options. The authors found that fondaparinux, rivaroxaban, and apixaban may be more e ective in the prevention of VTE than enoxaparin so we include the data for these agents below. When apixaban was compared to the standard treatment of enoxaparin 40 mg once daily, it showed 0.51 odds ratio for VTE incidence (95% CI 0.39-0.68). When fondaparinux was compared to enoxaparin 40 mg once daily there was an odds ratio of 0.38 for VTE incidence (95% CI 0.28-0.5) and when rivaroxaban 10 mg once https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 2/9 1/23/2019 InpharmD™ daily was compared to the standard enoxaparin dosing there was an odds ratio of 0.38 for VTE incidence (95% CI 0.29-0.5). While fondaparinux and rivaroxaban were associated with a higher risk of major or clinically relevant non-major (CRNM) bleeding than enoxaparin, apixaban showed a lesser incidence. Apixaban compared to fondaparinux in the same dosing showed an odds ratio of 0.56 for major/CRNM bleeding (95% 0.39-0.82) and for rivaroxaban the odds ratio was 0.65 (95% CI 0.5-0.86). Considering the history of HIT in a patient, heparin agents would be excluded from agent selection and the data shows the non-heparin agent that is superior in both safety and e cacy is apixaban. While rivaroxaban and fondaparinux showed superiority in e cacy, they appear to have a higher incidence of major or CRNM bleeding. [3] References: 1. Linkins LA, Dans AL, Moores LK, et al. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e495S-530S. 2. Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. 3. Hur M, Park SK, Koo CH, et al. Comparative e cacy and safety of anticoagulants for prevention of venous thromboembolism after hip and knee arthroplasty. Acta Orthop. 2017;88(6):634-641. Relevant Prescribing Information https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 3/9 1/23/2019 InpharmD™ Thrombocytopenia can occur with the administration of fondaparinux sodium. Thrombocytopenia of any degree should be monitored closely. Discontinue fondaparinux sodium if the platelet count falls below 100,000/mm3. Moderate thrombocytopenia (platelet counts between 100,000/mm3 and 50,000/mm3) occurred at a rate of 3.0% in patients given fondaparinux sodium 2.5 mg in the peri-operative hip fracture, hip replacement, or knee replacement surgery and abdominal surgery clinical trials. Severe thrombocytopenia (platelet counts less than 50,000/mm3) occurred at a rate of 0.2% in patients given fondaparinux sodium 2.5 mg in these clinical trials. During extended prophylaxis, no cases of moderate or severe thrombocytopenia were reported. Moderate thrombocytopenia occurred at a rate of 0.5% in patients given the fondaparinux sodium treatment regimen in the DVT and PE treatment clinical trials. Severe thrombocytopenia occurred at a rate of 0.04% in patients given the fondaparinux sodium treatment regimen in the DVT and PE treatment clinical trials. Occurrences of thrombocytopenia with thrombosis that manifested similar to heparin-induced thrombocytopenia have been reported with the use of fondaparinux sodium in postmarketing experience. [1] No relevant monitoring recommendations are included in the apixaban prescribing information. References: 1. Fondaparinux sodium [package insert]. Princeton, NJ.:Dr. Reddy’s Laboratories. INC.;2018 https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 4/9 1/23/2019 InpharmD™ Literature Review A search of the published medical literature revealed 3 studies investigating the researchable question: What is the drug of choice for DVT prophylaxis in a patient with a con rmed history of heparin induced thrombocytopenia (HIT)? Please see Tables 1-3 for your response. Table 1 Table 2 Table 3 Postoperative fondaparinux versus preoperative en venous thromboembolism in elective hip-replaceme double-blind comparison. Design Randomized Controlled Double-Blind Objective To evaluate the e cacy and safety of f in prophylaxis of VTE pre-surgically for surgery. https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 5/9 1/23/2019 InpharmD™ Study Groups Patients 18 years of age or older who w replacement surgery or for revision of surgery Exclusion Criteria - One of the followin endocarditis, documented congenital current ulceration or angssiodysplastic or brain, spinal, or ophthalmic surgery planned indwelling intrathecal or epid hours after the end of surgery, hypers porcine products, or iodinated contras anticoagulant treatment, concomitant be combined with contrast media, add creatinine in serum that was greater th patient, and a platelet count of less tha patients who needed anticoagulant th anticoagulant or brinolytic therapy or preceding the rst administration of th before the study was not prohibited. N=2309 patients Patients assessed = 1827 (per protoco Methods Patients were randomized in blocks of to be in once daily sub q injections of e mg/day started 6H after surgery) plus volume of enoxaparin syringe, or enox preoperatively) Treatment lasted 5-9 days post surger primary e cacy outcome assessed be occurred in person, by mail, or by pho Treatment could be extended with any after venography was completed. VTE needed treatment was left to the discr https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 6/9 1/23/2019 InpharmD™ Duration Trial - 1 year (December 1998 - January Assessment - 6 weeks including follow Outcome Measures Primary E cacy Outcome - VTE up to d thrombosis detected by mandatory bi symptomatic deep-vein thrombosis, o pulmonary embolism. Safety Outcomes - Bleeding and death Baseline Characteristics Safety Safety analysis analysis fondaparinux enoxapar Age n= 1140 n= 1133 66 67 Women 647 660 Weight (kg) 75 75 Hx of VTE 45 56 https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 7/9 1/23/2019 InpharmD™ Results Study met power estimated to be 800 VTE occurrence by day 11 fondaparinux 37/908 (4%) Enoxaparin 85/919 (9%) 95% CI -5.2(-8 Bleeding w/ Bleeding index ≥ 2 Fondaparinux 42/908 (4%) Enoxaparin 29/919 (3%) Adverse Events Common Adverse Events: N/A Serious Adverse Events: N/A Percentage that Discontinued due to A Study Author Conclusions Study authors conclude that fondapar e cacious agent than enoxaparin for InpharmD Researcher While this study is dated, it shows that two arms of the study group, and may they also do not conclude that there m bleeding in fondaparinux group (illustr Critique Discussion (0) https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 8/9 1/23/2019 InpharmD™ Our Story (/our_story) | FAQ (//support.inpharmd.com) | Privacy Policy (/privacy_policy) | Terms of Use (/terms_of_use) | Partners (/partners) https://inpharmd.com/what-is-the-drug-of-choice-for-dvt-prophylaxis-in-a-patient-with-a-confirmed-history-of-heparin-induced-thrombocytopenia-hit 9/9