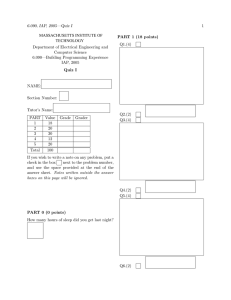
ALP Final draft MSc thesis
advertisement

Master’s Thesis On intestinal alkaline phosphatase and its role in high-fat diet-induced obesity By Annick D. van den Brand Toxicology and Environmental Health #3355411 – Utrecht University Under the supervision of Dr. Nynke I. Kramer Alternative Toxicology department Institute for Risk Assessment Sciences Content Layman’s Summary ................................................................................................................... 3 Abstract ...................................................................................................................................... 4 Introduction ................................................................................................................................ 5 Chapter 1 .................................................................................................................................... 7 Processing of dietary fat...................................................................................................... 7 Uptake FA by enterocytes ................................................................................................... 7 Intracellular transport and chylomicron formation ........................................................... 10 Exocytosis to lymphoid system ........................................................................................ 11 Chapter 2 .................................................................................................................................. 12 Effects of HFD on gut microbiota .................................................................................... 12 Effects of HFD on intestinal permeability ........................................................................ 13 Effects of HFD on pathogenesis development.................................................................. 14 Chapter 3 .................................................................................................................................. 17 Alkaline phosphatase ........................................................................................................ 18 IAP in response to HFD .................................................................................................... 19 Discussion ................................................................................................................................ 22 Conclusion ................................................................................................................................ 25 References ................................................................................................................................ 26 2 Layman’s Summary In this thesis, the adverse effects of a high fat diet on the integrity of the intestinal wall and the role of an enzyme, alkaline phosphatase, in ameliorating these effects is reviewed. Dietary fat is absorbed via the cells lining the small intestines. The gut wall also serves as a border membrane to protect to body from pathogens which reside in the gut. When consuming a high fat diet, the composition of the gut flora can change, resulting in an overgrowth of certain bacteria. These bacteria can produce the toxic lipopolysaccharide (LPS), which can trigger an inflammatory response. Thus, next to an increased fat uptake, a high fat diet can cause a local inflammation. These two factors can affect the gut wall in such a way that it the permeability increases. This ‘leakiness’ of the gut wall causes blood LPS levels to rise, which may result in a systemic inflammation or even a septic shock. High fatty acid levels due to the increased fat uptake may even result in insulin resistance which is linked to other diseases as type 2 diabetes and liver cirrhosis. An enzyme involved in the regulation of the uptake of fat is intestinal alkaline phosphatase (IAP). This enzyme can activate fatty acid transporters, and it is involved in the secretion of fat into the bloodstream. In addition, IAP can dephosphorylate LPS, thereby reducing its toxicity. Because of this dual role of IAP it has an interesting therapeutic potential, regarding the effects of a HFD such as obesity and insulin resistance. As it has been shown that mice lacking IAP activity become obese, administration of IAP may reduce an increased uptake and deposition of dietary fat. 3 Abstract In this review, literature available on the adverse effects of a high fat diet on the integrity of the intestinal border is reviewed. In addition, the role of the enzyme alkaline phosphatase mediating in the process of fat absorption is evaluated. Dietary fat is absorbed via the enterocytes in the proximal part of the small intestine. This process of fat uptake is mediated by an enzyme intestinal alkaline phosphatase (IAP). Next to its regulatory role in fat absorption, IAP has immune-related properties. It is able to dephosphorylate bacterial lipopolysaccharide (LPS), thereby reducing its toxicity. However, after consuming a high fat diet (HFD), the composition of the gut microbiota is altered, favoring the presence of the LPS producing gram negative bacteria. Increased levels of LPS can cause a local inflammation, which can alter the epithelial lining of the gut wall by disturbing, for example, the tight junctions between the enterocytes. The HFD-induced rise in LPS levels, but also increased tension in the enterocytes due to the increased fat absorption can result in an increase in membrane permeability. Subsequently, LPS and pathogens can enter the blood, which may eventually result in endotoxemia. Thus, a HFD can cause a local as well as systemic inflammation, next to just an increased fat uptake. The increased level of fatty acids (FA) itself is also linked to a range of pathologies, as FA can interfere with the insulin signaling cascade. Defects in insulin action may result in insulin resistance, which has also been correlated with type 2 diabetes and liver cirrhosis. As IAP has a regulatory role in both fat uptake and LPS detoxification, it has an interesting therapeutic value. Therapeutic IAP may supplement the depletion of IAP due to an increase in fat absorption and LPS levels, induced by a HFD. This may restore the negative regulation IAP has on fat uptake, and may reduce the inflammatory responses initiated by LPS. 4 Introduction Over 15% of the people within the European Union are obese, with this number ever increasing (OECD & EU 2010). A body mass index (BMI) exceeding 30 kg/m2 reduces life expectancy by six to seven years, while severe obesity (where BMI exceeds 35 kg/m2) can even reduce life expectancy by ten years (Haslam & James 2005; Whitlock et al. 2009). The American Health Association recently classified obesity as a disease, not because it is a direct cause of death, but because there are numerous secondary health risks related to an excess accumulation of body fat. Next to the direct effects and discomforts of increased adiposity, obese patients show an increased likelihood for the development of various other diseases as diabetes type II, several types of cancer and cardiovascular diseases (Frazier et al. 2011; Laugerette et al. 2011). Although there are genetic factors contributing to the accumulation of excess fat, the consumption of a high fat diet (HFD) appears to be a major causative factor of the development of obesity. Studies have been showing the development of obesity in mice being fed to a HFD, whereas no obese mice were observed after being fed a control diet where the total amount of energy consumption remained unchanged (Townsend et al. 2008). This implies that the development of obesity is not solely due to an increased caloric intake, but also due to the type of nutrients consumed (Lynes & Widmaier 2011). The precise molecular mechanisms by which a HFD is linked to the development of obesity are however not yet fully understood. It is known that fatty acids (FA) are absorbed by the small intestines, which are prone to morphological adaptation by external influences as diet (Frazier et al. 2011). Studies have shown that intestinal cells adapt to starvation or a HFD, reflected in the changes in gene expression and growth (Lynes & Widmaier 2011). This plasticity of the gut wall ensures that no available source of energy is to be lost, due to the constant state of change of one’s nutrient supply and energy demand. This underlines the importance of the molecular response of the gut wall to nutrient availability. An enzyme involved in the regulation of cellular uptake of FA is intestinal alkaline phosphatase (IAP). Studies have long been reporting a relationship between a high fat uptake and increased plasma levels of IAP, but the exact role of IAP in response to FA is not entirely elucidated (Inglis et al. 1967; Keiding 1966; Hansen et al. 2007). What is known is that IAP knockout mice have shown increased adiposity, suggesting IAP to be a negative regulator of fat absorption (Narisawa & Huang 2003). 5 Alkaline phosphatases (AP) are commonly present in not only humans, but also in rodents, bacteria and many other species (Millan 2006). As phosphatases, APs are able to remove phosphate groups from various types of molecules. The exact function of AP is still largely unknown, however it is commonly recognized that there is an anti-inflammatory role in the innate immune system, including the immune system of the gut (Lallès 2010; Pike et al. 2013). One of the targets of AP is the lipid A moiety of lipopolysaccharide (LPS). LPS can be found in gram negative bacteria, and holds several phosphate groups to its glucosamine disaccharide (Lallès 2010). LPS or other pathogen associated molecular patterns (PAMP) can trigger an inflammatory response when it stimulates pattern recognition receptors, such as the Toll-like receptor 4 (TLR4) (Moreira et al. 2012). AP mediated removal of only one phosphate group from LPS already results in a 100 fold reduction in toxicity (Bates et al. 2007; Schromm et al. 1998). As a dysregulation of fat absorption may result in obesity, understanding the role of IAP regarding absorption of FA may give insights in the molecular mechanism behind the development of HFD induced obesity. Here, the literature evidence of possible roles of IAP in the uptake of fat across the intestinal barrier is presented. In so doing, the process of FA uptake and the role of IAP are described. Subsequently, the mechanisms by which a HFD may induce obesity as well as other pathologies are evaluated. Lastly, the potential of IAP as a therapeutic target is discussed. 6 Chapter 1 The aim of the first chapter is to get a better understanding of the role of IAP in the absorption of fat in the small intestines. The process fat absorption, starting from the consumption of dietary fat, to the processing of the absorbed FAs, and the subsequent systemic delivery is reviewed in this thesis. Only when one has a mechanistic understanding of the process of FA absorption it is possible to evaluate how a disruption may lead to a pathogenesis. Processing of dietary fat In the consumed dietary products, the saturated or unsaturated FAs are mostly present as triacylglycerides (TAG). The enterocytes present in the small intestine however are not able to absorb these storage and transport forms of energy due to their size, which is why they require hydrolyzation. The large structures of TAGs are broken down in the mouth physically as well as by lingual lipase and by gastric lipase in the stomach (Pan & Hussain 2012), after which the bile fluids in the duodenum solubilize TAG in bile acid micelles. The TAG molecules are subsequently digested by pancreatic triglyceride lipase, carboxyl ester lipase, and pancreatic triglyceride lipase related protein-2 resulting in monoacylglycerols (MAG) and free FA, as reviewed in Pan and Hussain, 2012 (Pan & Hussain 2012). Uptake FA by enterocytes When the free FAs reach in the first part of the small intestine, the duodenum and the proximal part of the jejunum, they can be absorbed by enterocytes. Enterocytes are epithelial cells which, besides serving as a barrier against luminal pathogens, are involved in the absorption of dietary fat and other nutrients (Danielsen & Hansen 2006). The apical surface of the cells consists of microvilli, which serve to increase the surface area of the membrane. The apical membranes of these cells are covered with transporter proteins and enzymes which are involved in the uptake of dietary components (figure 1). The majority of these molecules reside within a lipid raft region of the membrane, a platform enriched with lipids, cholesterol and thus transporters, which function in membrane trafficking (Lingwood & Simons 2010). 7 Figure 1. Highly schematic overview of intestinal lumen and enterocyte. Mature enterocytes reside in the villi, whereas immature enterocytes develop from stem cells reside in the crypts. After absorption of dietary fat via the brush border, the fatty acids are transported transcellularly to be secreted via the basolateral membrane of the enterocyte, into the lymphatic system (Bowen, 2001). Free FA and MAG can either diffuse across the membranes of enterocytes, or passage may be facilitated by transporter proteins (Stahl 2004). Simple diffusion of FAs over the membrane occurs by a passive flip-flop mechanism, by which the FAs are initially bound the outer leaflet of the membrane followed by the subsequent flip of the un-ionized FA to the inner leaflet (Kamp & Hamilton 1992). Diffused free fatty acids are then bound to cytoplasmic fatty acid binding proteins which act as a sink for the entering FA (Glatz et al. 2010). Passive diffusion occurs when the concentrations of FA in the intestinal lumen are high, but when transport needs to occur against the concentration gradient, transporter proteins come into play. This review focusses on the transmembrane transport of free long chain fatty acids (LCFA) into the enterocytes, as little is known on MAG transport. Several transporter proteins that are involved in the transport of LCFA have been identified. FATP4, FABP and CD36 are three of the main transporter proteins present in enterocytes 8 (Stahl 2004; Glatz et al. 2010; Mansbach & Siddiqi 2010). The latter transporter protein is also known as fatty acid translocator (FAT), the rodent homologue of the human CD36, and has been reported to show a high affinity for LCFA (Baillie et al. 1996). CD36 resides in the lipid raft domains of the enterocytes, where the GPI-linked IAP is also located (figure 2) (Danielsen 1995). The activity of CD36 depends on its phosphorylated status, and as IAP is able to remove phosphate groups from a molecule, it has been proposed to be a regulator of CD36 activity (Lynes & Widmaier 2011). Studies have shown that a Thr92 dephosphorylation of CD36 by AP reversed the inhibition of the activity of the transporter protein, suggesting a close interplay between these molecules (Guthmann et al. 2002; Asch et al. 1993). 9 Figure 2. After Lynes and Wildmaier, 2011. Schematic overview of the interaction between intestinal alkaline phosphatase (IAP) and the long chain fatty acid (LCFA) transporter CD36. They both reside in the lipid raft areas on the brush border membrane of enterocytes. LCFA can interact with CD36 and only when the transporter is dephosphorylated by IAP on the Thr92 residue it is active, which will result in the uptake of LCFA. FA binding to transporter proteins and passage over the membrane of the enterocytes is followed by the formation of subapical vesicles. Within these vesicles, or lipid droplets, are the FAs transported to the ER for further processing. This vesicle formation occurs through clathrin-dependent endocytosis, and results in lipid droplet of which the membranes are highly enriched in IAP (Hansen et al. 2007). What mechanism is exactly initiating the endocytosis of FA is unknown, but Hansen et al., 2007 speculate that it is the rise of free FAs within the membrane that triggers the process of endocytosis. The FAs passing the enterocyte bilayer using the flip-flop mechanism may disrupt the balance between the inner and outer surface areas/leaflets. This imbalance may somehow account for the stimulation of endocytosis and pit formation (Hansen et al. 2007). Further research concluded that the FA are selectively inserted into the lipid raft domains of the membrane, which are important regions for membrane trafficking (Hansen et al. 2011). As IAP is also located in these lipid raft domains, it may explain the observed presence of IAP within the lipid droplets which result from FA uptake by endocytosis. Intracellular transport and chylomicron formation The uptake of FA from the lumen thus results in an increase of intracellular lipid droplets (Hansen et al. 2007), which are surrounded by endocytosed luminal enterocyte membrane containing IAP and other proteins (Narisawa & Huang 2003; Hansen et al. 2007). These molecules may escort the lipid droplet movement intracellularly towards the endoplasmic reticulum (ER) (Narisawa & Huang 2003), where the FAs are reesterified into TAGs. The resynthesis of FAs to TAGs is required because TAGs are a more inert product, as they yield more energy, that is. Also, not every target tissue is able to absorb and use FA as a source of energy (Mansbach & Siddiqi 2010).The absorbed free FAs which are not incorporated into lipid droplets, but bound to FABP, are also transported to the ER and reconstructed into TAGs. The TAGs are subsequently incorporated into chylomicrons, or, stored in a pool of fat 10 droplets inside the cytosol (Danielsen et al. 2013; Mansbach & Siddiqi 2010). How exactly the chylomicrons are transferred from the ER and Golgi remains unknown, but this membrane bound vesicles are probably involved in this transport (Mansbach & Siddiqi 2010). Exocytosis to lymphoid system Transporter vesicles presumably carry the chylomicrons towards the basolateral membrane of the enterocyte. Here they fuse with the membrane and exit the cell by reverse exocytosis. However, little is known about the exact mechanisms involved in the release of chylomicrons and absorption into the lymphoid system (Pan & Hussain 2012; Sabesin et al. 1977).After the release from the enterocytes, the chylomicrons with TAGs enter into lacteals, which are lymphatic vessels, which originate in the villi of the intestines (figure 1). The chylomicrons are then released into the bloodstream via the portal system and may subsequently distribute their content (Pan & Hussain 2012; Mansbach & Siddiqi 2010). 11 Chapter 2 An increased fat absorption due to a HFD has been linked to several pathologies as obesity, type 2 diabetes (T2D), and non-alcoholic fatty liver disease (NAFLD), but also not as apparent diseases as endotoxemia and liver cirrhosis. This chapter aims to get a better understanding of the mechanism behind the development of these diseases in response to a HFD. First the effect of a HFD on the gut microbiota is discussed, as well as the following effects of an altered intestinal epithelial wall in response to a HFD. Furthermore, the subsequent development of diseases linked to a HFD is addressed. Effects of HFD on gut microbiota Gut microbiota seem to be very important in the regulation of nutrient uptake, as they can facilitate the extraction of nutrients in the gut. There are indications that gut flora is particularly important regarding the uptake of fat in the small intestines. There are a few studies proposing some mechanisms of action on the influence gut microbes may have on FA absorption. One study showed that the microbiota in the gut can suppress intestinal Fiaf (fasting-induced adipocyte factor), which resulted in an increase of lipase activity and promoted the deposition of fat (Backhed et al. 2004). Following studies reported that the elevated Fiaf levels trigger the activity of coactivators which are involved in the regulation of FA oxidation (Backhed et al. 2007). It has been reported that the gut microbiota can change in response to a HFD, which is been suggested to be the link between a HFD and the development of several diseases related to an increased fat absorption (Frazier et al. 2011; de La Serre et al. 2010; Shen et al. 2013; Moreira et al. 2012). The composition of the gut flora seems to differ between lean and obese people which underlines the involvement of these microorganisms in fat uptake and a possible role in the development of obesity (DiBaise et al. 2008; de La Serre et al. 2010). It has been shown that the gut microbiota in the small intestines of obese patients consist of a different bacterial population, which can be evoked in response to a HFD (Moreira et al. 2012; de La Serre et al. 2010; Sabaté et al. 2008). A recent study suggested that due to consumption of a HFD, bile acid production is stimulated. The following increase of bile acid in the gut is facilitating the breakdown of dietary fat, but may also affect the composition of gut microbiota. Not all bacteria are able to deal with this change in their environment, potentially resulting in a selection towards the LPS producing gram negative bacteria. In addition, it has also been suggested that bile salts their selves may potentially be a threat on epithelial integrity 12 (Mansbach & Siddiqi 2010). However, there is a great lack of information on this matter, so the exact mechanism by which a HFD can alter the gut microbiota remains to be elucidated. However, what is clear is that a HFD can change the ratio between gram negative and gram positive bacteria, resulting in a dominating population of gram negative bacteria (Cani et al. 2007a; Cani et al. 2007b). The outer membrane of these bacteria contain LPS, and LPS levels have been shown to increase after excessive fat intake (Cani et al. 2007a; Laugerette et al. 2011; Delzenne & Cani 2011). As previously mentioned, LPS, or other PAMPs can trigger the immune response acting on the TLR4. When the TLR4 is activated, it can induce an inflammatory response via for example the NFĸB pathway (figure 3). Chronic inflammation can trigger the onset of a variety of diseases, as well as affect the integrity of the epithelial membrane of the enterocytes (De La Serre et al. 2010). Figure 3. Overview of Toll-like receptor 4 (TLR4) activation by lipopolysaccharide (LPS) as depicted by Laugerette et al., 2011. A: Structure of a lipopolysaccharide, comprising of an Oantigen, which is a repetitive glycan polymer, a core region which holds an oligosaccharide part and is attached to the lipid A region, which consists of a glucosamine disaccharide covered with multiple fatty acids and is phosphorylated. B: The inflammatory signaling induced by LPS binding to the TLR4. When activated, the TLR4 associates with membrane cluster of differentiation 14 (mCD14) to initiate the NFĸB signaling pathway. This ultimately results in the secretion of pro-inflammatory cytokines by immune cells. Effects of HFD on intestinal permeability Luminal enterocytes also function in the maintenance of the gut wall. Thus, next to the absorption of FA, they need to maintain a barrier which serves to exclude pathogens residing 13 in the gut. However, as a consequence of the HFD induced changes in microbial composition, the epithelial barrier of the gut lumen can be altered by the LPS induced inflammation (De La Serre et al. 2010). Several studies have been reporting leakiness of the gut wall after being fed to a HFD, which can be followed by an increase of systemic LPS levels (Laugerette et al. 2011). LPS from the gut lumen can either diffuse paracellularly via tight junctions (De La Serre et al. 2010; Moreira et al. 2012), or enter the system transcellularly via the enterocytes itself (Danielsen et al. 2013). A study by Danielsen et al., 2013 has reported a decrease in intestinal membrane integrity in a jejunum explant in vitro model after exposure to a HFD. The absorption of fat resulted in a leakiness of the crypt cells (figure 1), which are immature enterocytes and contain less IAP in their lipid rafts (Danielsen et al. 2013). It has also been reported that an excessive uptake of fat and LPS via chylomicrons, may increase the pressure in the intercellular space of the enterocytes. Due to this uptake, accumulation of chylomicrons may then result in a modification of junctional complexes between the epithelial cells (Salim & Söderholm 2011; Moreira et al. 2012), or may even cause membrane rupture (Moreira et al. 2012; Tso & Balint 1986). In addition, in vivo studies have been showing that high fat feeding can reduce the expression of several proteins associated with tight junctions (De La Serre et al. 2010; Moreira et al. 2012). Also, an activation of the TLR4 by LPS can alter the tight junctions between the enterocytes (Kohler et al. 2003). A HFD will therefore alter the membrane permeability, as after high fat feeding the population of LPS-containing bacteria increases. The consequence of this decreased membrane integrity is that even more LPS can enter the system. High LPS levels can cause a chronic inflammation, and this has been linked to a range of pathologies as inflammatory bowel diseases (Lallès 2010). Effects of HFD on pathogenesis development An increased fat uptake has been linked to a variety of diseases (DiBaise et al. 2008). Next to the danger of excessive deposition of fat around vital organs, a HFD has been linked to the occurrence of metabolic diseases (Frazier et al. 2011). As fat is a major source of energy for tissues in our body, dysregulation of its metabolism is hypothesized to have serious, general systemic consequences. An excess of lipid delivery to the liver, but also to the muscles requiring energy, has been linked to insulin resistance. Insulin is an important factor regulating one’s energy demand. 14 Insulin suppresses glucose production when blood concentrations rise, and ensures that excess glucose is stored in, for example, the liver, muscle or adipose tissue (Galbo & Shulman 2013). In liver cells, the reduction of glucose production is mitigated by the (phosphatidylinositide 3kinase) PI3K/Akt2 pathway. However, it has been shown that this signaling mechanism can be impaired by FAs, leading to an insulin resistance (Shulman 2000). Increased delivery of FAs to the liver can result in an accumulation of diacylglycerol (DAG) and can subsequently trigger the activation of PKCƐ, which inhibits the insulin receptor kinase activity (figure 4) (Galbo & Shulman 2013; Shulman 2000). The intracellular lipids may also be directly affecting PI3K, causing disruptive effects on the downstream signaling pathway. GLUT4 is a glucose transporter regulated by the PI3K/Akt2 pathway. A reduction in PI3K activity results in a decrease of translocation of the transporter to the plasma membrane of the cell, where GLUT4 normally transports glucose from the circulation into the cell (Shulman 2000; Bryant et al. 2002). There are also reports on the direct effects of FAs on impaired GLUT4 activity (Kahn 1992; Shulman 2000). The effects of free FA are not merely restricted to the liver cells, noted was that the PI3K/Akt2 pathway was also affected in muscle cells. Only in the muscle cells, excess FA activated PKCθ which resulted in the deactivation of insulin receptor kinase activity, and the subsequent altered effects on insulin functioning (Birkenfeld & Shulman 2013). Thus, initiated by increased FA uptake, hepatic, but also muscle cells may not be able to stimulate the down regulation of glucose production due to insulin sensitivity. Modulation of the insulin receptor may result in a disruption of the insulin-signaling cascade, and consequently a deficient handling of excess blood glucose concentrations. Chronic high levels of blood glucose concentrations are a factor in the onset of T2D (Galbo & Shulman 2013). 15 Figure 4. Mechanism of normal hepatic insulin action and insulin resistance, as proposed by Galbo and Shulman 2013. In the left section, a situation of normal insulin action is depicted. Insulin acts on its receptor, which leads to phosphorylation of IRS proteins, and the subsequent activation of the PI3K/Akt pathway. This pathway ultimately results in the suppression of glucose production, as well as the stimulation of glucose uptake from the blood. In the right panel, accumulation of diacylglycerol (DAG) and FAs trigger the activation of PKCƐ. The activation of this enzyme results in a deactivation of the kinase activity of the insulin receptor, and thus leading to an inhibition of the PI3K/Akt pathway including the subsequent inadequate suppression of glucose production. Insulin resistance can result in a redistribution of circulating glucose and FAs towards the liver, and has been linked to NAFLD (Cani et al. 2007a). This redistribution may be possible due to a regional alteration of FA/TAG mobilization. As the liver FATP and CD36 transporters are overexpressed in obese patients, relatively more fat can be absorbed by the liver cells, resulting in a redistribution of fat mobilization. Also, as mentioned in chapter one, dephosphorylation of CD36 by IAP leads to an activation of this transporter. As IAP levels rise during fat absorption, IAP-mediated activation of CD36 may be an underlying mechanism by which FA are redirected towards the liver (Birkenfeld & Shulman 2013; Greco et al. 2008). NAFLD is defined when the increased storage of lipid droplets will be present in more than 5% of the liver cells, and chronic deposition of fat in the liver may even result in liver cirrhosis which is irreversible and will cause major liver defects (Birkenfeld & Shulman 16 2013). That increased fat uptake may be an underlying cause of insulin resistance, T2D, and NAFLD, has been shown in several studies where a restriction of dietary fat remarkably improved the patients sensitivity to insulin, and reduced hepatic lipid content (Galbo & Shulman 2013; Petersen et al. 2005). Next to the direct effects of an increased fat deposition, excessive fat uptake is accompanied with increased serum levels of LPS (Cani et al. 2007a). Indeed, the majority of patients suffering from metabolic disorders as insulin resistance, obesity and diabetes show a high state of inflammation, reflected by an increased expression of pro-inflammatory cytokines (Moreira et al. 2012; Frazier et al. 2011). The overproduction of inflammatory cytokines and the activation of inflammatory pathways can be triggered by the systemic presence of endotoxins. This endotoxemia can develop in a systemic inflammation and can even lead to a septic shock (Hurley 1995). Recent evidence also links LPS produced by bacteria in the intestinal lumen to chronic liver diseases as liver cirrhosis (Pijls et al. 2013; Birkenfeld & Shulman 2013). There are studies suggesting that endotoxemia is the major cause in the development of obesity and insulin resistance (Cani et al. 2007a). However, it can also very well be that endotoxemia is only partly attributable to these pathologies, rather than a primary cause as the exact sequence of events remains unclear. This does not mean that the effects of a HFD on the development of endotoxemia is of minor importance, as it may partly explain the ever increasing prevalence of chronic diseases (Moreira et al. 2012; Cordain et al. 2005). Chapter 3 From the previous chapter it can be concluded that a HFD can cause a change the composition of the gut microbiota, which may result in local inflammation and the impairment of the epithelial barrier. This in turn causes an increased permeability of the gut. Therefore, systemic FA and LPS concentrations rise, which may ultimately result in a series of pathologies. As previously mentioned, IAP is an enzyme which is involved in the uptake of FA, and is able to dephosphorylate LPS. In this chapter the therapeutic role of IAP in the development of metabolic diseases will therefore be discussed. 17 Alkaline phosphatase Alkaline phosphatases (AP) are enzymes expressed in humans as well as numerous other species, including bacteria and zebrafish. As the name suggests, alkaline phosphatases are most active in alkaline environments. Peak activity occurs at an unusual pH 8-10.5 (Lynes & Widmaier 2011). There are several isoforms of alkaline phosphatase present in mammals; placental AP (PLAP), germ cell AP (GCAP), tissue nonspecific AP (TNAP) and IAP, all encoded by four different genes (Buchet et al. 2013). As previously mentioned, APs exert hydrolytic phosphatase activity which can remove phosphate groups from substrates as LPS, but also other DAMPs, and even from DNA or RNA (Pike et al. 2013; Buchet et al. 2013; Millan 2006). Studies have been reporting increased AP activity accompanied intestinal inflammation, suggesting an immune-related role for AP. It is known that IAP levels rise after a LPS, or other DAMP induced inflammation, yet AP can also suppress non-pathogen induced inflammation. Adenosine triphosphate (ATP) can trigger an inflammatory response, when it is released from cells in response to an inflammatory stimuli. As IAP is able to hydrolyze ATP, it may exert anti-inflammatory properties. In addition, TNAP levels have also been shown to rise in response to an intestinal inflammation (Lallès 2010; Pike et al. 2013). Furthermore, it has been reported that patients with inflammatory bowel diseases as Crohn’s disease and ulcerative colitis displayed lower expression of IAP mRNA, compared to non-inflamed tissue (Lallès 2010). This finding is also in agreement with an anti-inflammatory role of AP. However, most of the physiological functions of the APs are not fully known, yet KO studies have indicated some specific functions. It showed that TNAP is required for bone and teeth mineralization, and is also found in the liver and kidneys. IAP has been shown to reside in the epithelial membrane of the gut and is involved in the regulation of the uptake of dietary fat (Buchet et al. 2013). As the main entry of LPS into the system occurs through the cells of the gut wall, and as IAP plays a great role in the detoxification of LPS, IAP may be a very important mucosal defense factor. Therefore, there may be a great therapeutic potential for IAP. 18 IAP in response to HFD It has been shown that excessive fat absorption due to a HFD results in obesity. However, animal studies showed that despite the fact that the gut microbiota was altered, not all mice on a HFD became obese (De La Serre et al. 2010). This difference was suggested to be related to IAP, as this enzyme has been suggested to be a negative regulator of dietary fat absorption (Narisawa & Huang 2003). It was observed that the obese rats showed lower levels of IAP activity in relation to the non-obese rats on a low fat diet, and the rats on a high fat diet which were resistant to obesity (De La Serre et al. 2010). Moreover, IAP activity has been associated with a protective effect after LPS exposure and it has been reported that expression of IAP is induced by LPS stimulation (figure 5) (Bates et al. 2007; de La Serre et al. 2010). Figure 5. Proposed regulation of intestinal alkaline phosphatase (IAP) in response to endotoxin lipopolysaccharide (LPS), after Lallès 2010. A: When IAP expression or activity is high, it dephosphorylates LPS. In this way, the toll-like receptors (TLRs) are minimally stimulated and inflammatory responses remain low. B: When IAP activity is low, or a disruption in bacterial composition results in an overproduction of LPS, stimulation of the TLRs is high. This will result in an upregulation of inflammatory-related genes, and the expression of IAP. 19 IAP resides in the lipid raft region of the enterocyte membrane, where it can dephosphorylate the FA transporter CD36, thereby activating it (Lynes & Widmaier 2011). This is followed by an increased uptake of FA into the enterocytes. But, due to a concurring HFD induced change in gut microbiota, luminal LPS levels also increase. IAP can detoxify LPS by dephosphorylation of the lipid A region of LPS, and as mentioned before, removal of only one phosphate group already reduces toxicity with a 100 fold (Bates et al. 2007; Schromm et al. 1998). The exact mechanism by which a HFD induces this change of gut flora composition is not fully known, however, it has been suggested in chapter two that the increase in bile acid, required for the breakdown of dietary fat may play a role. As AP has a peak activity in alkaline environments, an increase of bile acid may reduce IAP action. This may attribute to the observed inflammatory response induced by LPS (David et al. 2013). By reducing the levels of LPS, IAP reduces the triggering of TLR4, which initiates the inflammatory response. Moreover, IAP is also able to block the translocation of NFĸB, the downstream inflammatory pathway of TLR4 (Lallès 2010). Normally, the uptake of FA is accompanied by elevated serum IAP levels, as IAP is incorporated into the chylomicrons which are required for FAs transport. However, when LPS levels rise too high due to a changed gut microbiota, IAP may become depleted. LPS can trigger an upregulation of genes related to IAP activity, but this may just simply not be sufficient enough when LPS levels are too high. In these cases, IAP present on the brush border membrane may merely be used to detoxify LPS, and may not be available and present anymore to be appropriately involved in the process of fat uptake (figure 6). The consequence of the absence of IAP on the epithelial membrane is that it may not accompany the transport of FA through the cells, and that therefore the IAP mediated retention on chylomicron formation may be lost. This depletion of IAP may also explain the inconsistent results of different studies regarding the response of IAP levels to a HFD. Some studies report an increase in IAP activity after feeding to a HFD, some show a decrease in IAP levels (De La Serre et al. 2010). It may be possible that differences in experimental design, that is % lipids in HFD, but also interspecific species differences, that are genetically present IAP levels, are responsible for the observed conflicting studies. Yet another reason that can explain the differences in research available may be time course related, as IAP activity may first be depleted, after which it may be up 20 regulated again. Differences in timing when measurements are taken may explain the observed contrasts in IAP activity (Lallès 2010). Figure 6. Overview of intestinal alkaline phosphatase (IAP) activity. IAP is able to detoxify LPS by the dephosphorylation of its lipid A moiety. Another function of IAP is the dephosphorylation of the CD36 transporter which facilitates fatty acid transport into the enterocytes. IAP is also suggested to be a negative regulator of fat absorption by reducing the secretion and transport of the fat containing chylomicrons in the enterocytes. 21 Discussion In this thesis, the aim was to paint a general picture on the effects of dietary fat and the subsequent development of several diseases. This was done by extensive literature research, and with a focus on the role of IAP. However, there is inconclusive data regarding mechanisms of fat uptake and the subsequent development of pathologies. Moreover, studies on the response of IAP to a HFD are contradictory. However, IAP has been suggested as a potential therapeutic drug regarding the development of metabolic diseases. As on the one hand, it has been established that IAP can detoxify LPS (Bates et al. 2007) and has been suggested to be a negative regulator of FA uptake as IAP knockout mice showed an increased fat deposition (Narisawa & Huang 2003). On the other hand however, IAP activates CD36 by dephosphorylation of the Thr92 residue (Lynes & Widmaier 2011), which leads to an uptake of FA into the cells. Thus, there seems to be a delicate balance where IAP regulates and mediates in multiple processes on FA uptake and LPS detoxification. Simply increasing luminal or systemic IAP levels may not reduce the uptake of fat into the system. However, as IAP does decrease the toxicity of LPS, high IAP levels may reduce the LPS initiated inflammatory response and the disruptive effects of the cytokines on membrane integrity. These high IAP levels will hereby prevent the gut wall from further damage induced by LPS, and maybe even the development of endotoxemia. As stimulation of the TLR4 by LPS induces IAP expression, this is a mechanism by which the body reduces the exposure to the toxic LPS. However, normal IAP regulation may not be able to withstand an excessive fat absorption and the increase of gram negative bacteria in the gut lumen induced by a HFD. As there are studies supporting the hypothesis that endotoxemia may be the primary cause of insulin resistance and other metabolic diseases instead of excessive FA (Shen et al. 2013), there may be a possible therapeutic role for IAP in the prevention of metabolic diseases. However the exact sequence of events leading to metabolic disorders remains unclear. It is recognized that IAP has a major therapeutic value, but there are still some bumps on the road. First of all, PLAP and GCAP are structurally very similar to IAP as they share an abundant sequence homology, and are clustered on the same chromosome (Lynes & Widmaier 2011; Buchet et al. 2013). Yet, specific functions of PLAP and GCAP remain largely unknown. Due to this similarity with IAP, there is a need for more information on the 22 functioning of these other phosphatases, and the receptors involved. When this is elucidated, undesirable effects of for example high systemic IAP levels can be better predicted. Nevertheless, there are studies reporting a potential for AP in several inflammation-associated diseases. Treatment with bovine IAP has been shown to decrease systemic inflammation after coronary bypass operations (Tuin et al. 2006). Also, AP treatment in sepsis-associated kidney injury has been shown to reduce the level of several markers of inflammation, thereby improving renal function (Peters et al. 2013). These studies all state that by dephosphorylation of LPS, and possibly other PAMPs or damaging factors as ATP, AP has a great potential in the treatment, and perhaps prevention of generalized inflammation. Figure 7. A proposed model where a high fat diet may induce the development of metabolic disorders adapted from De La Serre et al., 2010. A diet consisting of high dietary fat may lead to several metabolic disorders. A HFD can, next to the increased absorption of fatty acids (FA), alter the micro flora of the gut which results in an increase of LPS producing gram negative bacteria. This subsequently triggers TLR4 activation which results in an inflammatory response. Inflammation of the gut wall can cause alterations of tight junctions (TJs), which will increase the permeability of the gastro- intestinal (GI) wall. Due to the increased permeability, even more LPS can enter the system. Excessive uptake of FA can also 23 affect the permeability of the membrane, by alterations of the TJs. Moreover, increased plasma levels of FA and LPS may induce several metabolic diseases, of which the mechanisms behind are not entirely elucidated. Another very important application of IAP may be the targeting of the altered gut of newborns. It has been known that premature infants are very susceptible to inflammatory diseases in the gut. Necrotizing enterocolitis (NEC) is a severe inflammation of the gut wall, and to which premature intestines are specifically prone to (Bates et al. 2007; Chatterton et al. 2013). When IAP in the intestines of newborns is not expressed correctly, or the activity of IAP is somehow faulty or deficient, there may be an increased likelihood of LPS from the gut microbiota to trigger an inflammatory response. Supporting this school of thought is the fact that during normal postembryonic development, an increase of IAP activity occurs during the period where the gut flora is established (Bates et al. 2007). Also, in rodent studies it has been shown that IAP expression remained low during the suckling period, whereas its activity steadily increased to adult levels at the time when they started consuming a normal diet (Lallès 2010). In addition, mothers’ colostrum consists of a multitude of proteins and enzymes with anti-inflammatory properties, including IAP. It has been proposed this is the reason why premature born infants, which are formula fed, are more susceptible to intestinal inflammatory diseases as NEC (Chatterton et al. 2013). 24 Conclusion Taken all the literature evidence together, fat absorption in the proximal part of the small intestine is mediated by IAP. IAP on the lipid raft regions of enterocytes dephosphorylates FA transporter CD36, thereby activating it. IAP is also involved in the negative regulation of the secretion of chylomicron vesicles containing FA. When consuming a HFD however, IAP activity may become depleted, leading to an increased fat absorption. Increased levels of FA are accountable for the development of a series of diseases, as it can lead to a redirection of FA towards the liver and muscles. Here, it can induce insulin resistance, obesity and even liver cirrhosis. A HFD not only results in an increased deposition of excess fat, it can also result in a change of gut microbiota, favoring the composition towards gram-negative bacteria. These bacteria produce the endotoxin LPS, which can trigger an inflammatory response. Rising levels of LPS may also contribute to the depletion of IAP activity after consuming a HFD, as IAP can reduce LPS toxicity by the removal of its phosphate groups. In addition, the local inflammatory response mediated by LPS, can cause an alteration of the gut barrier. Tight junctions can be affected, also in response to a high fat uptake, resulting in an increased permeability of the epithelial membrane. Due to this increased permeability, more LPS can enter the system, consequently triggering more inflammatory responses. This endotoxemia has also been suggested to be, partly, accountable for a variety of diseases, including insulin resistance and obesity. As IAP is able to detoxify LPS, and has also been suggested to be a negative regulator of fat absorption, it has great therapeutic value however, more research on this matter is required. 25 References Asch, A. et al., 1993. Analysis of CD36 binding domains: ligand specificity controlled by dephosphorylation of an ectodomain. Science, 262, pp.1436–40. Backhed, F. et al., 2007. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proceedings of the national academy of science USA, 104(3), pp.979– 984. Backhed, F. et al., 2004. The gut microbiota as an environmental factor that regulates fat storage. Proceedings of the national academy of sciences of the United States of America, 101(44), pp.15718–15723. Baillie, A., Coburn, C. & Abumrad, N., 1996. Reversible binding of long-chain fatty acids to purified FAT, the adipose CD36 homolog. Journal of membrane biology, 153, pp.75–81. Bates, J.M. et al., 2007. Intestinal alkaline phosphatase detoxifies lipopolysaccharide and prevents inflammation in zebrafish in response to the gut microbiota. Cell host & microbe, 2(6), pp.371–82. Birkenfeld, A.L. & Shulman, G.I., 2013. Non alcoholic fatty liver disease, hepatic insulin resistance and type 2 diabetes. Hepatology, pp.1–32. Bryant, N., Govers, R. & James, D., 2002. Regulated transport of the glucose transporter GLUT4. Nature reviews. Molecular cell biology, 3, pp.267–277. Buchet, R., Millán, J. & Magne, D., 2013. Phosphatase Modulators J. L. Millán, ed., Totowa, NJ: Humana Press. Cani, P.D. et al., 2007a. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes, 56(July), pp.1761–1772. Cani, P.D. et al., 2007b. Selective increases of bifidobacteria in gut microflora improve highfat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia, 50(11), pp.2374–83. Chatterton, D. et al., 2013. Anti-inflammatory mechanisms of bioactive milk proteins in the intestine of newborns. The international journal of biochemistry & cell biology, 45(8), pp.1730–47. Cordain, L. et al., 2005. Origins and evolution of the Western diet: health implications for the 21st century. American society for clinical nutrition, 81(2), pp.341–354. Danielsen, E., 1995. Involvement of detergent-insoluble complexes in the intracellular transport of intestinal brush border enzymes. Biochemistry, 34(5), pp.1596–1605. Danielsen, E. et al., 2013. Permeabilization of enterocytes induced by absorption of dietary fat. Molecular membrane biology, 30(3), pp.261–72. 26 Danielsen, E. & Hansen, G., 2006. Lipid raft organization and function in brush borders of epithelial cells. Molecular membrane biology, 23, pp.71–79. David, L.A. et al., 2013. Diet rapidly and reproducibly alters the human gut microbiome. Nature. doi:10.1038 Delzenne, N. & Cani, P., 2011. Gut microbiota and the pathogenesis of insulin resistance. Current diabetes reports, 11, pp.154–159. DiBaise, J. et al., 2008. Gut microbiota and its possible relationship with obesity. Mayo Clinic proceedings, 83(4), pp.460–9. Frazier, T.H., DiBaise, J.K. & McClain, C.J., 2011. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Journal of parenteral and enteral nutrition, 35(1), pp.14–20. Galbo, T. & Shulman, G., 2013. Lipid-induced hepatic insulin resistance. Aging, 5(8), pp.582–583. Glatz, J., Luiken, J. & Bonen, A., 2010. Membrane fatty acid transporters as regulators of lipid metabolism: implications for metabolic disease. Physiological reviews, 90(1), pp.367–417. Greco, D. et al., 2008. Gene expression in human NAFLD. American journal of gastrointestinal and liver pathology, 294(5), pp.1281–1287. Guthmann, F. et al., 2002. Ectoprotein kinase-mediated phosphorylation of FAT/CD36 regulates palmitate uptake by human platelets. Cellular and molecular life sciences, 59, pp.1999–2003. Hansen, G. et al., 2011. Dietary free fatty acids form alkaline phosphatase-enriched microdomains in the intestinal brush border membrane. Molecular membrane biology, 28(2), pp.136–44. Hansen, G. et al., 2007. Intestinal alkaline phosphatase: selective endocytosis from the enterocyte brush border during fat absorption. American journal of physiology. Gastrointestinal and liver physiology, 293(6), pp.G1325–32. Haslam, D.W. & James, W.P.T., 2005. Obesity. Lancet, 366(9492), pp.1197–209. Hurley, J., 1995. Endotoxemia: methods of detection and clinical correlates. Clinical mircobiology reviews, 8(2), pp.268–292. Inglis, N., Krant, M. & Fishman, W., 1967. Influence of a fat-enriched meal on human serum (L-phenylalanine-sensitive) “intestinal” alkaline phosphatase. Proceedings of the society of experimental biology and medicine, 124, pp.699–702. Kahn, B., 1992. Facilitative glucose transporters: regulatory mechanisms and dysregulation in diabetes. Journal of cinical investigations, 89, pp.1367–1374. 27 Kamp, F. & Hamilton, J.A., 1992. pH gradients across phospholipid membranes caused by fast flip-flop of un-ionized fatty acids. Proceedings of the national academy of sciences of the United States of America, 89, pp.11367–11370. Keiding, N., 1966. Intestinal alkaline phosphatase in human lymph and serum. Scandinavian journal of clinical laboratory investigation, 18, pp.134–140. Kohler, H., McCormick, B. & Walker, W., 2003. Bacterial-enterocyte crosstalk: cellular mechanisms in health and disease. Journal of pediatric gastroenteroly nutrition, 36, pp.175–185. De La Serre, C. et al., 2010. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. American journal of gastrointestinal and liver physiology, 299(34), pp.440–448. Lallès, J.P., 2010. Intestinal alkaline phosphatase: multiple biological roles in maintenance of intestinal homeostasis and modulation by diet. Nutrition reviews, 68(6), pp.323–32. Laugerette, F. et al., 2011. Complex links between dietary lipids, endogenous endotoxins and metabolic inflammation. Biochimie, 93(1), pp.39–45. Lingwood, D. & Simons, K., 2010. Lipid rafts as a membrane-organizing principle. Science, 327(5961), pp.46–50. Lynes, M.D. & Widmaier, E.P., 2011. Involvement of CD36 and intestinal alkaline phosphatases in fatty acid transport in enterocytes, and the response to a high-fat diet. Life sciences, 88(9-10), pp.384–91. Mansbach, C. & Siddiqi, S., 2010. The biogenesis of chylomicrons. Annual review of physiology, 72, pp.315–33. Millan, J., 2006. Mammalian alkaline phosphatases: from biology to applications in medicine and biotechnolog. Moreira, A.P.B. et al., 2012. Influence of a high-fat diet on gut microbiota, intestinal permeability and metabolic endotoxaemia. The British journal of nutrition, 108(5), pp.801–9. Narisawa, S. & Huang, L., 2003. Accelerated fat absorption in intestinal alkaline phosphatase knockout mice. Molecular and cellular biology, 23(21), pp.7525–7530. OECD & EU, 2010. Health at a glance: Europe 2010, Pan, X. & Hussain, M.M., 2012. Gut triglyceride production. Biochimica et biophysica acta, 1821(5), pp.727–35. Peters, E. et al., 2013 Alkaline phosphatase as a treatment of sepsis-associated acute kidney injury. Journal of pharmacology and experimental therapeutics, 334(1), pp. 2-7 28 Petersen, K. et al., 2005. Reversal of Nonalcoholic Hepatic Steatosis, Hepatic Insulin Resistance, and Hyperglycemia by Moderate Weight Reduction in Patients With Type 2 Diabetes. Diabetes, 54(3), pp.603–608. Pijls, K.E. et al., 2013. Intestinal epithelial barrier function in liver cirrhosis: an extensive review of the literature. Liver international, 33(10), pp.1457–69. Pike, A.F. et al., 2013. A novel hypothesis for an alkaline phosphatase “rescue” mechanism in the hepatic acute phase immune response. Biochimica et biophysica acta, 1832(12), pp.2044–56. Sabaté, J. et al., 2008. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: a contributor to sever hepatic steatosis. Obesity surgery, 18(4), pp.371–377. Sabesin, S., Clark, S. & Holt, P., 1977. Ultrastructural features of regional differences in chylomicron secretion by rat intestine. Experimental and molecular pathology, 26(2), pp.277–289. Salim, S. & Söderholm, J.D., 2011. Importance of disrupted intestinal barrier in inflammatory bowel diseases. Inflammatory bowel diseases, 17(1), pp.362–81. Schromm, A., Brandenburg, K. & Loppnow, H., 1998. The charge of endotoxin molecules influences their conformation and IL-6-inducing capacity. Journal of immunology, 161(10), pp.5464–5471. Shen, J., Obin, M.S. & Zhao, L., 2013. The gut microbiota, obesity and insulin resistance. Molecular aspects of medicine, 34(1), pp.39–58. Shulman, G.I., 2000. On diabetes : insulin resistance Cellular mechanisms of insulin resistance. The journal of clinical investigation, 106(2), pp.171–176. Stahl, A., 2004. A current review of fatty acid transport proteins (SLC27). Pflügers Archiv : European journal of physiology, 447(5), pp.722–7. Townsend, K., Lorenzi, M. & Widmaier, E., 2008. High-fat diet-induced changes in body mass and hypothalamic gene expression in wild-type and leptin-deficient mice. Endocrinology, 33, pp.176–88. Tuin, A. et al., 2006 On the role and fate of LPS-dephosphorylating activity in the rat liver. American journal of physiology. Gastrointestinal and liver physiology, 290(2), pp. G377-385 Tso, P. & Balint, J., 1986. Formation and transport of chylomicrons by enterocytes to the lymphatics. American journal of physiology. Gastrointestinal and liver physiology, 250, pp.715–726. Whitlock, G. et al., 2009. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet, 373(9669), pp.1083–96. 29 30