VOYA & CAR-T marketing for Vietnam HK, 10July2018
advertisement

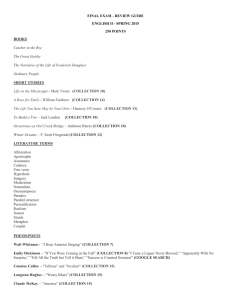
CAR-T treatment for Cancer and VOYA THERAPEUTICS 10 July 2018 Contents Immunotherapy for cancer & CAR-T ............................................................................................. 1 VOYA Therapeutics, the company manufacturing CAR-T cells in Malaysia ............................... 1 Appendix: Recent news on CAR-T ................................................................................................ 2 Appendix 01: CAR T-cells: an exciting frontier in cancer therapy............................................. 2 Appendix 02: Tragedy, Perseverance, and Chance — The Story of CAR-T Therapy................ 3 Appendix 03: ASCO named adoptive cell immunotherapy as the clinical cancer advance of the year .............................................................................................................................................. 5 Immunotherapy for cancer & CAR-T Immunotherapy is a new way of treating cancer by harnessing the host’s immune system. Instead of directly destroying cancer cells (such as by using chemotherapy or radiation), immunotherapy uses the patient’s own or donor’s immune cells (such as T or NK cells) to destroy cancer cells. Among the several approaches to immunotherapy, Chimeric Antigen Receptor T cell (CAR-T) therapy represents a remarkable scientific advance in the treatment of patients with cancers. CAR-T therapy is like bone marrow or stem cell transplant. It uses a patient’s own or a donor’s T cells which is modified in the lab to express chimeric antigen receptors (CARs). When the CART cells are re-infused into patient, the CAR receptor specifically target antigens expressed on cancer cells and the activated T cells then destroy the cancer cells. CAR-T cells have produced impressive clinical results which have led to US FDA approval in 2017 for tisagenlecleucel (marketed by Novartis in US as Kymriah) for the treatment of Acute Lymphoblastic Leukaemia and for axicabtagene ciloleucel (marketed by Gilead Sciences in US as Yescarta) for the treatment of Non-Hodgkin’s Lymphoma. CAR-T treatments for other cancers such as Myelomas, Brain, Colon, Ovarian and Thyroid are under development. CAR-T therapy is so effective it is the first and only cancer treatment that comes with a “money back guarantee” (that is, if a patient with Leukemia is NOT in remission 4 weeks after starting treatment, he or she doesn’t have to pay for the treatment). The American Society of Clinical Oncology (ASCO) has named adoptive cell immunotherapy as the clinical cancer Advance of the Year in 2017. To learn more about CAR-T, see the ASCO’s video https://youtu.be/fMiqO2Ivr_Y. Refer Appendix for recent news and background information on CART. VOYA Therapeutics, the company manufacturing CAR-T cells in Malaysia VOYA Therapeutics Sdn Bhd (VTSB) is a life science company developing, manufacturing and marketing CAR-T therapy for the treatment of Leukemias (ALL), Lymphomas (NHL), Myelomas and other cancers in Malaysia and SE Asia. Leukemias and Lymphomas are ranked as the top 8th and 9 th cancers in Malaysia and affects about 3000 people a year [Globocan 2012 data]. These cancers are highly prevalent too in other countries in Asia too. We are seeking partners in Asia to help promote this remarkable advanced therapy to benefit more patients who otherwise will have no other treatment options. 1 To date, in our ongoing trial in Malaysia, we have treated 8 patients with good results (only one treatment failure). For details, refer to our Abstract to be presented at a scientific meeting of the International Academy for Clinical Hematology (IACH) this September 2018 http://iach2018.cme-congresses.com/ Outside the clinical trial, we have also treated several patients on compassionate ground, including foreign patients who have travelled to Malaysia just for this as CAR-T treatment is not available yet in other SE Asian countries. Our experience with one patient CGN from Bandong Indonesia below. Patient CGN with her mum Patient CGN in remission after Hospital lab report confirming and brother (who donated his CAR-T treatment; celebrating patient CGN’s leukemia in bone marrow to her but the Xmas in December 2017 remission at 4 weeks after transplant failed), and Dr Lim CAR-T treatment. TO, VOYA’s CMO at hospital before CAR-T treatment Appendix: Recent news on CAR-T 1. Lancet Editorial. CAR T-cells: an exciting frontier in cancer therapy 2. Lisa Rosenbaum. Tragedy, Perseverance, and Chance — The Story of CAR-T Therapy. N Engl J Med 2017; 377;14 3. This year, ASCO named adoptive cell immunotherapy as the clinical cancer Advance of the Year. See Appendix01 See Appendix02 See Appendix03 Appendix 01: CAR T-cells: an exciting frontier in cancer therapy The Lancet DOI: http://dx.doi.org/10.1016/S0140-6736(17)32395-4 Published: 09 September 2017 On Aug 30, the US Food and Drug Administration (FDA) approved tisagenlecleucel (marketed by Novartis as Kymriah) as the first ever treatment that genetically modifies patients' own T cells. The approval is for children and young adults (up to 25 years of age) with relapsed or refractory acute B-cell lymphoblastic leukaemia—a leading cause of childhood cancer deaths. This treatment option is currently limited to 20 specially certified centres in the USA because of the complexity of the procedure and potentially serious side-effects. The patient's own T cells will be removed by leuka-pheresis and transported to Novartis's laboratory in Morris Plains, NJ, USA. In the laboratory, T cells will be genetically altered to produce receptors on their 2 surface called chimeric antigen receptors (CAR), multiplied, and then will be reinfused into the patient after a lymphodepleting chemotherapy regimen. These receptors allow T cells, which further replicate in the patient's body, to recognise the B-cell antigen CD19 on the tumour cell surface and kill these cancer cells. As a side-effect, this process can also cause the so-called cytokine release syndrome, which can be treated with supportive therapy, steroids, or the specific interleukin-6 blocker tocilizumab. B-cell aplasia (normal B cells also express CD19) and cerebral oedema have been observed as other serious side-effects. FDA approval follows early results of a continuing small (63 patients) phase 2 study, in which 52 patients achieved complete remission in the 3 months after drug administration. Longer-term data will be needed to allow true comparison of benefit-risk outcomes and cost benefit. The treatment is expensive at US$475 000. Novartis will waive the fee if there is no response at 1 month. This remarkable technical advance is exciting scientific progress in a disorder with few treatment options. But given the limited data supporting its use, the introduction of tisagenlecleucel should be seen as a first cautious step in an approach that needs much more refinement and research for this and other indications. Appendix 02: Tragedy, Perseverance, and Chance — The Story of CAR-T Therapy Lisa Rosenbaum. N Engl J Med 2017; 377;14 https://www.nejm.org/doi/full/10.1056/NEJMp1711886 In 2010, 5-year-old Emily Whitehead was diagnosed with acute lymphoblastic leukemia (ALL). Though her parents were told that if you had to have a kid with cancer, ALL was the best one to have, Emily’s course was hardly typical. After two rounds of chemotherapy, necrotizing fasciitis developed in both legs and she barely avoided amputation. Sixteen months later, she had a relapse. Bone marrow transplantation was recommended, but the Whiteheads, concerned about toxic effects, sought a second opinion at Children’s Hospital of Pennsylvania. There they learned about a new therapy, developed by University of Pennsylvania investigators and known as CART-19, which involved genetically engineering the patient’s own T cells to kill tumor cells. Unfortunately, a clinical trial had not yet been cleared by the Food and Drug Administration (FDA), and Emily’s leukemic cells were doubling daily. So Emily returned to her local hospital and received another round of intensive chemotherapy, which bought her 3 weeks but no remission. Out of options, one oncologist recommended hospice. But “That just didn’t make sense to us,” says Tom Whitehead, Emily’s father. When the Whiteheads said they wanted to return to Children’s Hospital, the oncologist told them that hospice was preferable to entering Emily into an experimental study that wouldn’t help her get better. But her parents opted to enroll her in a study, and she became the first child to receive CART-19. As a result, not only is she now a thriving 12-year-old, but her survival helped reenergize a line of research that was nearing failure. In August 2017, the FDA approved the first chimeric antigen receptor T-cell (CART) therapy, Novartis’s tisagenlecleucel, which uses the Penn-developed technology, for patients up to 25 years of age with relapsed or refractory ALL. Though the indication is narrow, the results are striking in a patient population with otherwise limited options: 83% of the 63 evaluable children who received tisagenlecleucel in Novartis’s phase 2 trial had complete elimination of malignant cells at 3 months.1 The approval is probably the first of many for CAR-T products. Gilead recently announced its $11.9 billion acquisition of Kite Pharma, whose CAR-T technology, initially developed at the National Institutes of Health (NIH), has shown efficacy in patients with chemorefractory, aggressive B-cell nonHodgkin’s lymphoma.2 And some 40 other companies, many in partnership with academic institutions, are racing to develop CAR-T technologies for myriad indications. Though early data are most promising 3 for other hematologic cancers, such as relapsed chronic lymphocytic leukemia (CLL),3 similar therapies may eventually prove effective for solid tumors as well. The emergence of CAR-T therapy, like most scientific advances, reflects the incremental insights of hundreds of scientists over decades — from surgeon William Coley’s recognition of the immune system’s potential for treating cancer when, in 1893, he injected streptococcus into inoperable osteosarcoma and observed the tumor shrink, to the making of the first CAR-T cells by the Israeli immunologist Zelig Eshhar in 1993.4 Indeed, the story of CAR-T therapy says as much about the methodical nature of scientific progress as it does about the passions that sustain it. As Carl June, the immunologist who led the development of Penn’s CAR-T technology, recalled, “So many times, I almost had to quit.” June spent his early career developing a technique to boost immune function in patients with HIV by modifying their T cells and inducing proliferation ex vivo. Though he and his colleague Bruce Levine would later build on this technique to engineer patients’ T cells to attack leukemia, June might have continued focusing solely on the basic science. But in 1996, his 41-year-old wife was diagnosed with ovarian cancer. June tried unsuccessfully to get a pharmaceutical company to provide the tools he needed to attempt immunotherapy. When his wife died in 2001, June resolved to apply emerging immunologic insights to the development of cancer therapies, even though that meant creating a biotech infrastructure within academia. The translational hurdles remained formidable. The field had been dogged by skepticism and setbacks, and the NIH wouldn’t fund a clinical trial. Once again, tragedy propelled the research forward. In 2001, Barbara and Edward Netter, having watched their daughter-in-law die of breast cancer, started the Alliance for Cancer Gene Therapy (ACGT), hoping to develop alternative approaches. In 2008, ACGT granted June and his coinvestigator David Porter $1 million, enough to treat their first three patients with relapsed CLL with CART-19. Two of the three patients achieved complete remission, but the investigators ran out of funding. Knowing they couldn’t prove efficacy statistically, they published their findings as case reports.3,5 Soon, the National Cancer Institute offered June a grant, and Novartis licensed Penn’s CAR-T technology. But June acknowledges the tenuous nature of anecdote: “Were we lucky? Were they representative? Would it be durable?” Indeed, anecdote can easily break a field rather than make it: the death of Jesse Gelsinger in a trial at Penn had set the field of gene therapy back at least a decade. And as both June and Stephan Grupp, the Children’s Hospital oncologist and principal investigator of the CART-19 trial in children, emphasized, had Emily died, the CAR-T field would probably have died with her. But though unexpected toxic effects in phase 1 studies can fell any new therapy, the unfortunate reality is that it often takes time, and human lives, to distinguish fatal toxic effects from those that can be managed. As Grupp explained, “There was no way to predict a great deal of what we learned. The toxicity issues can only be learned from human beings.” Emily Whitehead was a case in point. After receiving her third dose of CART-19, she developed high fevers, respiratory failure, and shock necessitating the use of three pressors. Though Emily was experiencing what’s now understood to be cytokine-release syndrome, which occurred in 78% of patients in Novartis’s phase 2 trial, it wasn’t clear at the time what was driving this response, much less how to treat it. That she survived gives new meaning to the adage “Chance favors the prepared mind.” Per protocol, participants’ blood was sent for cytokine analysis, with about a 2-week turnaround time. But as Emily rapidly deteriorated, Grupp called the lab and begged them to run Emily’s blood more quickly. Two hours later, in time for his 3 p.m. lab meeting, Grupp learned that Emily’s level of interleukin-6 was elevated 4 1000-fold. He recalls the meeting, as everyone pored over the results. “No one thought we should be thinking about this thing, IL6,” Grupp explained. “It isn’t even made by T cells.” That fact, however, made interleukin-6 acceptable for Emily’s doctors to target, since any interference with T-cell function could interfere with the antileukemic activity, without which she would die. But how to quash interleukin6? As Grupp and his lab members started Googling, June, giving a talk in Seattle, received the results and had an idea. His daughter, who has juvenile rheumatoid arthritis, had recently started taking tocilizumab, a monoclonal antibody that targets interleukin-6. As the investigators converged on a similar conclusion, one hurdle remained: how to get the drug in time for Emily? Once again, they got lucky. Tocilizumab was on the hospital’s formulary for rheumatologic indications, which meant that rather than having to wait for up to 2 days, by 8 p.m. that evening, Emily received a dose. Within hours, she began to improve, so dramatically that her doctors could barely wean the pressors fast enough. On her seventh birthday, Emily woke up. Eight days later, on the basis of a bone marrow biopsy, Grupp reported that the treatment had worked. Though the remissions achieved with CAR-T therapy are impressive, much remains unknown. CAR-T products vary in ways that will have implications for both efficacy and toxicity. Some variation arises from the chimeric antigen receptors (CARs) themselves, which are programmed to recognize various antigens and contain various types and numbers of costimulatory domains to induce proliferation. In the case of CART-19, for instance, the engineered T cells bind to lymphocytes displaying the CD19 antigen, a hallmark of leukemic B cells and thus an attractive target because humans can tolerate B-cell aplasia. Identifying antigen targets in solid tumors while preventing destruction of healthy tissue remains challenging, however, especially since the tumor microenvironment can be immunologically hostile to introduction of a CAR. Moreover, toxicities remain formidable. Though tocilizumab is now often used to manage the cytokine-release syndrome, other toxic effects, such as cerebral edema, remain poorly understood and difficult to manage. Meanwhile, the CAR-T discussion has become dominated by cost concerns. Critics argue that tisagenlecleucel’s $475,000 price tag is unaffordable and unjustifiable given the taxpayer-supported basic research underpinning its development, while manufacturers point to the tremendous investment required to produce the drug and fund trials. With many patients unable to afford their medications and ongoing instances of unconscionable drug-company profiteering, these discussions are both essential and complex. Regardless of the finances, we all hope that these remissions are prolonged or, even better, turn out to be cures. There is no way to know whether they will without prolonged observation, but while we carefully observe each patient, it is important to remember that therapeutic advances are motivated by more than money — that it’s the hope, vision, and perseverance of both patients and investigators that have made this critical conversation possible. Appendix 03: ASCO named adoptive cell immunotherapy as the clinical cancer advance of the year https://www.asco.org/research-progress/reports-studies/clinical-cancer-advances-2018/advance-year This year, ASCO named adoptive cell immunotherapy as the clinical cancer Advance of the Year. After decades of research, this powerful and decidedly unique way of treating cancer has become available to certain patients with an otherwise incurable blood cancer. What Is Adoptive Cell Immunotherapy? Immune cells navigate the body looking for anything that does not belong—bacteria, viruses, and even cancer cells. They do so by using their molecular feelers, or receptors, to scan for foreign molecules that 5 intruder cells display on their surface. Once an intruder is detected, a class of immune cells, known as cytotoxic T cells, move in to eliminate it. Unfortunately, cancers have a number of ways to hide from immune cells and avoid their attack. The recently successful immunotherapy approaches aim to remedy this by taking the brakes off the immune system with the use of targeted drugs, known as immune checkpoint inhibitors. Whereas adoptive cell immunotherapy also boosts the body’s immune defenses against cancer, it does so in a completely different way—by genetically re-engineering a patient’s own immune T cells. In the late 1980s, an immunologist was the first to experiment with genetically reprogramming T cells, now known as CAR T cells. CAR T cells are custom made to work against the cancer in each individual patient. To create these cells, researchers collect immune T cells from the patient and insert an artificial gene into the cells. The gene is designed to endow T cells with chimeric antigen receptors that can detect unique molecules on cancer cells after CAR T cells are multiplied in the laboratory and injected back into the patient. In essence, CAR T-cell therapy is both a gene therapy and an immunotherapy. When the CAR T-cell receptor attaches to a molecule on a cancer cell, it sends a signal to turn on the destruction machinery of the T cell. Unlike traditional cancer treatments, this living therapy needs to be given to the patient only once, because CAR T cells continue to multiply in the patient’s body. As a result, the anticancer effects of CAR T cells can persist and even increase over time. CAR T-Cell Therapy Is Poised to Transform Childhood ALL Treatment In 2017, researchers demonstrated that a CAR T-cell therapy known as tisagenlecleucel can eradicate relapsed ALL in children. This represents one of the most remarkable advances in the treatment of childhood cancer in the last decade and could dramatically change treatment paradigms for this disease. Tisagenlecleucel targets a protein, known as CD19, on malignant and normal B cells. In the United States, ALL will recur in approximately 600 children and young adults per year, despite achieving a response to initial therapy. After a relapse, ALL is difficult to treat, and survival is usually measured in weeks to months. Remission rates with current standard therapies in prior clinical trials have been only 20% with chemotherapy and 33% with targeted therapy.10,11 In a clinical trial of children and young adults with relapsed or refractory ALL, cancer went into remission within 3 months of receiving tisagenlecleucel in 52 (82%) of 63 patients, and 75% of patients remained relapse free at 6 months.12,13 On the basis of these findings, the FDA approved tisagenlecleucel for the treatment of children and young adults with B-cell ALL in August 2017.14 This global clinical trial confirmed the high efficacy that was demonstrated in prior, single-institution trials; however, the rate of immune-related adverse effects was high with tisagenlecleucel. Nearly 50% of patients experienced severe cytokine release syndrome (CRS), a complication during which CAR T cells produce a storm of inflammatory molecules. CRS can cause prolonged fever, low blood pressure, difficulty breathing, and problems with multiple organs. If severe, CRS may require intensive medical care, such as the use of a ventilator or medications known as pressors to increase blood pressure, and seizure medication. Although CRS can be serious and even life-threatening, doctors now have an effective medicine (tocilizumab) with which to curb and, in most cases, fully reverse the symptoms. In addition, neurologic complications occurred in 15% of patients in the study. A broad range of neurologic problems, including word recall issues, difficulty speaking, reduction of alertness, delirium, hallucinations, seizures, and coma, have been reported in prior clinical trials with CAR T-cell therapies. In most patients, such symptoms resolved on their own within a few days without long-term consequences, but several deaths have occurred, with severe neurologic complications in other CAR Tcell trials. In this ALL trial, there were no deaths related to either CRS or neurologic complications. The global ALL trial also helped to prove that patient access to this novel treatment could be broadened. It was the first time CAR T cells were produced from patient blood cells in an industrial manufacturing facility and distributed to patients via a global supply chain that included 25 centers in the United States, 6 Canada, Europe, Australia, and Japan. Until then, the production of CAR T cells was limited to few academic laboratories, without the ability to ship the cell product to patients around the world. CAR T-Cell Therapy Is Effective Against Hard-to-Treat Lymphoma in Adults CAR T cells that target CD19 have also been proven to be promising against another hard-to-treat cancer, diffuse large B-cell lymphoma (DLBCL), which is the most common type of non-Hodgkin lymphoma. In a multicenter clinical trial of patients with DLBCL that worsened after at least two prior therapies, the cancer responded to tisagenlecleucel in 59% of 51 patients and went into remission in 43% of patients.15 At 6 months, 79% of patients had not had a recurrence of lymphoma. Severe CRS occurred in 25% of patients, and neurologic complications in 13%. In a different clinical trial, patients with relapsed or refractory DLBCL, refractory primary mediastinal Bcell lymphoma, or transformed follicular lymphoma, received another CAR T-cell product called axicabtagene ciloleucel that also targets CD19.16 Among the first 92 patients who were treated, the response rate was 82%, with complete remissions occurring in 54% of patients. At a median follow-up of 8.7 months, 39% of patients were still in complete remission. Severe CRS occurred in 13% of patients; neurologic adverse effects occurred in 28% of patients. In late 2017, the FDA approved axicabtagene ciloleucel to treat adults with DLBCL that has not responded to or has recurred after at least two prior therapies.17 CAR T-Cell Therapy Sends Multiple Myeloma Into Remission The studies described above all included CAR T cells that were targeted to the B-cell biomarker CD19. A different type of CAR T-cell therapy that targets a biomarker known as B-cell maturation antigen seems to be effective against multiple myeloma. Despite recent advances in treatment, multiple myeloma—a cancer of plasma cells that make antibodies to fight infections—remains an incurable disease, with only approximately one-half of patients living 5 years after diagnosis. In an early clinical trial, the cancer responded to B-cell maturation antigen CAR T cells in 33 (94%) of 35 patients and went into complete remission in 14 patients18 (Updated data presented at the 2017 ASCO Annual Meeting in Chicago, IL). Only two patients experienced severe CRS, and none experienced neurologic complications from CAR T-cell therapy. 7