Cesarean Section Indications in Private Facility In Kenya
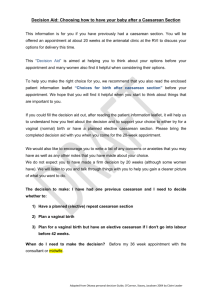
advertisement

A REVIEW OF CAESAREAN SECTION RATES, INDICATIONS AND OUTCOMES AT MP SHAH HOSPITAL – NAIROBI STUDY PROPOSAL SUBMITTED BY DR JAHONGA 2000 1 TABLE OF CONTENTS 2 1. 2. 3. 4. 5. 6. Title 3 List of abbreviations and definitions ..................................................................................... 4 Abstract 5 Introduction and literature review ......................................................................................... 6 Rationale .................................................................................................................................... 15 Objectives .................................................................................................................................. 16 6.1 Broad objective 6.2 Specific objectives 7. Methodology ............................................................................................................................. 16 a. Variables .............................................................................................................. 16 1.1 Study design ....................................................................................................... 16 1.2 Study area 1.3 Study population 1.4 Inclusion and Exclusion Criteria Sampling and sample size determination 7.5.1 Data collection .................................................................................................... 18 7.6.1 Data Management .............................................................................................. 18 7.6.2 Study period 7.6.3 Anticipated Study Constraints .......................................................................... 19 7.7 Ethical Considerations .................................................................................................... 19 7.8 Work Plan Budget estimate ............................................................................................ 20 7. References ............................................................................................................................... 21 8. APPENDIX 1: Questionnaire................................................................................................ 27 9. Appendix 2: Dummy tables .................................................................................................... 30 10. Appendix 3: Consent to participate ....................................................................................... 37 2 TITLE: A REVIEW OF CAESAREAN SECTION RATES, INDICATIONS AND OUTCOMES AT MP SHAH HOSPITAL - NAIROBI. PRINCIPAL INVESTIGATOR: Signed…………………………………Date…………………………….. DR. JAHONGA K.R., MBCHB DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY UNIVERSITY OF NAIROBI. SUPERVISORS DR. OYIEKE J.B., MB. CHB; MMED O/G NBI DIP. FERTIL. CONTROL SENIOR LECTURER AND CONSULTANT DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY UNIVERSITY OF NAIROBI. Signed……………………………….Date……………………………… DR. NDAVI P., MBCHB; MMED O/G NBI MSC. EPID (LOND.) DLSHTM SENIOR LECTURER AND CONSULTANT DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY UNIVERSITY OF NAIROBI. Signed……………………………..Date…………………………………... PROF. C.S. KIGONDU, PhD., F.I.R.S.T. SENIOR RESEARCH FELLOW DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY UNIVERSITY OF NAIROBI. Signed……………………………..Date…………………………………… PART FULLFILMENT OF THE DEGREE OF MMED IN OBSTETRICS AND GYNAECOLOGY. 3 LIST OF ABBREVIATIONS Definition of study concepts: 1. Still births: None of the signs of life are present at death, delivery 2. Neonatal death: Death of a live-born infant during the first 28 days after birth. This term is used in reference to the deaths that occurred before discharge from hospital since patients were not followed up after discharge. Perinatal deaths: Sum of still births plus 7 day neonatal deaths. 3. 4. Early perinatal death is the sum of still births plus neonatal deaths occurring 1st 24 hours. 5. Perinatal case fatality rate: Perinatal deaths per 1000 cesarean sections. 6. Maternal case fatality rate: Number of mothers who died having been delivered by caesarean section per 1000 caesarean section deliveries. 7. Perinatal morbidity will be defined as chart reference to 5 minute Apgar score of less than 7, incubation of infant, incubator care. A Correct 5 minute Apgar score will exclude fetus with gross malformations and extreme prematurity. 8. Gestational age at time of delivery will be defined by the number of completed weeks, based on Magael's rule. 9. Indication for caesarean section will be defined as chart reference to the indication/diagnosis: these will later be classified. 10. Caesarean section will be defined as delivery of an infant of 500gms or more through an incision of the anterior abdominal wall and the uterus. 11. Fetal distress will be diagnosed if only "fetal distress will be diagnosed if only "fetal distress" appears on the chart and validated by presence of meconium and FHR patterns 12. All multiple diagnosis deliveries in which one of the diagnosis is a previous caesarean section birth will be classified as "previous cesarean birth". 13. Cases having breech presentation with any other diagnosis will be assigned "breech". 14. Cases having diagnosis of dystocia and fetal distress will be assigned the class of "dystocia". This recognizes that dystocia can cause fetal distress. 4 Definition of study concepts: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Still births: None of the signs of life are present at delivery Neonatal death will be defined as death of a live-born infant during the first 28 days after birth. This term will be used in reference to the deaths that occurred before discharge from hospital since patients were not followed up after discharge. Perinatal deaths will be defined as sum of stillbirths plus 7-day neonatal deaths. Early perinatal death is the sum of stillbirths plus neonatal deaths occurring 1st 24 hours. Perinatal case fatality rate will be defined as perinatal deaths per 1000 cesarean sections. Maternal case fatality rate will be defined as number of mothers who died having been delivered by caesarean section per 1000 caesarean section deliveries. Perinatal morbidity will be defined as chart reference to 5 minute Apgar score of less than 7, incubation of infant, incubator care. A Correct 5 minute Apgar score will exclude fetus with gross malformations and extreme prematurity. Gestational age at time of delivery will be defined by the number of completed weeks, based on Nagael's rule. < 999 extremely low birth weight 1000 – 1499 very low birth weight 1500 – 2499 low birth weight Indication for caesarean section will be defined as chart reference to the indication/diagnosis: these will later be classified. Caesarean section will be defined as delivery of an infant of 500 grammes or more through an incision of the anterior abdominal wall and the uterus. Fetal distress will be diagnosed if only "fetal distress will be diagnosed if only "fetal distress" appears on the chart and validated by presence of meconium and FHR patterns All multiple diagnosis deliveries in which one of the diagnoses is a previous caesarean section birth will be classified as "previous cesarean birth". Cases having breech presentation with any other diagnosis will be assigned "breech". Cases having diagnosis of dystocia and fetal distress will be assigned the class of "dystocia". This recognizes that dystocia can cause fetal distress. 5 ABSTRACT This will be a descriptive retrospective cross-sectional study. The overall objective is to determine the caesarean section rates, indications and outcomes of cesarean section deliveries, in relation to demographic, obstetric and intrapartum factors. The study will involve all women delivered by caesarean section at M.P. Shah Hospital, a private hospital in Nairobi for the period 1st January 1998 and 31st December 1998. Most studies in Kenya have involved government hospitals. A structured questionnaire will be used in data collection. The investigator will seek a room from the hospital administration in order to facilitate the study. Apart form presenting the work as dissertation for M.Med thesis by the principle investigator, data obtained will be used to give recommendations on health care to policy makers. The study intends to compare findings with those of similar studies done locally. 6 BACKGROUND AND LITERATURE REVIEW Cesarean section is one of the commonest hospital based surgical procedures and its rate has been rising worldwide. it has been defined as the delivery of a fetus, placental and membranes through an incision in the abdominal and uterine walls (1). This term does not derive from the birth of Julius Caesar, as is popularly thought. From the inception as a postmortem procedure under the Roman law, Lex Cesarean (2) it has undergone refinements in technique aimed at modifying the risk of maternal morbidity and mortality which was pervasive. The low transverse incision by Kerr (9) is now popularly used as it also allows the possibility of vaginal birth after cesarean section in contrast to the classical incision which only allowed a repeat caesarean section delivery. The concept of vaginal birth after cesarean was proposed in the early 60s; however, it is only in the mid 1980s that it become popular; thus curtailing the upward spiral in cesarean section rates. Infact it is safe and has a high success rate of more than 60Valid %% of the trials of labour (10,23,24). Patients' role in demand for cesarean section is recognized to affect gains achieved by practise of trials of labour in previous cesarean. However, such an indication has not been documented in local studies. TRENDS IN CESAREAN SECTION RATES The trend world wide is that caesarean section rates are rising. Data summarizes the changes from 1965 to 1985 indicate an increase in the overall caesarean birth rate from 4.5Valid %% to 23Valid %% (10). However, some centres maintained a stable rate at less than 5Valid %% over the same period of time, without adverse perinatal or maternal outcome (12). Mati found a rate of 6Valid %% for Nairobi in the Nairobi birth survey (59). This study showed a higher rate of 13Valid %% for private hospitals, compared to the teaching hospital 6Valid %%. Currently, the cesarean section rate in the USA, Brazil and Chile is 25Valid %%, 40Valid %% and 37Valid %% respectively (39). In Kenya, caesarean section rate has varied with time, place and type of institution. Kenyatta National Teaching and Referral Hospital handling mainly high risk cases has maintained a rate of about 20Valid %% over a period of 17 years between 1975 and 1992 (13,14,15,72). However, this rate has almost doubled to about 42Valid %% currently (77). Pumwani Maternity Hospital, Nairobi, has had a rate of 4.3Valid %% 1983 (16) and 6.8Valid %% 1990 (17). Latest reports show it is currently at 10Valid %% (84). Similarly, low rates have been found in other centres. Kericho District Hospital, 1991 had a rate of 8.23Valid %% (18), Coast General Hospital has had a rate of 7.1Valid %% 1990 (19) and recently 6.7Valid %% 1996 (81). Nairobi Hospital has had a relatively high rate of 28.2Valid %% for the period 1995-1997 (20). Reasons for rise in caesarean section deliveries as As demonstrated by Henens et al (21) different factors have contributed to the rise in caesarean section deliveries and have varied with time, place, type of institution, policy of institution, technological advancement, qualification of personnel, mode of management of labour, social, demographic and economic factors, while consumer pressure, fear of litigation are increasingly becoming more important (24). The latter apply more so in private institutions. Availability of effective antibiotics, safe blood banking services, anaesthesia and improved technique and materials for performing caesarean section. Limited family size as a result of family planning methods has given way to demand for quality survival. The impact of demographic shifts has seen more women having their first birth at advanced maternal 7 age, which has been shown to be associated with antenatal and intrapartum complications necessitating caesarean section delivery (19,21,22). In the U.S.A, the number of patients having their first birth at age of at least 30 years has risen from 20 to 25 percent (22). The socio-economic status of the patient has had a significant role. Patients who have medical insurance compared to non-insured; cared for by obstetricians compared to low cadre health provider; private compared to clinic patient is more likely to have a cesarean delivery (14b). Hence, poor economic incentive to the obstetrician is associated with low cesarean section rate (40b). It has been found that the informed patient and or her spouse are likely to discuss labour with their physician and request or demand for cesarean section (74). `Fear' of undergoing natural birth or fear of perineal disruption with consequent impaired sexual function is known to be prevalent in Brazil, accounting for its high caesarean section rate (39). The role of litigation in caesarean delivery had not been documented locally. In the U.S.A. 70Valid %% of obstetricians have had litigation against them. It is thought that these are more likely to deliver by caesarean section (74) impacting on such chart diagnosis as fetal distress or dystocia. The role of HIV is likely to impact on caesarean section rates. It is estimated that worldwide, about 2.3 million HIV infected women give birth yearly. It is thought that elective caesarean section can reduce perinatal vertical transmission (80). CLINICAL INDICATIONS There is hardly any obstetrical condition that has not been managed by cesarean section. Common indications include repeat caesarean section, fetal distress, malpresentation, dystocia and obstetrical hemorrhage (13-24). Mati et al (59) demonstrated that breech vaginal delivery was associated with very high perinatal mortality rate. In this study, 80Valid %% breeches were delivered vaginally and only 20Valid %% by caesarean section. This led to the policy of caesarean section for all breeches, except for selected cases, hence accounting for increase in caesarean births. In the Nairobi Hospital study, only 3Valid %% of breeches had vaginal birth (20). In his study, Mati showed that breech delivery accounted for 2.7Valid %%, Karanja (13) and Rupani (19) found it to be significant. Repeat caesarean section delivery has been shown to contribute to high caesarean section rate of more than 50Valid %% (13,16,20,59,72) with dystocia and fetal distress as its major complications. Before the advent of vaginal birth after caesarean section, the rates were even higher. Dystocia encompasses multiple diagnosis such as cephalopelvic disproportion, failure to progress, failed induction, prolonged second stage, cervical dystocia and primary uterine inertia. Ojo et al demonstrated that Africans have a disadvantageous narrow pelvis and CPD is significantly a feature (45). In the absence of CPD, active management of labour by early amniotomy and use of syntocinon is an alternative to caesarean section (12). Other proposed alternatives to caesarean section include vaginal birth after caesarean section. Walton reported a success rate of 68Valid %% for Kenyatta National Hospital (72). In some center, use of prostaglandin and syntocinon augmentation have raised success rates. Most caesarean sections are performed as emergency procedures with an elective rate of less than 4Valid %% (15,18,19,81). However, Nairobi Hospital had an elective procedure rate of about 40Valid %%. Elective, compare to emergency cesarean section is associated with lower maternal mortality; however, latrogenic prematurity can be an outward effect. The low transverse incision is commonly used (13,18,19). It allows possibility of subsequent vaginal birth. However, the Kronig (8) incision has been used in conditions where the lower segment is not well 8 formed such as preterm breech delivery. Other types of incision include the classical incision. Karanja (13) and Rupani (19) reported a classical rate of 4Valid %% mainly for extensive adhesions from previous caesarean section delivery. General anesthesia is more commonly used in caesarean section deliveries (13,18,19,76), compared to regional anesthesia; it is associated with more complications. In his study, Kaihura (76) demonstrated that there was less morbidity associated with on of spinal anesthesia compared to general anesthesia. Benefits of caesarean section in reducing perinatal, maternal morbidity and mortality are well documented (10,11,12). Kenya has a maternal mortality ratio of 365/100,000 births (82) and it is thought that cesarean section could have prevented 25Valid %% of such deaths especially in rural areas where the procedure is underutilized (83). However, it has been argued that a decrease in perinatal mortality is still possible in spite of low caesarean section rate if active management of labour is practiced (12) and when there is an overall improvement in obstetrical and perinatal care. Other workers have also shown that in spite of rise in rates for fetal distress, there has been no noticeable decrease in cerebral palsy (41) while in 50Valid %% of cerebral palsy cases there is no evidence of birth asphyxia (42) and there is considerable evidence that the majority of damaged new born are injured prior to labour (43). Maternal morbidity and mortality following caesarean section vary greatly from series to series, but are consistency high than following vaginal delivery (26,44) both in developed and developing countries (45,48,49). This is partly due to the surgical procedure itself and other complications that require the operation. Risk factors for morbidity and mortality include unbooked status, emergency compared to elective procedure, use of GA, anemia, dehydration, duration of labour, repeated vaginal examinations. RATIONALE Cesarean section is a common hospital based procedure whose rate is rising worldwide, causing concern. There is need to periodically determine the rates, trends, indications, fetal and maternal outcomes as they relate to socio-demographic changes and institutional policies and to have a national consensus and audit system, which evaluate patient management and make contribution to national policy guidelines. This is particularly needful in Kenya to assess quality of health care and improve on it; the young population in Kenya with its high dependency ratio and HIV prevalence will impact much cesarean section as a service. Caesarean section is an instrument that is useful in halting vertical HIV transmission. The government is putting in place measures to alleviate poverty; it would be interesting to see how this impacts on cesarean section in Kenya. Low caesarean section rates in some parts of Kenya are not necessarily associated with good perinatal outcome. Hence the need for periodic evaluation of cesarean section rates with regard to demographic shifts, education, and family size among others. This will go a long way to assist policy makers to make effective health management systems. The safe motherhood programme advocates that each hospital publish its vital statistics, which include cesarean birth rates, maternal mortality and morbidity. There is need to understand complications that arise in regard to cesarean section delivery even in "good settings" like private hospitals in Kenya. This can help create a basis of standards. So far, few studies have been done in private institutions (which are of higher socio-economic status) and it is of interest to compare performance in these institutions with teaching and public hospitals (of generally low socioeconomic status). Private hospital patients are likely to be managed by obstetricians, have a high proportion of old nulliparous mothers, be of high education and socio-economic status, and are better informed and likely to request caesarean section. 9 OBJECTIVES BROAD OBJECTIVES To determine the caesarean section rates, indications, maternal and fetal outcomes at a private hospital in Nairobi. SPECIFIC OBJECTIVES 1. To determine the sociodemographic characteristics of patients who underwent caesarean section at MP Shah 2. To determine caesarean section rate at MP Shah Hospital over a period of one year 3. To determine the indications for caesarean section 4. To determine proportion of mothers who request for cesarean section 5. To determine the perinatal and maternal outcomes among patients who underwent caesarean section 6. To determine the relationship between indications for caesarean section and sociodemographic characteristics 7. To determine proportion of mothers who underwent BTL 8. To determine the proportion of mothers who are HIV 9. To recommend ways of reducing cesarean section rates, maternal and fetal morbidity and mortality. 10. To determine decision to incision time METHODOLOGY Study Design. This will be a retrospective descriptive study. Study area. The study will be conducted at MP Shah Hospital. Study period. 1st January 1998 to 31st December 1998 inclusive. However, this will depend on the duration it takes to achieve the desired sample size of 400 caesarean section cases. Study population. This will comprise all patients delivered by cesarean section at MP Shah Hospital during the period 1st January 1998 to 31st December 1998. Sample size determination The expected repeat caesarean section rate is approximately 50Valid %%. Accuracy is desired at 0.05 level. Z statistic is 1.96. The desired sample size n, will be calculated as follows N = Z2P(1 – P)/D2 Where N = minimum sample size to be determined P = expected caesarean section rate at 50Valid %% D = precision / reliability with which to determine P taken as 0.05 for 95Valid %% confidence limit Z = standard errors from the mean corresponding to 95Valid %% confidence level taken 1.96 The calculated sample size was therefore N = [(1.96)2x 0.5 (1- 0.5)]/0.052 10 N = 384 Therefore 400 cases will be used. This will be a convenient sampling procedure involving all women delivered by caesarean section during study period. Inclusion criteria 1. 2. For the purpose of calculating the caesarean section rates, all women who delivered during the study period will be included in the study to get the denominator. All women who delivered by caesarean section during the study period will be analysed. Exclusion criteria Laparotomies for rupture uterus and abdominal pregnancies; and pregnancies less than 28 weeks. Study instruments. This will consist of a questionnaire which will have closed and open-ended questions. It will have several parts. A. Demographic and general data B. Past obstetrical history C. History of index pregnancy D. Labour and operative E. Indication for cesarean section F. Fetal outcome G. Maternal outcome. DATA COLLECTION All patients admitted in the maternity ward of MP Shah Hospital and subsequently delivered by cesarean section during the study period (1st January 1998 to 31st December 1998) will form the study population. The names and file numbers of all the patients who delivered at the unit during the study period will be sought by use of the hospital birth register. This will be retrieved with the help of the records clerk. The files will be coded according to sequence of occurrence in register. Data will be extracted from the files and filled in precoded questionnaire by the principle investigator. Pretesting of questionnaire will be done to determine the suitability. An office will be sought for data collection from the administration. A clerical officer from the hospital will help in file retrieval. The names and file numbers of all patients who delivered at MP Shah Hospital for the period 1st January 1998 to 31st December 1998 will be sought from the birth register in the Maternity Unit, to determine their ages and mode of delivery. The proportion of those who delivered by caesarean section will give he caesarean section rate for the hospital. The age specific cesarian section rate will be calculated by determining the proportion of cesarean births for any specific age group. However, for this study, the files of all mothers who delivered by caesarean section will be sought and coded. A prepared questionnaire will be filled by the principal investigator using data extracted from the files. This will include maternal age, parity, indication of caesarean section, gestational age (completed weeks) calculated from LMP using Magaele's rule). Apgar score, weight in grammes at delivery, sex, maternal morbidity. Study concepts have been defined (see appendix on page 16). Pretesting of the questionnaire will be done on 20 files to determine the suitability and modification made accordingly. A retrieval rate of 95Valid %% is expected. Data management Data from the precoded questionnaire will be cleaned and entered into a computer program with the help of a qualified statistician. Data analysis 11 Frequency tables will be used to look for outliers. Cross tabulation will be done in accordance to the specific objectives in order to determine relationships. Differences will be tested using chi-square method at 95Valid %% confidence limit. A P value of < 0.05 will be considered statistically significant. Ethical considerations Approval to conduct the study will be sought from my the M.P. Shah hospital Board and Ethical Committee. Information obtained will be held in confidence. Study period Study constraints. It is anticipated that file retrieval may not be 100 percent. Clinical documents of a diagnosis may be vague. A single delivery may be associated with two or more indications for example one previous scar and fetal distress. Multiple diagnosis for example previous caesarean delivery and fetal distress will be classified under "previous scar" according to the model of Anderson et al (10). 12 COMPARISON OF RATES AND OUTCOME IN DIFFERENT REGIONS IN KENYA Nairobi hospital 28.2 35.5 40.5 -12.7% 13.5 -- Kenyatta Pumwani Chogoria Coast Kericho 18 50 49.5 4.3 10.3 46.1 25.5 7.1 27.5 3 8.2 20.5 6.25 -- 12.5 15/1000 76.8/1000 36.4 91.8 142 0.00/ 1.4 6.1 4.83 9.6 Maternal morbidity -(febrile) Primigravida 37.8 17.3 20.4 13 26.8 -- 26.3 30.8 36.6 Elective sterilization 22 -- 10.6 11.6 7.5 -- 19 74 10 Age ≥ 35 Age specific C/S rate for 28.9 primigravida Breech C/S 10 -- 9.1 6 6 -- -- 7.4 -- 6.8 15.2 -- 5.4 Classical C/S -- 4 4 3.6 Commonest indication Repeat C/S Repeat FD FD C/S rate Repeat C/S Elective C/S Prematurity Low birth wt Asphyxia Perinatal Mortality Maternal mortality Hospital duration ≥ days 8 Not clear 10.4 10.4 8.9 C/S 13 28.65 Repeat C/S Dystocia FD FD 2.4 6.7 Dystocia Repeat CS Coast 79 C/S rate Repeat C/S Elective 6.7 4.9 4.7 Pumwani S.K. 6.8 36 -- Prematurity Low birth wt Asphyxia ---- ---- Perinatal mortality/1000 Maternal mortality/1000 89 118 8.3 6.3 MP Shah Muriu Nairobi Birth Survey 20 42 -- 6.6 26 -14.3 16.9*1 minute Maternal morbidity 18 (febrile) Primigravida 50.6 19 36 25 Elective sterilization 6.5 -- -- 6.0 5.5 8.7 -- -- -- 60 30 1.1 0.6 11.9 Classical 18 -- 1 Commonest indication Dystocia FD Dystocia Repeat FD Age specific C/S rate for -days Breech C/S 28.9 14 13 C/S WORK PLAN TIME FRAME (MONTHS) ACTIVITIES 1 2 3 4 5 6 Proposal writing and Submission to ERB 2000 Data collection, entry, analysis and Report writing 2005 BUDGET Item 1. Literatures search, stationery, duplicating, photocopies 2. Proposal, typing and duplicating 3. Questionnaires, typing and duplicating 4. Payments to ethical committee for proposal reading 5. Traveling and lunch 6. Communication cost (mobile, telephone) 7. Payments to assistants for data collection 8. Data management, Cleaning, Entry, Analysis 9. Report typing and duplicating 10. Report binding 11. Sub-total 12. Contingency at 10 Valid %%. 13. TOTAL 14. Average cost 15. FUNDING: 15 Amount (Kshs) 10 000 5 000 10, 000 1 000 10000 5,000 10 000 6 000 4 000 2 000 75 000 7,500 82,000 85,000 MOH APPENDIX 1: QUESTIONNAIRE FOR CAESAREAN SECTION STUDY 1. Patient’s study number: 2. Patient file number SOCIODEMORGRAPHIC CHARACTERISTICS 3. Nationality............................................................................ 4. Age (in completed years) 5. Marital status 1. = Single 2. = Married 3. = Cohabiting 4. = Divorced/separated 5. = Widow 6. Occupation.......................................................................... 7. Religion 1. = Protestant 2. = Catholic 3. = Islam 4 = Hindu 5 = Other 6 = Missing PAST OBSTETRIC HISTORY 8. Parity 9. Abortions 10. Number of living children 11. Any still births? 1. Yes 2. No 12. Any neonatal deaths? 1. Yes 2. No 13. Previous caesarean section delivery stating number 1. None 2. 1 3. 2 4. 3 5. 4 or more FOR INDEX PREGNANCY 14. LMP day month 16 year 15. Gestation at delivery (include ultrasound dating whose LMP is not known) 16. Any antenatal complications? 1. None 2. Hypertensive disease 3. Diabetes mellitus 4. Anaemia 5. Infection e.g. malaria 6. Multiple Pg 7. APH 8. Malpresentation 9. Cervical incompetence 10. Others (specify) -------------------------------------------------------------------------------------------------LABOUR AND OPERATIVE 17. Date of admission 18. Date of discharge 19. Duration of stay in hospital (days) 20. Was she in labour? 1. Yes 2. No 21. If not in labour, was she induced? 1. Yes 2. No 22. If yes to question 21, what was the reason for induction? ....................................................................................................................................................................................... 23. Indication for caesarean section 1. Repeat C/S 2. Malpresentation/malposition 3. Fetal distress 4. Dystocia 5. APH 6. PET 7. Myomectomy/fibroids 8. BOH 9. Other (specify)....................................................................................................................................... 17 MATERNAL OUTCOME 1. Maternal death 2. PPH 3. hysterectomy 4. DIC 5. UTI 6. DVT 7. wound infection 8. foreign body 9. burst abdomen 10. febrile illness 11. Others (specify).................................................................................. FETAL OUTCOME 24. Single or multiple births? 1. Single 2. Multiple 25. Outcome of delivery 1. Live birth 2. FSB 3. MSB 4. Neonatal death 26. Neonatal Sex 1. Male 2. Female 27. Apgar score at 5 minutes 1. ≥ 7 2. 1 – 6 3. 0 28. If neonatal death, what was the cause of death? ................................................................................................................................................................................... 29. If neonatal death, what was the age at death 1. 0 – 24 hrs 2. 1 – 6 days 3. 1 – 4 weeks 30. Any congenital malformation 1. Yes 2. No 31. If yes to Q30, state type of malformation ------------------------------------------------------------------------------------------------------- 18 APPENDIX 2: DUMMY TABLES Table 1: Sociodemographic characteristics Characteristic 1. Nationality Kenyan Non Kenyan 2. Age 15 - 19 20 - 24 25 - 29 30 - 34 35 - 39 ≥ 40 3. Marital status Single Married Widow Divorced 4. Religion Protestant Catholic Muslim Hindu Other 5. Occupation Professional Business Housewife Student Booking status Yes No Freq Valid % Table 2: Distribution by mode of delivery Mode of delivery Freq Valid % SVD C/S Vacuum Breech vaginal delivery Total number of births Caesarean section rate*** Cesarean section rate = (Total number of caesarean section deliveries x 100)/total number of births Therefore caesarean section rate is _________________________ 19 Table 3: Summary of Means Characteristic Birth weight Age(years) Gestational age in weeks Duration of hospital stay (days) Duration decision-incision(hrs) Mean 3085.595 30.360 38.218 5.818 88.472 SD 680.728 5.111 2.358 3.160 125.924 median 3150.00 30.000 39.000 5.000 60.000 Max 5250.000 45.000 44.000 30.000 1200.000 Table 4: Previous obstetric performance Characteristic 1. Parity 0 1–2 3–4 ≥5 2. Still births None 1 2 or more 3. Neonatal deaths None 1 2 or more 4. Previous abortion None 1 2 or more 5. Previous c/s None 1 2 3 4 or more Freq Valid % Table 5: Antenatal complications Characteristics Freq. None Hypertensive disease Diabetes mellitus Anemia Infections e.g. malaria Multiple pregnancy APH Malpresentation/malposition Cervical incompetence Others Valid % 20 Minimum 450.000 16.000 26.000 0.000 0.200 Mode 3200.000 30.000 38.000 5.000 60.000 Table 6: HIV status Characteristics Negative Positive Frequency 66 9 Valid percent 88.0 12.0 Table 7: Timing of caesarean section Characteristics Elective Emergency Frequency 218 270 Valid Percent 44.7 55.3 Frequency 295 144 48 11 1 Valid Percent 59.1 28.9 9.6 2.2 0.2 Table 8: Rank of C/section Characteristics 0 1 2 3 4 Table 9: Time between decisions to incision Characteristics <= 30 min >= 30 min – 1 hr >1 hr – 1.5 hr >1.5 hr – 2 hr >2 hr – 3 hr >3 hr – 4 hr > 4 hr Elective Frequency 19 97 61 25 8 5 7 183 valid percent 4.7 24.0 15.1 6.2 2.0 1.2 1.7 45.2 Table 10: Overall indication of caesarean section Indication Freq Repeat caesarean section Malpresentation/malposition Fetal distress Dystocia APH PET Myomectomy/fibroids BOH HIV other **request for caesarean section 21 Valid % Table 11: Commonest indications for primary caesarean section Freq Percentage Dystocia Fetal distress Breech APH Request BOH Others Table 12: Indications for repeat caesarean section (one previous scar) Indication Elective Freq Emergency Valid % Freq Dystocia Fetal distress Breech presentation APH BOH Request HIV Other Table 13: Proportion of BTL between elective and emergency procedure Characteristic Freq Valid % Elective C/S+BTL Emergency C/S+BTL 22 Valid % Table 14: Caesarean section indication by timing: elective or emergency. Indications Elective Freq Emergency Valid % Repeat cesarean Dystocia Fetal distress Breech APH BOH Request Other OUTCOME OF DELIVERY DISTRIBUTION BY BIRTHWEIGHT Table 15: Distribution by Gestational age Gestational age Freq Valid % < 31 31-36 37-42 > 42 Proportion of prematurity = Table 16: Distribution by Birth weight Birth weight Freq Valid % <1000 1000 – 1499 1500 – 2499 2500-3999 > 4000 Total Proportion of term low birth weight = 23 Freq Valid % Table 17: Sex distribution Sex Freq Valid % Male Female Male: Female ratio = Table 18: Distribution of Apgar score at 5 min Apgar score Freq Valid % ≥ 7 1–6 0 Table 19: Outcome of delivery Outcome Live FSB MSB Table 20: Causes of neonatal morbidity Cause Freq Asphyxia prematurity Congenital malformation Malpresentation Iatrogenic Neonatal sepsis Jaundice Other Total Valid % Table 21: Type of congenital malformation Type Cardiac Neural tubes Downs syndrome Limb defects GIT Genito urinary Other Total Table 22: Causes of neonatal death Asphyxia Prematurity LBW RDS Lung malformations Other 24 Table 23: Distribution of perinatal deaths by indication and gestational age Characteristic NND FSB MSB Gestational age (wks) <31 31 – 36 37 – 41 ≥ 42 Birth weight <1000 1000 – 1499 1500 – 2499 2500 – 3599 ≥ 4000 Timing of C/S Elective Emergency Indication of C/S Primary C/S Repeat C/S HIV status Negative Positive Medical illness pregnancy (PET) Yes No in Cesarean section perinatal mortality rate = Timing of C/S Alive Freq Valid% NND Freq Valid% Elective Emergency 25 SB Freq Valid% Table 24: Neonatal Outcome versus timing of caesarean section Table 25: Maternal morbidity (non febrile) Morbidity Elective Freq Emergency Valid % Freq Valid% Blood transfusion ICU/HDU admission Cesarean hysterectomy Post C/S laparotomy Burst abdomen Other Table 26: Analysis of indications associated with major (non febrile) morbidity. Cause death of maternal Indications Parity Age of C/S Elective Table 27: Duration in hospital following cesarean section Number of days Freq Valid % ≤7 8-10 11-14 ≥ 15 26 Emergency REFERENCES. 1. Zuspan F.P. and Quilligan E.S. Douglas-Stromme operative obstetrics Ch. 16 pp 473 5th edition, 1988 Appleton and Lange 2. Hibbard T.L. Caesarean section in: Obstetric: Normal and problem pregnancies Chapter 17 Appleton and Lange. 3. 4. Ralph W. Hale. Current: Obstetrics and Gynecologic diagnosis and treatment Chapter 27 pp 560 8th edition Appleton and Lange. 5. Porro E. Della amputazione utero-ovariaca. 299 Milan, 1876. 6. Sanger M. My wong in reference to cesarean operation Am. J. Obstet Dis Women Child 20:593, 1887. 7. Frank F. Suprasymphila delivery and its relation to other operations in the presence of contracted pelvis Arch. Gynaecol 81:46, 1907. 8. Kronig B. Transperitonealer cervikaler Kaiserschnitt. p. 879. In poderlain A., Kronig B. (eds): Operative gynakologie, 1912. 9. Kerr J.M.M. The technique of cesarean section with special reference to the lower uterine segment incision Am. J. Obstet Gynecal 12: 729, 1926. 10. Anderson G.M., Lomas J. Determinants of the increasing cesarean birth rate. M Engl J. Med. 311:887, 1984. 27 11. Motzon F.C., Placek P.J., Tastel SM. Comparisons of national cesarean section rates M. Engl. J. Med 316: 386, 1987. 12. O'Driscall K., Foley M. Correlation of decrease in perinatal mortality and increase in cesarean section rate Obstet Gynecol 61: 1, 1983. 13. Karanja J.G. A review of caesarean section deliveries at the Kenyatta National Hospital in 1980 M.Med thesis, University of Nairobi, 1981. 14. Wanjohi E.M. Risk factors associated with wound infection after cesarean section at Kenyatta National Hospital M.Med thesis, U.O.N, 1989. 15. Muriu F.J.K. Caesarean section pattern at the Kenyatta National Hopsital (1989) M.med thesis, U.O.N, 1991. 16. Bansal Y.P. Caesarean sections - Indications and maternal mortality at Pumwani Maternity Hospital, Nairobi (1983) E.A.Med J. 64(11) 741-4, 1987. 17. Karanja S.K. A prospective study on the pattern of caesarean sections at Pumwani Maternity Hospital (1990) M.Med thesis, U.O.N., 1991. 18. Kudoyi W.O. A six months prospective study on the indications and outcome of caesarean sections at Kericho District Hospital (1991) M.Med thesis, U.O.N., 1993. 19. Rupani N.P. A prospective study of caesarean section deliveries at Coast General Provincial Hospital, Mombasa (1990) M.Med thesis, U.O.N., 1991. 20. Martha Okanga Haefler. The Nairobi Hospital caesarean section study II. The Nairobi Hospital proceedings vol. 2:206-233. 21. Leveno K., Cunningham C., Pritchard S. Caesarean section: An answer to the house of horne. Am. J. Obstet Gynecol 153:838, 1985. 28 22. Tastel S.M., Placek P.J., Liss T. Trends in the United States cesarean section rate for the 1980-1985 rise: Am. J. Public Health 77:955, 1987. 23. Riva H., Teech J. Vaginal delivery after cesarean section Am., J. Obstet Gynecol 81:501, 1961. 24. Shiono PA., McMellis D., Rhoads GS. Reasons for the rising cesarean delivery rates 1978-1984. Obstet Gynecol 69:696, 1987. 25. Phelan J.P., Clark SL., Diaz F et al. Vaginal birth after cesarean. Am. J. Obstet Gynecol 20:763, 1985. 26. Amirikia Hassan, Bohdan Z., Evans Tommy. Caesarean section: A 15 year review of changing incidence, indications and risks. Am. J. Obstet Gynaecol 140:81:1981. 27. Tahilnamaney MP., Boucher M., Eglinton G et al. Previous cesarean section and trial of labour: Factors related to uterine dehiscence. J. Reprod. Med 29:17, 1984. 28. Pedoweittz P., Schwartz R.M. The true incidence of silent rupture of cesarean section scars: A prospective analysis of 403 cases. Am. J. Obstet Gynecol 74:1701, 1957. 29. Mowat J., Bonner J. Abdominal wound dehiscence after cesarean. Br. Med, J. 2:256, 1971. 30. Finan MA., Mastrogiannis DS, Spellacy WM. The "Allis" test for easy cesarean delivery. Am. J. Obstet Gynecol 164:772, 1991. 31. Greenspoon JS, Kovacic A. 1991 breech extractions facilitated by glyceryl trinitrate sublingual spray Lancet 338:124-125. 32. Editorial Maternal health in Subsaharan Africa Lancet 1987 1:255-7. 34. In re A.C., 553A 2d 611(D.C. 1987). 35. Kolder E., Gallaghier J., Parsons MT. Court ordered obstetrical interventions. N. Engl. J. Med. 1987; 1192:316. 29 36. Consensus development conference on cesarean childbirth 1980; US Department of Health and Human Services. Public Health Service National Institutes of Health. 37. The future of obstetrics and gynaecology. Chicago: American Medical Association in cooperation with the American College of Obstetricians and Gynaecologists, 1987. 38. A.H. Sultan and S.L. Stanton. Preserving the pelvic floor and perineum during childbirth Elective caesarean section? BMJ 1996; 103:731-734. 39. Willians RL., Harvesiu WE. Cesarean section, fetal monitoring, and perinatal mortality. Am. J. Public Health 69: 874, 1979. 21. Leveno KJ., Cunningham FG., Pritchard JA. Cesarean section: An Answer to the hour of Horne?. Am. J. Obstet Gynecol 153:838, 1985. 40. Richards MPM 1979. Perinatal morbidity and mortality in private obstetric practice. Journal of maternal and child health. September: 341-345. 40b. Shearer E. Preventing unneccesary cesarean: A guide to labour management and detailed bibliography. Framingham, Massachussetes: C/Sec Inc. 1992. 41. Stanley FJ., Blair E. 1991 Why have we failed to reduce the frequency of cerebral palsy? Medical Journal of Australia 154:623-626. 42. Nelson KB., Ellensberg JH. Apgar scores as predictors of chronic neurologic disability Paediatrics 1981: 68(1): 36-44. 43. Rosen GM., Hobel CJ. Prenatal and perinatal factors associated with brain disorders. Obstet Gynecol 1986:68:416-422. Hibbard TL. Caesarean section in: Obstetrics: Normal and problem pregnancies. Chapter 7. 44. 30 45. Ojo VA., Okweneku FO. A critical analysis of the rates and indications for caesarean section in a developing country. Asian-Ocenia J. Obstet. Gynaecol 14(2) 185, 1988. 46. Sinei S.K.A. Post caesarean section febrile morbidity at Kenyatta National Hospital. Bacterial pattern and drug sensitivity M.Med thesis, U.O.N., 1981. 47. Rubin GL., Peterson HB, Rochat RW et al. Cesarean section-related maternal mortality in Massachusetts, 1954-1985. Obstet Gynecol 71: 385, 1988. 48. Adeleye A. Maternal mortality and caesarean section of the U.C.H. Ibadan, Nigeria (A 2 year study) Trop J. Obstet Gynaecol 3:37, 1982. 49. Oyegunle AO. Cesarean section and maternal mortality at LUMH,Nigeria Nig Med J. 6: 201, 1976. 50. E. Tedasse, M. Adane and M. Abiyou. Caesarean section deliveries at Tikur Anbessa Teaching Hospital, Ethiopia. E.A.M.J. 73:9: 1996. 51. Bercovivi B. Use of vacuum extroclu for the head delivery at cesarean section. Isr J. Med Sc. 1980; 16:201-3. 52. Hemminki E. Impact of caesarean section on future pregnancy - a review of cohort studies in the early 60s. National Research and Development Centre for Welfare and Health, Helsinki, Finland. Paediatric and Perinatal Epidemiology 10 (4): 366-79, 1996. 53. Van Roosmalen J. 1988 Maternal health care in South Western Highlands of Tanzania. PhD thesis, University of Leiden, Leiden. 54. Chavhan SP., Roach H., Maef RW 2nd, Magann EF., Morrison JC., Martin JM Jr. Cesarean section for suspected fetal distress. Does the decision-inclusion time make a difference?. Journal of reproductive medicine 42(6): 347-52, 1997. 31 55. Smith JF., Hernandez C., Wax JR. Fetal laceration injury at cesarean delivery. Obstet Gynecol 90: 3:344-6. 56. Stembera Z. How can we prevent a further increase in the rate of cesarean sections in the Czech republic? (Czech) Ceska gyneckologic 60:6: 283-9, 1995. 57. Robson MS., Scudamore IW., Walsh SM. Using the medical audit cycle to reduce cesarean section rates. AMJ. Obset Gynecol 174(1): 199-205, `1996. 58. El tabbakh GH, Watson JD. Post partum hysterectomy. Int. J. Gynaecology and Obstetrics. 50(3): 257-62 1995. 59. Mati J.K.G., Aggrawal V.P., Sanghvi H.C.G., Lucas S., Corkhill R. (1983). The Nairobi Birth Survey III. Labour and delivery. J. Obstet Gynaecol East Cent. Africa 2(2): 47. 60. Chile Murray SF., Serani Pradenas F. Cesarean birth trends in Chile, 1986 to 1994. Birth 24 (4): 258-63, 1997. 61. ACOG technical bulletin. Dystocia and the augmentation of labour, Int. Journal of gynaecology and Obstetrics 53(1): 73-80, 1996. 62. Semprini AE., Castagna C., Ravizzam, Fiore S., Savasi V., Muggiasca ML. Gross E., Guerra B., Tibaldi C., Scaravelli G. et al. The incidence of complications after caesarean section in 156 HIV-positive women. AIPS 9(8): 913-7, 1995. 64. Gerald G.J. et al Vaginal birth after cesarean section. The impact of patient resistance to trial of labour. AMJ. Obs/Gy. 164:1441:1991. 65. De MOH R.K., Scandmire H.F. The physician factor as a determinant of cesarean birth rates. AMJ. Obstet Gynecol 162: 1593-6029 1996. 66. Wilcos C.F. et al. The measurement of blood loss during cesarean section. AMJ Obstet Gynecol 77:772, 1959. 32 67. Nielsen T.F. (1986). Caesarean section: A controversial feature of modern obstetric practice. Gynaecol Obstet Invest 21:57. 68. Kasule J., Gumbon Mason D. J. Obs Gynecol 10:47, `1992. 69. Craig E. Conservatism in obstetrics NY Med J. 1916; 104:1-3. Carlson C., Lybell-Lindahl G., Ingemarsson I. Extradural bloc in patients who have previously undergone cesarean section Br. J. Anaesth 52: 827, 1980. 70. Dewhurst C. The rupture cesarean section Scar. J. Obstet Gynaecol Br. Commonw 1957: 74:113-118. 71. Flamm B. Vaginal birth after cesarean section: Controversies old and new. Clin Obstet Gynecal 1985; 28:4:735-744. 72. Walton S.M. The antenatal and intrapartum management of patients with previous caesarean section scars. E. Afri. Med. J. 55:1, 1978. Walton Trial of vaginal delivery in vertex for PS as .................... 73. Department of Health Changing childbirth part I and II. Report of the expert maternity group. London: HMSU, 1993. 74. Ryding EH. Investigation of 33 women who demanded a cesarean section for personal reasons. Acta. Obstet Gynecol Scand 1993: 72: 280-285. 75. David M. Kaihora A prospective study on the outcome of caesarean sections at Chogoria Hopsital 1996. M.Med Thesis 1997 33 76. Gerald F.J. et al Vaginal birth after caesarean section. The impact of patient resistance to a trial of labour Am. J. Obstet. Gynaecol: 164:1441, 1991. 77. Birth register Labour ward, Kenyatta National Hospital (unpublished). 78. Aga-khan - Nairobi 79. Mater Hospital 80. Laura E. Riley, Michael F. Green Elective caesarean delivery to reduce the transmission of HIV NEJM 340: 1032-1033, 1999. 81. Teckle G. Egziabher A retrospective analysis of caesarean section, incidence, indications and complications at the Coast Provincial General Hospital, Mombasa, Kenya between first of January 1996 and December 1996 M.Med thesis 1998. 82. Ministry of Health 1994 Kenya's health policy framework Government of Kenya. 83. Report on determinants of caesarean section: Kenyan experience. 84. NCC Appendix 3: Letter of Approval from Ethical Committee 34 04.05 05 crude results Sociodemorgraphic. Nationality Kenyan Foreigners Number % 459 38 Total 497 92.3 7.6 3 56 153 171 82 21 Total 486 0.6 11.5 31.4 35.1 16.8 4.3 311 26 162 62.3 5.2 32.4 332 149 12 3 66.9 30 2.4 0.6 Age 15 – 19 20 – 24 25 – 29 30 – 34 35 – 39 40 and above Marital status Married Single Unknown Occupation Professional Housewife Auxiliary Student Religion 35 Distribution by parity Para 0 Para 1 Para 2 Para 3 Para 4 Para 5 Para 6 Para 11 Total Number 145 153 107 48 11 5 4 1 474 % 30.5 32.2 22.5 10.1 2.3 1 0.8 0.2 Caesarean section rate by primary report Number Primary caesarean section 283 Repeat caesarean section 191 Total 474 % 59.7 40.2 100 Distribution of caesarean section by timing Number Emergency caesarean section 215 Elective caesarean section 263 Total 478 % 44.98 53.02 55.02 Distribution of caesarean section by rank Number No previous primary caesarean 283 section 1 previous scar 136 2 previous scar 40 3 previous scar 10 4 previous scars 1 Total 474 % 59.7 28.6 9.2 2.1 0.2 100 36 Overall indication of caesarean section n = 478 Number Repeat caesarean section 191 Malpresentation / malposition 61 Fetal distress 58 Dystocia 65 Obstetric hemorrhage 29 PET/IUGR 24 Myomectomy / fibroids 9 BOH 5 Reduced fetal movements 17 Request 1 ROV 1 Previous uterine perforation 2 Elderly prigravida 2 HIV + 1 Congenital mal 2 HSIL 1 Vaginal cept 1 Spinal injury 1 Indication for primary caesarean section n = 283 Malpresentation/malposition Breech 29 OPP 20 Transverse lie 5 Fake topubes 4 Unstable lie 1 Shoulder Compound 2 Fetal distress 21.56% 58 20.50% Dystocia Contracted pelvis CPP Poor progress Cervical dystocia Failed vacuum Prolonged labor Obstructed labor 4 53 4 2 2 22.97 Obstetric hemorrhage Abruptio placenta Placenta previa Placenta increta APH 16 2 1 1 37 % 40.2 12.76 12.13 13.6 6.07 5.02 1.88 1.05 3.56 0.21 0.21 0.41 0.41 0.21 0.41 0.21 0.21 0.21 ROV 10.25% PET/IUGR eclampsia 12+8+4 Myomectomy/ fibroids 8.48% 5+4 3.18% BOH, reduced FM IPS: Indications n = 136 Malpresentation/ malposition breech OPP Obline Transverse Placenta topuses Unstable lie Fetal distress 7 1 1 1 7.35% 4 2.94% Dystocia CPD Poor progress Dystocia Failed vacuum/forceps Failed trial Contracted pelvis 36 2 1 5 33.83% Obstetric hemorrhage Abruptio Placenta previa Placenta increta ROV Cord prolapse PET /Hypertensive disease Eclampsia IUGR 5 1 1 1 1 5.88% 10 6 2 2 7.35% Myomectomy Fibroid Previous uterine perforation 1 1 1 38 BOH 2.21 4 Reduced FM 2.94% 9 Others prom 6.62% 5 Unstated 3.68% 3 22.79% IPS (unqualified) Number = 30 IPS (unqualified) + BTL = 6 39 Time between decision to incision Characteristics <= 30 min >= 30 min – 1 hr >1 hr – 1.5 hr >1.5 hr – 2 hr >2 hr – 3 hr >3 hr – 4 hr > 4 hr Elective Frequency 19 97 61 25 8 5 7 183 valid percent 4.7 24.0 15.1 6.2 2.0 1.2 1.7 45.2 Frequency 443 47 3 Valid percent 89.9 9.5 0.6 Frequency 299 200 Valid percent 59.9 40.1 Apgar score at 5 minutes Characteristics >7 1–7 0 Ever had C/section? Characteristics No Yes Number of previous C/section Characteristics 0 1 2 3 4 Frequency 295 144 48 11 1 Valid Percent 59.1 28.9 9.6 2.2 0.2 Frequency 218 270 Valid Percent 44.7 55.3 Percent 459 1 3 17 2 Valid percent 92.4 0.2 0.6 3.4 0.4 Elective / emergency Characteristics Elective Emergency Nationality Characteristics Kenyan Ugandan Pakistani Indian DR Congo 40 British Somali French Sudanese Zambian Japanese Ethiopian Rwandese 3 6 1 1 1 1 1 1 0.6 1.2 0.2 0.2 0.2 0.2 0.2 0.2 Frequency 311 26 Valid percent 92.3 7.7 Frequency 149 6 16 5 41 12 20 24 15 33 12 14 4 11 73 1 1 3 9 3 3 1 4 1 5 2 4 11 5 3 2 1 Valid percent 30.1 1.2 3.2 1.0 8.3 2.4 4.0 4.8 3.0 6.7 2.4 2.8 0.8 2.2 14.7 0.2 0.2 0.6 1.8 0.6 0.6 0.2 0.8 0.2 1.0 0.4 0.8 2.2 1.0 0.6 0.4 0.2 Marital status Characteristics Married Single Occupation Characteristics Housewife Hair dresser Accountant Sales lady Teacher Doctor Clerk Banker Telephonist Business Scientist Administrator Lecturer Nurse Secretary Insurance broker Librarian Sub. Staff Computer assistant Preacher TV/video producer Loan officer Travel agent Driver Student Valuer Lawyer Operational officer Cashier Textile designer Editor Social worker 41 Cateress 1 0.2 Frequency 256 87 50 21 6 17 1 Valid percent 58.4 19.9 11.4 4.8 1.4 3.9 0.2 Frequency 1 3 Valid percent 0.2 0.6 Frequency 1 2 35 105 141 97 49 23 18 5 4 4 3 1 1 1 4 Valid percent 0.2 0.4 7.1 21.3 28.5 19.6 9.9 4.7 3.6 1.0 0.8 0.8 0.6 0.2 0.2 0.2 0.8 Frequency 4 5 451 3 Valid percent 0.9 1.1 97.4 0.6 Religion Characteristics Protestant Catholic Muslim Hindu Other Christian Orthodox Education Characteristics Primary Tertiary Duration of hospital stay Characteristics 0 1 3 4 5 6 7 8 9 10 11 12 14 18 21 28 30 What was the state? Characteristics Fresh Macerated N/A Not indicated 42 Missing cases Characteristics No Yes Frequency 372 125 Valid percent 74.8 25.2 Frequency 447 52 Valid percent 89.6 10.4 Frequency 498 1 Valid percent 99.8 0.2 Frequency 31 407 Valid percent 7.1 92.9 Frequency 61 424 Valid percent 12.6 87.4 Frequency 240 222 Valid percent 51.9 48.1 Frequency 472 13 Valid percent 97.3 2.7 CSMORE Characteristics No Yes Request Characteristics No Yes Single birth Characteristics No Yes Live birth Characteristics No Yes Sex of child Characteristics Male Female Neonatal death Characteristics No Yes 43 Cause of death Characteristics Apnoec attach Severe asphyxia Perforated uterus Respiratory failure N/A Frequency 1 1 1 1 472 Valid percent 0.2 0.2 0.2 0.2 99.0 Frequency 8 1 473 Valid percent 1.7 0.2 98.1 Frequency 424 65 Valid percent 86.7 13.3 Age at death Characteristics 0 -24 hrs 1 – 4 wks N/A Congenital malformations Characteristics No Yes 44 Congenital malformation specified Characteristics N/A Neural Genitourinary Musculoskeletal Other Circumcised Nauroria Meconium aspiration Jaundice Premature Neural, musculoskeletal Jaundice, sepsis Asphyxia Frequency 424 3 1 8 31 2 1 1 13 1 1 1 1 Valid percent 86.9 0.6 0.2 1.6 6.4 0.4 0.2 0.2 2.7 0.2 0.2 0.2 0.2 Frequency 66 9 Valid percent 88.0 12.0 Frequency 6 15 4 Valid percent 24.0 60.0 16.0 Frequency 13 439 Valid percent 2.9 97.1 Frequency 8 63 380 4 Valid percent 1.8 13.8 83.5 0.9 HIV status if done Characteristics Negative Positive Baby transferred Characteristics Transferred Left behind Intubation Was a patient booked? Characteristics No Yes Gestational age in weeks Characteristics < 31 31 – 36 37 – 42 > 42 45 Table of Means Characteristic Birth weight Age(years) Gestational age in weeks Duration of hospital stay (days) Duration decisionincision(hrs) Mean 3085.595 30.360 38.218 5.818 SD 680.728 5.111 2.358 3.160 median 3150.00 30.000 39.000 5.000 Max 5250.000 45.000 44.000 30.000 88.472 125.924 60.000 1200.000 0.200 46 Minimum 450.000 16.000 26.000 0.000 Mode 3200.000 30.000 38.000 5.000 60.000 wanyonyi RESULTS Duration the period studied were 126,000 deliveries and 276 cases of ruptured giving an incidence of 276:126,000 which is 1:219. The number of cases was obtained from theatre registers. Out of 276 cases only 103 clinical case records could be retrieved for analysis. Table 1: Age distribution of patients with uterine rapture Age 15 – 19 20 – 24 25 – 29 30 – 34 35 – 40 Total Number 5 28 25 19 16 93 Percentage 5.5 30.2 26.9 20.5 17.4 100 The majority of these patients were between 20 – 29 years who accounted for 50% the study subjects. The mean is 27.1 ± 5.9 with minimum being 17 years and maximum being 40 years. Table 2: Parity of patients with uterine rapture Parity Number 0 16 1 30 2–4 52 F5 5 Percentage 15.5 29.1 50.5 4.9 The majority of patients were multiparous with parity ranging between 2 – 4 children who accounted for 50.5%. Para 1+0 accounted for 29.1 and primipara 15.5% while grand multipara was only 4.9%. Table 3: antenatal care attendance and place attendance Number Yes Yes 100(97.1%) Rural health centre 2 City council clinic/PMH 98 Private 1 None 2 Total 103 Percentage No 3 (2.9%) 2.0 97.0 1.0 1.9 100 Antenatal care attendance was 97.1%. Most of them attended Nairobi Council health facilities or PMH antenatal clinic accounting for 97%. Rural health centre 2% and private 1% while those who didn’t attend any were 2 (1.9%) Table 4: Indication for previous scars 47 Indication N/I CPD FD Transverse lie Twins Malpresenation APH Breech Prolonged Big baby BOH Number 16 16 7 4 1 4 1 1 2 4 1 Percentage 28.0 28.0 12.0 7.0 1.7 7.0 1.7 1.7 3.5 7.0 1.7 NI – not indicated, CPD –cephalopelvic disproportion, FD – fetal distress, APH – antepartum hemorrhage, BOH – bad obstetric history. From the results above, it’s clear that most of the cesarean scars done previously were not clearly indicated on the maternal antenatal card and in the file. However, CPD accounted for 18.4% with fetal distress 8.0%, transverse lie 4.6% some with malpresentation and big baby. Twins, APH, Breech and BOH had one each. From the study, it was noted that vaginal operative deliveries were not common in Pumwani Maternity Hospital. There were 2 (2.0%) of two vacuum extraction only. It was also noted that most referrals came from home in labour with 97.8% of patients. Table 5: No of Previous cesarean scars No. of scars Number 0 46 1 44 2 10 3 & over 2 Percentage 45.1 43.1 9.8 2.0 In this study one previous scar accounted for 43%. Two previous scars about 10% while 3 and more had 2% Table 6: Use of Syntocinon Syntocinon Yes No Total Number 36 10 46 Percentage 78.0 22.0 100 46 cases were reviewed, 36 (78%) had been on syntocinon while 10 (22%) didn’t use. Table 7: signs of obstructed labour Signs Yes (%) No (%) 48 Dehydration Vulval oedema Caput Moulding Meconium stained liquor Oedema of bladder 46(50.5) 35(38.5) 73(80.2) 56(61.5) 59(4.8) 70(77.0) 45(49.5) 56(61.5) 18(19.8) 35(38.5) 32(35.2) 21(23.0) Dehydration of the mother was present in 46(50.5). Vulval oedeme was present in 35 (28.5%), marked caput in 73(80.2%), moulding was in 56(61.5%) and meconium stained liquor 59(64.8%), while oedema of the bladder at operation was present in (77.0%) of the cases. Table 8: Symptom/Signs Symptom/signs Lower abdominal pain Vaginal bleeding Tachycardia Hypotension Tenderness lower abdomen Yes (%) 94 (97.9) 63(65.6) 58(60.4) 62(64.4) 94(97.7) No (%) 2 (2.1) 33(34.4) 38(39.6) 34(35.4) 2(2.1) Symptoms and signs for impending or uterine rapture were lower abdominal pain which was present in 94(97.9%), tenderness in lower abdomen (97.9%) vaginal bleeding 63(65.6%) and tachaycardia was 62(64.6%). The fetal heart was present in 61(62.9%) of the patients. Table 9: Type of rapture of uterus Type of rapture Number Impending 1 Spontaneous 46 Previous scar 55 Percentage 1.1 46.1 52.9 The type of rapture involved spontaneous and rapture of previous scar were 46(45.1%) cases of spontaneous rapture and 55(54%) had previous scar. There was one case of impending rapture. Table 10: Site of rapture at operation. Anterior 8 Anterior low segment 81 Posterior 5 Lateral aspect 1 Anterior & Low segment 3 Anterior low segment & 1 posterior Not recorded 3 7.8 79.4 4.9 1.0 2.9 1.0 2.9 The site of rapture had anterior lower segment accounting for the largest number of cases about 80%. Table 11: Extension of uterine ruptures to other structures Extension Number Percentage None 74 72.5 Broad ligament 8 7.8 49 Bladder Cervix & vagina Bladder, cervix & vagina Total 4 15 1 102 3.9 14.7 1.0 100 27.5% of ruptures had tears which extended to neighboring structures. The cervix and vagina was more common accounting for 15%. It was noted one patient had tears involving the bladder, cervix and vagina. Table 12: Type of operation done Operation Number Repair 94 Subtotal hysterectomy 5 Total hysterectomy 2 Repair /subtotal 1 Died 1 Percentage 91.3 4.9 1.1 1.0 1.0 91.3% of patients had repair of uterine rupture while subtotal hysterectomy was about 5% and total hysterectomy was done in 2 patients. One patient died intraoperatively. Table 13 maternal and fetal outcome Maternal/fetal outcome No Mother survived 96 Mother died 7 Still births 42 Neonatal death 4 Alive & Discharge 57 % 93.2 6.8 40.8 3.9 55.3 The maternal outcome at operation found 96(93.2%) survived and 7 (6.8%) died intraoperatively thereafter. The fetal outcome, the number of still births were 42(40.8%), neonatal death 4(3.9%) and alive and discharged 57(55.3%). The duration of stay in hospital was as follows; Table 14: duration of hospital stay in weeks Weeks No <1 7 1- 2 66 2–3 13 >3 10 N/A 7 % 6.8 64.4 12.1 9.7 6.8 73 (70.9%) had a hospital stay of 1 – 2 weeks in hospital. 12.1% had hospital stay of between 2 – 3 weeks while more than 3 weeks were about 10%. 50 Mp shah Objective I During the study period of Jan 1998 –March 2000 a total of 494 cesarean section files were reviewed. There were a total of 2067 deliveries as shown in table 1 Table 1: type of deliveries Type of delivery SVD CS VE Breech Forceps No 1292 596 152 25 2 Percentage (%) 62.5 28.8 7.4 1.2 0.1 There were 596 caesarean section deliveries over the study period, thus the cesarean section rate was calculated as 596/2067 multiplied by 100, giving a rate of 28.83% 494 files were retrieved, thus the file retrieval rate was calculated as 494/596 multiplied by 100, giving a retrieval rate of 82.86%. Booking status 439 patients were booked Not booked 55 Booking rate = 439/494 x 100 = 88.87% Type of CS Elective 153 (30.66%) Emergency 346 (69.34%) Rank of CS Primary CS I Ps More than I Ps Objective 2 Indications for CS? Indication Repeat CS CPP Fetal distress Malpresentation PET Reduced FM APH IUGR No 177 80 80 43 35 21 21 15 % 1% CS 327 (64.53%) Repeat CS 177 (35.47%) Objective 3 There were two CS done on request (case file No.) 51 Objective 4 There were 25 women who had BTL at CS. No Elective Emergency % Objective 6 HIV status among CS patients. In 75 patients, HIV status stated. In 424 patients, status not stated. Of the 75, 66 were negative, 9 were positive. HIV infection rate 9/25 x 100 = 12% (approximately) Indications of CS among positive: janet. Fetal outcomes Single wins Live FSB MSB Apgar score at 5 minutes: >7 388 1–6 41 0 7 Birth weight: <999 1000-1499 1500-1999 2000-2499 2500-2999 3000-3499 3500-3999 3 8 21 40 117 155 52 REPORT WRITING 53 OBSTETRICS LONG COMMENTARY PROJECT TITLE: A REVIEW OF CAESAREAN SECTION RATES INDICATIONS AND OUTCOMES AT MP SHAH HOSPITAL - NAIROBI 54 LIST OF ABBREVIATIONS Definition of study concepts: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Still births: None of the signs of life are present at delivery Neonatal death will be defined as death of a live-born infant during the first 28 days after birth. This term will be used in reference to the deaths that occurred before discharge from hospital since patients were not followed up after discharge. Perinatal deaths will be defined as sum of stillbirths plus 7-day neonatal deaths. Early perinatal death is the sum of stillbirths plus neonatal deaths occurring 1st 24 hours. Perinatal case fatality rate will be defined as perinatal deaths per 1000 cesarean sections. Maternal case fatality rate will be defined as number of mothers who died having been delivered by caesarean section per 1000 caesarean section deliveries. Perinatal morbidity will be defined as chart reference to 5 minute Apgar score of less than 7, incubation of infant, incubator care. A Correct 5 minute Apgar score will exclude fetus with gross malformations and extreme prematurity. Gestational age at time of delivery will be defined by the number of completed weeks, based on Nagael's rule. < 999 extremely low birth weight 1000 – 1499 very low birth weight 1500 – 2499 low birth weight Indication for caesarean section will be defined as chart reference to the indication/diagnosis: these will later be classified. Caesarean section will be defined as delivery of an infant of 500 grammes or more through an incision of the anterior abdominal wall and the uterus. Fetal distress will be diagnosed if only "fetal distress will be diagnosed if only "fetal distress" appears on the chart and validated by presence of meconium and FHR patterns All multiple diagnosis deliveries in which one of the diagnoses is a previous caesarean section birth will be classified as "previous cesarean birth". Cases having breech presentation with any other diagnosis will be assigned "breech". Cases having diagnosis of dystocia and fetal distress will be assigned the class of "dystocia". This recognizes that dystocia can cause fetal distress. 55 ABSTRACT Background: Cesarean section is the commonest hospital based-operation whose rate is rising worldwide. The rates and trends depend on medical, socioeconomic factors, education and indications such as request for cesarean section, even in the absence of a medical indication. MP Shah Hospital is private hospital in Nairobi, where socioeconomic status of the population is high, and that patients are more informed and are likely to demand for cesarean section. The study involved all women delivered by caesarean section at M.P. Shah Hospital, for the period 1st January 1998 and March 2000. Most studies in Kenya have involved government hospitals. Objective: to determine the cesarean rates, indications and outcomes in a private hospital Study site: MP Shah Hospital Study design: This was descriptive cross- sectional retrospective analytical study. Study methodology: A pre- tested structured questionnaire was used by the principle investigator to abstract information from case files. Results were computed and analyzed using SPSS version 10.0 Results The majority (92.3%) was Kenyans and 97% had booked to deliver at the hospital. The mean age of the population was 30.4± 5 years, adolescents comprising 12%. 62.3% were married and 66% were in professional employment. The cesarean section rate was 28%, of which 55.3% were emergencies. For emergencies the decision- to-incision time was less than an hour in 52% of the cases. The commonest indications were repeat cesarean section (40%), dystocia 13.6% malposition or malpresentation 12.8% and fetal distress 12.1%. Only two cases requested for cesarean section. 36% had antenatal complications with PET comprising 60% of the complications. The HIV status was documented in only 66 (13.2%) cases, of which 9 (12%) were positive. One HIV case had an elective cesarean section. 13.2% of the population had surgical sterilization. 15 (3%) were multiple births. The mean gestational age at cesarean section was 38.2 weeks± 2.6 weeks with 15.6% being preterm infants. The mean birth weight was 3086 gm ±680 gm with 15% being low birth weight. There were 8 stillbirths and 7 neonatal deaths. Asphyxia occurred in 44 (8.9%) of the cases, of whom 6 were transferred to another hospital for intensive care. There was one term neonatal death with multiple congenital anomalies, the rest were due to extreme prematurity. During the study period there were no maternal deaths. Maternal morbidity occurred in 18.8% with prolonged hospital duration being commonest cause. Two cases were admitted to ICU with DIC associated with eclampsia, and two were admitted in HDU due to poor reversal. Most cases (87%) were discharged within one week of admission. Conclusion Caesarean section rate is high. Cases of request for CS are negligible. Recommendation 56 INTRODUCTION BACKGROUND AND LITERATURE REVIEW Cesarean section is one of the commonest hospital based surgical procedures and its rate has been rising worldwide. it has been defined as the delivery of a fetus, placental and membranes through an incision in the abdominal and uterine walls (1). This term does not derive from the birth of Julius Caesar, as is popularly thought. From the inception as a postmortem procedure under the Roman law, Lex Cesarean (2) it has undergone refinements in technique aimed at modifying the risk of maternal morbidity and mortality which was pervasive. The low transverse incision by Kerr (9) is now popularly used as it also allows the possibility of vaginal birth after cesarean section in contrast to the classical incision which only allowed a repeat caesarean section delivery. The concept of vaginal birth after cesarean was proposed in the early 60s, however, it is only in the mid 1980s that it become popular; thus curtailing the upward spiral in cesarean section rates. In fact it is safe and has a high success rate of more than 60% of the trials of labour (10,23,24). Patients' role in demand for cesarean section is recognized to affect gains achieved by practise of trials of labour in previous cesarean. However, such an indication has not been documented in local studies. TRENDS IN CESAREAN SECTION RATES The trend worldwide is that caesarean section rates are raising. Data summarizes the changes from 1965 to 1985 indicate an increase in the overall caesarean birth rate from 4.5% to 23% (10). However, some centers maintained a stable rate at less than 5% over the same period of time, without adverse perinatal or maternal outcome (12). Mati found a rate of 6% for Nairobi in the Nairobi birth survey (59). This study showed a higher rate of 13% for private hospitals, compared to the teaching hospital 6%. Currently, the cesarean section rate in the USA, Brazil and Chile is 25%, 40% and 37% respectively (39). In Kenya, caesarean section rate has varied with time, place and type of institution. Kenyatta National Teaching and Referral Hospital handling mainly high risk cases has maintained a rate of about 20% over a period of 17 years between 1975 and 1992 (13,14,15,72). However, this rate has almost doubled to about 42% currently (77). Pumwani Maternity Hospital, Nairobi, has had a rate of 4.3% 1983 (16) and 6.8% 1990 (17). Latest reports show it is currently at 10% (84). Similarly, low rates have been found in other centers. Kericho District Hospital, 1991 had a rate of 8.23% (18), Coast General Hospital has had a rate of 7.1% 1990 (19) and recently 6.7% 1996 (81). Nairobi Hospital has had a relatively high rate of 28.2% for the period 1995-1997 (20). Reasons for rise in caesarean section deliveries as As demonstrated by Henens et al (21) different factors have contributed to the rise in caesarean section deliveries and have varied with time, place, type of institution, policy of institution, technological advancement, qualification of personnel, mode of management of labour, social, demographic and economic factors, while consumer pressure, fear of litigation are increasingly becoming more important (24). The latter apply more so in private institutions. Availability of effective antibiotics, safe blood banking services, anesthesia, improved technique and materials for performing caesarean section all contribute to make caesarean section a safe procedure. Limited family rise as a result of family planning methods has given way to demand for quality survival. The impact of demographic shifts has seen more women having their first birth at advanced maternal age, which has been shown to be associated with antenatal and intrapartum complications necessitating 57 caesarean section delivery (19,21,22). In the USA. the number of patients having their first birth at age of at least 30 years has risen from 20 to 25 percent (22). The socio-economic status of the patient has had a significant role. Patients who have medical insurance compared to non-insured; cared for by obstetricians compared to low cadre health provider; private compared to clinic patient is more likely to have a cesarean delivery (14b). Hence, poor economic incentive to the obstetrician is associated with low cesarean section rate (40b). It has been found that the informed patient and or her spouse are likely to discuss labour with their physician and request or demand for cesarean section (74). `Fear' of undergoing natural birth or fear of perineal disruption with consequent impaired sexual function is known to be prevalent in Brazil, accounting for its high caesarean section rate (39). The role of litigation in caesarean delivery had not been documented locally. In the U.S.A 70% of obstetricians have had litigation against them. It is thought that these are more likely to deliver their patients by caesarean section (74) impacting on such chart diagnosis as fetal distress or dystocia. The role of HIV is likely to impact on caesarean section rates. It is estimated that worldwide, about 2.3 million HIV infected women give birth yearly. It is thought that elective caesarean section can reduce perinatal vertical transmission (80). CLINICAL INDICATIONS There is hardly any obstetrical condition that has not been managed by cesarean section. Common indications include repeat caesarean section, fetal distress, malpresentation, dystocia and obstetrical haemorrhage (13-24). Mati et al (59) demonstrated that breech vaginal delivery was associated with very high perinatal mortality rate. In this study, 80% breeches were delivered vaginally and only 20% by caesarean section. This led to the policy of caesarean section for all breeches, except for selected cases, hence accounting for increase in caesarean births. In the Nairobi Hospital study, only 3% of breeches had vaginal birth (20). Prematurity which is often associated with breech presentation comparends the use of caesarean section. In his study, Mati showed that breech delivery accounted for 2.7%, Karanja (13) and Rupani (19) found it to be significant. Repeat caesarean section delivery has been shown to contribute to high caesarean section rate of more than 50% (13,16,20,59,72) with dystocia and fetal distress as its major complications. Before the advent of vaginal birth after caesarean section, the rates were even higher. Dystocia encompasses multiple diagnoses such as cephalopelvic disproportion, failure to progress, failed induction, prolonged second stage, cervical dystocia and primary uterine inertia. Ojo et al demonstrated that Africans have a disadvantageous narrow pelvis and CPD is significantly a feature (45). In the absence of CPD, active management of labour by early amniotomy and use of syntocinon is an alternative to caesarean section (12). Other proposed alternatives to caesarean section include vaginal birth after caesarean section. Walton reported a success rate of 68% for Kenyatta National Hospital (72). In some center, use of prostaglandin and syntocinon has raised success rates. Most caesarean sections are performed as emergency procedures with an elective rate of less than 4% (15,18,19,81). However, Nairobi Hospital had an elective procedure rate of about 40%. The latter is associated with lower maternal mortality, however, latrogenic prematurity can be an outward effect. The low transverse incision is commonly used (13,18,19). It allows possibility of subsequent vaginal birth. However, the Kronig (8) incision has been used in conditions where the lower segment is not well 58 formed such as preterm breech delivery. Other types of incision include the classical. Karanja (13) and Rupani (19) reported a classical rate of 4% mainly for extensive adhesions from previous caesarean section delivery. General anaesthesia is more commonly used in caesarean section deliveries (13,18,19,76), compared to regional anaesthesia, it is associated with more complications. In his study, Kaihura (76) demonstrated that there was less morbidity associated with on of spinal anaesthesia compared to general anaesthesia. Benefits of caesarean section in reducing perinatal, maternal morbidity and mortality are well documented (10,11,12). Kenya has a maternal mortality ratio of 365/100,000 births (82) and it is thought that cesarean section could have prevented 25% of such deaths especially in rural areas where the procedure is underutilised (83). However, it has been argued that a decrease in perinatal mortality is still possible in spite of low caesarean section rate if active management of labour is practised (12) and when there is an overall improvement in obstetrical and perinatal care. Other workers have also shown that inspite of rise in rates for fetal distress, there has been no noticeable decrease in cerebral palsy (41) while in 50% of cerebral palsy cases there is no evidence of birth asphyxia (42) and there is considerable evidence that the majority of damaged new borns are injured prior to labour (43). Maternal morbidity and mortality following caesarean section vary greatly from series to series, but are consistency high than following vaginal delivery (26,44) both in developed and developing countries (45,48,49). This is partly due to the surgical procedure itself and other complications that require the operation. Risk factors for morbidity and mortality include unbooked status, emergency compared to elective procedure, use of GA, anaemia, dehydration, duration of labour, repeated vaginal examinations. RATIONALE Cesarean section is a common hospital based procedure whose rate is rising worldwide causing concern. There is need to periodically determine the rates, trends, indications, fetal and maternal outcomes as they relate to socio-demographic changes and institutional policies and to have a national consensus and audit system, which evaluate patient management and make contribution to national policy guidelines. This is particularly needful in Kenya to assess quality of health care and improve on it; the young population in Kenya with its high dependency ratio and HIV prevalence will impact much cesarean section as a service. Caesarean section is an instrument that is useful in halting vertical HIV transmission. The government is putting in place measures to alleviate poverty; it would be interesting to see how this impacts on cesarean section in Kenya. Low caesarean section rates in some parts of Kenya are not necessarily associated with good perinatal outcome. Hence the need for periodic evaluation of cesarean section with regard to demographic shifts, education, family size among others. This will go a long way to assist policy makers to make effective health management systems. The safe motherhood programme advocates that each hospital publish its vital statistics, which include cesarean birth rates, maternal mortality and morbidity. There is need to understand complications that arise in regard to cesarean section delivery even in "good settings" like private hospitals in Kenya. This can help create a basis of standards. So far, few studies have been done in private institutions (which are of higher socio-economic status) and it is of interest to compare performance in these institutions with teaching and public hospitals (of generally low socio-economic status). 59 Private hospital patients are likely to be managed by obstetricians, have a high proportion of old nulliparous mothers, be of high education and socio-economic status, be better informed and likely to request caesarean section. OBJECTIVES BROAD OBJECTIVES To determine the caesarean section rates, indications, maternal and fetal outcomes at a private hospital in Nairobi. SPECIFIC OBJECTIVES 11. To determine the sociodemographic characteristics of patients who underwent caesarean section at MP Shah 12. To determine caesarean section rate at MP Shah Hospital over a period of one year 13. To determine the indications for caesarean section 14. To determine proportion of mothers who request for cesarean section 15. To determine the perinatal and maternal outcomes among patients who underwent caesarean section 16. To determine the relationship between indications for caesarean section and sociodemographic characteristics 17. To determine proportion of mothers who underwent BTL 18. To determine the proportion of mothers who are HIV 19. To recommend ways of reducing cesarean section rates, maternal and fetal morbidity and mortality. 20. To determine decision to incision time METHODOLOGY Study Design. This will be a retrospective descriptive study. Study area. The study will be conducted at MP Shah Hospital. Study period. 1st January 1998 to 31st December 1998 inclusive. However, this will depend on the duration it takes to achieve the desired sample size of 400 caesarean section cases. Study population. This will comprise all patients delivered by cesarean section at MP Shah Hospital during the period 1st January 1998 to 31st December 1998. Sample size determination The expected repeat caesarean section rate is approximately 50%. Accuracy is desired at 0.05 level. Z statistic is 1.96. The desired sample size n, will be calculated as follows N = Z2P(1 – P)/D2 Where N = minimum sample size to be determined P = expected caesarean section rate at 50% 60 D = precision / reliability with which to determine P taken as 0.05 for 95% confidence limit Z = standard errors from the mean corresponding to 95% confidence level taken 1.96 The calculated sample size was therefore N = [(1.96)2x 0.5 (1- 0.5)]/0.052 N = 384 Therefore 400 cases will be used. This will be a convenient sampling procedure involving all women delivered by caesarean section during study period. Inclusion criteria 1. 2. For the purpose of calculating the caesarean section rates, all women who delivered during the study period will be included in the study to get the denominator. All women who delivered by caesarean section during the study period will be analysed. Exclusion criteria Cases of ruptured uterus and abdominal pregnancies; and pregnancies less than 28 weeks will be excluded. DATA COLLECTION All patients admitted in the maternity ward of MP Shah Hospital and subsequently delivered by cesarean section during the study period (1st January 1998 to 31st December 1998) will form the study population. The names and file numbers of all the patients who delivered at the unit during the study period will be sought by use of the hospital birth register. This will be retrieved with the help of the records clerk. The files will be coded according to sequence of occurrence in register. Data will be extracted from the files and filled in pre-coded questionnaire by the principle investigator. Pre-testing of questionnaire will be done to determine the suitability. An office will be sought for data collection from the administration. A clerical officer from the hospital will help in file retrieval. The names and file numbers of all patients who delivered at MP Shah Hospital for the period 1st January 1998 to 31st December 1998 will be sought from the birth register in the Maternity Unit, to determine their ages and mode of delivery. The proportion of those who delivered by caesarean section will give he caesarean section rate for the hospital. The age specific cesarian section rate will be calculated by determining the proportion of cesarean births for any specific age group. However, for this study, the files of all mothers who delivered by caesarean section will be sought and coded. A prepared questionnaire will be filled by the principal investigator using data extracted from the files. This will include maternal age, parity, indication of caesarean section, gestational age (completed weeks) calculated from LMP using Magaele's rule). Apgar score, weight in grammes at delivery, sex, maternal morbidity. Study concepts have been defined (see appendix on page 16). Pretesting of the questionnaire will be done on 20 files to determine the suitability and modification made accordingly. A retrieval rate of 95% is expected. Data management. Data from the precoded questionnaire will be cleaned and entered into a computer program with the help of a qualified statistician. Data analysis Frequency tables will be used to look for outliers. Cross tabulation will be done in accordance to the specific objectives in order to determine relationships. Differences will be tested using chi-square method at 95% confidence limit. A P value of < 0.05 will be considered statistically significant. Ethical considerations 61 Approval to conduct the study will be sought from my the M.P. Shah hospital Board and Ethical Committee. Information obtained will be held in confidence. Study period Study constraints. It is anticipated that file retrieval may not be 100 percent. Clinical documents of a diagnosis may be vague. A single delivery may be associated with two or more indications for example one previous scar and fetal distress. Multiple diagnosis for example previous caesarean delivery and fetal distress will be classified under "previous scar" according to the model of Anderson et al (10). 62 RESULTS Table 1: Sociodemographic characteristics Characteristic 1. Nationality Kenyan Non Kenyan 2. Age 15 - 19 20 - 24 25 - 29 30 - 34 35 - 39 ≥ 40 3. Marital status** Single Married 4. Religion Protestant Catholic Muslim Hindu Other 5. Occupation Professional Business Housewife Student Booking status Yes No Education Primary Tertiary File retrieval rate Freq Valid % 459 38 92.3 7.6 3 56 153 171 82 21 0.6 11.5 31.4 35.1 16.8 4.3 311 26 62.3 5.2 273 87 50 21 7 62.3 19.9 11.4 4.8 1.8 332 149 12 3 66.9 30 2.4 0.6 439 13 97.1 2.9 1 3 494 x 100/596 25 75 82.9 63 Table 2: Distribution by mode of delivery Mode of delivery Freq Valid % SVD 1292 62.5 C/S 596 28.8 Vacuum delivery 152 7.4 Breech vaginal delivery 25 1.2 Forceps 2 0.1 Total number of deliveries 2067 Caesarean section rate 596 x 100/2067 28.3 Table 3: Summary of Means Characteristic Birth weight Age(years) Gestational age in weeks Duration of hospital stay (days) Duration decisionincision(hrs) Mean 3085.595 30.360 38.218 5.818 SD 680.728 5.111 2.358 3.160 median 3150.00 30.000 39.000 5.000 Max 5250.000 45.000 44.000 30.000 Minimum 450.000 16.000 26.000 0.000 88.472 125.924 60.000 1200.000 0.200 Table 4: Previous obstetric performance Characteristic 1. Parity*** 0 1–2 3–4 ≥5 2. Still births Yes No 3. Neonatal deaths Yes No 4. Previous abortion Yes No Freq Valid % 145 260 59 10 30.5 54.7 12.4 2 17 482 3.4 96.4 36 463 7.2 92.8 Table 5: Antenatal complications Characteristics Freq. None Valid % 64 Mode 3200.000 30.000 38.000 5.000 60.000 Hypertensive disease Diabetes mellitus Anemia UTI Infections e.g. malaria Multiple pregnancy APH Malpresentation/malposition Cervical incompetence Fibroids/ infertility Cardiac disease in pregnancy Trauma/burns Elderly primigravida Asthma HIV infected 108 1 8 6 4 15 3 4 7 4 1 6 Muniu 4 9 (66) 12 Table 6: Timing of caesarean section Characteristics Frequency Elective 218 Emergency 270 Valid Percent 44.7 55.3 Table 7: Rank of C/section Characteristics 0 1 2 3 4 Frequency 295 144 48 11 1 Valid Percent 59.1 28.9 9.6 2.2 0.2 Table 10: Time between decisions to incision Characteristics Frequency (n= 222) <= 30 min 19 >= 30 min – 1 hr 97 >1 hr – 1.5 hr 61 >1.5 hr – 2 hr 25 >2 hr – 3 hr 8 >3 hr – 4 hr 5 > 4 hr 7 valid percent 8.6 43.7 27.5 11.3 3.6 2.3 3.1 Table 11: Overall indication of caesarean section Freq Repeat caesarean section 204 Malpresentation / malposition 61 Fetal distress 58 Dystocia 65 Obstetric hemorrhage 29 PET/IUGR 24 Valid % 40.2 12.76 12.13 13.6 6.07 5.02 65 Myomectomy / fibroids BOH Reduced fetal movements Request for C/S ROV Previous uterine perforation Elderly primigravida HIV + Congenital mal HSIL Vaginal septum Spinal injury 9 5 17 2 1 2 2 1 2 1 1 1 1.88 1.05 3.56 0.42 0.21 0.41 0.41 0.21 0.41 0.21 0.21 0.21 One patient who was a primigravida requested for C/S. The second patient was one previous scar with an adequate pelvis (ELP). Table 12: Commonest indications for primary caesarean section Malpresentation/malposition Breech 29 OPP 20 Transverse lie 5 Face to pubes 4 Unstable lie 1 Shoulder Compound 2 Fetal distress 21.56% 58 20.50% Dystocia Contracted pelvis CPP Poor progress Cervical dystocia Failed vacuum Prolonged labor Obstructed labor 4 53 4 2 2 22.97 Obstetric hemorrhage Abruptio placenta Placenta previa Placenta increta APH ROV 16 2 1 1 10.25% PET/IUGR eclampsia 12+8+4 66 8.48% 5+4 Myomectomy/ fibroids 3.18% BOH, reduced FM Table 13: Indications for repeat caesarean section (one previous scar) Indication Elective Freq Emergency Valid % Freq Valid % Dystocia Fetal distress Breech presentation APH BOH Request HIV Other Table 13: Proportion of BTL between elective and emergency procedure Characteristic Freq Valid % Elective C/S+BTL Emergency C/S+BTL 44 patients underwent BTL at caesarean section. Table 15: Caesarean section indication by timing: elective or emergency. Indications Elective Freq Emergency Valid % Repeat cesarean Dystocia Fetal distress Breech APH BOH 67 Freq Valid % Request Other OUTCOME OF DELIVERY DISTRIBUTION BY BIRTHWEIGHT Table 16: Distribution by Gestational age Characteristics Frequency < 31 8 31 – 36 63 37 – 42 380 > 42 4 Valid percent 1.8 13.8 83.5 0.9 Proportion of prematurity = 71 x 100/455 = 15.6% Table 17: Distribution by Birth weight Birth weight Freq (n = 485) Valid % <1000 3 0.7 1000 – 1499 9 1.7 1500 – 2499 61 12.6 2500-3999 379 78.6 > 4000 33 6.3 Proportion of low birth weight = 15 % Table 18: Sex distribution Sex Freq Valid % Male 240 51.9 Female 222 48.1 Male: Female ratio = 68 Table 19: Distribution of Apgar score at 5 min Apgar score Freq (n = 492) ≥7 441 1–6 44 0 7 Table 20: Outcome of delivery Outcome Freq (n=508) Live 500 FSB 7 MSB 1 Valid % 89.6 8.9 1.4 Valid % 98.4 1.4 0.2 Table 21: severe neonatal morbidity Characteristics Transferred Left behind Intubated Frequency 6 15 4 Valid percent 24.0 60.0 16.0 Table 21: Causes of neonatal morbidity Cause Freq Asphyxia prematurity Congenital malformation Malpresentation Iatrogenic Neonatal sepsis Jaundice Other Total Valid % Table 22: Type of congenital malformation Characteristics Frequency N/A 424 Neural 3 Genitourinary 1 Musculoskeletal 8 Other 31 Circumcised 2 Nauroria 1 Meconium aspiration 1 Jaundice 13 Premature 1 Neural, musculoskeletal 1 Jaundice, sepsis 1 Asphyxia 1 Valid percent 86.9 0.6 0.2 1.6 6.4 0.4 0.2 0.2 2.7 0.2 0.2 0.2 0.2 69 Table 23: Causes of neonatal death Asphyxia Prematurity Apnoec attack RDS Lung malformations Severe-congenital malformation. Other Freq (n = 7) 1 1 1 1 1 1 1 Valid % Table 24: Distribution of perinatal deaths by indication and gestational age Characteristic NND FSB MSB Gestational age (wks) <31 31 – 36 37 – 41 ≥42 Birth weight <1000 1000 – 1499 1500 – 2499 2500 – 3599 ≥ 4000 Timing of C/S Elective Emergency Indication of C/S Primary C/S Repeat C/S HIV status Negative Positive Medical illness in pregnancy (PET) Yes No Cesarean section perinatal mortality rate = 70 Table 25: Neonatal Outcome versus timing of caesarean section Table 26: Maternal morbidity and mortality Freq Blood transfusion ICU/HDU admission Febrile morbidity PPH Pueperal infection Prolonged hospital stay (more than 7 days) Left baby behind** Grief Dissatisfied with care Discharged against medical advice ARF DVT UTI 2 4 13 7 5 35 1 1 1 1 2 2 Table 27: Duration in hospital following cesarean section Number of days Freq Valid % ≤7 478 87 8-10 46 9.2 11-14 11 1.6 ≥15 14 2.2 71 Valid% COMPARISON OF RATES AND OUTCOME IN DIFFERENT REGIONS IN KENYA Nairobi hospital 28.2 35.5 40.5 -12.7% 13.5 -- Kenyatta Pumwani Chogoria Coast Kericho 18 50 49.5 4.3 10.3 46.1 25.5 7.1 27.5 3 8.2 20.5 6.25 -- 12.5 15/1000 76.8/1000 36.4 91.8 142 0.00/ 1.4 6.1 4.83 9.6 Maternal morbidity -(febrile) Primigravida 37.8 17.3 20.4 13 26.8 -- 26.3 30.8 36.6 Elective sterilization 22 -- 10.6 11.6 Hospital duration ≥ 8 Not clear days Age ≥ 35 10 7.5 -- 19 74 -- 9.1 6 6 Age specific C/S rate for 28.9 primigravida Breech C/S 10 -- -- 7.4 -- 6.8 15.2 -- 5.4 Classical C/S -- 4 4 3.6 Commonest indication Repeat C/S Repeat FD FD C/S rate Repeat C/S Elective C/S Prematurity Low birth wt Asphyxia Perinatal mortality Maternal mortality 10.4 10.4 8.9 C/S 72 28.65 Repeat C/S Dystocia FD FD 2.4 6.7 Dystocia Repeat CS Coast 79 C/S rate Repeat C/S Elective 6.7 4.9 4.7 Pumwani S.K. 6.8 36 -- Prematurity Low birth wt Asphyxia ---- ---- Perinatal mortality/1000 Maternal mortality/1000 89 118 8.3 6.3 MP Shah Muriu Nairobi Birth Survey 20 42 -- 6.6 26 -14.3 16.9*1 minute Maternal morbidity 18 (febrile) Primigravida 50.6 19 36 25 Elective sterilization 6.5 -- -- 6.0 5.5 8.7 -- -- -- 60 30 1.1 0.6 11.9 Classical 18 -- 1 Commonest indication Dystocia FD Dystocia Repeat FD Age specific C/S rate for -days Breech C/S 28.9 73 13 C/S Discussion ABSTRACT Background: Cesarean section is the commonest hospital based-operation whose rate is rising worldwide. The rates and trends depend on medical, socioeconomic factors, education and indications such as request for cesarean section, even in the absence of a medical indication. MP Shah Hospital is private hospital in Nairobi, where socioeconomic status of the population is high, and that patients are more informed and are likely to demand for cesarean section. The study involved all women delivered by caesarean section at M.P. Shah Hospital, for the period 1st January 1998 and March 2000. Most studies in Kenya have involved government hospitals. Objective: to determine the cesarean rates, indications and outcomes in a private hospital Study site: MP Shah Hospital Study design: This was descriptive cross- sectional retrospective analytical study. Study methodology: A pre- tested structured questionnaire was used by the principle investigator to abstract information from case files. Results were computed and analyzed using SPSS version 10.0 Results The majority (92.3%) was Kenyans and 97% had booked to deliver at the hospital. The mean age of the population was 30.4± 5 years, adolescents comprising 12%. 62.3% were married and 66% were in professional employment. The cesarean section rate was 28%, of which 55.3% were emergencies. For emergencies the decision- to-incision time was less than an hour in 52% of the cases. The commonest indications were repeat cesarean section (40%), dystocia 13.6% malposition or malpresentation 12.8% and fetal distress 12.1%. Only two cases requested for cesarean section. 36% had antenatal complications with PET comprising 60% of the complications. The HIV status was documented in only 66 (13.2%) cases, of which 9 (12%) were positive. One HIV case had an elective cesarean section. 13.2% of the population had surgical sterilization. 15 (3%) were multiple births. The mean gestational age at cesarean section was 38.2 weeks± 2.6 weeks with 15.6% being preterm infants. The mean birth weight was 3086 gm ±680 gm with 15% being low birth weight. There were 8 stillbirths and 7 neonatal deaths. Asphyxia occurred in 44 (8.9%) of the cases, of whom 6 were transferred to another hospital for intensive care. There was one term neonatal death with multiple congenital anomalies, the rest were due to extreme prematurity. During the study period there were no maternal deaths. Maternal morbidity occurred in 18.8% with prolonged hospital duration being commonest cause. Two cases were admitted to ICU with DIC associated with eclampsia, and two were admitted in HDU due to poor reversal. Most cases (87%) were discharged within one week of admission. Conclusion Caesarean section rate is high. Cases of documented request for CS are negligible. Recommendation INTRODUCTION BACKGROUND AND LITERATURE REVIEW Cesarean section is one of the commonest hospital based surgical procedures and its rate has been rising worldwide. it has been defined as the delivery of a fetus, placental and membranes through an incision in the abdominal and uterine walls (1). This term does not derive from the birth of Julius Caesar, as is popularly thought. From the inception as a postmortem procedure under the Roman law, Lex Cesarean (2) it has undergone refinements in technique aimed at modifying the risk of maternal morbidity and mortality which was pervasive. The low transverse incision by Kerr (9) is now popularly used as it also allows the possibility of vaginal birth after cesarean section in contrast to the classical incision which only allowed a repeat caesarean section delivery. The concept of vaginal birth after cesarean was proposed in the early 60s, however, it is 74 only in the mid 1980s that it become popular; thus curtailing the upward spiral in cesarean section rates. In fact it is safe and has a high success rate of more than 60% of the trials of labour (10,23,24). Patients' role in demand for cesarean section is recognized to affect gains achieved by practise of trials of labour in previous cesarean. However, such an indication has not been documented in local studies. TRENDS IN CESAREAN SECTION RATES The trend worldwide is that caesarean section rates are raising. Data summarizes the changes from 1965 to 1985 indicate an increase in the overall caesarean birth rate from 4.5% to 23% (10). However, some centers maintained a stable rate at less than 5% over the same period of time, without adverse perinatal or maternal outcome (12). Mati found a rate of 6% for Nairobi in the Nairobi birth survey (59). This study showed a higher rate of 13% for private hospitals, compared to the teaching hospital 6%. Currently, the cesarean section rate in the USA, Brazil and Chile is 25%, 40% and 37% respectively (39). In Kenya, caesarean section rate has varied with time, place and type of institution. Kenyatta National Teaching and Referral Hospital handling mainly high risk cases has maintained a rate of about 20% over a period of 17 years between 1975 and 1992 (13,14,15,72). However, this rate has almost doubled to about 42% currently (77). Pumwani Maternity Hospital, Nairobi, has had a rate of 4.3% 1983 (16) and 6.8% 1990 (17). Latest reports show it is currently at 10% (84). Similarly, low rates have been found in other centers. Kericho District Hospital, 1991 had a rate of 8.23% (18), Coast General Hospital has had a rate of 7.1% 1990 (19) and recently 6.7% 1996 (81). Nairobi Hospital has had a relatively high rate of 28.2% for the period 1995-1997 (20). Reasons for rise in caesarean section deliveries as As demonstrated by Henens et al (21) different factors have contributed to the rise in caesarean section deliveries and have varied with time, place, type of institution, policy of institution, technological advancement, qualification of personnel, mode of management of labour, social, demographic and economic factors, while consumer pressure, fear of litigation are increasingly becoming more important (24). The latter apply more so in private institutions. Availability of effective antibiotics, safe blood banking services, anesthesia, improved technique and materials for performing caesarean section all contribute to make caesarean section a safe procedure. Limited family rise as a result of family planning methods has given way to demand for quality survival. The impact of demographic shifts has seen more women having their first birth at advanced maternal age, which has been shown to be associated with antenatal and intrapartum complications necessitating caesarean section delivery (19,21,22). In the USA. the number of patients having their first birth at age of at least 30 years has risen from 20 to 25 percent (22). The socio-economic status of the patient has had a significant role. Patients who have medical insurance compared to non-insured; cared for by obstetricians compared to low cadre health provider; private compared to clinic patient is more likely to have a cesarean delivery (14b). Hence, poor economic incentive to the obstetrician is associated with low cesarean section rate (40b). It has been found that the informed patient and or her spouse are likely to discuss labour with their physician and request or demand for cesarean section (74). `Fear' of undergoing natural birth or fear of perineal disruption with consequent impaired sexual function is known to be prevalent in Brazil, accounting for its high caesarean section rate (39). The role of litigation in caesarean delivery had not been documented locally. In the U.S.A 70% of obstetricians have had litigation against them. It is thought that these are more likely to deliver their patients by caesarean section (74) impacting on such chart diagnosis as fetal distress or dystocia. 75 The role of HIV is likely to impact on caesarean section rates. It is estimated that worldwide, about 2.3 million HIV infected women give birth yearly. It is thought that elective caesarean section can reduce perinatal vertical transmission (80). CLINICAL INDICATIONS There is hardly any obstetrical condition that has not been managed by cesarean section. Common indications include repeat caesarean section, fetal distress, malpresentation, dystocia and obstetrical haemorrhage (13-24). Mati et al (59) demonstrated that breech vaginal delivery was associated with very high perinatal mortality rate. In this study, 80% breeches were delivered vaginally and only 20% by caesarean section. This led to the policy of caesarean section for all breeches, except for selected cases, hence accounting for increase in caesarean births. In the Nairobi Hospital study, only 3% of breeches had vaginal birth (20). Prematurity which is often associated with breech presentation comparends the use of caesarean section. In his study, Mati showed that breech delivery accounted for 2.7%, Karanja (13) and Rupani (19) found it to be significant. Repeat caesarean section delivery has been shown to contribute to high caesarean section rate of more than 50% (13,16,20,59,72) with dystocia and fetal distress as its major complications. Before the advent of vaginal birth after caesarean section, the rates were even higher. Dystocia encompasses multiple diagnoses such as cephalopelvic disproportion, failure to progress, failed induction, prolonged second stage, cervical dystocia and primary uterine inertia. Ojo et al demonstrated that Africans have a disadvantageous narrow pelvis and CPD is significantly a feature (45). In the absence of CPD, active management of labour by early amniotomy and use of syntocinon is an alternative to caesarean section (12). Other proposed alternatives to caesarean section include vaginal birth after caesarean section. Walton reported a success rate of 68% for Kenyatta National Hospital (72). In some center, use of prostaglandin and syntocinon has raised success rates. Most caesarean sections are performed as emergency procedures with an elective rate of less than 4% (15,18,19,81). However, Nairobi Hospital had an elective procedure rate of about 40%. The latter is associated with lower maternal mortality; however, latrogenic prematurity can be an outward effect. The low transverse incision is commonly used (13,18,19). It allows possibility of subsequent vaginal birth. However, the Kronig (8) incision has been used in conditions where the lower segment is not well formed such as preterm breech delivery. Other types of incision include the classical. Karanja (13) and Rupani (19) reported a classical rate of 4% mainly for extensive adhesions from previous caesarean section delivery. General anesthesia is more commonly used in caesarean section deliveries (13,18,19,76), compared to regional anesthesia, it is associated with more complications. In his study, Kaihura (76) demonstrated that there was less morbidity associated with on of spinal anesthesia compared to general anesthesia. Benefits of caesarean section in reducing perinatal, maternal morbidity and mortality are well documented (10,11,12). Kenya has a maternal mortality ratio of 365/100,000 births (82) and it is thought that cesarean section could have prevented 25% of such deaths especially in rural areas where the procedure is underutilized (83). However, it has been argued that a decrease in perinatal mortality is still possible in spite of low caesarean section rate if active management of labour is practiced (12) and when there is an overall improvement in obstetrical and perinatal care. Other workers have also shown that in spite of rise in 76 rates for fetal distress, there has been no noticeable decrease in cerebral palsy (41) while in 50% of cerebral palsy cases there is no evidence of birth asphyxia (42) and there is considerable evidence that the majority of damaged newborns are injured prior to labour (43). Maternal morbidity and mortality following caesarean section vary greatly from series to series, but are consistency high than following vaginal delivery (26,44) both in developed and developing countries (45,48,49). This is partly due to the surgical procedure itself and other complications that require the operation. Risk factors for morbidity and mortality include unbooked status, emergency compared to elective procedure, use of GA, anaemia, dehydration, duration of labour, repeated vaginal examinations. 77 NAIROBI HOSPITAL WORK 1996 A RETROSPECTIVE STUDY OF CAESAREAN SECTION INDICATIONS AND OUTCOME AT NAIROBI HOSPITAL FOR THE PERIOD 1ST JANUARY TO 31ST DECEMBER 1996 PRINCIPAL INVESTIGATOR DR. JAHONGA CO-INVESTIGATORS DR. WANJIHIA DR. WANJALA DR. KAGIA DR. THAGANA REPORT PRESENTED AT THE DIVISIONAL MEETING OF OBSTETRICS AND GYNAECOLOGY, THE NAIROBI HOSPITAL BOARD ROOM, ON 12TH FEBRUARY 1997 BY DR. JAHONGA 78 SUMMARY A retrospective study of caesarean section and outcome was carried out at Nairobi Hospital. A total of 654 deliveries were conducted over the same period of which 190 were caesarean section giving a caesarean section of 29.05Valid %%. The commonest indications for caesarean sections were Repeat caesarean section (34.74Valid %%) Malpresentation /malposition (16.8Valid %%) Fetal distress (15.63Valid %%) There was only one case of caesarean section on request. There were 6 perinatal deaths associated with caesarean section giving a perinatal mortality rate of 30.3 per one thousand. Antenatal care for the patients was provided for by 50 obstetricians and 4 midwives. On average there were about 110 deliveries per month giving approximately 4 deliveries per day MATERIALS AND METHODS The names and file numbers of all patients who delivered by caesarean section at Nairobi Hospital Maternity Unit from 1st January to 30th June 1996 both inclusive were obtained from the Nairobi Hospital labour ward register of deliveries. A prepared questionnaire was filled using data extracted from these records. This data included maternal age, parity, and indications for caesarean section, gestational age, and weight of baby at birth and mode of delivery. Analysis of caesarean section showed that 195 patients had lower uterine section transverse incisions and one had a classical due to extensive adhesions from two previous scars. One patient in advanced labour with compound presentation underwent emergency hysteromy, but was included in the study. Most elective procedures took place on Mondays and Fridays; and the least on Tuesdays. Seventy nine (41,6Valid %%) operations were performed as elective, 111 (58.4Valid %%) as emergencies. All operations were performed under general anesthesia. Of the dead babies, only one had a post mortem report which indicated cause of death as hyaline membrane disease. 79 RESULTS During the study period, there were 654 deliveries of which 190 were caesarean sections. Table 1: Distribution by mode of delivery. Mode of delivery SVD caesarean section Vacuum delivery Breech delivery Total 381 190 56 8 Percentage 58.26 29.05 8.56 1.22 Table 1 shows mode of delivery giving caesarean section rate of 29.05Valid %%. There were 6 sets of twins delivered by caesarean section and 2 sets by vaginal delivery. It would be of interest to know what number of those who had spontaneous vertex deliveries had a previous caesarean section. One set of twins was delivered by hysterectomy. There was one twin pregnancy with one fetus mummified. Amongst those who underwent caesarean section, only 4 cases had a vaginal delivery following a previous caesarean section. Table 2: Age distribution of patients at time of caesarean section. Age group (years) 15 – 20 21 -25 26 – 30 31 – 35 36 – 40 41 – 50 Total Frequency 3 20 73 61 31 3 Percentage 1.3 10.55 38.42 32.11 16.31 1.3 The maternal age distribution is shown in table 2 and it shows that 73 (38.42Valid %%) of the cases were in the age group 26 – 30. there were 3 (1.3Valid %%) cases in the age group 15 – 20 years, and 3 cases in the age group 41 – 45 years old. The mean age was 31.8 years. Table 3: Parity distribution of patients at time of caesarean section. Parity 0 1 2 3 4 5 6 Frequency 75 62 36 15 5 3 1 Percentage 38.1 31.5 18.3 7.6 2.5 1.5 0.6 Table 3 shows the parity distribution in the study. The highest number of cases 75 (38.1Valid %%) was recorded in the primigravida and the last 1 (0.6Valid %%) was recorded in the grand multiparous. There were 5 (2.5Valid %%) elderly primigravidas. 80 Plan of action on admission Plan of action on admission Elective caesarean section Emergency caesarean section Trial of scar Induction of labour Monitor labour 79 39 13 33 26 Previous perinatal loss in the population. There were 11 mothers associated with stillbirths, 7 of whom this occurred in their first pregnancy and was associated with PET. Two had ruptured uterus with FSB and two had neonatal deaths. Antenatal complications in the population (n = 71) Complication Hypertensive disease in pregnancy Bleeding Cervical stitch Multiple pregnancy Chronic renal disease Asthma Diabetes mellitus Neurological disease (stroke with paralysis) Trauma (RTA) Hyperemesisgravidum UTI Malaria Ovarian cystectomy in pregnancy Sickle cell Rhesus negative Number 36 5 5 6 2 2 1 1 1 2 2 1 1 2 2 Those who did not have a complication were 62.4Valid %%. Those associated with complications were 37.6Valid %%. Table 4: Rank of caesarean section by mode of delivery (n = 190) Rank 1 2 3 4 Elective caesarean Emergency section caesarean section 32 92 28 16 18 2 1 1 Total Percentage 124 44 20 2 66.26 23.15 10.52 1.0 Table 4 shows the distribution by rank of caesarean sections. One hundred and twenty four (66.26Valid %%) were primary caesarean sections, 66(33.74Valid %%) were repeats. 81 Table 5: Overall indications for caesarean section Indication of caesarean section Repeat caesarean section Malpresentation/malposition Fetal distress Dystocia Obstetrical haemorrhage PET/IUGR Myomectomy/fibroids BOH Reduced fetal movements Others Freq 66 32 29 23 12 10 5 4 4 5 Percentage 34.74 16.84 15.63 12.11 6.16 5.26 2.63 2.10 2.10 5.26 Table 6: Primary caesarean section indications (n = 124) Primary caesarean section Freq indication Malpresentation/ malposition 32 Breech 17 OPP 10 Oblique 3 Face pubes 1 Unstable lie 1 Fetal distress 29 Dystocia 22 CPD 15 Poor progress 3 DTA 1 Cervical dystocia 1 Failed forceps 1 prolonged labour 1 Obstetrical hemorrhage 12 abruptio placenta 8 placenta previa 2 placenta increta 1 APH (Unknown cause) 1 PET/IUGR 10 Myomectomy /fibroid 5 BOH 4 Reduced fetal movements 4 Others 6 Percentage 16.84 15.26 6.31 6.31 5.26 2.63 2.10 2.10 3.15 Table 7: One previous scar indications ( n = 44) Indications CPD Failed trial Diagnosis unstated Malpresentation PET Myomectomy Freq 12 7 7* 6 2 2 Percentage 12.27 15.91 15.91 13.63 4.54 4.54 82 BOH 2 APH 1 Others 5 Others include: postdatism, previous uterine rapture, reduced fetal movements, scheduled for elective 4.54 2.27 11.36 * All were elective procedures. Of all the 111 emergency caesarean sections, 39 (35Valid %%) underwent the operation on admission while 72 (65Valid %%) laboured prior to the caesarean section. Outcome of delivery Table 8: Distribution of birthweight (grams) Birthweight (grams) ≤ 2499 2500 – 3999 ≥ 4000 Frequency 21 148 14 Percentage 12.4 80 7.6 Table 8 shows the distribution of birthweights. The range was 1390 – 4442 with a mean of 3109 grams. Low birth weights were 21 (12.4Valid %%). Table 9: Distribution of gestational age Gestational age 31 – 36 37 – 42 > 42 Total Frequency 21 165 4 Percentage 12.8 86.6 2.1 Table 7 shows the distribution by gestational age in complete weeks. The range was 31 to 42 weeks, with a mean of 38 weeks. 83 Table 10: Distribution of perinatal deaths by gestational age and indications Type of perinatal death Noenatal death 1 Gestational age Indication Comment 41 PET + abruptio Patient admitted for induction and noted to have severe bradycardia 2 33 PET/IUGR 3 Fresh still birth 1 40 PET/ induction 39 Abruptio bradicardia 2 Macerated still birth 33 39 PET + abruptio Presented with APH IUFD + 2 previous Admitted with labour scars pains & loss of fetal movements for two days Patient electively delivered due to severe IUGR Had previous FSB due to PET placenta, Loss of fetal movements for one day Congenital malformations There were 7 cases of clinically identified congenital malformations as follows: Malformation Mongal Meningocele Deformity of the right upper limb Extra digits Hypospadia Cord abnormality Frequency 1 1 1 2 1 1 Neonatal morbidity There were 7 babies with severe asphyxia requiring intubation, 1 baby with iatrogenic injury from scapel nick. Maternity morbidity There were 4 cases (1.58Valid %%) of maternity morbidity. Two cases of febrile morbidity; 1 urinary tract infection, and the other no pathogen was isolated from urine and high vaginal swab specimens. There was 1 case of hemorrhage due to placenta increta who underwent emergency hysterectomy and was transfused 2 unis of blood. There was no maternal mortality. 84 Hospital duration The average hospital duration was 5 days with a range of 4 to 19 days. One mother stayed for 14 days after hysterectomy and another who presented as an emergency with 3 previous scars in labour stayed for 19 days. Contraception Nineteen patients underwent bilateral tubal ligation with the caesarean section giving a BTL rate of 10Valid %%. Table 1: Place Nairobi Hospital Kenyatta National Hospital Pumwani Maternity Period 1996 1980 Rate 29.05 17.8 1983 4.3 Coast General 1990 7.1 Kericho 1990 8.22 Nairobi birth survey Ethiopian 1983 1992-1993 6.6 8 Italy Zaire 1980 – 1983 1. public 2. private 1992 11.8 13.3 12.0 Czech Republic 1986 – 1994 10 USA 85 Reference Karanja J.G., Mmed thesis UON 1981 Bausai Y.P. et al E.A.M.J 64(11) 741-4, 1987 Rupani M.P, Mmed thesis, UON 1991 Kudoyi W.O M.Med thesis UON 1993 EMJ 1983 EMJ 1995 vol. 72 pp 6660 – 63 Perazzini F. et al Br. J.Obst.Gyn 99 p 203, 1992 Tidsskr nor laegforen (Norway) 1996 116(1) p67 – 71 Ceskagynekol (Czech Republic) 1995, 60(6) p283 – 9 Table 2: Comparison of findings by other studies Nairobi Hospital Karanja Kudoyi Rupani Bausai Muriu Nairobi birth survey Rank of caesarean section Primary 66.26 48.8 77.68 72.5 69 56.6 - Repeat 33.74 51.2 22.32 27.5 31 43.5 - Table 3: Overall indications for caesarean section Nairobi Hospital Repeat caesarean section, malpresenation/malposition, fetal distress, dystocia CPD, repeat c caesarean section, fetal distress Dystocia, repeat caesarean section, malpresentation / malposition CPD, repeat caesarean section, prolonged labour, fetal distress - Karanja Kudoyi Rupani Bausai Muriu Sociodemorgraphic. Freq Valid %% 86 Nationality Kenyan Foreigners Age 15 – 19 20 – 24 25 – 29 30 – 34 35 – 39 40 and above Marital status Married Single Unknown Occupation Professional Housewife Auxiliary Student Religion 459 38 Total 497 92.3 7.6 3 56 153 171 82 21 Total 486 0.6 11.5 31.4 35.1 16.8 4.3 311 26 162 62.3 5.2 32.4 332 149 12 3 66.9 30 2.4 0.6 Freq 145 153 107 48 11 5 4 1 474 Valid %% 30.5 32.2 22.5 10.1 2.3 1 0.8 0.2 Distribution by parity Para 0 Para 1 Para 2 Para 3 Para 4 Para 5 Para 6 Para 11 Total Caesarean section rate by primary report Primary caesarean section Repeat caesarean section Total Freq 283 191 474 Valid %% 59.7 40.2 100 Distribution of caesarean section by timing Emergency caesarean section Freq 215 Valid %% 44.98 87 Elective caesarean section Total 263 478 53.02 55.02 Distribution of caesarean section by rank Freq No previous primary caesarean 283 section 1 previous scar 136 2 previous scar 40 3 previous scar 10 4 previous scars 1 Total 474 Overall indication of caesarean section Repeat caesarean section Malpresentation / malposition Fetal distress Dystocia Obstetric hemorrhage PET/IUGR Myomectomy / fibroids BOH Reduced fetal movements Request ROV Previous uterine perforation Elderly prigravida HIV + Congenital mal HSIL Vaginal cept Spinal injury Valid %% 59.7 28.6 9.2 2.1 0.2 100 n = 478 Freq 191 61 58 65 29 24 9 5 17 1 1 2 2 1 2 1 1 1 Valid %% 40.2 12.76 12.13 13.6 6.07 5.02 1.88 1.05 3.56 0.21 0.21 0.41 0.41 0.21 0.41 0.21 0.21 0.21 Indication for primary caesarean section n = 283 Malpresentation/malposition Breech OPP Transverse lie Fake topubes Unstable lie Shoulder Compound Fetal distress 29 20 5 4 1 2 21.56Valid %% 58 88 20.50Valid %% Dystocia Contracted pelvis CPP Poor progress Cervical dystocia Failed vacuum Prolonged labor Obstructed labor 4 53 4 2 2 22.97 Obstetric hemorrhage Abruptio placenta Placenta previa Placenta increta APH ROV 16 2 1 1 10.25Valid %% PET/IUGR eclampsia 12+8+4 Myomectomy/ fibroids 8.48Valid %% 5+4 3.18Valid %% BOH, reduced FM IPS: Indications n = 136 Malpresentation/ malposition breech OPP Obline Transverse Placenta topuses Unstable lie Fetal distress 7 1 1 1 7.35Valid %% 4 2.94Valid %% Dystocia CPD Poor progress Dystocia Failed vacuum/forceps Failed trial Contracted pelvis 36 2 1 5 89 33.83Valid %% Obstetric hemorrhage Abruptio Placenta previa Placenta increta ROV Cord prolapse PET /Hypertensive disease Eclampsia IUGR 5 1 1 1 1 5.88Valid %% 10 6 2 2 7.35Valid %% Myomectomy Fibroid Previous uterine perforation 1 1 1 BOH 2.21 4 Reduced FM 2.94Valid %% 9 Others prom 6.62Valid %% 5 Unstated 3.68Valid %% 3 22.79Valid %% IPS (unqualified) Number = 30 IPS (unqualified) + BTL = 6 90 CORRECTIONS FORR ALLAN Save on diskette Teach Robet how to make and delete boxes and draw tables. He is my assistant when u r away If possible le him know where each typed document is LET ME HAVE A LOOK at the work b4 u quit. This applies to all assignments Return the work for filing or ask me where u should file it 6.5.5 Page 19 and 20 have a problem with the margin Can we use the format on hiv proposal to work out the time line 91