Cardiac Signal Transduction: G-Protein Pathways in Heart & Vessels
advertisement

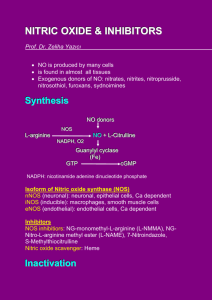
Cardiac Signal Transduction Mechanisms (G-Protein-Linked) There are several major signal transduction mechanisms found in cells of the cardiovascular system, the most important being the Gprotein and nitric oxide-cyclic GMP pathways. Described below are the G-protein-coupled pathways found in the heart. Signal transduction mechanisms regulating vascular smooth muscle contraction and relaxation are found elsewhere (Click Here). Gs-Protein and Gi-Protein Coupled Signal Transduction G-proteins are linked to an enzyme, adenylyl cyclase, that dephosphorylates ATP to form cyclic AMP (cAMP). Gs-protein (stimulatory G-protein) activation (e.g., via β-adrenoceptors) increases cAMP by activating adenylyl cyclase. cAMP then activates PK-A (cAMP stimulated protein kinase) and causes increased cellular influx of Ca++ by phosphorylation and activation of L-type calcium channels, and enhanced release of Ca++ by the sarcoplasmic reticulum in the heart. These and other intracellular events increase inotropy (muscle contractility), chronotropy (heart rate), dromotropy (velocity of electrical conduction) and lusitropy (relaxation rate). Activation of Gi-proteins (inhibitory G-protein), for example by adenosine and muscarinic agonists binding to their receptors, decreases cAMP (through adenylyl cyclase inhibition), inactivates PK-A, decreases Ca++ entry into the cell and release by the sacroplasmic reticulum, and increases outward, hyperpolarizing K+ currents. Gi-protein activation produces effects that are opposite to those elicited by Gs-protein activation. Because Gi-protein effects are primarily found in the SA node and AV node where there are important Gi-protein coupled receptors, activation of this pathway leads to a decrease in sinus rate and AV nodal conduction velocity with minimal effects on muscle contractility. In contrast, Gs-protein strongly stimulates muscle contraction in addition to having nodal effects. Gq-Protein and IP3- Coupled Signal Transduction The IP3 pathway is linked to activation of α1-adrenoceptors, angiotensin II (AII) receptors, and endothelin-1 (ET-1) receptors and therefore is stimulated by alpha-agonists, angiotensin II and endothelin-1. These receptors are coupled to a phospholipase C (PL-C)coupled Gq-protein, which when activated, stimulates the formation of inositol triphosphate (IP3) from phosphatidylinositol biphosphate (PIP2). Increased IP3 stimulates Ca++ release by the sarcoplasmic reticulum in the heart, thereby increasing inotropy as one of its actions. Altered Signal Transduction in Heart Disease Altered signal transduction mechanisms have a significant role in the loss of inotropy in heart failure. For example, desensitization of β1-adrenoceptors in the heart decreases inotropic responses to sympathetic activation. Uncoupling of the β1-adrenoceptor and the Gsprotein reduces the ability to activate adenylyl cyclase. If the ability of protein kinase A to phosphorylate L-type calcium channels is impaired, then calcium influx into the cell is reduced, leading to a smaller release of calcium by the sarcoplasmic reticulum. Reduced calcium release impairs excitation-contraction coupling, thereby decreasing inotropy. Vascular Signal Transduction Mechanisms There are several signal transduction mechanisms that modulate intracellular calcium concentration and therefore the state of vascular tone. Two different mechanisms will be described here: 1) G-protein-coupled pathway, and 2) the nitric oxide-cGMP pathway. G-Protein Coupled Signal Transduction Like heart muscle, the Gs-protein coupled pathway in smooth stimulates stimulates adenylyl cyclase (AC), which catalyzes the formation of cAMP. Unlike the heart, however, an increase in cAMP in vascular smooth muscle causes reduced contraction (i.e., relaxation). The reason for this opposite effect is that calcium-calmodulin activates myosin light chain kinase (MLCK) in vascular smooth muscle, which phosphorylates myosin and causes contraction; however, MLCK is inhibited by cAMP. The Gs-protein is coupled to several important receptors that bind vasodilator substances, among which are β2-adrenoceptors (bind to β2-agonists such as epinephrine and isoproterenol), A2 purinergic receptors (bind to adenosine), and IP receptors (bind prostacyclin, PGI2). Gi-proteins in vascular smooth muscle are coupled to α2-adrenoceptors. Binding of these receptors to an agonist such as norepinephrine causes a reduction in cAMP, which leads to smooth muscle contraction. Gq-proteins in vascular smooth muscle are coupled to α1-adrenoceptors (bind to norepinephrine), ETA receptors (bind to endothelin1), AT1 receptors (bind to angiotensin II), V1 receptors (bind to vasopressin), and muscarinic (M3) receptors. Two signal transduction pathways are linked to Gq-proteins: phospholipase C pathway (forms inositol triphosphate, IP3) and Rho-kinase pathway. IP3 pathway stimulates SR release of calcium and activates protein kinase C (PK-C) via formation of diacylglycerol (DAG), which stimulates contraction. The Rho-kinase pathway (not shown in figure) inhibits myosin light chain phosphatase, which enhances contraction. To summarize, the following agonists act directly on vascular smooth muscle causing contraction via Gq-protein: norepineprhine, epinephrine, angiotensin II, endothelin-1, arginine vasopressin, and acetylcholine. A special note regarding epinephrine. Its binding to Gs-protein-coupled β2-adrenoceptors versus Gq-protein-coupled α1-adrenoceptors is concentration dependent because β2-adrenoceptors have a higher affinity for epinephrine than α1-adrenoceptors. Therefore, at low epinephrine concentrations vasodilation occurs, whereas at high concentrations vasoconstrictor responses become dominant. cGMP-Coupled Signal Transduction A third mechanism that is very important in regulating vascular smooth muscle tone is the nitric oxide (NO)-cGMP system. Vascular endothelial cells normally produce NO, which diffuses from endothelial cells to adjacent smooth muscle cells where it activates guanylyl cyclase leading to increased formation of cGMP and vasodilation. The precise mechanisms by which cGMP relaxes vascular smooth muscle is unclear; however, cGMP can activate a cGMP-dependent protein kinase, inhibit calcium entry into the vascular smooth muscle, activate K+ channels (causing hyperpolarization), and decrease IP3. Acetylcholine (ACh), whether administered intravascularly or released by cholinergic autonomic (parasympathetic) nerves, binds to muscarinic receptors (M3) located on the vascular endothelium, which stimulates the formation and release of NO as described above to produce vasodilation. Although ACh binds to M3 receptors located on both endothelial and vascular smooth muscle cells, if the endothelium is normal then the formation of endothelial-derived NO overrides smooth muscle M3-mediated contraction. If the endothelium is damaged so that NO release is reduced, then ACh-induced vasodilation is changed to ACh-induced vasoconstriction. Certain antihypertensive and antianginal drugs are called nitrodilators because they release NO, and thereby mimic the effect of endothelial produced NO to produce vasodilation.