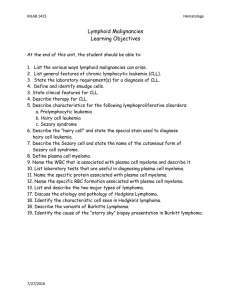
B-cell Neoplasms 2021
advertisement

B-Cell Neoplasms Acute Lymphoblastic Leukemia/Lymphomas and Mature B-cell Non-Hodgkin Lymphomas/Leukemias Belinda R. Fender, M.D. ATSU/KCOM Copyright © 2018, A.T. Still University/Kirksville College of Osteopathic Medicine. This presentation is intended for ATSU/KCOM use only. No part of this presentation may be distributed, reproduced or uploaded/posted on any Internet web sites without the expressed written consent from the author or ATSU/KCOM Department Chairperson. Lymphoid Neoplasms: Two Major Groups •Precursor lymphoid neoplasms (acute leukemias/lymphomas) • B-ALLLBL • T-ALL/LBL •Mature lymphoid neoplasms • Non-Hodgkin lymphomas/leukemias • B-NHL • T/NK-NHL • Hodgkin lymphomas Leukemia vs. Lymphoma Acute versus Chronic Disease B-lymphocyte maturation From Hematopathology, E. Jaffee et. al., p.108, Saunders, 2010. Mature B-cell Neoplasms Diffuse Large B-cell Lymphoma B-lymphocyte development and function. Illustration by A. Y. Chen. Blood Journal, Nov. 2008. CLP, common lymphoid progenitor; SHM, somatic hypermutation; and CSR, class switch recombination. NHL – General Comments • Older age group than acute leukemia • Arise in lymph nodes or extranodal sites • Spread is unpredictable. • Staging not as useful as for HL. • +/- monoclonal protein • Many types Relative Frequencies of Mature B-cell Lymphomas in Adults From: S. Swerdlow et. al., WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed., 2008, IARC Press, p. 164 Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma • Most common leukemia in adults. • Older adults, M>F • Involves peripheral blood and bone marrow (if leukemia) • +/- involvement of lymph nodes, liver, spleen and other sites. • Fatigue, autoimmune hemolytic anemia, infections, +/- M-protein CLL/SLL lymphadenopathy CLL/SLL: Peripheral blood Smudge cell CLL/SLL: Lymph Node CLL/SLL: Bone Marrow Maslak, P. ASH Image Bank 2009 CLL/SLL Natural History • About 1/3 never need therapy. • About 1/3 will eventually need therapy. • About 1/3 will immediately need therapy. • Rai or Binet staging system. • Prognosis depends upon stage, performance status, molecular/cytogenetic markers, and the presence/absence of transformation. RAI BINET • 0: Lymphocytosis in blood and marrow • 1: Lymphocytosis and lymphadenopathy • II: Lymphocytosis and hepatosplenomegaly • III: Lymphocytosis and anemia • IV: Lymphocytosis and thrombocytopenia • A: No cytopenia; <3 lymphoid areas enlarged • B: No cytopenia; >3 lymphoid areas enlarged • C: Anemia or thrombocytopenia present CLL/SLL Staging CLL Progression Richter Transformation to DLBCL CLL-Prolymphocytic Leukemia Diffuse Large B-Cell Lymphoma • 30-40% of all non-Hodgkin’s lymphomas • Middle age and elderly, most commonly. • Usually arises de novo. • Secondary cases have worse prognosis. • Underlying immunodeficiency = risk factor. • Aggressive. Requires therapy DLBCL Risk Factors: • Infection • Immunodeficiency • Autoimmune disease • Pre-existing low-grade B-cell lymphoma Diffuse Large B-Cell Lymphoma DLBCL: Morphology Size Assessment Centroblastic Variant Immunoblastic Variant Anaplastic Variant DLBCL variants (taken at different magnification) Follicular Lymphoma •Second most common NHL in U.S. •Middle age – older adults •t(14;18)(q32;q21) in most •Indolent but incurable. •Most present at late stage. •Old grading system = 3 grades •New grading system = 2 grades •May undergo Richter transformation. Follicular Lymphoma: Gross Spleen with many small nodules Lymph node. “Fish flesh”, nodular Scanning view of lymph node Centroblasts (large cells) and centrocytes (small cleaved cells) Follicular Lymphoma Low grade (1-2) High grade (3) Follicular Lymphoma Neoplastic follicle (white open arrow, lower left) is positive for Bcl-2 stain. Normal follicle (white closed arrow, upper center) is negative. Immunostain for Bcl-2 Follicular Lymphoma in Blood—”Buttock” cells Plasma Cell Neoplasms •Neoplasms of terminally-differentiated B-lymphocytes (plasma cells) •Middle-aged to elderly persons •Usually secrete monoclonal immunoglobulin. •May be preceded by monoclonal gammopathy of uncertain significance (MGUS). Myeloma •Malignant cells suppress proliferation of normal plasma cells. •Death usually from bleeding or infection. •Renal failure is common. •DX based on combination of pathological, clinical, and radiologic findings: bone marrow plasmacytosis, osteolytic bone lesions, monoclonal gammopathy, end-organ damage Punched out appearance of skull Myeloma Lytic lesions in skull Normal Serum Protein Electrophoresis Pattern Serum Protein Electrophoresis with Monoclonal Protein M-protein Hypogammaglobulinemia Serum Protein Electrophoresis IgG Kappa on Immunofixation serum urine Peripheral blood: Rouleaux Atypical plasma cells on aspirate. Appearance on the biopsy Myeloma Anaplastic myeloma, aspirate Anaplastic myeloma, biopsy Anaplastic Myeloma Amyloidosis -- Pathogenesis Perivascular Amyloid – H&E stain Perivascular Amyloid – Congo Red Amyloid Plasmacytomas: Solitary Neoplasms of Monoclonal Plasma Cells • Extraosseous. Arise outside of bone marrow. 3-5% of plasma cell neoplasms. • Intraosseous. Arise within bone marrow. 3-5% of plasma cell neoplasms. • No clinical features of myeloma. • Normal immunoglobulins. • No anemia, hypercalcemia, or renal failure. • Treat both types with radiotherapy. Extraosseous plasmacytoma •Most are in upper respiratory tract and sinuses. •+/- low levels of monoclonal protein. •Good prognosis. About 70% are disease-free after 10 yrs. Solitary Plasmacytoma of Bone Small M-protein in up to 70%. •Frequently present with pain at site; may have fractures. •Up to 2/3 evolve into myeloma or additional plasmacytomas. Lymphoplasmacytic Lymphoma and Waldonstrom Macroglobulinemia • Rare lymphoma • Older adults, slight male predominance • Majority have M-protein, usually IgM (Waldenstrom macroglobulinemia). • Hyperviscosity in <30%. • Involves bone marrow. • May involve other organs. • Incurable Lymphoplasmacytic Lymphoma Purpuric rash Lymphoplasmacytic Lymphoma and Waldonstrom Macroglobulinemia Extranodal Marginal Zone Lymphoma of MALT Type (MALT lymphoma) •Generally arise in chronic inflammatory disorders. •Associated with Helicobacter pylori in stomach. •Usually occur in adults. •Indolent course. Usually localized early, widespread in late stages. Extranodal Marginal Zone Lymphoma of MALT Type Mantle Cell Lymphoma • Middle-aged to older patients • Male predominance. • Lymph nodes most common • Spleen and marrow, +/- blood involvement, or GI involvement • Most patients present in late stage. • Median survival 3-5 years. Incurable • t(11;14)(q13;q32), overexpression of cyclin-D1. Mantle Cell Lymphoma Lymph node. Low power magnification Lymph node. High power magnification Starry sky appearance. Macrophages, apoptotic cells. Blastoid Mantle Cell Lymphoma Burkitt Lymphoma Above: Massive involvement of ovaries by Burkitt lymphoma Left: Lymphomatous involvement of the face by Burkitt lymphoma Endemic Sporadic • Equatorial Africa. • Mainly in children • Jaw and facial bone involvement common. Also gonadal, breast, abdominal sites. • Geographic location corresponds to malaria. • Worldwide, low incidence • Children and young adults • Abdominal tumors most common; also gonads, kidneys and breast. Jaw tumors are rare. • EBV positive in about 30% Burkitt Lymphoma Burkitt Lymphoma, Immunodeficiencyassociated • Mainly seen in adults. • Mainly seen in association with HIV/AIDS. • Post-transplant • Iatrogenic (drugs for autoimmune dz) • Involves lymph nodes and bone marrow in most. • EBV positivity varies with cause. Burkitt Lymphoma Pathogenesis • Immunophenotype: • Mature B-cell markers (CD19, CD20, CD10, BCL6, CD38) • CD34 and TdT are uniformly negative. (Not blasts.) • Possibly is a polymicrobial disease (malaria, arboviruses, EBV). t(8;14) is characteristic. Burkitt Lymphoma: “Starry Sky” Burkitt Lymphoma/Leukemia Bone Marrow Aspirate • May have leukemic involvement. • Cells look blast-like. • Deeply basophilic cytoplasm, usually with many lipidcontaining vacuoles • Immunophenotype of more mature B-cells