- The Journal of Arthroscopic and Related Surgery
advertisement

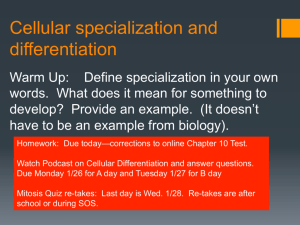
Can Arthroscopically Harvested Synovial Stem Cells Be Preferentially Sorted Using Stage-Specific Embryonic Antigen 4 Antibody for Cartilage, Bone, and Adipose Regeneration? Jingting Li, M.S., Douglas D. Campbell, B.S., George K. Bal, M.D., and Ming Pei, M.D., Ph.D. Purpose: The aim of this study was to investigate the relation between stage-specific embryonic antigen 4 (SSEA4) expression and synovium-derived stem cell (SDSC) lineage differentiation. Methods: Human SDSCs were collected during arthroscopic surgery from 4 young patients with anterior cruciate ligament injuries. Passage 2 SDSCs were sorted by fluorescence-activated cell sorting using phycoerythrin-conjugated monoclonal antibody against SSEA4 into 3 groups: SSEA4(þ) cells, SSEA4() cells, and unsorted control cells. After 1 more passage, expanded cells from each group were evaluated for SSEA4 expression by use of flow cytometry as well as multilineage differentiation capacities, including chondrogenesis, adipogenesis, and osteogenesis, using biochemical analysis, histologic analysis, immunostaining, and realtime polymerase chain reaction. Results: After cell sorting, 1 more passage expansion decreased SSEA4(þ) cells from 99.8% to 79.2% and increased SSEA4() cells from 4.4% to 53.3% compared with 70.3% in the unsorted cell population. SSEA4() SDSCs with a lower cell proliferation exhibited higher chondrogenic potential (in terms of the ratio of glycosaminoglycan to DNA [P < .001] and COL2A1 [type II collagen] messenger RNA [mRNA] [P < .001]) and adipogenic potential (in terms of oil red O staining and quantitative assay [P ¼ .007], LPL [lipoprotein lipase] mRNA [P ¼ .005], and CEBP [CCAAT/enhancer-binding protein alpha] mRNA [P ¼ .010]). In contrast, SSEA4(þ) SDSCs retained cell expansion and enhanced osteogenic capacity, as evidenced by intense calcium deposition stained by alizarin red S and a significantly elevated expression of OPN (osteopontin) mRNA (P ¼ .007). Conclusions: In this study, for the first time, we showed the benefit of using the surface marker SSEA4 in SDSCs to preferentially sort a mixed population of cells. SSEA4(þ) SDSCs indicated a strong potential for osteogenesis rather than chondrogenesis and adipogenesis. Clinical Relevance: SDSCbased mesenchymal tissue regeneration can be easily achieved by arthroscopic harvesting followed by quick cell sorting. M esenchymal stem cells (MSCs) are a unique population of adult stem cells that have the ability to differentiate into multiple lineages, such as bone, fat, and cartilage. Recent clinical trials using MSC cellular From the Stem Cell and Tissue Engineering Laboratory, Department of Orthopaedics (J.L., D.D.C., G.K.B., M.P.), Department of Exercise Physiology (J.L., M.P.), and Department of Mechanical & Aerospace Engineering (M.P.), West Virginia University, Morgantown, West Virginia, U.S.A. This project was partially supported by research grants from the West Virginia University Senate Research Grant Award (R-12-010), the AO Foundation (S-12-19P), the Musculoskeletal Transplant Foundation, and the National Institutes of Health R03 Program (1 R03 AR062763-01A1 and 5 R03 DE021433-02). The authors report that they have no conflicts of interest in the authorship and publication of this article. Received July 3, 2013; accepted December 16, 2013. Address correspondence to Ming Pei, M.D., Ph.D., Stem Cell and Tissue Engineering Laboratory, Department of Orthopaedics, West Virginia University, PO Box 9196, One Medical Center Drive, Morgantown, WV 265069196, U.S.A. E-mail: mpei@hsc.wvu.edu Ó 2014 by the Arthroscopy Association of North America 0749-8063/13457/$36.00 http://dx.doi.org/10.1016/j.arthro.2013.12.009 352 therapies have shown considerable promise and a broad therapeutic potential in regenerative treatment of many common diseases.1 MSCs of synovial origin, referred to as synovium-derived stem cells (SDSCs), have been found to display an enhanced capability for chondrogenesis when compared with MSCs from other origins, supporting the notion of a tissue-specific stem cell for articular cartilage regeneration.2-6 SDSCs may be easily acquired under arthroscopic observation with a small punch biopsy providing sufficient cells for clinical use.7 Although MSCs may be harvested from a wide variety of sources, such as bone marrow, adipose, periosteum, muscle, perichondrium, and synovium, it has been challenging to isolate and purify them because of limited selectivity of available markers.6,8 Specific surface markers for identifying MSCs with high self-renewal and desired lineage differentiation have potential for clinical applications. A recent article reviewed potential markers that may serve to indicate enhanced chondrogenic differentiation capabilities of SDSCs.9 One such surface marker that has gathered interest is the glycolipid stage-specific embryonic Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 30, No 3 (March), 2014: pp 352-361 SSEA4-SORTED SDSC DIFFERENTIATION antigen 4 (SSEA4). This antigen, previously used as a marker for embryonic stem cell identification, has recently been discovered to also serve as a marker for MSCs.10 Recent studies indicated that human synovium-derived stem cells (hSDSCs) and human bone marrow stromal cells (hBMSCs) expanded on decellularized stem cell matrix (DSCM) exhibited an upregulation of SSEA4 expression with concomitantly enhanced self-renewal and chondrogenic potential.11-13 These observations motivated us to investigate the relation between the surface marker SSEA4 expression and hSDSC lineage differentiation. The aim of this study was to investigate the relation between SSEA4 expression and SDSC lineage differentiation. We hypothesized that SSEA4 as a surface marker could preferentially sort hSDSC populations with lineage differentiation potentials for cartilage, bone, and adipose tissue regeneration. Methods Preparation of hSDSCs Random biopsy specimens from the intimal layer of synovial tissue were obtained aseptically during arthroscopic surgery from the knees of 4 young patients (3 men and 1 woman; mean age, 23 years) with anterior cruciate ligament injuries. The inclusion criteria were specified as patients aged between 18 and 30 years and undergoing knee arthroscopy. The exclusion criteria included patients with any history of inflammatory arthropathy, previous knee surgery, immunodeficiency, connective tissue disorders or septic arthritis, and chronic infection (bacterial, fungal, or viral). This project was approved by the institutional review board (protocol H-23564), and consent was obtained from each patient before the deidentified sample was collected. The method for digesting synovial tissue was described previously.6 In brief, after temporary storage in culture medium at 4 C, the synovial tissue was finely minced and digested at 37 C for 30 minutes in phosphate-buffered saline solution (PBS) containing 0.1% trypsin and then for 2 hours in a 0.1% solution of collagenase P in alpha modified eagle medium/10% fetal bovine serum (FBS). The cell suspension was passed through a 70-mm nylon filter, and the cells were collected from the filtrate by centrifugation. Cells were cultured in growth medium (alpha modified eagle medium/10% FBS, 100-U/mL penicillin, 100-mg/mL streptomycin). Nonadherent cells were removed by a PBS wash on days 2 and 4. SSEA4-Based Cell Sorting Passage 2 hSDSCs were labeled with phycoerythrinconjugated monoclonal antibody against SSEA4 (BioLegend, San Diego, CA) in PBS without Ca2þ and Mg2þ supplemented with 2.5-mmol/L EDTA, 1% FBS, and 25-mmol/L N-(2-hydroxyethyl)-piperazine-N0 -2ethanesulfonic acid (HEPES), followed by cell sorting with FACSAria (BD Biosciences, San Jose, CA) into 3 353 groups: SSEA4(þ) cells, SSEA4() cells, and unsorted cells serving as a control. Phycoerythrin was excited at 488 nm by an argon ion laser, and fluorescence was detected by use of a 575/26 filter. Dead cells were excluded by gating on forward and side scatter. Data were analyzed by the FCS Express 3 software package (De Novo Software, Los Angeles, CA). All sorted and unsorted cells were expanded for 1 more passage and were then evaluated for SSEA4 expression by use of flow cytometry as well as multilineage differentiation capacities, including chondrogenesis, adipogenesis, and osteogenesis, using biochemical analysis, histologic analysis, immunostaining, and real-time polymerase chain reaction (PCR). Multilineage Induction and Differentiation Analysis Chondrogenic Induction. As described in our previous study,12 3 105 hSDSCs from each group were centrifuged at 500g for 5 minutes in a 15-mL polypropylene tube to form a pellet. After overnight incubation, the pellets were transferred to a serum-free chondrogenic medium consisting of high-glucose Dulbecco modified eagle medium, 40-mg/mL proline, 107-mol/L dexamethasone, 100-U/mL penicillin, 100-mg/mL streptomycin, 0.1mmol/L ascorbic acid-2-phosphate, and 1 ITS Premix (6.25-mg/mL insulin, 6.25-mg/mL transferrin, 6.25-mg/mL selenous acid, 5.35-mg/mL linoleic acid, and 1.25-mg/mL bovine serum albumin; BD Biosciences) with the supplementation of 10-ng/mL transforming growth factor b3 (PeproTech, Rocky Hill, NJ) in a 37 C, 5% CO2/ 5% O2 incubator for up to 27 days. On days 0 and 27, pellets from each group were collected for evaluation of chondrogenic differentiation by histochemistry, immunohistochemistry, biochemistry, and quantitative real-time PCR. Histochemistry and Immunohistochemistry. The pellets (n ¼ 2) were fixed in 4% paraformaldehyde at 4 C overnight, followed by dehydrating in a gradient ethanol series, clearing with xylene, and embedding in paraffin blocks. Five-micrometer sections underwent histochemical staining with alcian blue (Sigma-Aldrich, St. Louis, MO) (counterstained with fast red) for sulfated glycosaminoglycans (GAGs). For immunostaining, the sections were immunolabeled with primary antibodies against type I collagen (Abcam, Cambridge, MA) and type II collagen (II-II6B3; Developmental Studies Hybridoma Bank, Iowa City, IA), followed by the secondary antibody of biotinylated horse anti-mouse immunoglobulin G (Vector Laboratories, Burlingame, CA). Immunoactivity was detected by use of Vectastain ABC reagent (Vector Laboratories) with 3,30 diaminobenzidine as a substrate. Biochemical Analysis for DNA and GAG Content. The pellets (n ¼ 4) were digested at 60 C for 6 hours with 125mg/mL papain in PBE buffer (100-mmol/L sodium phosphate buffer and 10-mmol/L EDTA, pH 6.5) 354 J. LI ET AL. containing 10-mmol/L cysteine. To quantify cell density, the amount of DNA in the papain digestion was measured with the Quant-iT PicoGreen dsDNA Assay Kit (Invitrogen, Carlsbad, CA) with a CytoFluor Series 4000 (Applied Biosystems, Foster City, CA). GAG was measured by use of dimethylmethylene blue dye and a Spectronic BioMate 3 Spectrophotometer (Thermo Scientific, Milford, MA) with bovine chondroitin sulfate (Sigma-Aldrich) as a standard. Adipogenic Induction. Expanded hSDSCs were replated at 10,000 cells/cm2 in T25 flasks. Once cells reached 100% confluence, the culture medium was switched to adipogenic induction medium consisting of growth medium supplemented with 1-mmol/L dexamethasone, 0.5-mmol/L isobutyl-1-methyxanthine, 200-mmol/L indomethacin, 10-mg/mL insulin, and 1-nmol/L 3,30 50 triiodo-L-thyronine for an additional 21 days. Oil red O (ORO) staining and quantitative assays were conducted as described previously.12 In brief, adipogenically induced hSDSCs (n ¼ 3) were fixed in 4% paraformaldehyde for 60 minutes and stained with 0.3% ORO solution (Sigma-Aldrich) for 30 minutes. After rinsing in distilled water, cells were photographed with an AmScope Microscope Digital Camera (model MD1900; iScope, Irvine, CA). ORO was extracted from cells using 100% isopropanol, and the absorbance was determined at 510 nm. For a blank control, we used 100% isopropanol. The ORO optical density value was normalized by total DNA content. TaqMan real-time PCR was used for quantification expression of adipogenic marker genes. Osteogenic Induction. Expanded hSDSCs were replated at 8,000 cells/cm2 in T25 flasks. Once cells reached 90% confluence, the culture medium was switched to osteogenic induction medium consisting of growth medium supplemented with 0.01-mmol/L dexamethasone, 10mmol/L b-glycerol phosphate, 50-mmol/L ascorbate-2phosphate, and 0.01-mmol/L 1,25-dihydroxyvitamin D3 for an additional 21 days. Osteogenic differentiation was assessed by use of alizarin red S (ARS) staining for calcium deposition and TaqMan real-time PCR for quantification expression of osteogenic marker genes.12 In brief, osteogenically induced hSDSCs (n ¼ 3) were fixed with 70% ice-cold ethanol for 1 hour and then incubated in 40-mmol/L ARS at pH 4.2 for 20 minutes at room temperature with agitation on an orbital shaker (60 rpm). After 2 rinses with deionized water, matrix mineral-bound staining was photographed under a Nikon TE300 Inverted Phase Contrast Microscope (Nikon, Tokyo, Japan). Accumulated calcium was extracted using 0.5 mL of 0.5 N hydrochloric acid and quantified according to the manufacturer’s instructions in a QuantiChrom Calcium Assay Kit (BioAssay Systems, Hayward, CA). Total calcium was calculated from standard solutions prepared in parallel and normalized to the total protein content. The values of blank controls were subtracted from the corresponding samples. TaqMan Quantitative PCR. As described previously,12 total RNA was extracted from the samples (n ¼ 4) using a ribonuclease-free pestle in TRIzol (Invitrogen). Two micrograms of messenger RNA (mRNA) was used for reverse transcriptase with the High-Capacity cDNA Archive Kit (Applied Biosystems) at 37 C for 120 minutes. Chondrogenic marker genes (COL1A1 [assay ID Hs00164004_m1] and COL2A1 [assay ID Hs00156568_m1]); adipogenic marker genes (LPL [lipoprotein lipase] [assay ID Hs00173425_m1] and CEBP [CCAAT/enhancer-binding protein alpha] [assay ID Hs00269972_m1]); and an osteogenic marker gene (OPN [osteopontin] [assay ID Hs01587814_g1]) were purchased from Applied Biosystems. Eukaryotic 18S ribosomal RNA (assay ID HS99999901_s1) was carried out as the endogenous control gene. Real-time PCR was performed with the iCycler iQ Multi-Color RealTime PCR Detection System (Biorad, Hercules, CA), and the data were calculated with computer software (PerkinElmer, Wellesley, MA). Relative transcript levels were calculated as c ¼ 2DDCt, in which DDCt ¼ DE DC, DE ¼ Ctexp Ct18s, and DC ¼ Ctct1 Ct18s. Power Analysis Estimation of the sample size and power for this study was performed with JMP software (SAS Institute, Cary, NC). Previous results obtained in our laboratory indicated differences in both GAG amount (obtained by biochemical analysis) and chondrogenic marker genes (COL1A1, COL2A1, LPL, CEBP, and OPN, evaluated by TaqMan quantitative PCR) of approximately 5 times their within-group standard deviations (signal-to-noise ratio). We had 4 samples per group, which provided 82% power. Statistical Analysis Numerical data are presented as the mean and standard error of the mean. The Mann-Whitney U test was used for pair-wise comparison in biochemistry, ORO assay, and real-time PCR data analysis. All statistical analyses were performed with SPSS statistical software (version 13.0; SPSS, Chicago, IL). P < .05 was considered statistically significant. Results Sorting Mixed Population of SDSCs Into Distinct Populations With SSEA4 After cell sorting by flow cytometry, as shown in Fig 1, the percentage of SSEA4-positive cells was 99.8% in the sorted SSEA4(þ) group and 4.4% in the sorted SSEA4() group, distinct from 73.4% in the unsorted cells. After 1 more passage expansion from the sorted SSEA4-SORTED SDSC DIFFERENTIATION 355 Fig 1. Flowchart of research design. Passage 2 hSDSCs labeled with phycoerythrin-conjugated SSEA4 were sorted by fluorescenceactivated cell sorting. The SSEA4 expression pattern showed 3 populations: SSEA4()/SSEA4(þ)1, SSEA4(þ)2, and SSEA4(þ)3. SSEA4() and SSEA4(þ)2 hSDSCs were chosen to have cells with a more uniform SSEA4 expression. SSEA4 expression levels in both the positive (99.8%) and negative (4.4%) groups were confirmed after sorting. Both sorted groups were expanded for another passage with unsorted cells serving as a control; the SSEA4 percentages in the unsorted cells, SSEA4(þ) cells, and SSEA4() cells were 70.3%, 79.2%, and 53.3%, respectively. Expanded cells from all 3 groups were induced in chondrogenic, adipogenic, or osteogenic medium before analysis. (FL2-H: fluorescence intensityheight; PE-A, phycoerythrinabsorbance.) cells, we found that, compared with 70.3% in the unsorted cells, SSEA4-positive cells decreased to 79.2% in the SSEA4(þ) group and increased to 53.3% in the SSEA4() group. Compared with a slight increase in the SSEA4(þ) group, the cell number dramatically decreased to 57.0% in the SSEA4() group, suggesting that SSEA4 is a positive indicator for stem cell proliferation. SSEA4(D) Expression Does Not Favor hSDSC Chondrogenesis After 27 days of chondrogenic induction, cell pellets from the SSEA4(þ), SSEA4(), and unsorted population groups were analyzed and compared for their ability to grow cartilage. Morphologic analysis included staining for sulfated GAG with alcian blue (Fig 2A), as well as immunohistochemical staining for type II collagen (Fig 2B) and type I collagen (Fig 2C). Size differences were found to exist between the pellets, with the SSEA4() population producing a visibly larger pellet than the SSEA4(þ) population. This finding suggests that enhanced chondrogenesis occurred in the SSEA4() population of cells because of the larger pellet formed. Biochemical analysis (Fig 2D) allowing for the quantification of DNA and GAG to assess the ratio of GAG to DNA, otherwise known as the chondrogenic index, showed the amount of DNA present as well as the significantly elevated chondrogenic index observed in the SSEA4() population compared with the SSEA4(þ) population (1.493 0.086 ug/ug v 1.173 0.015 ug/ug, n ¼ 4, P < .001). Real-time PCR 356 J. LI ET AL. Fig 2. Chondrogenic induction and evaluation of SSEA4-sorted hSDSCs. After cell sorting, unsorted (control) and sorted [SSEA4(þ) and SSEA4()] cells were expanded for 1 more passage. The expanded cells were cultured in a pellet system supplemented with a serum-free chondrogenic induction medium for 27 days. (A) Alcian blue (AB) staining was used for sulfated GAG, (B) immunohistochemistry (IHC) was for type II collagen (Col II), and (C) type I collagen (Col I). (Original magnification 100.) Quantitative data included (D) biochemical analysis (DNA and GAG amount as well as ratio of GAG to DNA [i.e., chondrogenic index]), (E) real-time PCR analysis for COL2A1, and (F) COL1A1 mRNAs. Data are shown as mean standard deviation (n ¼ 4). The asterisks indicate significant differences (P < .05). data were consistent with the previously mentioned histologic and biochemical data. COL2A1 mRNA was found to have significantly elevated levels in the SSEA4() population relative to the SSEA4(þ) population (4.280 0.124 v 1.001 0.048, n ¼ 4, P < .001) (Fig 2E). Alternatively, the COL1A1 mRNA level was found to be significantly elevated in the SSEA4(þ) population compared with the SSEA4() population (1.000 0.024 v 0.554 0.008, n ¼ 4, P < .001) (Fig 2F). SSEA4(D) Expression Does Not Favor hSDSC Adipogenesis After 21 days of adipogenic induction, the quantitative data from ORO staining (Fig 3A) showed that there was significantly more ORO staining in the SSEA4() population than in the SSEA4(þ) population (1.145 0.142 v 0.695 0.062, n ¼ 4, P ¼ .007) (Fig 3B). Realtime PCR data showed that both the LPL and CEBP genes were found to be expressed at significantly higher levels in the SSEA4() population relative to the SSEA4(þ) population (1.230 0.049 v 1.001 0.053, n ¼ 4, P ¼ .005, and 1.162 0.037 v 1.001 0.049, n ¼ 4, P ¼ .010, respectively) (Fig 3C), supporting the results observed with ORO staining. SSEA4(D) Expression Benefits hSDSC Osteogenesis After 21 days of osteogenic induction, ARS staining showed that SSEA4(þ) cells produced distinct bone nodules with extensive calcium staining; very little, if any, calcium staining was seen in the SSEA4() population (Fig 4A). The SSEA4(þ) population also displayed a significantly elevated expression of OPN relative to the SSEA4-SORTED SDSC DIFFERENTIATION 357 Fig 3. Adipogenic induction and evaluation of SSEA4-sorted hSDSCs. (A) After cell sorting, unsorted (control) and sorted [SSEA4(þ) and SSEA4()] cells were expanded for 1 more passage. The expanded cells were incubated in an adipogenic induction medium for 21 days. (B) ORO staining was used for lipids. (Original magnification 200.) Quantitative data included biochemical analysis (ORO optical density [OD] adjusted by total DNA content). (C) Real-time PCR analysis for LPL and CEBP mRNAs (adipogenic markers). Data are shown as mean standard deviation (n ¼ 4). The asterisks indicate significant differences (P < .05). SSEA4() population (1.010 0.173 v 0.462 0.062, n ¼ 4, P ¼ .007) (Fig 4B). Discussion In this study we hypothesized that SSEA4 as a surface marker could preferentially sort hSDSC populations with lineage differentiation potentials for cartilage, bone, and adipose tissue regeneration. We found that SSEA4() SDSCs had lower proliferation but higher chondrogenic and adipogenic potential whereas SSEA4(þ) SDSCs showed retained proliferative and enhanced osteogenic abilities. The utility of the surface marker SSEA4 in identification of chondrogenic, adipogenic, and osteogenic differentiation of SDSCs could help us better understand its role in mesenchymal differentiation and potential clinical regenerative medicine applications. We chose hSDSCs as target cells in this study rather than hBMSCs because we expected to find an appropriate adult stem cell for cartilage repair; SDSCs are stem cells that are easily accessible and have a sufficient cell number and favorable differentiation capacity. Despite the fact that BMSCs were the first stem cells discovered14 with multilineage differentiation potentials,15 the harvesting process is an invasive technique and results in a low harvest rate. The colony formation rate of primary BMSCs is approximately 1/ 105 to 20/105, the lowest among MSCs from mesenchymal tissues.16 The tendency to develop hypertrophy and endochondral ossification when induced to undergo chondrogenesis also discouraged its application in cartilage regeneration.17 Unlike BMSCs, SDSCs are harvested from synovial tissue, which can be conducted by arthroscopy, a minimally invasive surgical procedure. According to Sakaguchi et al.,7 a mean of 21,000 cells/mg of synovium could be obtained, indicating that a small sample of synovium harvested with 358 J. LI ET AL. Fig 4. Osteogenic induction and evaluation of SSEA4-sorted hSDSCs. (A) After cell sorting, unsorted (control) and sorted [SSEA4(þ) and SSEA4()] cells were expanded for 1 more passage. The expanded cells were incubated in an osteogenic induction medium for 21 days. ARS staining was used for calcium deposition. (Original magnification 200.) (B) Quantitative data included real-time PCR analysis for OPN mRNA (osteogenic marker). Data are shown as mean standard deviation (n ¼ 4). The asterisk indicates a significant difference (P < .05). punch biopsy would be sufficient to obtain SDSCs for clinical treatment. The colony number for nucleated cells derived from synovium was 100-fold higher than that for cells from bone marrow. Those cells also achieved the highest colony-forming efficiency, fold increase, and growth kinetics among stem cells derived from bone marrow, adipose, muscle, and periosteum.18 SDSCs are also considered a tissue-specific stem cell for chondrogenesis, retaining stronger proliferative and chondrogenic potential.3 Despite the advantages of SDSCs over BMSCs for cartilage regeneration, like other stem cells, donor age and ex vivo expansion resulting in cell senescence are also challenges for the application of SDSCs in cartilage regeneration.19 Our recent findings indicated that DSCM could rejuvenate SDSCs during ex vivo cell propagation, enhancing cell proliferation and chondrogenic potential.20 This cell expansion system has been tested in primary chondrocytes and nucleus pulposus cells, as well as adult stem cells.11,20 Most recently, we found that the unique components and elasticity of DSCM deposited by fetal hSDSCs might be responsible for the rejuvenation of adult hSDSCs in terms of the lower apoptosis rate and higher proliferative and chondrogenic potentials.21 The combination of this expansion system with a growth factor (such as basic fibroblast growth factor [fibroblast growth factor 2]) and low oxygen (5% O2) contributed to a 36-fold cell number increase in only a 6-day expansion compared with the untreated control group without compromising SDSC chondrogenic potential.12 The previously mentioned evidence suggested that DSCM, a 3-dimensional matrix that can be deposited by a tissuespecific stem cell from young and healthy donors, is easily available through a decellularizing process, which shows promise for providing a sufficient number of highquality SDSCs for clinical applications. Recent findings showed that SSEA4 was expressed by human MSCs isolated from a variety of sources, including amniotic fluid,22 bone marrow,13,23 dermis,24 ligament,25 synovium,11,12 and umbilical cord blood.26 The existence of SSEA4 in many types of stem cells raises the question of whether SSEA4 levels represent a population in stem cells favoring a lineage-specific differentiation. Maddox et al.27 found that the level of SSEA4 in either human breast tissue stem cells or human abdominal adipose tissue stem cells (hASCs) remained relatively consistent with passaging. However, SSEA4-positive hASCs exhibited a higher potential for differentiation toward osteogenic and adipogenic cell lineages in vitro when compared with a mixed population.27 In an independent study using hASCs, Mihaila et al.28 found that SSEA4(þ) hASCs exhibited an enhanced capacity to differentiate into endothelial cells and osteoblasts. Consistent with these previous reports, our data showed that SSEA4(þ) SDSCs exhibited an enhanced osteogenic capacity. In this study we cannot explain the increase of SSEA4positive cells in the SSEA4() group after passaging; it could be because of the presence of a group of highly proliferative cells within the heterogeneous SDSC population, as in the findings of Karystinou et al.29 We also found that SSEA4() hSDSCs exhibited enhanced chondrogenic and adipogenic capacities. SSEA4(þ) did not favor hSDSC chondrogenesis, which is corroborated by a recent report that SSEA4 was not a marker for chondrogenic potential in cultured human chondrocytes and hBMSCs.30 An assumed shared pathway between adipogenesis and chondrogenesis in SSEA4() hSDSCs SSEA4-SORTED SDSC DIFFERENTIATION 359 Fig 5. Clinical perspectives using surface marker SSEA4 sorting for SDSC lineage differentiation. Synovial tissue is harvested by arthroscopy, followed by enzyme digestion to release SDSCs. If more cells are needed, cell expansion can be processed with the addition of growth factors (GFs) such as fibroblast growth factor 2 (FGF2) and/or DSCM. Fluorescence-activated cell sorting (FACS) can be used to preferentially separate SSEA4(þ) and SSEA4() cells for cartilage, bone, and adipose regeneration. was supported by a recent report that CD271(þ) SDSCs had greatly enhanced chondrogenic capabilities, as well as adipogenic potential.31 In BMSCs, various projects have shown that osteogenesis and adipogenesis appear to involve competing pathways. Most evidence to support this supposition comes from osteoporosis studies, in which increased bone marrow adipose tissue is known to correlate with decreased bone volume.32 More specifically, Li et al.33 showed the effects of overexpression of S100A16 resulting in a significant increase in ORO staining with a decrease in ARS staining and, vice versa, with decreasing expression of S100A16, suggesting direct and competing effects of osteogenesis and adipogenesis. In addition, hypoxic conditions have been found to affect MSC differentiation. Induction of the transcription factor hypoxia-inducible factor 1 has been found to enhance osteogenesis and inhibit adipogenesis in BMSCs.34 These findings suggest that certain proteins in BMSCs have the capability to simultaneously promote differentiation of 1 lineage fate while inhibiting differentiation of the competing lineage. Our findings suggest a similar scenario in SDSCs. When examining the amount of lipid staining in the sorted cell populations, as well as the adipogenic mRNA levels, we observed a significant elevation in the SSEA4() cells. Alternatively, calcium staining and osteogenic mRNA levels were elevated in the SSEA4(þ) cells. These data support the theory of competing pathways involved in adipogenic and osteogenic differentiation, despite the stem cell source used. Interestingly, it appears that the presence of the surface marker SSEA4 allows for a significant induction of SDSCs into bone formation, despite previous evidence that SDSCs have a reduced capability for osteogenesis.3 Our results are in line with previous reports showing that SSEA4 could be a positive marker for selecting BMSCs with higher proliferative and osteogenic potentials both in vitro and in vivo, which provide a useful tool for enumerating BMSCs in vivo.23,35 These data indicate the strong role of SSEA4 in osteogenesis and provide evidence of the benefit of using SSEA4 as a potential marker for stem cellebased bone regeneration. As summarized in Fig 5, synovial tissue can be easily obtained by minimally invasive arthroscopic procedures. Enzymatic digestion is able to release stem cells from synovium. If more cells are needed, the initial number of SDSCs can be magnified through the addition of growth factors such as fibroblast growth factor 2 and/or expansion using DSCM. Expanded cells can be quickly sorted based on surface marker SSEA4 staining 360 J. LI ET AL. using flow cytometry. Ultimately, these SSEA4(þ) and SSEA4() cells could be applied in autologous cartilage, bone, or fat regeneration. Limitations One limitation of this study was the unstable expression of SSEA4 in the sorted groups after cell expansion. Because of the insufficient cell number in the SSEA4() group available for multilineage differentiation evaluation, all 3 groups were expanded for 1 more passage. Flow cytometry was used to evaluate SSEA4 expression in expanded cells. We found that, compared with 70.3% in the unsorted cells, the SSEA4(þ) cells decreased the SSEA4 expression percentage from 99.8% to 79.2% whereas the SSEA4() cells had an increased percentage from 4.4% to 53.3%. Despite the fact that the change in SSEA4 expression after cell expansion was not what we expected, the difference of about 10% among the 3 groups [SSEA4(þ) > unsorted > SSEA4()] did contribute a significant difference in multilineage differentiation capacities. Given the enhanced osteogenic potential in the SSEA4() SDSC population and considering the inherent properties of SDSCs favoring chondrogenesis and BMSCs benefiting osteogenesis, it will be interesting to investigate whether this SSEA4-based cell sorting approach can concentrate the BMSC population with higher osteogenic capacity. The low number of patients tested in this study is also a limitation of our report. Because the focus was on the expression of SSEA4 in the overall SDSC population, synovial samples collected from 4 young patients were pooled for this study. The donor-to-donor variability will be explored in a future investigation. Conclusions In this study, for the first time, we showed the benefit of using the surface marker SSEA4 in SDSCs to preferentially sort a mixed population of cells. SSEA4(þ) SDSCs indicated a strong potential for osteogenesis rather than chondrogenesis and adipogenesis. This study provides evidence showing that SDSC-based mesenchymal tissue regeneration can be easily achieved by arthroscopic harvesting followed by quick cell sorting. Acknowledgment The authors thank Suzanne Danley for her help in editing the manuscript. References 1. Wagner J, Kean T, Young R, Dennis JE, Caplan AI. Optimizing mesenchymal stem cell-based therapeutics. Curr Opin Biotechnol 2009;20:531-536. 2. Bilgen B, Ren Y, Pei M, Aaron RK, Ciombor DM. CD14negative isolation enhances chondrogenesis in synovial fibroblasts. Tissue Eng Part A 2009;15:3261-3270. 3. Jones BA, Pei M. Synovium-derived stem cells: A tissuespecific stem cell for cartilage engineering and regeneration. Tissue Eng Part B 2012;18:301-311. 4. Pei M, He F, Boyce BM, Kish VL. Repair of full-thickness femoral condyle cartilage defects using allogeneic synovial cell-engineered tissue constructs. Osteoarthritis Cartilage 2009;17:714-722. 5. Pei M, He F, Kish V, Vunjak-Novakovic G. Engineering of functional cartilage tissue using stem cells from synovial lining: A preliminary study. Clin Orthop Relat Res 2008;466: 1880-1889. 6. Pei M, He F, Vunjak-Novakovic G. Synovium-derived stem cell-based chondrogenesis. Differentiation 2008;76: 1044-1056. 7. Sakaguchi Y, Sekiya I, Yagishita K, Muneta T. Comparison of human stem cells derived from various mesenchymal tissues: Superiority of synovium as a cell source. Arthritis Rheum 2005;52:2521-2529. 8. Nöth U, Rackwitz L, Steinert AF, Tuan RS. Cell delivery therapeutics for musculoskeletal regeneration. Adv Drug Deliv Rev 2010;62:765-783. 9. Campbell D, Pei M. Surface markers for chondrogenic determination: A highlight of synovium-derived stem cells. Cells 2012;1:1107-1120. 10. Yanagisawa M. Stem cell glycolipids. Neurochem Res 2011;36:1623-1635. 11. Li J, He F, Pei M. Creation of an in vitro microenvironment to enhance human fetal synovium-derived stem cell chondrogenesis. Cell Tissue Res 2011;345:357-365. 12. Li JT, Jones B, Zhang Y, Vinardell T, Pei M. Low density expansion rescues human synovium-derived stem cells from replicative senescence. Drug Deliv Transl Res 2012;2: 363-374. 13. Pei M, He F, Kish VL. Expansion on extracellular matrix deposited by human bone marrow stromal cells facilitates stem cell proliferation and tissue-specific lineage potential. Tissue Eng Part A 2011;17:3067-3076. 14. Friedenstein AJ. Precursor cells of mechanocytes. Int Rev Cytol 1976;47:327-359. 15. Muraglia A, Cancedda R, Quarto R. Clonal mesenchymal progenitors from human bone marrow differentiate in vitro according to a hierarchical model. J Cell Sci 2000;113: 1161-1166. 16. Castro-Malaspina H, Ebell W, Wang S. Human bone marrow fibroblast colony-forming units (CFU-F). Prog Clin Biol Res 1984;154:209-236. 17. Pelttari K, Winter A, Steck E, et al. Premature induction of hypertrophy during in vitro chondrogenesis of human mesenchymal stem cells correlates with calcification and vascular invasion after ectopic transplantation in SCID mice. Arthritis Rheum 2006;54:3254-3266. 18. Yoshimura H, Muneta T, Nimura A, Yokoyama A, Koga H, Sekiya I. Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res 2007;327:449-462. 19. Li JT, Pei M. Cell senescence: A challenge in cartilage engineering and regeneration. Tissue Eng Part B 2012;18:270-287. 20. Pei M, Li JT, Shoukry M, Zhang Y. A review of decellularized stem cell matrix: A novel cell expansion system for cartilage tissue engineering. Eur Cell Mater 2011;22:333-343; discussion 343. SSEA4-SORTED SDSC DIFFERENTIATION 21. Li JT, Hansen K, Zhang Y, et al. Rejuvenation of chondrogenic potential by young stem cell microenvironment. Biomaterials 2014;35:642-653. 22. De Coppi P, Bartsch G Jr, Siddiqui MM, et al. Isolation of amniotic stem cell lines with potential for therapy. Nat Biotechnol 2007;25:100-106. 23. Gang EJ, Bosnakovski D, Figueiredo CA, Visser JW, Perlingeiro RC. SSEA-4 identifies mesenchymal stem cells from bone marrow. Blood 2007;109:1743-1751. 24. Vaculik C, Schuster C, Bauer W, et al. Human dermis harbors distinct mesenchymal stromal cell subsets. J Invest Dermatol 2012;132:563-574. 25. Zhang J, Pan T, Im HJ, Fu FH, Wang JH. Differential properties of human ACL and MCL stem cells may be responsible for their differential healing capacity. BMC Med 2011;9:68. 26. Suila H, Pitkänen V, Hirvonen T, et al. Are globoseries glycosphingolipids SSEA-3 and -4 markers for stem cells derived from human umbilical cord blood? J Mol Cell Biol 2011;3:99-107. 27. Maddox JR, Ludlow KD, Li F, Niyibizi C. Breast and abdominal adipose multipotent mesenchymal stromal cells and stage-specific embryonic antigen 4 expression. Cells Tissues Organs 2012;196:107-116. 28. Mihaila SM, Frias AM, Pirraco RP, et al. Human adipose tissue-derived SSEA-4 subpopulation multi-differentiation potential towards the endothelial and osteogenic lineages. Tissue Eng Part A 2013;19:235-246. 361 29. Karystinou A, Dell’Accio F, Kurth TB, et al. Distinct mesenchymal progenitor cell subsets in the adult human synovium. Rheumatology 2009;48:1057-1064. 30. Schrobback K, Wrobel J, Hutmacher DW, Woodfield TB, Klein TJ. Stage-specific embryonic antigen-4 is not a marker for chondrogenic and osteogenic potential in cultured chondrocytes and mesenchymal progenitor cells. Tissue Eng Part A 2013;19:1316-1326. 31. Arufe MC, De la Fuente A, Fuentes I, De Toro FJ, Blanco FJ. Chondrogenic potential of subpopulations of cells expressing mesenchymal stem cell markers derived from human synovial membranes. J Cell Biochem 2010;111: 834-845. 32. Kawanabe N, Murata S, Fukushima H, et al. Stage-specific embryonic antigen-4 identifies human dental pulp stem cells. Exp Cell Res 2012;318:453-463. 33. Li D, Zhang R, Zhu W, et al. S100A16 inhibits osteogenesis but stimulates adipogenesis. Mol Biol Rep 2013;40: 3465-3473. 34. Wagegg M, Gaber T, Lohanatha FL, et al. Hypoxia promotes osteogenesis but suppresses adipogenesis of human mesenchymal stromal cells in a hypoxia-inducible factor1 dependent manner. PLoS One 2012;7:e46483. 35. Rosu-Myles M, McCully J, Fair J, et al. The globoseries glycosphingolipid SSEA-4 is a marker of bone marrowderived clonal multipotent stromal cells in vitro and in vivo. Stem Cells Dev 2013;22:1387-1397.