British Medical Bulletin Advance Access published February 21, 2008
Ocular regeneration by stem cells: present
status and future prospects
G. Astrid Limb* and Julie T. Daniels
UCL Institute of Ophthalmology, London EC1V 9EL, UK
Source of data: The review summarizes the achievements to date and the
present areas of stem cell investigations in the ophthalmic field, based on a
literature search and knowledge gained by the authors’ work in the subject.
Areas of agreement: Owing to its accessibility, the cornea constitutes an easy
anatomical target for stem cell regeneration. On this basis, limbal epithelial stem
transplantation is the only ocular cell-based therapy already in use in the clinical
setting.
Areas of controversy: Regeneration of the retina, a less accessible and complex
neural tissue, currently constitutes a major challenge. Investigations into the
potential use of stem cells for retina regeneration have generated variable data
and no therapies have yet been designed for human treatments.
Growing points: Despite the present limitations, it has been progressively
accepted that various stem cells may have potential use for the development of
cell-based therapies to restore retinal function.
Areas for research development: There is need to understand the cell
requirements and environmental conditions that may promote functional
integration and long-term survival of stem cells within the diseased retina. At
present, this constitutes a major area of research.
Keywords: retinal stem cells/Muller stem cells/limbal epithelial stem cells/
retina/cornea
Accepted: January 21,
2008
*Correspondence to:
Dr G. A. Limb, UCL
Institute of
Ophthalmology, 11 Bath
Street, London EC1V 9EL,
UK. E-mail: g.limb@ucl.ac.
uk
British Medical Bulletin 2008; 1–15
DOI:10.1093/bmb/ldn008
& The Author 2008. Published by Oxford University Press.
All rights reserved. For permissions, please e-mail: journals.permissions@oxfordjournals.org
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
Background: Advances in the stem cell field provide much hope for the use of
these cells in the regeneration of ocular tissue damaged by diseases for which
no treatments are yet available. Here, we discuss the current status and
limitations on the application of stem cells to ocular therapies, and consider the
future prospects for their use in the restoration of vision.
G. A. Limb and J. T. Daniels
Introduction
Page 2 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
Recent developments in the stem cell field have widened the prospects
of applying cell-based therapies to regenerate ocular tissues that have
been irreversibly damaged by disease or injury. In the clinical setting,
stem cell transplantation to repair and regenerate human corneal epithelium has been successfully used for several years.1 Understandably,
the corneal surface provides an easy anatomical site in which stem cellbased therapies can be implemented without using invasive methods.
This is not the case with less accessible and complex tissues responsible
for visual function, such as the neural retina and the retinal pigment
epithelium (RPE), for which many problems to establish such therapies
remain to be solved.
Different parts of the eye derive from different types of embryonic
tissue: the neurosensory retina and the RPE arise from the neuroectoderm, the corneoscleral and uveal tunics develop from the mesoderm
and the lens derives from the ectoderm.2 Therefore, regeneration of the
different ocular tissues poses a significant challenge due to their cellular
diversity and to the organization of neural networks found in the
retina and the optic nerve. In this context, the feasibility of regeneration may depend on the complexity of the tissue to be repaired. For
example, regeneration of RPE may provide a relatively easy target for
stem cell-based therapies as this constitutes a single cell monolayer.
The neural retina, however, may require more complex protocols for
its regeneration due to its multilayer structure of specialized neurons
and glial cells. During early disease, regeneration of a single neural cell
type may prove more feasible than in late disease when all types of
neurons have been compromised. Whichever the case, retinal repair
and regeneration may not only require a better understanding of the
molecular mechanisms that promote stem cell differentiation into functional neurons and glia, but also of the requirements for successful
migration, integration and survival of the transplanted cells. This is of
special importance as a retina in need of repair may have lost the developmental cues that allow permissiveness for neural integration, and it
is most likely to exhibit pro-inflammatory and gliotic barriers that
prevent successful regeneration by transplanted cells. Here we summarize the achievements to date in the field of stem cell therapies to treat
ocular disease, and draw attention to the existing hurdles that need to
be overcome in order to establish successful cell-based treatments to
restore visual function.
Ocular regeneration by stem cells
Retina
Stem cells and retinal development
Criteria for choosing the source of stem cells for human retinal transplantation
Early experimental studies in the 1980s to regenerate visual function
included the transplantation of whole eyes to genetically eyeless salamanders,12 the implantation of peripheral nerves into adult rat retina13
and the grafting of embryonic rat retina into a lesion site of adult rat
retinae.14 Since then, several approaches to regenerate retina have been
made in various experimental models of retinal degeneration using
British Medical Bulletin 2008
Page 3 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
It has been known for a long time that fish and amphibians have the
ability to regenerate neural retina throughout life, and that stem cells
capable of regenerating the retina in these species are located at the
ciliary margin.3 The presence of stem cells in the retinal ciliary margin
has also been documented in avians and small mammals,4 and more
recent studies have identified retinal stem cells in the same region of
the human eye.5 In addition, Müller glial cells have been shown to
have the potential to regenerate new neurons in response to acute
damage in the newly born chick6 and rat retina.7 That Müller glia
exhibit neurogenic characteristics in the adult eye have been further
supported by the unequivocal demonstration that in the adult zebra
fish, Müller glia form the retinal stem cell niche and that they are able
to generate retinal stem cells after retinal injury.8 Interestingly, more
recent investigations have identified a population of Müller glial cells
with stem cell characteristics in the adult human retina (illustrated in
Fig. 1),9 which suggests that the human retina, like in the zebrafish,
may have some potential for regeneration.
During development, Müller glia and retinal neurons share a
common progenitor that is multipotent at all stages of retinal histogenesis.10 This evidence derives from examination of the progeny of a
single mouse retinal progenitor cell transfected with a retrovirus, which
generated clones containing up to three types of neurons, whereas
others contained a combination of neurons and Müller glia, Müller
glia alone or a single type of neuron.10 Studies of retinal neurogenesis
in small vertebrates have shown that the generation of retinal neurons
follows an evolutionary conserved sequence, in which retinal ganglion
cells, cone photoreceptors, horizontal cells and a population of amacrine cells are born during early stages of retinal histogenesis, whereas
bipolar cells, Müller glia and most rod photoreceptors are born during
late stages of histogenesis.11
G. A. Limb and J. T. Daniels
stem cells derived from several sources. These include brain-derived
stem cells,15 embryonic retinal progenitor cells, ciliary epithelium and
stem cells from the postnatal eye,16 human embryonic stem cells,17
umbilical cord tissue cells and mesenchymal stem cells,18 bone marrow
stem cells19 and Müller stem cells9 (illustrated in Fig. 2). However,
despite intensive research in the field, to date there is no sufficient
evidence for widespread stem cell integration into the retina, long-term
graft survival or complete restoration of visual function.
The human neural retina, like any mammalian, is organized into three
different nuclear cell layers that harbour six different types of neurons
and circa 60 neuronal subtypes. The outer layer is populated by photoreceptor cells (light sensitive neurons); the middle layer (known as the
inner nuclear layer) homes bipolar, amacrine and horizontal cells and the
innermost layer (known as the ganglion cell layer) predominantly contains ganglion cells and displaced amacrine cells.20 Upon visual stimuli,
all retinal neurons undergo a complex cascade of neural interactions
through activation of synaptic pathways which finally lead to ganglion
Page 4 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
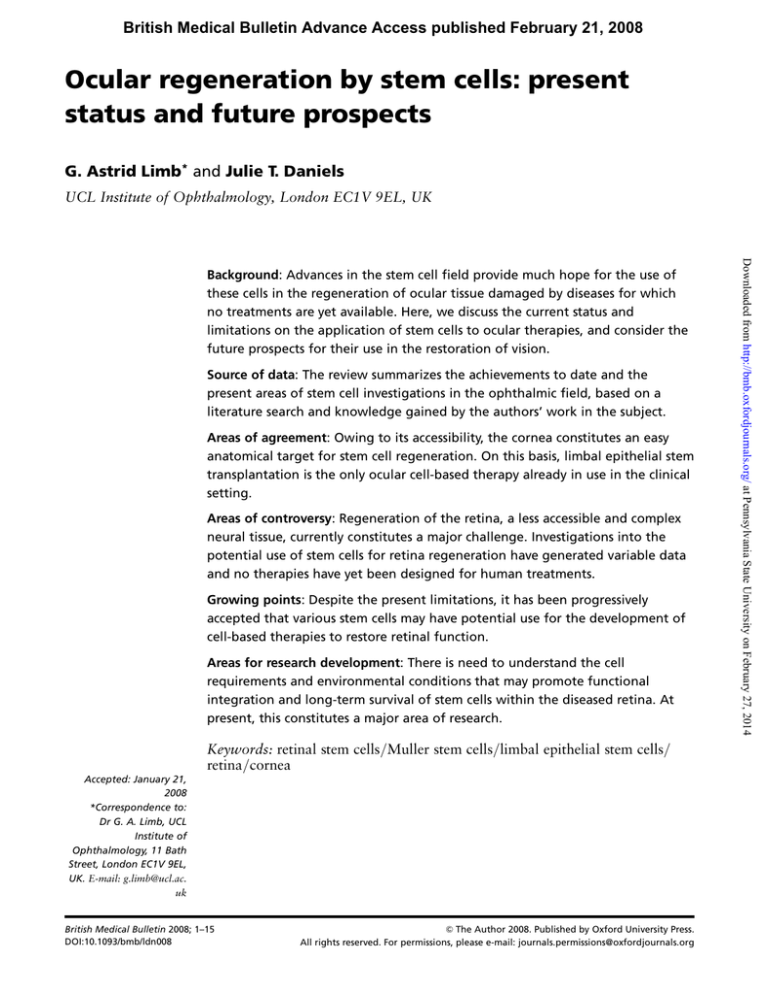
Fig. 1 Characteristics of human Müller stem cells in vitro. (A) Characteristic morphology of
human Müller stem cells in culture. (B) Upon culture on extracellular matrix and growth
factors, these cells form aggregates in vitro. They are known as neurospheres. Cells present
within the neurospheres stain for nestin (green), a marker of neural stem cells. (C) Müller
stem cells can be induced to express features of retinal neurons in vitro. Cells stained for
Sox2, a progenitor marker (red) and peripherin, a photoreceptor cell marker (green).
Ocular regeneration by stem cells
cells conveying visual messages via the optic nerve onto the brain. This
complex process requires intact axonal connections, which are lost
during retinal degeneration, and potential restoration of visual function
critically depends on whether transplanted neurons can re-establish the
dynamic neural network of the retina. Potential success of stem cellbased therapies may therefore depend on whether grafted cells can differentiate into the different retinal neurons, and whether these neurons can
re-establish normal synaptic pathways within the host retina.
Although significant progress has been made in recent years towards
the understanding of the molecular mechanisms that determine retinal
cell specification in fish, amphibians and small vertebrates, and there is
much overlap in the expression of progenitor markers in the developing
human retina with that of other species,5,9 it is well recognized that
there is still much to be learned about the signals that lead to specific
neuronal development in the human eye. In this context, although different types of stem cells can be potentially used for regeneration of the diseased human retina, it may be more appropriate, as suggested by recent
studies21 to use adult cells that have already undergone crucial developmental stages to make them committed to become retinal neurons. This
would bypass extensive procedures that may be needed for in vitro
differentiation of embryonic, haematopoietic, mesenchymal or brain
stem cells into retinal progenitor cells, especially since we do not know
in depth the molecular pathways needed for such differentiation. In
addition to the state of differentiation of stem cells potentially used for
British Medical Bulletin 2008
Page 5 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
Fig. 2 Müller stem cell transplantation in experimental models of retinal degeneration.
Following 2 weeks after transplantation of adult human Müller stem cells into the subretinal space of the dystrophic RCS rat, only a small number of transplanted cells (green) is
able to migrate and integrate into the retina. ONL, outer nuclear layer ( photoreceptor
cells); INL, inner nuclear layer. Red staining indicates the expression of recoverin, a protein
expressed by photoreceptor cells.
G. A. Limb and J. T. Daniels
transplantation, special consideration should be given to the environment in which stem cells are to be transplanted. Since the diseased retina
is not a permissive milieu in which stem cells could easily integrate, but
damaged tissue in need of repair, it also may be necessary to design
adjuvant therapies to modify the extracellular matrix to facilitate functional stem cell integration. As evidence for the existence of ‘adult’
retinal stem cells in the human eye has been presented, it is clear that
these cells may have advantages in terms of immediate clinical application, safety and feasibility for transplantation.
Retinal stem cells can be isolated and induced to proliferate in vitro
from the foetal and adult eye by enzymatic dissociation, followed by
culture in the presence of growth factors such as fibroblast growth
factor and epidermal growth factor.5,9 Several markers have been identified that allow the characterization of these cells, including nestin and
bIII tubulin,22,23 as well as various transcription factors and proteins
expressed by retinal stem cells during in vivo development. Some of the
most important factors known to characterize neural retina stem cells
include: (i) Sonic hedgehog protein (Shh), which in early development
promotes differentiation of progenitor cells into ganglion cells and acts
as a signalling molecule; (ii) Pax6, a regulatory factor that promotes
multipotency of retinal progenitor cells; (iii) Basic helix-loop-helix
(bHLH) transcription factors, such as Math 5 and NeuroD, which
upon activation drive progenitor cells towards the ganglion cell and
amacrine lineages, respectively; (iv) Chx10, one of the earliest markers
of the developing retina, which is required for retinal cell proliferation
and formation of bipolar cells and (v) Sox2, a transcription factor
found in early neurogenesis, which is down-regulated as cells differentiate and migrate to the different retinal cell layers.22,23 Expression of
Sox2 has also been shown in precursors of the human foetal retina and
constitutes an important marker of Müller stem cells in the adult
human eye.9 Other factors recognized to drive differentiation of retinal
progenitors include the receptors for fibroblast growth factors (FGF-R)
and epidermal growth factor (EGF-R), which play an important role in
neural and glial differentiation.23
Prevalent diseases that may potentially benefit from stem cell therapies
Neural cell death is the ultimate cause of blindness as a result of retinal
degenerative diseases, including age-related macular degeneration
Page 6 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
Characterization and isolation of retinal stem cells
Ocular regeneration by stem cells
Retinal pigment epithelium
The RPE constitutes a monolayer of pigmented cells attached to the
inner surface of the Bruch’s membrane. It is directly positioned over
the photoreceptor outer segments and plays an important role in
retinal homeostasis.26 RPE dysfunction occurs in severe retinal diseases
such as RP and AMD,27 for which stem cell transplantation to regenerate RPE cells may constitute a promising approach for treatment of
these diseases.
Major advances in the development of stem cell therapies to regenerate RPE have been made during the last few years, with the findings
that human embryonic stem cells provide a well-characterized and
reproducible source of RPE that could potentially be used for human
clinical studies.28 Transplantation of RPE derived from human embryonic cells have been transplanted in animal models of RPE degeneration
and has been shown to improve photoreceptor cell survival.29 On this
basis, extensive research on the potential of stem cells to regenerate
RPE cells for transplantation to patients with RP and AMD is being
actively pursued by several groups. Human RPE cells derived from
embryonic cells have not yet been used in the clinical setting, but with
the technology and knowledge available at present, it would not be
long before these cells can be applied to human therapies. However, as
with any other cell therapy, generation of these cells need to be performed under therapeutic conditions, and their safety and immunogenicity need to be examined before they can be applied to human
treatments.
British Medical Bulletin 2008
Page 7 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
(AMD), proliferative diabetic retinopathy (PDR), end-stage glaucoma,
retinitis pigmentosa (RP), proliferative vitreoretinopathy and inherited
retinal diseases. AMD is the leading cause of blindness in the western
world, affecting between 20 and 25 million people worldwide.24 It is
estimated that between 200 000 and 300 000 individuals in the UK are
registered as blind or partially sighted as a result of AMD.24 In
England and Wales, DR is the most common cause of blindness among
adults aged 16 –64, afflicting more than 35% of individuals after 20
years of diabetes.25 At present, treatments with anti-angiogenic factors,
laser photocoagulation and surgical treatments are only able to delay
visual loss in these patients, but in a long term, it is impossible to
prevent blindness finally occurring. On this account, the only hope for
restoration of sight is the development of stem cell-based therapies to
replace the damaged neurons and that could potentially integrate into
the remaining neuronal network.
G. A. Limb and J. T. Daniels
Cornea
Stem cell maintenance of corneal epithelium
Present approaches to corneal stem cell therapy
Ocular surface failure resulting from LESC deficiency can occur as the
result of primary (inherited eye disease) but more commonly as the
result of acquired factors, including chemical burn injury, contact lens
keratopathy, chronic limbitis, limbal surgery or Stevens– Johnson
Syndrome. When LESC deficiency occurs the neighbouring conjunctival epithelium, which is normal prevented from encroaching in the
corneal surface by the LESCs, migrates to cover the ocular surface in a
process known as conjunctivalization. When this happens, the patient
can experience repeated epithelial erosion, blood vessel growth across
the normally avascular cornea, inflammation, pain and eventual loss of
sight. Previous clinical approaches to the treatment of LESC deficiency
included autologous transplantation of limbal tissue from the
Page 8 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
The transparency of the cornea and therefore visual acuity is dependent
upon the integrity and functionality of the outermost layer, the epithelium. Corneal epithelial stem cells reside at the junction between the
cornea and neighbouring conjunctival epithelium in a region known as
the limbus. These cells, known as limbal epithelial stem cells (LESC),
are responsible for maintaining the corneal epithelium throughout life.
When a stem cell in the limbus divides in response to homeostatic cell
loss, it gives rise to transient amplifying cells which migrate, proliferate
and differentiate to populate the entire corneal epithelium. Evidence
for the corneal limbus being the source of an adult stem cell population
was first suggested by observations in the early 1970s that pigment in
the epithelium of heavily pigmented eyes migrated in lines from the
limbus to the central cornea in healed eccentric epithelial defects.30
The existence of slow-cycling limbal epithelial basal cells was later
confirmed by observations that cells localized at the limbus retained
tritiated thymidine label for long periods of time, a characteristic of
slow cycling stem cells.31 Detailed examination of the corneal limbus
niche has recently shown the existence of characteristic topographical
structures associated with concentrated deposits of LESCs, which
predominantly occur in the superior and inferior limbus.32 It is interesting to speculate that these regions, which are normally covered by
the upper and lower eye lids, have evolved to provide a degree of
protection to the stem cells from environmental insults such as ultraviolet light.
Ocular regeneration by stem cells
Fig. 3 LESC transplantation in the clinical practice. (A) Left eye of a patient affected by
Aniridia in which LESC failure had led to severe corneal opacity and neovascularization. (B)
The same eye 6 months after transplantation of allogeneic LESC cultured on human amniotic membrane. Note a much improved transparency and reduced vascularization. (Images
kindly provided by Mr AJ Shortt, Moorfields Eye Hospital, London.)
British Medical Bulletin 2008
Page 9 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
contralateral healthy eye to the diseased eye. Although successful, this
procedure carries the risk of creating LESC deficiency in the donor
eye.33 Alternatively, limbal tissue allografts have been performed using
living related or cadaveric donor material. However, due to the abundance of HLA-DR antigens and Langerhans cells in the graft, patients
must undergo long-term systemic immunosuppression.
In 1997, the first successful cultured stem cell therapy for LESC
failure was reported in two patients with chemical burn injuries.1 The
procedure involved the isolation and ex vivo expansion of autologous
LESCs from a 1 to 2 mm2 limbal biopsy for transplantation. The clinical outcome was promising with both patients experiencing improved
vision for at least 2 years (illustrated in Fig. 3).1 Since then a number
of centres around the world have employed the technique using a
variety of different cell culture protocols and carrier systems for transferring the cells to the patient, including the use of cultured LESCs
from allogeneic cadaveric donors.34
The various methods for LESC therapy production and reported
clinical outcomes have been comprehensively reviewed recently.35 The
overall success rate for the combined results of cultured autologous and
allogeneic LESC therapy treatments is 70%. The caveats to consider
when interpreting the reported data include the subjectivity of assessment in some studies, the differing aetiologies of LESC failure, the cell
culture protocols adopted, the myriad of previous ocular surgical interventions and the pre and post-operative management. Despite these
limitations, the data suggest that cultured LESC therapy is a beneficial
adjunct for the treatment of ocular surface failure.
At present, there is much research centered around the evaluation of
alternative stem cell sources for corneal stem cell transplantation,
including embryonic stem cells.36 One autologous cell source of
G. A. Limb and J. T. Daniels
significant interest is the oral mucosal epithelial cell (OMEC) or buccal
keratinocyte population. The first reports on the use of cultured
OMECs for the treatment of LESC deficient patients initially showed
promising results, but subsequent studies have shown that neovascularization can occur in some patients after transplantation.37 This indicates
that there is still a lot to be understood about the interactions between
the corneal stem cell and its niche environment with respect to regulation and function.
Despite the proliferative capacity of LESC, conclusive identification of
their specific markers has not yet been achieved. A number of ‘negative
limbal basal cell markers’ including absence of cytokeratins 3 and 12,
connexins and gap junctions have been proposed, along with ‘positive
limbal basal cell markers’ including co-localization of vimentin and
keratin 19, immuno-localization of the glycolytic enzyme alphaenolase, high levels of expression of epidermal growth factor (EGF)
receptors and expression of the transcription factors p63a, PAX6 and
Shh.38 Further investigations into the expression of specific markers by
LESC may aid in the identification of these cells and facilitate the diagnosis of LESC failure.
Clinical limitations and accessibility to LESC transplantation
The main clinical limitation to the use of cultured LESC therapy is the
availability of autologous donor tissue. Although cultured allogeneic
cells may be used in combination with systemic immuno-suppression,
there are indications that donor allogeneic LESCs do not survive in the
long term, and therefore immuno-suppression may not be required
beyond a period of 9 months.39 This was suggested by evidence that
donor DNA cannot be detected after these period, yet, patients maintain a corneal epithelium that appears to be of autologous origin.
These observations raise the interesting question about the mechanism
of cultured LESC therapy efficacy. It is possible that bone marrow stem
cells may be the source of the newly regenerated corneal epithelium, or
that the allogeneic cells may in some cases provide a permissive
environment for previously quiescent autologous LESCs to regain function. Key to the outcome of cultured LESC therapy in the cornea
appears to be the pre-operative management of inflammation and
infection both of which will compromise the efficacy of the treatment
if not fully controlled.35 In order to prospectively identify those
Page 10 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
Characterization of LESC
Ocular regeneration by stem cells
Other progenitor cells in the eye
Recent evidence shows that the conjunctiva is also a source of stem
cells. A detailed in vitro study of the clonogeneic properties of the
ocular surface epithelia revealed a uniform distribution of putative
stem cells in the bulbar and forniceal conjunctiva.40 It showed that
conjunctival epithelial and goblet cells derive from a common progenitor with high proliferative capacity that gives rise to goblet cells at least
twice during their life cycle and at precise moments prior to senescence. Conjunctival epithelial cell progenitors which can give rise to
goblet and non-goblet cell phenotypes have been cultured in vitro on
amniotic membrane and have been shown that like the LESC, are slow
cycling and label retaining. Cultured conjunctival epithelial cells,
thought to contain a proportion of stem cells, have been used to successfully treat patients with ocular surface damage.41
RPE and iris pigment epithelium from adult murine eyes, as well as
choroid and scleral cells from adult human eyes, have been shown to
de-differentiate in vitro to express antigens of retinal neurons.
However, the capacity of long-term cell renewal and evidence that they
constitute a true population of stem cells has not yet been proven. In
addition, there is some evidence that LESC exhibit neural plasticity,42
raising the possibility of exploring these cells to generate retinal neural
progenitors.
Other recent studies have identified a population of keratocyte progenitors in the corneal stroma of the murine and human eyes.
Progenitor cells derived from the corneas of C57BL6/J mice are able to
British Medical Bulletin 2008
Page 11 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
patients who may benefit from cultured stem cell transplantation, not
just in the eye, clearly defined objective parameters of pre and postoperative assessment must be developed to enable proper comparisons
between studies.
Provision of cell therapies, particularly customized autologous treatments will remain expensive until the issues around scale-up and commercialization have been addressed. Therapies at present conducted
under research protocols (which still need to meet the provisions of the
EU Tissue and Cells Directive) are produced by highly specialized
research-driven facilities and hence are not widely available to the
population. The clinical follow-up time required to critically evaluate
cell therapy safety and efficacy in patients is time-consuming and difficult to do in any volume in regular clinics. However, it is anticipated
that in the future this will change as new innovations deliver more efficient cell therapy production protocols and robust methods to assess
clinical outcome.
G. A. Limb and J. T. Daniels
Regulatory issues affecting established stem cell therapies
In order to produce and deliver cell therapies in Europe, it is now
necessary to comply with the provisions of the EU Tissues and Cells
Directive. In the UK, this is governed by the Human Tissue Authority
(HTA). The purpose is to protect patient safety and to ensure that the
best quality products are used in clinical trials and routine practice.
This involves producing the therapy in a controlled clean room
environment under an extremely stringent quality management system
akin to the principles of Good Manufacturing Practice used by the
pharmaceutical industry.45 This poses great practical challenges when
cultivating cells in a dynamic living system compared with drug manufacture, and would have huge financial repercussions in the health
service if cell therapies were to be widely established to treat ocular
disease.
Conclusions
Stem cell-based therapies for ocular repair and regeneration constitute
a major hope for the restoration of visual function in individuals
whose ocular tissue has been irreversibly damaged by disease or
trauma. At present, the only cells with well-recognized clinical application in the ophthalmic field are the LESC for corneal repair.
Experience gained from this approach would potentially help with the
design of stem cell-based therapies to regenerate other ocular tissues,
particularly the retina. There is much speculation on the capability of
newly discovered sources of retinal progenitors, but before establishing
any new therapy, we must understand the real potential of each cell
source to regenerate retinal neurons. In addition, there is the need to
carefully address important issues that are at present precluding the
Page 12 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
form spheres, express Pax6 and maintain their keratocyte phenotype
after several passages.43 Similarly, stromal cells isolated from the
region surrounding the human corneal limbus express Pax6 and the
ABCG2 transporter protein observed in many adult stem cells. Upon
culture with FGF2, they express keratocyte markers; and following
differentiation, they acquire chondrogenic and neurogenic characteristics,44 indicating a multipotent ability of these cells. These findings
suggest that keratocyte progenitors have potential use for cell-based
therapies to treat many corneal diseases, and exploration of their capabilities would further advance stem cell therapies to treat ocular surface
disease.
Ocular regeneration by stem cells
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
British Medical Bulletin 2008
Pellegrini G, Traverso CE, Franzi AT, Zingirian M, Cancedda R, De Luca M (1997)
Long-term restoration of damaged corneal surfaces with autologous cultivated human epithelium. The Lancet, 349, 990– 993.
Graw J (1996) Genetic aspects of embryonic eye development in vertebrates. Dev Genet, 18,
181–197.
Raymond PA, Hitchcock PF (1997) Retinal regeneration: common principles but a diversity
of mechanisms. Adv Neurol, 72, 171– 184.
Moshiri A, Close J, Reh TA (2004) Retinal stem cells and regeneration. Int J Dev Biol, 48,
1003– 1014.
Coles BL, Angenieux B, Inoue T et al. (2004) Facile isolation and characterization of human
retinal stem cells. Proc Natl Acad Sci USA, 101, 15772– 15777.
Fischer AJ, Reh TA (2001) Müller glia are a potential source of neural regeneration in the
postnatal chicken retina. Nature Neurosci, 4, 247–252.
Das AV, Mallya KB, Zhao X et al. (2006) Neural stem cell properties of Muller glia in the
mammalian retina: regulation by Notch and Wnt signaling. Dev Biol, 299, 283– 302.
Raymond PA, Barthel LK, Bernardos RL, Perkowski JJ (2006) Molecular characterization of
retinal stem cells and their niches in adult zebrafish. BMC Dev Biol, 6, 36.
Lawrence JM, Singhal S, Bhatia B et al. (2007) MIO-M1 cells and similar Müller glial cell
lines derived from adult human retina exhibit neural stem cell characteristics. Stem cells, 25,
2033– 2043.
Cepko CL, Austin CP, Yang X, Alexiades M, Ezzeddine D (1996) Cell fate determination in
the vertebrate retina. Proc Natl Acad Sci USA, 93, 589–595.
Marquardt T, Gruss P (2002) Generating neuronal diversity in the retina: one for nearly all.
Trends Neurosci, 25, 32–38.
Harris WA (1982) The transplantation of eyes to genetically eyeless salamanders: visual projections and somatosensory interactions. J Neurosci, 2, 339–353.
So KF, Aguayo AJ (1985) Lengthy regrowth of cut axons from ganglion cells after peripheral
nerve transplantation into the retina of adult rats. Curr Eye Res, 4, 253 –265.
Turner JE, Blair JR (1986) Newborn rat retinal cells transplanted into a retinal lesion site in
adult host eyes. Brain Res, 391, 91– 104.
Young MJ, Ray J, Whiteley SJ, Klassen H, Gage FH (2000) Neuronal differentiation and
morphological integration of hippocampal progenitor cells transplanted to the retina of
immature and mature dystrophic rats. Mol Cell Neurosci, 16, 197–205.
Chacko DM, Das AV, Zhao X, James J, Bhattacharya S, Ahmad I (2003) Transplantation of
ocular stem cells: the role of injury in incorporation and differentiation of grafted cells in the
retina. Vision Res, 43, 937– 946.
Page 13 of 15
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
establishment of human retinal therapies. Problems to be solved
comprise the standardization of isolation and expansion methods to
preserve stem cell phenotype, the identification of requirements for
neural differentiation and preparation of cellular scaffolds for grafting,
the modulation of the extracellular matrix to promote cell migration
and neural synapses, the prevention of immune rejection and tumour
development and, very important, the identification of conditions that
maintain graft survival. Despite many practical problems, there is
general optimism among the medical and scientific community that
stem cell-based therapies to restore visual function could become a
reality in a non-distant future.
G. A. Limb and J. T. Daniels
Page 14 of 15
British Medical Bulletin 2008
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
17 Banin E, Obolensky A, Idelson M et al. (2006) Retinal incorporation and differentiation of
neural precursors derived from human embryonic stem cells. Stem Cells, 24, 246– 257.
18 Lund RD, Wang S, Lu B et al. (2007) Cells isolated from umbilical cord tissue rescue
photoreceptors and visual functions in a rodent model of retinal disease. Stem Cells, 25,
602–611.
19 Otani A, Dorrell MI, Kinder K et al. (2004) Rescue of retinal degeneration by intravitreally injected adult bone marrow-derived lineage-negative stem cells. J Clin Invest, 114,
765–774.
20 Masland RH (2004) Neuronal cell types. Curr Biol, 14, R497–R500.
21 MacLaren RE, Pearson RA, MacNeil A et al. (2006) Retinal repair by transplantation of
photoreceptor precursors. Nature, 444, 203–207.
22 Ahmad I, Das AV, James J, Bhattacharya S, Zhao X (2004) Neural stem cells in the mammalian eye: types and regulation. Semin Cell Dev Biol, 15, 53 –62.
23 Fischer AJ, Reh TA (2003) Growth factors induce neurogenesis in the ciliary body. Dev Biol,
259, 225–240.
24 Chopdar A, Chakravarthy U, Verma D (2003) Age related macular degeneration. BMJ, 326,
485–488.
25 Kohner EM, Aldington SJ, Stratton IM et al. (1998) United Kingdom Prospective Diabetes
Study, 30: diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and
associated risk factors. Arch Ophthalmol, 116, 297– 303.
26 Strauss O (2005) The retinal pigment epithelium in visual function. Physiol Rev, 85,
845–881.
27 Nowak JZ (2006) Age-related macular degeneration (AMD): pathogenesis and therapy.
Pharmacol Rep, 58, 353–363.
28 Klimanskaya I, Hipp J, Rezai KA, West M, Atala A, Lanza R (2004) Derivation and comparative assessment of retinal pigment epithelium from human embryonic stem cells using
transcriptomics. Cloning Stem Cells, 6, 217–245.
29 Lund RD, Wang S, Klimanskaya I et al. (2006) Human embryonic stem cell-derived cells
rescue visual function in dystrophic RCS rats. Cloning Stem Cells, 8, 189–199.
30 Davanger M, Evenson A (1971) Role of the pericorneal structure in renewal of corneal epithelium. Nature, 229, 560–561.
31 Cotsarelis G, Cheng G, Dong G, Sun TT, Lavker RM (1989) Existence of slow-cycling limbal
epithelial basal cells that can be preferentially stimulated to proliferate: implications on epithelial stem cells. Cell, 57, 201– 209.
32 Shortt AJ, Secker GA, Munro PM, Khaw PT, Tuft SJ, Daniels JT (2007) Characterisation of
the limbal epithelial stem cell niche: novel imaging techniques permit in-vivo observation and
targeted biopsy of limbal epithelial stem cells. Stem Cells, 5, 1402–1409.
33 Jenkins C, Tuft S, Lui C, Buckley R (1993) Limbal transsplantation in the management of
chronic contact lens-associated epitheliopathy. Eye, 7, 629–633.
34 James SE, Rowe A, Ilari L, Daya S, Martin R (2001) The potential for eye bank limbal rings
to generate cultured corneal epithelial allografts. Cornea, 20, 488–494.
35 Shortt AJ, Secker GA, Notara MD et al. (2007) Transplantation of ex-vivo cultured limbal
epithelial stem cells—a review of current techniques and clinical results. Surv Ophthalmol,
52, 483– 502.
36 Ahmad S, Stewart R, Yung S et al. (2007) Differentiation of human embryonic stem cells into
corneal epithelial like cells by in vitro replication of the corneal epithelial stem cell niche.
Stem Cells, 25, 1145– 1155.
37 Nishida K, Yamato M, Hayashida Y et al. (2004) Corneal reconstruction with
tissue-engineered cell sheets composed of autologous oral mucosal epithelium. N Engl J Med,
351, 1170–1172.
38 Chee KY, Kicic A, Wiffen SJ (2006) Limbal stem cells: the search for a marker. Clin
Experiment Ophthalmol, 4, 1 –2.
39 Daya SM, Watson A, Sharoe JR et al. (2005) Outcomes and DNA analysis of ex vivo
expanded stem cell allograft for ocular surface reconstruction. Ophthalmology, 112,
470–477.
40 Pellegrini G, Golisano O, Paterna P et al. (1999) Location and clonal analysis of stem cells
and their differentiated progeny in the human ocular surface. J Cell Biol, 145, 769– 782.
Ocular regeneration by stem cells
41 Dogru M, Tsubota K (2005) Survival analysis of conjunctival limbal grafts and amniotic
membrane transplantation in eyes with total limbal stem cell deficiency. Am J Ophthalmol,
140, 305–306.
42 Zhao X, Das AV, Thoreson WB et al. (2002) Adult corneal limbal epithelium: a model for
studying neural potential of non-neural stem cells/progenitors. Dev Biol, 250, 317 –331.
43 Yoshida S, Shimmura S, Shimazaki J, Shinozaki N, Tsubota K (2005) Serum-free spheroid
culture of mouse corneal keratocytes. Invest Ophthalmol Vis Sci, 46, 1653– 1658.
44 Du Y, Funderburgh ML, Mann MM, SundarRaj N, Funderburgh JL (2005) Multipotent stem
cells in human corneal stroma. Stem Cells, 23, 1266– 1275.
45 Daniels JT, Secker GA, Shortt AJ, Tuft SJ, Seetharaman S (2006) Stem cell therapy delivery—
treading the regulatory tightrope. Regen Med, 1, 715– 719.
Downloaded from http://bmb.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014
British Medical Bulletin 2008
Page 15 of 15