PDF of this Article
advertisement

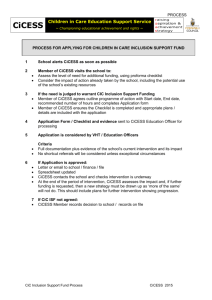
Original Article C-REACTIVE PROTEIN, RHEUMATOID FACTOR AND CIRCULATORY IMMUNE COMPLEX AS MARKERS FOR MONITORING TREATMENT OF INFECTIVE ENDOCARDITIS Seyed Mohammad Alavi1, Fatemeh Ahmadi2, Rouhangiz Nashibi3 ABSTRACT Objectives: To evaluate the diagnostic usefulness of serum C-reactive protein (CRP), rheumatoid factor (RF) and circulatory immune complex (CIC) determinations in monitoring the outcome of infective endocarditis (IE). Methodology: In this prospective analytic descriptive study CRP, RF and CIC were measured on admission and 4 weeks after initiation of standard antibiotic regimen in 30 hospitalized patients with IE in an educational hospital between 2006 and 2007 in Ahvaz a city south west Iran . Duke criteria were used for diagnosis of IE. CRP and RF were examined using quantitative neflometry (Binding site kit, UK) and CIC was detected by semi quantitative immune diffusion (Baharafshan SIRD kit, Iran). Data were evaluated using statistical analyses in SPSS (version 12, USA) software for windows. Results: The fall in serum C-reactive protein or RF was significant (P=<0.05) when a patient had a full recovery, but no such behavior was observed in CIC (P>0.05). Only two of the 30 patients, who had elevated CRP, RF and CIC week four failed to response and one needed cardiac surgery. Conclusions: The C-reactive protein proved to be a good tool for monitoring the treatment of IE. Also RF proved useful in the assessment of patients with IE, but the value of CIC was negligible. KEYWORDS: C-reactive protein, Rheumatoid factor, Circulatory immune complex, Infective endocarditis. Pak J Med Sci October - Decmber 2009 (Part-I) Vol. 25 No. 5 825-828 How to cite this article: Alavi SM, Ahmadi F, Nashibi R. C-reactive protein, Rheumatoid factor and circulatory immune complex as markers for monitoring treatment of infective endocarditis. Pak J Med Sci 2009;25(5):825-828. 1. Dr Seyed Mohammad Alavi, MD, Associated Professor of Medical College 2. Dr Fatemeh Ahmadi, MD 3. Dr Rouhangiz Nashibi, MD 1-3: Infectious disease ward, Razi Hospital, Joundishapour University of Medical Sciences, Ahvaz, Iran, Joundishapour Infectious Diseases and Tropical Medicine Research Center, Ahvaz, Iran. Correspondence Dr Seyed Mohammad Alavi No: 52, West 11 Avenue, Kianabad, Ahvaz, Iran Email: alavi1329dr@yahoo.com * Received for Publication: May 5, 2009 * Accepted: August 20, 2009 INTRODUCTION Infection of the endocardial surface of the heart called infective endocarditis (IE) is a serious infection with significant morbidity and mortality associated with the need for prolonged parentral antibiotic treatment.1,2 Early diagnosis, regular follow up and monitoring treatment have greatly reduced the i ncidence of treatment failure and mortality rate by modifying antibiotic regimen and applying proper intervention as well as cardiac surgery.1-3 Pak J Med Sci 2009 Vol. 25 No. 5 www.pjms.com.pk 825 Seyed Mohammad Alavi et al. There are many laboratory tests for monitoring treatment such as erythrocyte sedimentation rate (ESR), white blood cell count (WBC), C-reactive protein (CRP), rheumatoid factor (RF), circulatory immune complex (CIC), precalcitonine and interlukin-6 (IL-6).1,4-6 There are great differences between countries in the use of these tests. New markers of inflammation such as precalcitonine and IL-6 are used frequently in developed countries whereas useful older tests such as CRP, ESR, RF, CIC, and WBC are used in developing or resource limited countries.5,6 Published studies have shown that CRP, ESR andWBC are useful laboratory tests in monitoring the response to therapy in patients with bacterial infection such as meningitis as well as septicemia.6,7 Previous studies about usefulness of these tests in monitoring treatment of IE are associated with controversial results.4-6,8-10 Because of lacking data about utility of these tests in Iranian IE patients, we designed this study to evaluate the clinical usefulness of CRP, RF and CIC in monitoring treatment of hospitalized patients with IE in educational hospital between 2006 and 2007in Ahvaz. METHODOLOGY All the patients with IE diagnosed between 2006 and 2007 in an educational hospital(Razi hospital) affiliated to Jundishapur University of Medical Sciences in Ahvaz,the capital city of Khuzestan south west Iran, were analyzed in a prospective analytic descriptive study. Duke criteria was used for diagnosis of IE (Table-I), patients were treated by standard antibacterial regimen according AHS (American Heart Society) accepted by Iranian Infectious Disease and Tropical Medicine Board.1-3 The values of CRP, RF and CIC were examined on admission and 4 weeks after initiation of antibacterial treatment. Two blood samples (5ml) obtained from each patient on admission and after 4 weeks of treatment. Samples were passed to laboratory. 2.5 ml of each sample were used for CRP and RF, remaining 2.5 ml was preserved at -20º C until sending to Central laboratory in Tehran (under standard condition) for CIC examination. Samples were examined for CRP and 826 Pak J Med Sci 2009 Vol. 25 No. 5 www.pjms.com.pk RF in a private laboratory in Ahvaz by using quatitative neflometry (Binding site kit, UK). CIC was detected by semiquantitative immune diffusion (Baharafshan SIRD kit, Iran). Reference value for RF was <30 IU/ml, CRP concentration of <4 mg/l was considered normal and CIC value >1.4mg/ml was considered positive. At the day 7 of treatment, IE defined as cured when the fever and other sign and symptoms were subsided, patients with fever (in spite of 7 day appropriate treatment) or neurological and embolic manifestation or the need for cardiac surgery were defined as failure treatment. Data was collected by medical chart included age,sex,blood culture results,echocardiographic findings, received antibiotic before and after admission, clinical findings and outcome of IE.Data were analyzed in SPSS software (version 12,USA) by using t test,chisquare test and Fisher’s exact test. Association of laboratory tests with the outcome of treatment was analyzed using odds ratio (OR) with 95% confidence interval (CI). P values<0.05 were considered significant. RESULTS Of total 30 patient 26(86.7%) were male and 4(13.3%) were female. The mean age ± SD of female was 38.25 ± 22.92 years and of male was 29.19 ± 6.75 years, with the range of 20-70 for both. CRP before treatment(on the admission) was elevated in 30 patients(100%) with the mean value of 72.38 ± 42.59.CRP values 4 weeks after treatment remained significantly high in four patients(13.3%).CRP was significantly lower in patients who cured than in those who failed to treatment(P<0.05). OR for cure was over two fold (OR=2.4,95% CI,1.2-4.4;P=0.004). RF before treatment was positive in 26 (86.6%) and four weeks after treatment was positive in 8 (26.6%). Significant difference in RF positivity was observed between results before and after treatment (P<0.05). Before and after treatment CIC was positive in 27(90%) and 23(76.6%) patient respectively. There was no difference in CIC positivity between patients with cure and patients with failure to treatment (P>0.05).Results of CRP,RF and CIC values are shown in Infective Endocarditis Treatment monitoring Table-I: The Duke criteria for the Clinical Diagnosis of Infective Endocarditis Major criteria 1. Positive blood culture: Typical microorganism for infective endocarditis 2. Evidence of endocardial involvement: Positive echocardiograma, Minor criteria 1. Predisposition: predisposing heart condition or injection drug use 2-fever> 38.0°C 3. Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, Janeway lesions 4. Immunologic phenomena: glomerulonephritis, Osler’s nodes, Roth’s spots, rheumatoid factor 5. Microbiologic evidence: positive blood culture but not meeting major criterion as noted previouslyb or serologic evidence of active infection with organism consistent with infective endocarditis Transesophageal echocardiography is recommended for assessing possible prosthetic valve endocarditis or complicated endocarditis.bExcluding single positive cultures for coagulase-negative staphylococci and diphtheroids, which are common culture contaminants, and organisms that do not cause endocarditis frequently, such as gram-negative bacilli.Note: HACEK, Haemophilus spp., Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella species. a Table-II.Two patients failed to response to treatment because of cardiac complication needed to cardiac surgery in one patient and glomerulonephritis in another patient. DISCUSSION The present study revealed that determination of CRP is a useful tool to monitor the outcome of IE. The serum CRP concentration was significantly lower when a patient cured of IE than when failed response to antibacterial therapy. This finding is consistent with some earlier studies11-13 but, is in disagreement with Hryniewiecki et al.8Thomson et al,reported that serial determination of CRP was useful in monitoring of the patient’s response to the therapy of IE,and failure to treatment was associated with high CRP concentration.13 Hryniewiecki and colleagues explained no significant correlation between CRP and outcome of IE treatment, the tendency of consecutive CRP concentrations to decrease (from 27.1 ± 23.9 mg/l to 22 ± 18.3 mg/l) was not significant and CRP was not a useful tool for IE treatment monitoring.8 These differences may be due to: 1-existence of valvular disease in Hryniewiecki’s patients which prevent decreasing in CRP values, 2-difference in CRP assay in these studies (ELISA vs. neflometry). Our study showed that RF is an acceptable and useful marker of the therapeutic response in treatment of IE. Effective antibiotic therapy resulted in decreasing of RF values. This finding is in agreement with Koeglenberg’s study11 but, differs from Thomson’s work.13 Thomson et al, reported that cure of IE was not associated with low serum concentration of RF. We believe that these opposite results are due to difference in clinical course of IE in study population. RF in serum of sub acute IE patients is usually higher than in patients with acute IE.1,2 Majority of our patients were in sub acute phase of IE whereas patients of Thomson’s study were in acute phase of illness. In this study serum concentration of CIC on admission and four weeks after treatment were equivalent. CIC was not a useful tool for clinical monitoring of IE outcome. This finding is in Table-II: Laboratory results for monitoring infective endocarditis in Ahvaz Lab. On admission After treatment P value OR,95% CI tests Cured Failed CRP 72.38 ± 42.59 44.16 ± 30.64 79.12 ± 47.03 0.004 OR=2.4,95% CI,1.2-4.4 RF 60.45 ± 71.42 41.25 ± 49.37 61.72 ± 69.09 0.013 OR=1.7,95%CI,0.8-2.1 CIC 0.847 ± 0.16 0.80 ± 0.19 0.814 ± 0.27 0.27 OR=1.02,95%CI,0.5-1.1 CRP;C-reactive protein (mg/l), RF; rheumatoid factor(IU/ml),CIC; circulatory immunecomplex (mg/ ml),Lab; laboratory, OR; odds ratio, CI; confidence interval, IU; international unit. Difference with Pvalue lower than 0.05 are significant Pak J Med Sci 2009 Vol. 25 No. 5 www.pjms.com.pk 827 Seyed Mohammad Alavi et al. agreement with Thomson et al13 and Agrawal et al,14 but, is in disagreement with Messias-Reason et al, 15 Schned et al16 and Bayer et al.17 Messias-Reason, reported that CIC is pathogenic in IE and has high serum concentration in complicated or died patients. CIC value in cured patients is significantly lower than in complicated patients.15 Schned et al explained that CIC was significantly elevated in the patients who died when compared to those who had a good recovery (P < 0.02 and suggested CIC as possible markers for severity or monitoring treatment the disease.16 Bayer et al, suggested that Circulating immune-complex levels were correlated with out come of IE, and CIC levels fell to zero with successful antimicrobial or surgical therapy.17 This difference may be due to our study population. Majority of our patients were injecting drug users, in which because of frequent injections, immune complex are frequently found in high concentration in their serum.1,2 Our study has some limitation such as small sample size, injecting drug users and the impact of their underlying condition ( infectious disease and probably human immune deficiency virus infection) on the our result, In addition lacking laboratory facility for performance CIC examination in Ahvaz and possible hazard to samples in transportation to Tehran in spite of our extreme caution. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. ACKNOWLEDGMENT The authors wish to thank the chief and personnel of Jundishapoor Infectious and Tropical Research Center (JITRC)for supporting of this study. We also acknowledge the chief and personnel of the infectious disease department of Razi hospital and Dr Moradzadegan the chief of Pasteur laboratory for kind assistance. Conflict of interest: This study was funded by JITRC and there is no conflict of interest. REFERENCES 1. Karchmer AW, Infective Endocarditis in: Kasper AS, Hauser SL, Longo DL,Jameson JL.(edts).Harrison’s Principles of Internal Medicine, 16th Edition, New York, Mcgraw-Hill Companies 2005;731-40. 828 Pak J Med Sci 2009 Vol. 25 No. 5 www.pjms.com.pk 14. 15. 16. 17. Fowler VG, Scheld WM, Bayer AS. Endocarditis and intravascular infections. In: Mandell GL, Bennett JE, DolinR. Principles and Practice of Infectious Diseases.6th edition, Philadelphia, Churchill Livingstone, 2005;975-1022. Anderson JL. Infective Endocarditis in: HURST’S The Heart, 11 th edition, New York, Mcgraw-Hill Companies 2004;764-800. Gabay C, Kushner I. Acute phase protein and other systemic responses to inflammation. N Engl J Med 1999;340:448-54. Gendrel D, Raymond J, Coste J, Moulin F, Lorrot M, Guérin S, et al. Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs. viral infections. Pediatr Infect Dis J 1999;18:875-81. Heiro M, Helenius H, Sundell J, Koskinen P, Engblom E, Nikoskelainen J, et al. Utility of serum C-reactive protein in assessing the outcome of infective endocarditis. Eur Heart J 2005;26(18):1873-81. Ehl S, Gering B, Bartmann P, Högel J, Pohlandt F. C-reactive protein is a useful marker for guiding duration of antibiotic therapy in suspected neonatal bacterial infection. Pediatrics 1997;99:216-21. Hryniewiecki T, Rawczyñska-Englert I, Sitkiewicz D, Jab³oñski D. Comparison of interleukin-6 and C-reactive protein serum concentrations assessment in diagnosis of infective endocarditis. Pol Arch Med Wewn 2002;108(4):947-52. Kerr MA, Wilton E, Naama JK, Whaley K. Circulating immune complexes associated with decreased complementmediated inhibition of immune precipitation in sera from patients with bacterial endocarditis. Clin Exp Immunol 1986;63(2):359-66. Buess T, Ludwig C. Diagnostic value of C-reactive protein in comparison with erythrocyte sedimentation as routine admission diagnostic test. Schweiz Med Wochenschr 1995;125(4):120-4. Koegelenberg CF, Doubell AF, Orth H, Reuter H. Infective endocarditis: improving the diagnostic yield. Cardiovasc J S Afr 2004;15(1):14-20. Wallace SM, Walton BI, Kharbanda RK, Hardy R, Wilson AP, Swanton RH. Mortality from infective endocarditis: clinical predictors of outcome. Heart 2002;88(1):53-60. Roberts-Thomson PJ, Koh LY, Kennedy A, Smith MD, Neoh S, Turnidge J. Serological investigations in the diagnosis and management of infective endocarditis. Aust N Z J Med 1986;16(6):761-5. Agarwal R, Bahl VK, Malaviya AN, Krishnan S, Chopra P. Immunologic parameters in infective endocarditis: a prospective study. Indian Heart J 1991;43(3):179-83. Messias-Reason IJ, Hayashi SY, Nisihara RM, Kirschfink M. Complement activation in infective endocarditis: correlation with extracardiac manifestations and prognosis. Clin Exp Immunol 2002;127(2):310-5. Schned ES, Inman RD, Parris TM, Kimberly RP, Redecha PB, Christian CL. Serial circulating immune complexes and mononuclear phagocyte system function in infective endocarditis. J Lab Clin Med 1983;102(6):947-59. Bayer AS, Theofilopoulos AN, Eisenberg R, Dixon FJ, Guze LB. Circulating immune complexes in infective endocarditis. N Engl J Med 1976;295(27):1500-5.