Ultraviolet Radiation and the Anterior Eye
advertisement

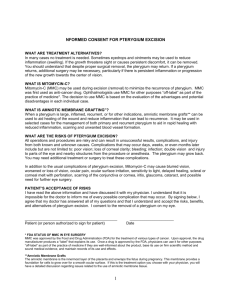
REVIEW Ultraviolet Radiation and the Anterior Eye Minas Coroneo, Abstract: The eye is on the one hand dependent on visible light energy and on the other hand can be damaged by these and the contiguous ultraviolet (UV) and infrared wavelengths. Diseases of the eye in which sunlight has been implicated have been termed the ophthalmohelioses, and these conditions pose a significant problem to the eye health of many communities. The ophthalmohelioses have a tremendous impact on patients’ quality of life and have significant implications on the cost of health care. Although cataract is not entirely caused by insolation, it now seems certain that sunlight plays a contributory role—cataract extraction is one of the, if not the most, commonly performed surgical procedures in many societies. Pterygium, typically afflicting a younger population, adds a tremendous burden, both human and financial, in many countries. We review evidence that peripheral light focusing by the anterior eye to the sites of usual locations of pterygium and cataract plays a role in the pathogenesis of these conditions. Recognition of the light pathways involved with foci at stem cell niches has directed our investigations into inflammatory and matrix metalloproteinase-related pathophysiologic mechanisms. An understanding of the intracellular mechanisms involved has provided some insight into how medical treatments have been developed for the effective management of ocular surface squamous neoplasia. The concept of peripheral light focusing has also provided direction in the prevention of these diseases. This has resulted in improved sunglass design and the further development of UV-blocking contact lenses. With the development of ocular UV fluorescence photographic techniques, we have been able to demonstrate preclinical ocular surface evidence of solar damage. Evidence that diet may play a role in the development of certain conditions is reviewed. The conundrum of the public health message about solar exposure is also reviewed, and in this context, the potential role of vitamin D deficiency is summarized. The eye may play a role in the development of individualized assessment techniques of solar damage, perhaps allowing us to provide better advice to both individuals and populations. Key Words: Ultraviolet—eye—Pterygium—Cataract—Ocular surface squamous neoplasia—Dysphotopsia—Sunglasses—Contact lens—Sun protection. (Eye & Contact Lens 2011;0: 000–000) From the Department of Ophthalmology, University of New South Wales, Sydney, Australia. Disclosure: The author discloses that he is the inventor of US Patent 7,217,289: Treatment of photic disturbances in the eye, US Patent 7,846,467: Ocular scaffold for stem cell cultivation and methods of use, US Patent application 20060204474: Treatment of epithelial layer lesions, US Patent application 20050287115: Treatment of ocular lesions; is a consultant to Allergan, Inc in the area of medical treatment of pterygium and dry eye and has received research funds and travel support; receives royalties from Eagle Vision Inc in relation to a dry eye product; and has been a consultant to Johnson and Johnson Vision Care Inc and has received research funds and travel support.. Address correspondence and reprint requests to Minas Coroneo, M.Sc., M.S., M.D., Department of Ophthalmology, Prince of Wales Hospital, High St. Randwick, NSW 2031, Sydney, Australia; e-mail: M.Coroneo@unsw.edu.au Accepted May 6, 2011. DOI: 10.1097/ICL.0b013e318223394e Eye & Contact Lens ! Volume 0, Number 0, Month 2011 M.Sc., M.S., M.D. A s the terrestrial invasion by amphibians commenced, an essential adaptation was the development of filters to screen out more energetic wavelengths that were absorbed by the surface layers of the marine environment. Although perhaps relatively effective, at least in creatures with relatively short life spans, the vast array of conditions, particularly those that afflict the human eye suggests that only a partial solution to this problem was engineered. In one sense, these conditions, particularly of the anterior eye, can be seen as evidence of suboptimal adaptation to terrestrial life. The conditions in which sunlight has been implicated (with varying degrees of certainty) in the pathogenesis have been termed the ‘‘ophthalmohelioses’’1,2 (Table 1) as the ophthalmic correlate of the dermatohelioses. This group of conditions has been of great interest to Australian ophthalmologists for reasons of history and climate. In Australia’s first medical publication of 1840,3 it is stated, ‘‘In this climate the eye is more liable to be affected than in England. There is a Sun that for many months in the year shines with a power and a brilliancy, that ‘‘at home’’ we are not cognizant of.’’ Ida Mann, first Professor of Ophthalmology at Oxford, during her years in Australia recounts that it ‘‘is the land of sin, sand, sorrow and sore eyes . it’s the climate.’’4 Kerkenezov5 in 1956 was the first to observe that white people with pterygia suffered from hyperkeratoses and rodent ulcers—an early clinical indication of the role of ultraviolet (UV) radiation. Further, pterygia developed about a decade before the dermatohelioses. Thus, an early link was made between UV insolation and both pterygium and skin malignancy—at that time the link with cutaneous melanoma was being proposed.6 Cameron7 author of one of the few monographs on the subject, recognized that pterygium was most common between latitudes 40!N and 40!S and for island populations. Thus, a relative !pterygium belt" straddles the equator, paralleling local atmospheric UV energy intensity. Yet, much of the UV light that strikes the eye is reflected, indirect light (albedo) and the elegant studies of Urbach,8 demonstrated that reflected light struck the eyes. It was therefore not surprising that the ophthalmohelioses were prevalent in places of high ground reflectance or in individuals exposed under these conditions. This may explain why there is a pterygium prevalence of 8.6% in Greenland9,10 at 61!N of the equator (compare 7.3% in the Australian Blue Mountains11) where there is less than a third of direct UVB found in the equatorial regions. Ultraviolet exposure may thus be similar if terrain reflectivity is taken into account.12 Also, because of the indirect and geometric nature of this exposure (vide infra), individual exposure is likely to have been inaccurately estimated from the standard questionnaires used in epidemiologic studies13—individual exposures and factors peculiar to individuals could result in underestimation of exposure. 1 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. M. Coroneo The prevalence of pterygium has been relatively high as Australia’s first full-time ophthalmologist, Evans14 reported on a new operation in 1893—a tradition continued by D’Ombrain15 in 1948. He noted ‘‘I have pinguecula in both eyes; they formed in my twenty-second year when I possessed my first motor bicycle and before I learnt the wisdom of wearing goggles; my late father, an ophthalmic surgeon, noticed the pinguecula and made me wear goggles.’’ This was perhaps early recognition of the importance of side light in ocular UV exposure and the fact that conventional spectacles offer inadequate protection. Another early observation that side light rather than direct light is important in pterygium pathogenesis is that pterygium is found in the fixing eye of patients with exotropia where it is expected that the nasal region of the exotropic eye be more exposed.16 In extremely bright light, the nondominant eye is closed, explaining why pterygium initially afflicts the dominant eye.17 Work from our unit in the 1980s described high pterygium prevalence rates in Indigenous Australians, approximately 15% in older age groups as compared with 6% to 12% in nonaborigines.18 This was believed to be because aborigines ‘‘spend all their waking hours outdoors caus[ing] them to be more exposed to solar radiation.’’ Yet, in examining 200 Aborigines in South Australia in 1888, the author was ‘‘struck with the absence of Pterygium in individuals so exposed.’’19 Although speculative, it is possible that this earlier population had not been exposed to trachoma (unlike their 1980 counterparts20), a disease known to affect the limbus,21 after which, pterygium has been associated22 and observed to develop.23 These observations raise the possibility that a double insult to the limbus (and corneal epithelial stem cells), infection then UV exposure may increase the risk of developing pterygium. Another possibility is the Westernization of the diets of Indigenous Australians, with a resultant reduction in protection from UV light (vide infra). Another intriguing aspect of pterygium research is the lack of an animal model. This may be because the human eye has a unique morphology whereby the sclera and limbus are exposed,24,25 whereas in most other species, the eyelids cover the limbus or the limbus is heavily pigmented and therefore protected from exposure to light. Humans also have large temporal visual field that not only aids survival but also acts as a large collecting zone for UV light, incident on the temporal limbus. In addition to the potentially harmful effects of normal levels of sunlight on the eye, there have also been concerns about the ozone hole and the ophthalmic consequences of increased ocular UV insolation.26 PERIPHERAL LIGHT FOCUSING AND PTERYGIUM PATHOGENESIS During my first weeks as an ophthalmology trainee in 1982, I noticed that light incident from the side was focused by the anterior eye to areas in the nasal aspect of the eye and ocular adnexa. I was putting on a necktie a day or so after my Departmental Chair had commented on what he considered to be my overly formal dress when this observation was made. At the time, in studying optics, I had learned about the related phenomenon of sclerotic scatter whereby light was believed to traverse the cornea by a pathway of internal reflection. I subsequently discovered that foci at the nasal limbus had been noted earlier; however, foci at the 2 Eye & Contact Lens ! Volume 0, Number 0, Month 2011 eyelid margin and on the nasal equator of the crystalline lens had not been observed. There was a realization that the usual (nasal) location of pterygium and pinguecula coincided with an intense focus of peripheral light and that light damage to limbal structures (including corneal epithelial stem cells27) would be important in pathogenesis (Fig. 1). In initial studies,28–30 we determined pathways by which the anterior eye, acting as a side-on lens, focuses light onto the opposite side of the eye, most noticeably to the distal (nasal) limbus (type 1 phenomenon). Light proceeds across the anterior eye by traversing the anterior chamber and not by the so-called sclerotic scatter. The degree of limbal focusing is determined in part by the corneal shape and anterior chamber depth, and this may explain, in part, why particular individuals in a particular environment are afflicted. The transcameral light pathways were confirmed using computer-assisted optical ray–tracing techniques.31–33 We calculated that the peak light intensity at the distal limbus is approximately 20 times that of the incident light intensity29—this has further been refined in subsequent studies to take into account corneal shape31,32 and focusing on the crystalline lens.33 The limbal effect peak intensity was found at an incident angle of 104!.33 Furthermore, it seems that the light focus is actually not a spot but a complex arc shape—explaining why it is difficult to appreciate when viewing along the path of incident light. The earliest report of peripheral light focusing (PLF) is from the work of von Helmholz.34 By asking a subject to accommodate, he was able to observe a movement of the light focus anteriorly, neatly demonstrating that the anterior crystalline lens surface (and iris) move forward during accommodation. Graves35 described a method of corneal illumination, termed sclerotic scatter, in which light was presumed to pass horizontally across the cornea by total internal reflection within the corneal stroma. Although this is considered as a possible pathway in initial observations,28 initial ray-tracing studies29 determined that this mechanism could not occur. Another early report from Mackevicius36 linked the observation of a limbal focus to pterygium pathogenesis. Rizzuti37 used a penlight in keratoconus patients to illuminate the temporal limbus and noticed distal limbal focusing. He claimed that this was not seen in normal corneas. Our calculations predicted that a steeply curved cornea (as is seen in keratoconus) would be expected to produce an intense distal limbal focus.31 Furthermore ‘‘normal’’ corneas also produce such foci. It was noticed in cattle38 that limbal foci occurred and coincided with the sites of precursor lesions for squamous carcinoma—ironically we used bovine eyes to work out the optical pathways involved29 in conjunction with ray-tracing experiments. Light focusing was again implicated in pterygium pathogenesis,39 but the pathway was believed to be by sclerotic scatter (transcorneal) and the mechanism of pathogenesis to involve damage to subconjunctival tissue, dellen formation and subsequent pterygium formation. These previous studies failed to define the precise optical pathways, the intensity of the limbal focus, the potential to damage stem cells and the pathophysiologic mechanisms involved (vide infra). They also failed to recognize that limbal focusing was one of a series of foci induced by the peripheral optics of the anterior eye. Although the characteristic location of pterygium is at the nasal limbus, pterygia can be located temporally. In one series, this was seen in only 2% of cases,40 yet in one study of sawmill workers, 15% demonstrated temporal pterygium alone, and 11% Eye & Contact Lens ! Volume 0, Number 0, Month 2011 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 UV Radiation and the Anterior Eye FIG. 1. Coincidence of the usual location of ptergium (upper left panel) with an intense nasal light focus (right and lower panels), after peripheral light focusing at the nasal limbus. demonstrated both temporal and nasal pterygia together.41 We have demonstrated light focusing at the temporal limbus,28 and this is most easily demonstrated in patients with a low nasal bridge, possibly explaining why temporal pterygium may be more prevalent in certain racial groups. In an Arabic population, temporal pterygium was reported in 2.4% of cases,42 whereas in a Chinese TABLE 1. Ophthalmic Conditions in Which Sunlight Has been Implicated in Pathogenesis Eyelid Ocular surface Crystalline lens Uvea Vitreous Retina Glaucoma Ocular posture Systemic (conditions with potential for ophthalmic involvement) Wrinkles; sunburn, photosensitivity reactions, cicatricial ectropion, dermatochalasis, premalignant changes, malignancy—BCC, squamous cell carcinoma, primary acquired melanosis, melanoma Pinguecula, pterygium, climatic keratopathy (Labrador keratopathy), actinic granuloma, keratitis (flash, snow blindness), arcus, band keratopathy, corneal endothelial polymorphism, reactivation of herpetic keratitis, scleritis in porphyria, senile scleral plaques, postphotorefractive keratectomy haze, dysplasia and malignancy of the cornea or conjunctiva, vernal catarrh Cataract, anterior capsular herniation, early presbyopia, capsular pseudoexfoliation, subluxation in Marfan syndrome, intraocular lens dysphotopsia Melanoma, miosis, pigment dispersion, uveitis, blood–ocular barrier incompetence Liquification Photic maculopathy, erythropsia, macular degeneration, choroidal melanoma, visual loss with photostress in carotid stenosis, circadian rhythm disturbances Experimental Intermittent exotropia Xeroderma pigmentosum, BCC, basal cell nevus syndrome, porphyria cutanea tarda, polymorphous light eruption, photosensitivity (drugs, uremia) immunosuppression, myopia, cranial arteritis, herpes zoster ophthalmicus, vitamin D deficiency BCC, basal cell carcinoma. q 2011 Lippincott Williams & Wilkins population, this was reported in 6.7% of the cases.43 There was an early suggestion that a large nose would protect the eye from sunlight,44 and this seems to be true for peripheral light crossing the midline in the direction of the temporal limbus. Apart from renewal of corneal epithelium, the limbus maintains a barrier so that normally conjunctival and corneal epithelium remains separated. Although little direct UV light strikes the ocular surface, with PLF, an intense beam crosses the anterior chamber, little altered by aqueous humor45 and strikes the basal and relatively unprotected stem cells. Thus, PLF circumvents the normal protection of this corneal stem cell niche by the more superficial limbal cells that normally absorb directly incident light.46 Because stem cells are pluripotent and capable of division, we postulated that alteration by UV light could result in a tissue mass of several cell types that traverse the limbal barrier and invade the cornea. Our observations are also consistent with the finding that the presence of a pterygium can be associated with deep corneal changes at the level of the endothelium and Descemet membrane and that endothelial cell density may be lower in these eyes.47 Furthermore, limbal focusing may also affect corneal nerves as they cross the limbus, allowing the possibility of neuropeptide involvement in pterygium pathogenesis and explaining corneal sensory alterations in pterygium patients.48 If corneal nerves are implicated, their radial distribution may also help to explain pterygium shape. Because the eye provides the only substantial lens focusing system on the body, pterygium (and perhaps cortical cataract) would be expected to develop earlier than the dermatohelioses, explaining Kerkenezov’s5 early observations. Thus, if we are exposed to increasing amounts of UV radiation, increased pterygium prevalence may be an early consequence of this exposure, because the pathologic processes would be sped up as a result of an exposure of light focused by at least an order of magnitude by the anterior eye. Pterygium prevalence may turn out to be a marker for increased human UV insolation. A second light focusing effect can be observed if the light source is moved more anteriorly (than the location required to produce 3 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. M. Coroneo Eye & Contact Lens ! Volume 0, Number 0, Month 2011 FIG. 2. Coincidence of early onset cortical lens opacity (lower upper panel) with an intense focus, evident on the ocular surface (right upper panel) after transcameral and translenticular passage of focused peripheral light. a limbal focus). Light is focused through the pupil (circumventing the protective effect of the iris) and onto the crystalline lens equator stem cells (Fig. 2). Light then exits the eye through the vascular ciliary body and appears as a red spot on the ocular surface.28–30 Ray-tracing studies of these transcameral/translenticular pathways have confirmed that the peak intensity of visible light varies between 33.7 and 34.8. Focusing of UVA results in higher peak intensities of 30.6 to 38.6 with maximum peak intensities occurring at angles of incidence of 82! to 86!.33,49 The inferonasal localization of early cortical cataract has been reported as far back as 1889,50 and this has been confirmed by several subsequent studies.51,52 Because the germinative zone of the crystalline lens is located equatorially, this region may be more sensitive to focused UV radiation than other parts of the crystalline lens.53 This type-2 peripheral focusing effect has also provided an explanation for an intraocular lens–associated glare phenomenon known as dysphotopsia.54–56 In this phenomenon, the peripheral optics of intraocular lenses allow a prismatic effect resulting in side light being directed posterior to the ora serrata so that the far peripheral retina is poorly illuminated, resulting in a scotoma (or arcs of light, coincident with retinal foci). This is a relatively common and annoying phenomenon and these observations may result in improved intraocular lens design. This background work has also enabled us to explain the shape of both pterygium57 and cortical spoke cataract.58 Using computational models, we examined the growth and movement of limbal epithelial cells and lens cells, respectively. In the case of pterygium, a focal limbal insult would result in a wing-shaped lesion and for the crystalline lens, if clusters of germinative cells are caused to opacify, the resultant cataract is predominantly spoke shaped. A third type of PLF effect can be demonstrated on the eyelid margin,28 the site of a stem cell population.59 We postulated that this might account for the nasal predilection for eyelid skin malignancy.60 Although these focusing phenomena are most easily seen with visible light, they also occur at 308 nm,28 this is not unexpected as the cornea transmits significant amounts of these energetic and biologically active wavelengths (60% of radiation at 320 nm and 80% at 400 nm.45 The association of exposure to broadband UV radiation and visible light61 with pterygium is therefore not surprising. 4 In relation to alterations induced in limbal stem cells, we have demonstrated that Fuchs Flecks, seen ahead of the leading edge of the pterygium head, contain p63-a-positive epithelial cell clusters, further evidence that pterygia develop from limbal epithelial progenitors.62 PATHOPHYSIOLOGY Although our understanding is incomplete, multiple processes seem to be involved, and these may be classified as inherited or individual factors, environmental triggers (UV light, viral infections) and factors that perpetuate pterygium growth (cytokines, growth factors and matrix metalloproteinases). These processes are summarized in Figure 3 and have been extensively reviewed.63–66 In the absence of an animal model for pterygium, we have relied on cell culture studies and by being the first group to culture pterygium epithelial cells67 were able to investigate the effects of UV light at a molecular level. This was a critical step in that we believed that UV-induced changes in corneal epithelial stem cells were the driving force behind corneal invasion by the pterygium. Although other elements, fibroblasts, vascular, neural elements, and an inflammatory process are involved and mesenchymal–epithelial interactions,68 we believed it most likely that epithelial cells drive the process of invasion. Hallmarks of the pathologic condition of pterygium are the destruction of Bowman membrane as corneal invasion by the pterygium proceeds and elastosis, previously interpreted as evidence of a degenerative process. In attempting to elucidate how these processes occur, we began by investigating the role of matrix metalloproteinses (MMPs) in pterygium pathogenesis.69–73 Matrix metalloproteinses are a family of zinc-dependent endopeptidases that are involved in remodeling of the extracellular matrix and altering cell surface molecules. The actions of MMPs are counterbalanced by tissue inhibitors of metalloproteinases (TIMPs), and MMPs are key mediators of photoaging where they regulate proliferation, cell migration, inflammation, and angiogenesis (see Chui and Coroneo65). Epithelial cells, fibroblasts, vascular cells and infiltrating immune cells produce MMPs in pterygia. We have demonstrated an overexpression of MMPs relative to TIMPs in the pterygium head and have seen this is a key factor in the invasive Eye & Contact Lens ! Volume 0, Number 0, Month 2011 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 UV Radiation and the Anterior Eye FIG. 3. Ultraviolet (UV) light activates multiple processes that may contribute to the formation of a pterygium. The UV induces oxidative stress and epidermal growth factor receptor activation, leading to production of cytokines, growth factors, and matrix metalloproteinases. These effector molecules mediate the influx of inflammatory cells, angiogenesis, proliferation, fibrosis, and extracellular matrix degradation commonly observed in pterygia (courtesy of Dr. J. Chui). nature of this condition.67 Several factors, including UV exposure, cytokines (IL-1 and transforming growth factor-a [TNF-a]) and growth factors (epidermal growth factor and TNF-a) have been shown to induce expression of MMPs in pterygium cells.65,66,74,75 The MMP-2 and MMP-9 seem to be associated with disease progression76 raising the possibility that MMPs could be targeted in the management of recurrent disease.66 We have also shown that Gelatinase B (MMP-9) was the most abundant gelatinolytic enzyme present in tears, elevated approximately twofold in eyes with pterygia versus the contralateral control eyes.70 This may be a contributing factor77 to the ocular surface inflammation and dry eye syndrome seen in pterygium patients78–perhaps presenting another therapeutic opportunity in treatment with topical cyclosporine.79 Another potential mode of action of cyclosporine is by the inhibition of the tachykinin NK1 receptors80 that we have localized to infiltrating fibroblasts, mononuclear cells and the epithelia of pterygia.48 In general terms, exposure of cells to UV induces activation of epidermal growth factor receptors (EGFRs) and subsequent downstream signaling through the mitogen-activated protein kinase pathways65,66,81 that are partially responsible for expression of proinflammatory cytokines, and matrix metalloproteinases in pterygium cells. Growth factor receptors and associated signaling pathways are activated as an early response to UV exposure, occurring independently of ligand binding and believed to involve UVgenerated reactive oxygen species.66 This response is common to the ocular surface (pterygium) and the skin, where UV induces phosphorylation and internalization of the EGFR within minutes of exposure, followed by activation of three mitogen-activated protein kinase (MAPK) pathways: extracellular signal-regulated kinase (ERK), c-jun amino-terminal kinase (JNK), and p38. In pterygium, UV activation of the ERK pathway is shown to induce production of MMP-1,73,75 whereas activation of the stress-related JNK and p38 pathways contributes to IL-6 and IL-8 induction72 with overexpression of EGFR82 contributing to amplification of these signaling q 2011 Lippincott Williams & Wilkins pathways. Transcription factors are induced downstream of EGFR and MAPK activation, including activator protein-1 (AP-1) and nuclear factor-kB (NF-kB), which mediate some cellular responses to UV damage (see 66). The UVB activation of the JNK pathway induces production of c-Jun and combined with c-Fos forms the AP-1 complex responsible for induction of MMP-1.73 The EGFRinduces NF-kB activation; however, this is believed to occur through signaling pathways involving tumor necrosis factor receptor-interacting protein and NF-kB–inducing kinase. NF-kB mediates UV-induced release of IL-1, IL-6, and TNF-a from cultured human corneal epithelial cells. It is therefore possible that UV-induced NF-kB activation may lead to the induction of these cytokines and growth factors in pterygium. In extending this work to cataractogenesis, we have demonstrated specific localization of MMP-1 within lens epithelium and lens fibers of cortical cataract.83 There was relatively little immunohistochemical staining for MMP-2, MMP-3, and MMP-9 and TIMP-1, TIMP-2, and TIMP-3 intracellularly within the cortical fibers of 13 cataractous lenses. The inferonasal quadrant contained a proportionally higher number of intracellular lens fibers staining and intensity of observed staining for MMP-1 The superotemporal quadrant contained the least number and lowest intensity of observed MMP and TIMP immunoreactivity. By comparison, observed immunostaining in control lenses was low for MMP-1, MMP-2, MMP-3, and MMP-9 and TIMP-1, TIMP-2, and TIMP-3 and was equal in all crystalline lens quadrants. We were also able to demonstrate that IL-1 and TNF-alpha upregulated the expression of MMP-2, MMP-3, and MMP-9, and UV-B upregulated the expression of MMP-1 in a human lens epithelial cell line. These findings were consistent with the pattern of light focusing onto a zone of germinative epithelium in which MMP induction can be demonstrated and which coincides with a known disease pattern. We also investigated MMP and TIMP activities in the zonular fibers in normal and Marfan syndrome lenses and demonstrated positive immunoreactivity for MMP-1, MMP-3, and MMP-9 in Marfan lens zonules, with no evidence of TIMP-1, TIMP-2, 5 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 M. Coroneo or TIMP-3 immunoreactivity.84 In contrast, no MMP-1 or MMP-3 staining was observed in the zonule of normal lenses, but TIMP-1, TIMP-2, and TIMP-3 were detected. We hypothesized that in the Marfan syndrome, the product of the defective FBN1 gene is susceptible to degradation by MMPs as compared with normal fibrillin (a key component of the zonule) and that the dysregulation of MMPs and TIMPs results in the progressive damage to the lens zonules and subsequent lens subluxation. Because in Marfan syndrome the crystalline lens typically dislocates superotemporally (as a consequence of weakening of the inferonasal zonule), we postulated that PLF could result in an increased exposure of the inferonasal zonule to UV light. This could further reduce fibrillin expression and perhaps increased MMP expression in this region resulting in early damage to the zonule, thereby explaining the pattern of lens dislocation.85 We have also investigated the potential role of MMPs in another of the ophthalmohelioses, ocular surface squamous neoplasia (OSSN)86 that often originates at the limbus but can affect the conjunctiva and cornea. We demonstrated that a higher proportion of OSSN surgical specimens stained for MMP-1, MMP-3 and TIMP-2 and TIMP-3 compared with normal conjunctiva. We established cell lines from tissue explants of both dysplastic and normal conjunctival epithelial cells and showed that cells derived from dysplastic tissue are more sensitive to UVB radiation than normal conjunctival cells. Although in OSSN cells MMP-1 and MMP-3 mRNA expressions were induced by UV in a mitogen-activated protein kinase–dependent fashion, in normal conjunctival cells, the same enzymes were upregulated only at (higher) doses that induced apoptosis. Ocular surface squamous neoplasia had a tendency to recur after treatment and traditional surgical procedures such as excision and cryotherapy are destructive and can have long-term consequences for the ocular surface.87 Topical treatment with Interferon alfa-2b which is a well tolerated and generally efficacious has greatly improved management of OSSN. We have demonstrated a rapid clinical response to combined treatment with topical interferon alfa2b and all-trans retinoic acid (ATRA), consistent with the synergistic effects of interferon alfa-2b and ATRA in combination, both in vitro and in vivo in nonocular neoplasia.87 These observations stimulated our interest in underlying mechanisms of action, and using our pterygium model, we have investigated UV-activated signaling pathways that mediate cytokine and growth factor production see whether these pathways are sensitive to blockade by Interferon or ATRA.72 Inhibitors of ERK1/2, JNK, and p38 MAPKs significantly abolished UVB-mediated increases in IL-6, IL-8, and vascular endothelial growth factor in this system. ATRA and Interferon dose dependently abrogated IL-6 and IL-8 but showed no effect on vascular endothelial growth factor expression after UV exposure, demonstrating a greater antiinflammatory than antiangiogenic response. This area shows some promise in developing better and less invasive medical treatments for this group of diseases.66 PREVENTION The late Professor Fred Hollow, after many years of work in outback Australia, set out sensible guidelines for preventing these diseases.88 He addressed issues relating to housing, eye protection and the likely protective effect of the siesta in certain cultures. Before 6 further considering these factors, two other areas of importance are the effectiveness of public health campaigns in relation to solar damage and the identification of individuals at risk of developing these diseases and a means by which to monitor early sun damage. Given that Australia has one of the highest skin cancer incidence and mortality rates in the world,89 the effectiveness of public health measures is a major concern. A survey of 652 Brisbane students aged 13–17 years showed only a moderate level of knowledge with respect to UV, sunlight, and the eyes.90 There was a greater knowledge about sunlight and body protection than eye protection, and although 71% of the subjects owned a pair of sunglasses, 81% of the subjects wore only sunglasses occasionally or not at all. The reported frequency of wearing sunglasses was significantly related to personal, family and peer attitudes to such use but not to media advertising. Australian national surveys during the 1990s of 78,032 students from age 7 to 12 years showed that only 11% of the students routinely followed all three protective behaviors of wearing a hat, sunscreen, and clothes that cover the body91 Sun protection practices among adolescents are suboptimal and have continued to decline significantly over time. It has been concluded that future educational programs will require an innovative approach to modify adolescent behaviors in relation to sun exposure and sun protection.92 To this end, we have developed a method that may detect early (preclinical) ocular surface sunlightinduced damage using UV fluorescence photography (UVFP).93,94 We have shown areas of nasal limbal fluorescence in eyes that are otherwise clinically normal (Fig. 4). These areas of fluorescence are consistent with focal damage induced by PLF. In a study in schoolaged children, we were able to detect these changes in children from the age of 9 years. The prevalence of these changes increased with chronological age, with clinical changes (pinguecula) being noted from age 13 years. We were surprised to find that in the 12- to 15-year age group, 81% of children showed evidence of damage (clinical and preclinical). As pointed out, pterygia have been found to develop about a decade before UV-induced skin conditions and thus may be an early indicator of increased UV insolation. Changes detected on UVFP may prove to be the earliest indicator of UV changes in the body. During the course of these studies, we found that both the children and their parents were interested in the changes that we could demonstrate. It may be that this graphic demonstration of early preclinical and clinical changes of sun damage will reinforce the important health message to reduce sun exposure and adopt preventative measures. By using UVFP, we went on to investigate the patterns of fluorescence in established pterygia.94 Four patterns were seen—80% of the patients demonstrated fluorescence at the leading edge of the pterygium, at the limbus or both. We postulated that the areas of fluorescence represented areas of cellular activity within the pterygium. The lack of fluorescence was believed to occur in pterygia that are ‘‘burned out’’ and represent disease that is no longer active. In relation to housing, on the one hand, it provides shelter from the elements on the other, modern architecture may allow increased sunlight indoors and indoor glare can be problematic.88 Some building materials have a high UV reflectance— in Kenya, hats were worn indoors in houses with corrugated iron roofs and no ceilings as ‘‘galvanized sheets did not repel all the sun’s rays’’ or more likely, result in high levels of scattered UV light indoors. Corrugated galvanized iron, invented in the 1840s, is a strong, lightweight, corrosion resistant, inexpensive, easily transported material Eye & Contact Lens ! Volume 0, Number 0, Month 2011 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 UV Radiation and the Anterior Eye FIG. 4. Interpalpebral regions of a 12-year-old girl who demonstrated an apparently normal ocular surface (upper panels). The corresponding UV fluorescence photographs (lower panels) demonstrate areas of fluorescence at the nasal limbus of each eye. and has been widely used in buildings, but it seems that it highly reflects UV light. Modern paints resist the elements and may also be highly reflective of UV light, potentially increasing our exposure close to, if not in, our shelters. SUNGLASSES Sunglasses are usually recommended as a form of protection against sunlight, yet conventional sunglasses are often a fashion accessory. However, sunglasses have several added disadvantages: 1. They reduce glare from direct, visible light and may allow wearers to increase their exposure to UV albedo.30 The eye is the body’s most efficient light warning system and represents the only means to caution a person adequately against the dangers of sunlight, because the skin itself is not able to announce overexposure rapidly enough to force its owner to get out of the sun in time. Modern man has invented remedies for the light sensitivity of the eye to be able to spend more time in the sun without feeling uncomfortable.95 In one study, people wearing sunglasses were less likely to wear hats and protective clothing.96 A possible link between the use of sunglasses and the risk of developing skin cancer, especially malignant melanoma, has been suggested.95 The development of UV-safe sunglasses that transmit visible light has been suggested.95 Lenses that cut out wavelengths below 400 nm have been recommended.88 2. Wearing sunglasses under conditions of extreme albedo (as in the Antarctic) can be associated with the development of photokeratoconjunctivitis (‘‘snow blindness’’),97 possibly the result of inactivation of the natural protective mechanism of squinting.98 3. As the pupil response is most sensitive to visible light, conventional sunglasses may allow pupil dilation in proportion to the darkness of the sunglasses99 and increased intraocular insolation. q 2011 Lippincott Williams & Wilkins 4. The potential decrease in low-contrast visual acuity.100 5. Spectacle frame associated reduction in visual field.101,102 6. Inconvenience—discomfort from frame, scratched lenses, fogging, and expense. In certain sports in which participants either are known to have a high prevalence of pterygium, such as surfing, or where it is potentially high, such as sailboard riding. A range of sunglasses, some of which float, and caps have been developed; however, a casual survey on any surfing beach in Sydney, Australia, would suggest that these devices are not widely used. Furthermore, there are other sports such as tennis or cricket where sun exposure may be substantial and sunglasses are inconvenient because of rapid, sudden movements or perspiration resulting in fogging or lens grime. The participants of these sports often play unprotected and would benefit from a more sophisticated protective strategy. In this setting, UV-blocking contact lenses may play a role because they typically span the limbus and are currently the most effective means of reducing if not eliminating peripheral light foci (vide infra). Sunglass styles vary considerably, particularly because until recently various Standards have not addressed the issue of side protection.103 Standard-setting groups are just starting to recognize that lateral protection afforded by sunglasses is of considerable importance. As a consequence, side protection can vary from extremely effective to nonexistent. Even with wraparound-style sunglasses, side exposure can still be considerable. Thus, in one study, the movement of the sunglass frame 6 mm from the forehead resulted in the variation of the percentage of UV reaching the eyes ranging from 3.7% to 44.8%.104 It was found that the amount of attenuation is highly variable and depends mainly on their size, shape, and wearing position of the spectacles. CONTACT LENSES A better understanding of the advantages offered by UVblocking contact lenses in relation to the specific ocular advantage 7 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 M. Coroneo of shielding the limbus to prevent PLF,32,33 and the development of better contact lenses105–108 has resulted in renewed interest in this area. These contact lenses have been available for many years,109 but have not been widely adopted109,110 perhaps because of the long lag-time111 between UV exposure and disease manifestation. We have confirmed that PLF focusing is greatly attenuated by the use of UV-absorbing contact lenses.32 The UVA and UVB sensors were placed on the nasal limbus of a model eye that was mounted in the orbit of a mannequin head and exposed to sunlight in three insolation environments within the region of Sydney, Australia. The temporal limbus was exposed to a UV light source placed at various angles behind the frontal plane, and PLF was quantified with the sensor output. The PLF for UVA and UVB was determined with no eyewear, with sunglasses and with commercially available soft contact lenses, with and without UV-blocking capability. The intensity of UVA peaked at an incident angle of approximately 120!, the level at which the UVB response was also at its maximum.32 The intensification of UVA was up to 318.3. Ultraviolet-blocking contact lens reduced the intensity of PLF for UVA and UVB by an order of magnitude, whereas clear contact lenses showed little effect. Only the UV-blocking contact lens achieved a significant reduction of UVA and UVB irradiance in urban, beach, and mountain locations. The use of UV-blocking contact lenses, as a supplement to sunglasses with appropriate UVblocking properties, provides safe, effective, and inexpensive protection of the cornea, limbus, and crystalline lens, in settings in which wearing sunglasses or hats is undesirable or impractical. Contact lenses can offer UV protection against all angles of incidence, including the peak-response angle; however, the conjunctiva and the eyelids would require additional protection. Conventional advice is to wear sunglasses and an adequate hat, yet in the Sanya Eye Study, it was evident that wearing a hat (without glasses) does not offer sufficient protection. In this study, pterygium prevalence was 75%, and of those surveyed, 96% wore hats, and less than 10% wore sunglasses.112 ROLE OF DIET Early studies have linked choline deficiency,113 and pellagra,114 deficiency of niacin (vitamin B3) with development of pterygium, but further studies have not been conducted. Because inflammation is associated with pterygium growth and symptoms and medical treatments that safely suppress inflammation can stabilize this disease, it is possible that the anti-inflammatory attributes of Mediterranean and traditional diets may play a role in protecting against the severity or progression of this illness.115 Choline (and a metabolite, betaine) has been identified as a likely antiinflammatory component of the Mediterranean diet.116,117 It is possible that sunlight-induced processes such as oxidative stress either in the skin or in the eye would trigger inflammation that would be less well countered in choline deficiency.115 It has been suggested that the low rates of melanoma found in Mediterranean countries could be partly because of a protective effect of the Mediterranean diet.118,119 After carefully controlling for several sun exposure and pigmentary characteristics, a protective effect for weekly consumption of fish, shellfish, drinking tea daily, and a high consumption of vegetables, in particular carrots, cruciferous and leafy vegetables and fruits, and of these in particular citrus fruits, was found.119 Because the incidence of skin cancer is increasing 8 despite the use of externally applied sun protection strategies, it has been proposed119 that nutrients reducing photo-oxidative damage could play a beneficial role in skin cancer prevention. As penetrating photo-oxidative UVA radiation reduces skin and blood antioxidants and damages cell components, dietary antioxidant vitamins, minerals, and phytochemicals, in addition to n-3 polyunsaturated fatty acids, n-9 monounsaturated fatty acids, and low proinflammatory n-6 polyunsaturated fatty acids, have demonstrated protective properties.119 This study concluded that the presence of these substances in the traditional Greek-style Mediterranean diet might have contributed to the low rates of melanoma in the Mediterranean region despite high levels of solar radiation. It has also been suggested that sunlight-induced dermal production of vitamin D may play a role in the benefits of a Mediterranean lifestyle.120 Although this must be balanced against risk (vide infra), this diet may be protective against the development of not only melanoma but also nonmelanoma skin malignancy.121 There is strong circumstantial evidence122–124 that omega-3 fatty acids are also protective against the development of the nonmelanoma skin cancers, such as basal cell and squamous cell carcinomas, that can affect both the eyelids and ocular surface. Vitamin D may also reduce UV-induced DNA damage in skin,125 and there is evidence that a process regulated by the Vitamin D receptor may regulate genoprotection against carcinogenic mutagens in the skin, perhaps involving stem cell populations in the follicle.126 This may be important in pterygium pathogenesis in that pterygium has been reported in diseases in which there is a deficient ability to repair damage caused by UV light such as xeroderma pigmentosum127 and perhaps Cockayne syndrome.128 Thus !internal" protection through dietary and nutritional supplementation could complement the !external" sun-protection strategies that should be in place.115 Yet, we now seem to be sending mixed messages in relation to sun exposure in relation to health. Vitamin D deficiency has become of increasing interest because of its association with many common disease processes and also because of an apparent increase in prevalence—it has been referred to as a world pandemic.129 Humans have evolved to depend on the sun for their vitamin D requirements (wavelengths between 270 and 300 nm130), and although some foods naturally contain vitamin D, foods that are fortified with vitamin D are often inadequate to satisfy vitamin D requirements.131,132 It is the view of some individuals that recommendations for the avoidance of all sun exposure has put the world’s population at risk of developing vitamin D deficiency.129,131 In Australia, where a dramatic increase in skin cancer rates resulted in the promotion of never exposing the skin to direct sunlight without sun protection—clothing or sunscreen, the so-called ‘‘sun-safe’’ message, resulted in a marked increase in the risk of developing vitamin D deficiency.133 A recent review134 has concluded that sunscreen, in the manner used by the general public, does not cause vitamin D insufficiency. It identifies that implementing guidelines suggesting that sun exposure duration for sufficient vitamin D production is limited by the complex interaction of contributory factors and that no recommendation can be made that is both safe and accurate enough for general public usage. There is thus a need to balance the risk of skin cancer and the ophthalmohelioses from too much sun exposure with maintaining adequate vitamin D levels to maintain general health, including maintaining bone mass and perhaps avoiding myopia by avoiding Eye & Contact Lens ! Volume 0, Number 0, Month 2011 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 too little sun exposure. The eye may play a role in this process—if we can teach children and teenagers about early sun-related eye damage,93 it may be possible to give a personalized recommendation to changes in their lifestyle. This approach has the possibility of reducing morbidity, mortality, improving quality of life, and reducing the cost to society of diseases that may well prove to be avoidable. ACKNOWLEDGMENTS Much of the work summarized in this overview is the result of long-term collaborations with Denis Wakefield, Nick di Girolamo, Jeanie Chui, and David Mackey. Jeanie Chui provided assistance with Figure 3 and its description. REFERENCES 1. Coroneo MT. Albedo concentration in the anterior eye and the ophthalmohelioses. Master of Surgery Thesis, University of N.S.W, 1992. 2. Coroneo MT, Müller-Stolzenburg NW, Ho A. Peripheral light focusing by the anterior eye and the ophthalmohelioses. Ophthalmic Surg 1991;22:705–711. 3. Welch RP. A Familiar Treatise on Diseases of the Eye. Sydney, Australia, T. Trood, 1840. 4. Gye C. The Cockney and the Crocodile. London, United Kingdom, Faber and Faber, 1962. 5. Kerkenezov N. A ptergium survey of the far north coast of New South Wales. Trans Ophthalmol Soc Aust 1956;16:110–119. 6. Lancaster HO. Some geographical aspects of the mortality from melanoma in Europeans. Med J Aust 1956;43:1082–1087. 7. Cameron M. Pterygium Throughout the World. Springfield, IL, Charles C Thomas, 1965. 8. Urbach F. Geographic pathology of skin cancer. In: Urbach F, ed. The Biologic Effects of Ultraviolet Radiation. Oxford, Pergamon, 1969, pp 635–650. 9. Norn MS. Prevalence of pinguecula in Greenland and in Copenhagen, and its relation to pterygium and spheroid degeneration. Acta Ophthalmol (Copenh) 1979;57:96–105. 10. Norn MS. Spheroidal degeneration, keratopathy, pinguecula, and pterygiumin Japan (Kyoto). Acta Ophthal Scand 1984;62:54–60. 11. Panchapakesan J, Hourihan F, Mitchell P. Prevalence of pterygium and pinguecula: The blue mountains eye study. Aust N Z J Ophthalmol 1998; 26(suppl 1):S2–S5. 12. Wittenberg S. Solar radiation and the eye: A review of knowledge relevant to eye care. Am J Optom Physiol Optics 1986;63:676–689. 13. Sliney DH. Geometrical assessment of ocular exposure to environmental UV radiation—Implications for ophthalmic epidemiology. J Epidemiol 1999;9(suppl 6):S22–S32. 14. Evans T.A new operation for pterygium. Transactions of the Third Session, Intercolonial Medical Congress of Australasia, Sydney, Australia, 1892. Charles Potter Govt Printer, 1893. 15. D’Ombrain A. The surgical treatment of pterygium. Br J Ophthalmol 1948; 32:65–71. 16. Saad RS. Pterygium, pinguecula and visual acuity. Aust J Ophthal 1977;5:52–66. 17. Jensen OL. Pterygium, the dominant eye and the habit of closing one eye in sunlight. Acta Ophthalmol (Copenh) 1982;60:568–574. 18. Moran DJ, Hollows FC. Pterygium and ultraviolet radiation: A positive, correlation. Br J Ophthalmol 1984;68:343–346. 19. Symons MJ. Some remarks on pterygium. The Australasian Medical Gazette. 1888;7:162–164. 20. National Trachoma and Eye Health Program. Sydney, Australia, Royal Australian College of Ophthalmologists, 1980. 21. Dawson CR, Juster R, Marx R, et al. Limbal disease in trachoma and other ocular chlamydial infections: Risk factors for corneal vascularisation. Eye 1989;3:204–209. 22. Ben-Amer MI. Pterygium in a Libyan village. Rev Int Trach Pathol Ocul Trop Subtrop Sante Publique 1989;66:63–71. 23. Butler G. On Australian ophthalmia. Lancet 1894;64:415. 24. Kobayashi H, Kohshima S. Unique morphology of the human eye and its adaptive meaning: Comparative studies on external morphology of the primate eye. J Hum Evol 2001;40:419–435. 25. Kobayashi H, Kohshima S. Unique morphology of the human eye. Nature 1997;387:767–768. q 2011 Lippincott Williams & Wilkins UV Radiation and the Anterior Eye 26. Favilla I. Ocular effects of ultraviolet radiation. In: Health Effects of Ozone Layer Depletion. Canberra, Australia, Australian Government Publishing Service, 1989, pp 96–113. 27. Davinger M, Evensen A. Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature 1971;229:560–561. 28. Coroneo MT. Albedo concentration in the anterior eye: A phenomenon that locates some solar diseases. Ophthalmic Surg 1990;21:60–66. 29. Coroneo MT, Muller-Stolzenburg NW, Ho A. Peripheral light focusing by the anterior eye and the ophthalmohelioses. Ophthalmic Surg 1991;22: 705–711. 30. Coroneo MT. Pterygium as an early indicator of ultraviolet insolation: A hypothesis. Br J Ophthalmol 1993;77:734–739. 31. Maloof AJ, Ho A, Coroneo MT. Influence of corneal shape on limbal light focusing. Invest Ophthalmol Vis Sci 1994;35:2592–2598. 32. Kwok LS, Kuznetsov VA, Ho A, et al. Prevention of the adverse photic effects of peripheral light-focusing using UV-blocking contact lenses. Invest Ophthalmol Vis Sci 2003;44:1501–1507. 33. Kwok LS, Daszynski DC, Kuznetsov VA, et al. Peripheral light focusing as a potential mechanism for phakic dysphotopsia and lens phototoxicity. Ophthalmic Physiol Opt 2004;24:119–129. 34. von Helmoltz H. Treatise on physiological optics. In: Southall JPC, ed. Mechanism of Accommodation. Vols. 1 and 12. 3rd ed. New York, NY, Dover Publications, 1962, pp 143–172. 35. Graves B. Diseases of the cornea. In: Berens C, ed. The Eye and its Diseases, Chapter XXV. Philadelphia, PA, WB Saunders, 1936, pp 443–557. 36. Mackevicius L. Pterygium. Probable etiology due to persistent photothermal microtrauma. Arch Oftalmol B Aires 1968;43:126–130. 37. Rizzuti AB. Diagnostic illumination test for keratoconus. Am J Ophthalmol 1970;70:141–143. 38. Taylor RL, Hanks MA. Developmental changes in precursor lesions of bovine ocular carcinoma. Vet Med Small Anim Clin 1972;67:669–671. 39. Arenas E. Etiopatologia de la pinguecula y el pterigio. Pal Oftal Panam 1978 2:28–31. 40. Diponegoro RMA, Mulock-Hower AW. A statistical contribution to the study of the aetiology of pterygium. Folia Ophthalmol Orient 1936;2:195–210. 41. Detels R, Dhir SP. Pterygium: A geographical study. Arch Ophthalmol 1967;78:485–491. 42. Dolezalova V. Is the occurrence of a temporal pterygium really so rare? Ophthalmologica 1977;174:88–91. 43. Wu K, He M, Xu J, et al. Pterygium in aged population in Doumen County, China. Yan Ke Xue Bao 2002;18:181–184. 44. Handmann M. Ueber den Beginn des altersstares in der unterenlinsenhalfte. Klinischstatistische Studien an 845 Augen mit Cataracta senilis incipiens nebst Bemerkungen über die Cataracta glaukomatosa und diabetica. Klin Montsbl Augenheilkd 1909;47:692–720. 45. Hoover HL. Solar ultraviolet irradiation of the human cornea, lens, and retina: Equations of ocular irradiation. Appl Optics 1986;25:359–368. 46. Podskochy A. Protective role of corneal epithelium against ultraviolet radiation damage. Acta Ophthalmol Scand 2004;82:714–717. 47. Mootha VV, Pingree M, Jaramillo J. Pterygia with deep corneal changes. Cornea 2004;23:635–638. 48. Chui J, Di Girolamo N, Coroneo MT. The role of substance P in the pathogenesis of pterygia. Invest Ophthalmol Vis Sci 2007;48:4482–4489. 49. Maloof AJ, Ho A, Coroneo MT. Anterior segment peripheral light concentration and the crystalline lens. Invest Ophthalmol Vis Sci 1994;35,1327. Abstract 332. 50. Duke-Elder S, MacFaul PA. Radiational injuries. In: System of Ophthalmology. Injuries, Part 2, Non-Mechanical Injuries. Vol. XIV. London, United Kingdom, Henry Kimpton, 1972, pp 837–1010. 51. Rochtchina E, Mitchell P, Coroneo M, et al. Lower nasal distribution of cortical cataract: The blue mountains eye study. Clin Exper Ophthalmol 2001;29:111–115. 52. Abraham AG, Cox C, West S. The differential effect of ultraviolet light exposure on cataract rate across regions of the lens. Invest Ophthalmol Vis Sci 2010;51:3919–3923. 53. Lofgren S, Ayala M, Kakar M, et al. UVR cataract after regional in vitro lens exposure. Invest Ophthalmol Vis Sci 2002;43. E-Abstract 3577. 54. Coroneo MT, Pham T, Kwok LS. Off-axis edge glare in pseudophakic dysphotopsia. J Cataract Refract Surg 2003;29:1969–1973. 55. Coroneo M. Consultation section. J Cataract Refract Surg 2005;31:652–653. 56. Coroneo MT. Consultation section. Cataract surgical problem. Consultation response. J Cataract Refract Surg 2011;37:424–425. 57. Kwok LS, Coroneo MT. A model for pterygium formation. Cornea 1994; 13:219–224. 58. Kwok LS, Coroneo MT. Temporal and spatial growth patterns in the normal and cataractous human lens. Exp Eye Res 2000;71:317–322. 9 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. M. Coroneo 59. Liu S, Li J, Tan DT, et al. The eyelid margin: A transitional zone for 2 epithelial phenotypes. Arch Ophthalmol 2007;125:523–532. 60. Lindgren G, Diffey BL, Larko O. Basal cell carcinoma of the eyelids and solar ultraviolet radiation exposure. Br J Ophthalmol 1998;82:1412–1415. 61. Taylor HR, West S, Muñoz B, et al. The long-term effects of visible light on the eye. Arch Ophthalmol 1992;110:99–104. 62. Chui J, Coroneo MT, Tat LT, et al. Ophthalmic pterygium: A stem cell disorder with premalignant features. Am J Pathol 2011;178:817–827. 63. Coroneo MT, Di Girolamo N, Wakefield D. The pathogenesis of pterygia. Curr Opin Ophthalmol 1999;10:282–288. 64. Di Girolamo N, Chui J, Coroneo MT, et al. Pathogenesis of pterygia: Role of cytokines, growth factors, and matrix metalloproteinases. Prog Retin Eye Res 2004;23:195–228. 65. Chui J, Coroneo MT. Pterygium pathogenesis, actinic damage, and recurrence. Chapter 1. In: Hovanesian J, ed. Pterygium: Techniques and Technologies for Surgical Success. Thorofare, NJ, Slack, in press. 66. Chui J, Di Girolamo N, Wakefield D, et al. The pathogenesis of pterygium: Current concepts and their therapeutic implications. Ocul Surf 2008;26–47. 67. Di Girolamo N, Tedla N, Kumar RK, et al. Culture and characterisation of epithelial cells from human pterygia. Br J Ophthalmol 1999;83: 1077–1082. 68. Kato N, Shimmura S, Kawakita T, et al. Beta-catenin activation and epithelial-mesenchymal transition in the pathogenesis of pterygium. Invest Ophthalmol Vis Sci 2007;48:1511–1517. 69. Di Girolamo N, McCluskey P, Lloyd A, et al. Expression of MMPs and TIMPs in human pterygia and cultured pterygium epithelial cells. Invest Ophthalmol Vis Sci 2000;41:671–679. 70. Di Girolamo N, Wakefield D, Coroneo MT. Differential expression of matrix metalloproteinases and their tissue inhibitors at the advancing pterygium head. Invest Ophthalmol Vis Sci 2000;41:4142–4149. 71. Di Girolamo N, Coroneo MT, Wakefield D. Active matrilysin (MMP-7) in human pterygia: Potential role in angiogenesis. Invest Ophthalmol Vis Sci 2001;42:1963–1968. 72. Di Girolamo N, Coroneo MT, Wakefield D. UVB-elicited induction of MMP-1 expression in human ocular surface epithelial cells is mediated through the ERK1/2 MAPK-dependent pathway. Invest Ophthalmol Vis Sci 2003;44:4705–4714. 73. Di Girolamo N, Coroneo M, Wakefield D. Epidermal growth factor receptor signaling is partially responsible for the increased matrix metalloproteinase-1 expression in ocular epithelial cells after UVB radiation. Am J Pathol 2005;167: 489–503. 74. Di Girolamo N, Kumar RK, Coroneo MT, et al. UVB-mediated induction of interleukin-6 and -8 in pterygia and cultured human pterygium epithelial cells. Invest Ophthalmol Vis Sci 2002;43:3430–3437. 75. Di Girolamo N, Wakefield D, Coroneo MT. UVB-mediated induction of cytokines and growth factors in pterygium epithelial cells involves cell surface receptors and intracellular signaling. Invest Ophthalmol Vis Sci 2006;47:2430–2437. 76. Yang SF, Lin CY, Yang PY, et al. Increased expression of gelatinase (MMP-2 and MMP-9) in pterygia and pterygium fibroblasts with disease progression and activation of protein kinase C. Invest Ophthalmol Vis Sci 2009;50:4588–4589. 77. Seo MJ, Kim JM, Lee MJ, et al. The therapeutic effect of DA-6034 on ocular inflammation via suppression of MMP-9 and inflammatory cytokines and activation of the MAPK signaling pathway in an experimental dry eye model. Curr Eye Res 2010;35:165–175. 78. Li M, Zhang M, Lin Y, et al. Tear function and goblet cell density after pterygium excision. Eye 2007;21:224–228. 79. Yalcin Tok O, Burcu Nurozler A, Ergun G, et al. Topical cyclosporine A in the prevention of pterygium recurrence. Ophthalmologica 2008;222:391–396. 80. Gitter BD, Waters DC, Threlkeld PG, et al. Cyclosporin A is a substance P (tachykinin NK1) receptor antagonist. Eur J Pharmacol 1995;289: 439–446. 81. Nolan TM, DiGirolamo N, Sachdev NH, et al. The role of ultraviolet irradiation and heparin-binding epidermal growth factor-like growth factor in the pathogenesis of pterygium. Am J Pathol 2003;162:567–574. 82. Liu Z, Xie Y, Zhang M. Overexpression of type I growth factor receptors in pterygium. Chin Med J (Engl) 2002;115:418–421. 83. Sachdev NH, Di Girolamo N, Nolan TM, et al. Matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases in the human lens: Implications for cortical cataract formation. Invest Ophthalmol Vis Sci 2004;45:4075–4082. 84. Sachdev NH, Di Girolamo N, McCluskey PJ, et al. Lens dislocation in Marfan syndrome: Potential role of matrix metalloproteinases in fibrillin degradation. Arch Ophthalmol 2002;120:833–835. 10 Eye & Contact Lens ! Volume 0, Number 0, Month 2011 85. Sachdev N, Wakefield D, Coroneo MT. Lens dislocation in Marfan syndrome and UV-B light exposure. Arch Ophthalmol 2003;121:585. 86. Ng J, Coroneo MT, Wakefield D, et al. Ultraviolet radiation and the role of matrix metalloproteinases in the pathogenesis of ocular surface squamous neoplasia. Invest Ophthalmol Vis Sci 2008;49:5295–5306. 87. Skippen B, Tsang HH, Assaad NN, et al. Rapid response of refractory ocular surface dysplasia to combination treatment with topical all-trans retinoic acid and interferon alpha-2b. Arch Ophthalmol 2010;128:1368–1369. 88. Hollows FC. Ultraviolet radiation and eye diseases. Trans Menzies Foundation 1989;15:113–117. 89. Sinclair C, Foley P. Skin cancer prevention in Australia. Br J Dermatol 2009:161(suppl 3):116–123. 90. Lee GA, Hirst LW, Sheehan M. Knowledge of sunlight effects on the eyes and protective behaviors in adolescents. Ophthalmic Epidemiol 1999;6: 171–180. 91. Livingston PM, White V, Hayman J, et al. Sun exposure and sun protection behaviours among Australian adolescents: Trends over time. Prev Med 2003;37:577–584. 92. Livingston PM, White V, Hayman J, et al. Australian adolescents’ sun protection behavior: Who are we kidding? 20070604 DCOM–20070802. 93. Ooi JL, Sharma NS, Papalkar D, et al. Ultraviolet fluorescence photography to detect early sun damage in the eyes of school-aged children. Am J Ophthalmol 2006;141:294–298. 94. Ooi JL, Sharma NS, Sharma S, et al. Ultraviolet fluorescence photography: Patterns in established pterygia. Am J Ophthalmol 2007;143:97–101. 95. Krengel S. Wearing sunglasses a risk factor for the development of cutaneous malignant melanoma? Int J Dermatol 2002;41:191–192. 96. Threlfall TJ. Sunglasses and clothing—An unhealthy correlation? Aust J Public Health 1992;16:92–196. 97. Hedblom EE. Snowscape eye protection. Development of a sunglass for useful vision with comfort from antarctic snowblindness, glare, and calorophthalgia. Arch Environ Health 1961;2:685–704. 98. Deaver DM, Davis J, Sliney DH. Vertical visual fields-of-view in outdoor daylight. Lasers Light Ophthalmol 1996;7:121–125. 99. Sliney DH. Photoprotection of the eye—UV radiation and sunglasses. J Photochem Photobiol B 2001;64:166–175. 100. Morris A, Temme LA, Hamilton PV. Visual acuity of the U.S. Navy jet pilot and the use of the helmet sun visor. Aviat Space Environ Med 1991;62: 715–721. 101. Dille JR, Marano JA. The effects of spectacle frames on field of vision. Aviat Space Environ Med 1984;55:957–959. 102. Steel SE, Mackie SW, Walsh G. Visual field defects due to spectacle frames: Their prediction and relationship to UK driving standards. Ophthalmic Physiol Opt 1996;16:95–100. 103. ISO DIS 12312-1 Eye and face protection—Sunglasses and related eyewear—Part 1: Sunglasses for general use. 2010. 104. Rosenthal FS, Bakalian AE, Lou CQ, et al. The effect of sunglasses on ocular exposure to ultraviolet radiation. Am J Public Health 1988;78:72–74. 105. Hickson-Curran SB, Nason RJ, Becherer PD, et al. Clinical evaluation of ACUVUE contact lenses with UV blocking characteristics. Optom Vis Sci 1997;74:632–638. 106. Giasson CJ, Quesnel NM, Boisjoly H. The ABCs of ultraviolet-blocking contact lenses: An ocular panacea for ozone loss? Int Ophthalmol Clin 2005;45:117–139. 107. Walsh JE, Bergmanson JP, Saldana G Jr, et al. Can UV radiation-blocking soft contact lenses attenuate UV radiation to safe levels during summer months in the southern United States? Eye Contact Lens 2003;29(suppl 1): S174–S179; discussion S190–S191, S192–S194. Erratum in: Eye Contact Lens 2003;29:135. 108. Walsh JE, Bergmanson JP, Wallace D, et al. Quantification of the ultraviolet radiation (UVR) field in the human eye in vivo using novel instrumentation and the potential benefits of UVR blocking hydrogel contact lens. Br J Ophthalmol 2001;85:1080–1085. 109. Bergmanson JP, Pitts DG, Chu LW. The efficacy of a UV-blocking soft contact lens in protecting cornea against UV radiation. Acta Ophthalmol (Copenh) 1987;65:279–286. 110. Bergmanson JP, Pitts DG, Chu LW. Protection from harmful UV radiation by contact lenses. J Am Optom Assoc 1988;59:178–182. 111. Bergmanson JP, Walsh JE, Harmey J. UV Overdose vs hyperoxia. Eye Contact Lens 2005;31:95. 112. Sasaki K, Sasaki H, Honda R, et al. High prevalence of pterygium in the population of a tropical area in China—Sanya eye study. Invest Opthalmol Vis Sci 2007;48:E-5292. 113. Beard HH, Dimitry JT. Some observations upon the chemical nature of the pterygium. Am J Ophthal 1945;28:303–305. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited. Eye & Contact Lens ! Volume 0, Number 0, Month 2011 114. Ascher KW, Anderson JR. A pterygium map. Acta XVII Conc Ophthal 1954;3:1640–1641. Discussion. 115. Coroneo MT, Coroneo H. Feast Your Eyes: The Eye Health Cookbook. West Lakes, S. Australia, Seaview Press, 2010. ISBN 9781740085618. 116. Detopoulou P, Panagiotakos DB, Antonopoulou S, et al. Dietary choline and betaine intakes in relation to concentrations of inflammatory markers in healthy adults: The ATTICA study. Am J Clin Nutr 2008;87: 424–430. 117. Zeisel SH. Is there a new component of the Mediterranean diet that reduces inflammation? Am J Clin Nutr 2008;87:277–278. 118. Fortes C, Mastroeni S, Melchi F, et al. A protective effect of the Mediterranean diet for cutaneous melanoma. Int J Epidemiol 2008;37:1018–1029. 119. Shapira N. Nutritional approach to sun protection: A suggested complement to external strategies. 2010;68:75–86. 120. Wong A. Incident solar radiation and coronary heart disease mortality rates in Europe. Eur J Epidemiol 2008;23:609–614. 121. Black HS, Rhodes LE. The potential of omega-3 fatty acids in the prevention of non-melanoma skin cancer. Cancer Detect Prev 2006;30: 224–232. 122. Jackson MJ, Jackson MJ, McArdle F, et al. Effects of micronutrient supplements on UV-induced skin damage. Proc Nutr Soc 2002;61:187–189. 123. Black HS, Rhodes LE. The potential of omega-3 fatty acids in the prevention of non-melanoma skin cancer. Cancer Detect Prev 2006;30: 224–232. q 2011 Lippincott Williams & Wilkins UV Radiation and the Anterior Eye 124. Kune GA, Bannerman S, Field B, et al. Diet, alcohol, smoking, serum betacarotene, and vitamin A in male nonmelanocytic skin cancer patients and controls. Nutr Cancer 1992;18:237–244. 125. Mason RS, Sequeira VB, Dixon KM, et al. Photoprotection by 1alpha, 25dihydroxyvitamin D and analogs: Further studies on mechanisms and implications for UV-damage. J Steroid Biochem Mol Biol 2010;121:164–168. 126. Dowd DR, MacDonald PN. The 1, 25-dihydroxyvitamin D3-independent actions of the vitamin D receptor in skin. J Steroid Biochem Mol Biol 2010;121: 317–321. 127. Goyal JL, Rao VA, Srinivasan R, et al. Oculocutaneous manifestations in xeroderma pigmentosa. Br J Ophthalmol 1994;78:295–297. 128. MacKenzie F, Hirst LW, Hilton A. Pterygia and retinitis pigmentosa. Aust N Z J Ophthalmol 1994;22:145–146. 129. Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr 2008;87:S1080–S1086. 130. Hume EM, Lucas NS, Smith HH. On the absorption of vitamin D from the skin. Biochem J 1927;21:362–367. 131. Wolpowitz D, Gilchrest BA. The vitamin D questions: How much do you need an how should you get it? J Am Acad Dermatol 2006;54:301–317. 132. Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med 2009;169:626–632. 133. McGrath JJ, Kimlin MG, Saha SM, et al. Vitamin D insufficiency in southeast Queensland. Med J Aust 2001;174:150–151. 134. Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther 2010;23:48–60. 11 Copyright @ Contact Lens Association of Opthalmologists, Inc. Unauthorized reproduction of this article is prohibited.