Thermally Induced Apoptosis, Necrosis, and Heat Shock Protein
advertisement
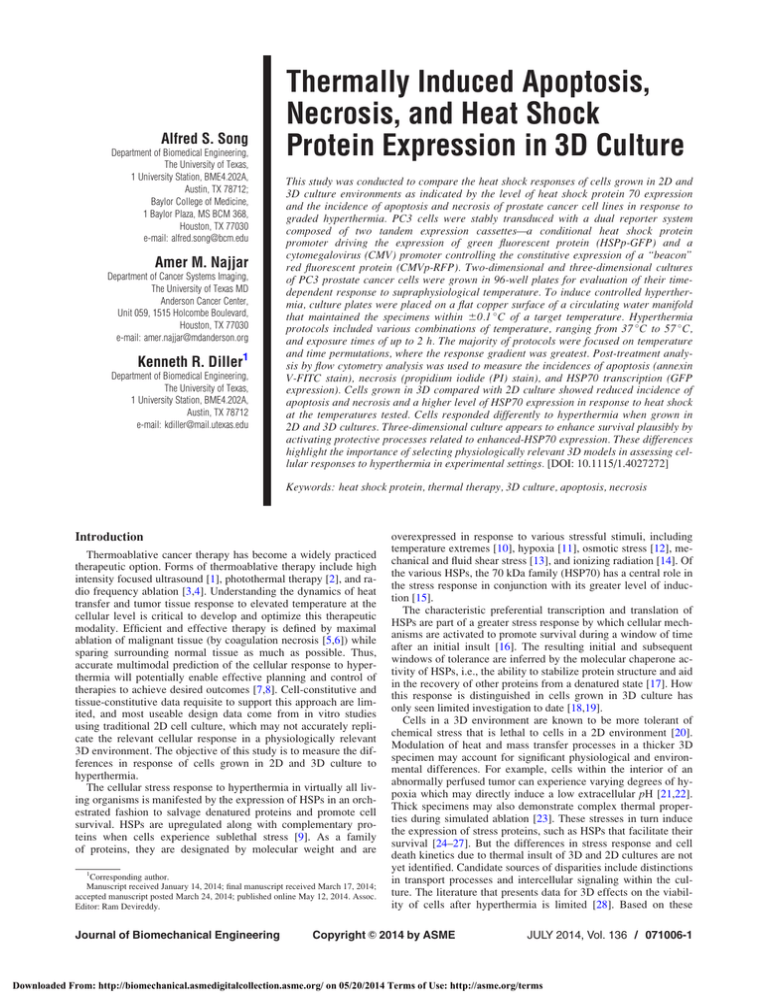
Alfred S. Song Department of Biomedical Engineering, The University of Texas, 1 University Station, BME4.202A, Austin, TX 78712; Baylor College of Medicine, 1 Baylor Plaza, MS BCM 368, Houston, TX 77030 e-mail: alfred.song@bcm.edu Amer M. Najjar Department of Cancer Systems Imaging, The University of Texas MD Anderson Cancer Center, Unit 059, 1515 Holcombe Boulevard, Houston, TX 77030 e-mail: amer.najjar@mdanderson.org Kenneth R. Diller1 Department of Biomedical Engineering, The University of Texas, 1 University Station, BME4.202A, Austin, TX 78712 e-mail: kdiller@mail.utexas.edu Thermally Induced Apoptosis, Necrosis, and Heat Shock Protein Expression in 3D Culture This study was conducted to compare the heat shock responses of cells grown in 2D and 3D culture environments as indicated by the level of heat shock protein 70 expression and the incidence of apoptosis and necrosis of prostate cancer cell lines in response to graded hyperthermia. PC3 cells were stably transduced with a dual reporter system composed of two tandem expression cassettes—a conditional heat shock protein promoter driving the expression of green fluorescent protein (HSPp-GFP) and a cytomegalovirus (CMV) promoter controlling the constitutive expression of a “beacon” red fluorescent protein (CMVp-RFP). Two-dimensional and three-dimensional cultures of PC3 prostate cancer cells were grown in 96-well plates for evaluation of their timedependent response to supraphysiological temperature. To induce controlled hyperthermia, culture plates were placed on a flat copper surface of a circulating water manifold that maintained the specimens within 60.1 C of a target temperature. Hyperthermia protocols included various combinations of temperature, ranging from 37 C to 57 C, and exposure times of up to 2 h. The majority of protocols were focused on temperature and time permutations, where the response gradient was greatest. Post-treatment analysis by flow cytometry analysis was used to measure the incidences of apoptosis (annexin V-FITC stain), necrosis (propidium iodide (PI) stain), and HSP70 transcription (GFP expression). Cells grown in 3D compared with 2D culture showed reduced incidence of apoptosis and necrosis and a higher level of HSP70 expression in response to heat shock at the temperatures tested. Cells responded differently to hyperthermia when grown in 2D and 3D cultures. Three-dimensional culture appears to enhance survival plausibly by activating protective processes related to enhanced-HSP70 expression. These differences highlight the importance of selecting physiologically relevant 3D models in assessing cellular responses to hyperthermia in experimental settings. [DOI: 10.1115/1.4027272] Keywords: heat shock protein, thermal therapy, 3D culture, apoptosis, necrosis Introduction Thermoablative cancer therapy has become a widely practiced therapeutic option. Forms of thermoablative therapy include high intensity focused ultrasound [1], photothermal therapy [2], and radio frequency ablation [3,4]. Understanding the dynamics of heat transfer and tumor tissue response to elevated temperature at the cellular level is critical to develop and optimize this therapeutic modality. Efficient and effective therapy is defined by maximal ablation of malignant tissue (by coagulation necrosis [5,6]) while sparing surrounding normal tissue as much as possible. Thus, accurate multimodal prediction of the cellular response to hyperthermia will potentially enable effective planning and control of therapies to achieve desired outcomes [7,8]. Cell-constitutive and tissue-constitutive data requisite to support this approach are limited, and most useable design data come from in vitro studies using traditional 2D cell culture, which may not accurately replicate the relevant cellular response in a physiologically relevant 3D environment. The objective of this study is to measure the differences in response of cells grown in 2D and 3D culture to hyperthermia. The cellular stress response to hyperthermia in virtually all living organisms is manifested by the expression of HSPs in an orchestrated fashion to salvage denatured proteins and promote cell survival. HSPs are upregulated along with complementary proteins when cells experience sublethal stress [9]. As a family of proteins, they are designated by molecular weight and are 1 Corresponding author. Manuscript received January 14, 2014; final manuscript received March 17, 2014; accepted manuscript posted March 24, 2014; published online May 12, 2014. Assoc. Editor: Ram Devireddy. Journal of Biomechanical Engineering overexpressed in response to various stressful stimuli, including temperature extremes [10], hypoxia [11], osmotic stress [12], mechanical and fluid shear stress [13], and ionizing radiation [14]. Of the various HSPs, the 70 kDa family (HSP70) has a central role in the stress response in conjunction with its greater level of induction [15]. The characteristic preferential transcription and translation of HSPs are part of a greater stress response by which cellular mechanisms are activated to promote survival during a window of time after an initial insult [16]. The resulting initial and subsequent windows of tolerance are inferred by the molecular chaperone activity of HSPs, i.e., the ability to stabilize protein structure and aid in the recovery of other proteins from a denatured state [17]. How this response is distinguished in cells grown in 3D culture has only seen limited investigation to date [18,19]. Cells in a 3D environment are known to be more tolerant of chemical stress that is lethal to cells in a 2D environment [20]. Modulation of heat and mass transfer processes in a thicker 3D specimen may account for significant physiological and environmental differences. For example, cells within the interior of an abnormally perfused tumor can experience varying degrees of hypoxia which may directly induce a low extracellular pH [21,22]. Thick specimens may also demonstrate complex thermal properties during simulated ablation [23]. These stresses in turn induce the expression of stress proteins, such as HSPs that facilitate their survival [24–27]. But the differences in stress response and cell death kinetics due to thermal insult of 3D and 2D cultures are not yet identified. Candidate sources of disparities include distinctions in transport processes and intercellular signaling within the culture. The literature that presents data for 3D effects on the viability of cells after hyperthermia is limited [28]. Based on these C 2014 by ASME Copyright V JULY 2014, Vol. 136 / 071006-1 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms documented observations, we hypothesized that cells growing in 3D culture, which more closely mimics an in vivo environment, will be more resistant to heat-induced stress response than cells cultured in 2D. The work presented herein provides specific evidence of dissimilarities between thermally induced cell death and HSP70 expression in 2D and 3D cultures of prostate cancer cells, including data relating to a potential mechanism of action. Materials and Methods Cells. Human prostate cancer cells (American Type Tissue Collection, Cat No. CRL-1435TM) were maintained in a tissue culture incubator at 37 C with 95% relative humidity and 5% CO2 in F12K Kaighn’s Modification (Gibco, Cat No. 21127) supplemented with 10% certified fetal bovine serum (Gibco LOT: 776620), and 1% Penicillin–Streptomycin. In other experiments, PC3 cells were transduced with a retrovirus to stably express a dual reporter system composed of two tandem expression cassettes—a conditional HSP70 promoter driving the expression of green fluorescent protein (HSPp-GFP) and a CMV promoter controlling the constitutive expression of a “beacon” tdTomato (CMVp-tdTomato). These cells, designated PC3-HSPp-GFP/ CMVp-tdTomato, were sorted three times to enrich the transgeneexpressing population. Two-Dimensional Cell Culture. Cells to be analyzed by flow cytometry were maintained in polystyrene culture vessels. The growth media was changed every third day, and cells were tested when approximately 70% confluent. The cells were passed as needed, or when plates reached approximately 90% confluence, by washing with phosphate buffered saline, release with a solution of 0.25% trypsin, and plating into the desired vessel. 3D Cell Culture. Phenol red free high concentration Matrigel (BD Biosciences Cat No. 354262) was used in a 1:2 dilution with complete media to create a gelled layer at least 1 mm thick, resulting in a volume of 35–50 ll in each well of a 96 well plate. The coated plate was kept at 4 C overnight to dissipate air bubbles and to level the surface of the Matrigel. Coated plates were placed in an incubator for at least 2 h to solidify the Matrigel prior to seeding. Control 2D cultures were seeded on the same plates in wells adjacent to Matrigel. After seeding, the cells were allowed to attach overnight (at least 8 h) prior to heating and analysis. Cell Viability Measurement by Colorimetric Assay. Watersoluble tetrazolium, WST-1, was utilized to determine the thermal dose range at which transition to irreversible cell injury occurs. Cells were cultured in 2D culture until 70% confluent, harvested with 0.25% trypsin, counted using a hemocytometer, diluted with complete media, and aliquoted into thin walled PCR tubes at a density of 15,000 cells in 100 ll of growth media. Twelve samples were then heated simultaneously in an Eppendorf thermal cycler across a thermal gradient with temperatures corresponding to 37, 37.4, 38.7, 40.6, 42.9, 45.5, 48.2, 50.8, 53.2, 55.2, 56.5, and 57.2 C for durations of 5, 10, 15, 20, 30, 60, 90, and 120 min. All samples were subsequently transferred to an optical 96 well plates after heating and placed in an incubator. Ten microliters of Roche Cell Proliferation Reagent WST-1 (Cat No. 05015944001) was added to each well 1 h prior to analysis on a Tecan Safire microplate reader 24 h after heat shock. Heating and Recovery of Cells for Flow Cytometry. A custom designed and fabricated controlled temperature water circulation chamber was utilized to heat cells in 96 well culture plates for subsequent analysis by flow cytometry. The chamber consisted of a flat copper upper surface onto which culture plates could be placed and a lower volume with inlet and outlet ports through which water from a bath was circulated to cause uniform forced convection heating on the bottom of the copper plate. The chamber maintained the solution within the culture plate wells within 60.1 C of a target temperature in both space and time. The chamber and water bath assembly were contained in an insulated housing with air circulated and heated by a proportional-integral-derivative (PID) control system to match the target temperature. The apparatus was preheated for 30 min prior to use to minimize the thermal transients. Culture plates were placed on the heated copper surface with a minimal layer of water from the bath to minimize thermal contact resistance between the two solid surfaces. Understanding that experimental apparatus can affect the thermal history of specimen [29], this apparatus and protocol represent a best effort to reduce thermal transients as well as contamination of the cell cultures. Immediately following heat shock, plates were placed in an incubator at 37 C, 95% relative humidity, and 5% CO2 until 2 h prior to analysis, which amounted to 10 or 22 h of recovery at 37 C followed by 3–4 h of preparation and analysis at 4 C. Incubation of the cells at 4 C during the preparation time interval results in a 4-fold to 6-fold decrease in reaction rate, which indicates that cellular kinetics are not significantly altered during the sample preparation time from the experimental end-point until analysis [30]. Harvesting of Cells From 2D and 3D Culture for Flow Cytometry. Cells were harvested by first liquefying the Matrigel on ice for at least 30 min and transferring the overlaying growth media to a 15 ml conical tube prechilled on ice. Ice cold BD cell recovery solution (Cat No. 354253) and 0.25% trypsin were mixed at a 1:1 ratio, and 200 ll was added to the culture vessels to further release the cells within the Matrigel layer. An additional 100 ll of cold trypsin was added to the culture vessels which were then incubated at 37 C for 15 min before the contents were transferred to a 15 ml conical tube. Trypsin was neutralized by adding 1 ml of cold media with serum. Cells were centrifuged at 400 g, the supernatant aspirated, and the pellet resuspended in 100 ll of media, and prepared for analysis with either annexin V-FITC and PI or green fluorescence (EGFP). Annexin V-FITC/PI Staining and EGFP Analysis for Flow Cytometry. Flow cytometry analysis was performed on a FACS Calibur flow cytometer (BD Biosciences). The proportion of apoptotic and necrotic events within a cell population was determined by flow cytometry analysis based on annexin V-FITC and PI staining (BD Biosciences Cat No. 556547). Cells which were annexin V-FITC positive but PI negative were considered to have undergone apoptosis. Cells which were double positive for both fluorophores were counted as necrotic. Cultures were plated overnight, heated, and harvested approximately 2 h prior to analysis as described above. Cells were resuspended in 110 ll of media containing 5 ll annexin V-FITC and 5 ll PI. Each sample was mixed by gentle pipetting and incubated for 15 min at room temperature in the dark. Cells were diluted by the addition of 400 ll of media and then transferred to plastic flow cytometry tubes. Samples were placed on ice until analysis on a BD Biosciences FACS Calibur flow cytometer. Populations were not gated in apoptosis and necrosis experiments. Thresholds to delineate apoptotic from necrotic populations were set based on control specimen for each individual experiment, such that extreme outlying events were excluded. Expression of HSP70 in PC3-HSPp-GFP/CMVp-tdTomato cells was determined by measuring GFP expression by flow cytometry. Trypsinized cells were suspended in 400 ll of growth media and GFP expression was determined in the gated viable cell population. Inhibition of Caspases for Flow Cytometry. Caspase-3 was inhibited by pre-incubating PC3 cells with Ac-DEVD-CHO (Enzo Life Sciences Cat No. ALX-260-030-M001) at a final concentration of 100 nM for 3 h immediately prior to heat shock. Pan-caspase inhibition was accomplished by pre-incubating cells with 20 lM Z-VAD-FMK (Enzo Life Sciences Cat No. 071006-2 / Vol. 136, JULY 2014 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Transactions of the ASME ALX-260-020-M001) for 30 min prior to heat shock. Heat shock was carried out on the custom designed heating apparatus at 45 C for 120 min followed by a 22-h recovery time prior to analysis. Measurement of Caspase Activity. Caspase-3 enzymatic activity in cell extracts was measured using the substrate AcDEVD-AMC (Enzo Life Sciences Cat No. ALX-260-031-M001), which is fluorescently activated upon catalysis by caspase-3. Cells were grown to 70% confluence in 25 cm2 tissue culture dishes, heated with the water bath chamber, and allowed to recover at 37 C until analyzed at 6, 12, or 24 h. At the time of assay, 100–200 ll of lysis buffer was added (5x Lysis Buffer: 250 mM HEPES pH 7.4, 25 mM CHAPS, 25 mM DTT). Cell lysate was centrifuged at 1000xg to pellet nuclei and debris, and the supernatant was saved and stored at 20 C until analysis. Cell lysate (10 ll) was added to 90 ll of reaction buffer containing 5 lM AcDEVD-AMC 20 mM HEPES pH 7.4, 0.1% CHAPS, 5 mM DDT, 2 mM EDTA. Staurosporine-treated Jurkat cell extract served as the positive control. A Tecan Safire plate reader was used to measure substrate catalysis at excitation and emission wavelengths of 360 6 5 nm and 440 6 10 nm, respectively. Results High Throughput Identification of Peak Metabolic Activity and Viability Threshold. In order to examine the cellular viability during hyperthermia on a broad scope, a wide spectrum of thermal doses was applied to PC3 cells grown in 2D culture. Cellular viability was determined by WST-1 conversion. The objective was to identify the transition conditions at which hyperthermia results in irreversible cellular injury and cell death. This threshold region could be evaluated in greater detail and resolution. Heating duration ranged from 5 to 120 min at temperatures ranging from 37 C to 57.2 C (Fig. 1). The results demonstrate two salient features. First, a peak in metabolic activity (WST-1 indirectly reflects mitochondrial activity) at 42.9 C for 20 min, and second, a clear temperature and duration threshold beginning at 50.8 C for 5 min and gradually declining in temperature as duration increases beyond which cells are fated to undergo cell death by apoptosis or necrosis (black region), and below which cells survive. This threshold region between cell death and cell viability was selected for further detailed examination to determine the relationship between HSP expression and apoptotic events. Thermal Dose to Specifically Evoke Apoptosis or Necrosis 24 h Poststress in 2D Cell Culture. Based on the identified cell viability threshold region, two hyperthermia temperature/time Fig. 1 Normalized WST-1 absorbance of PC3 cells for long durations of heating at various temperatures at approximately 12 h later. Each point is normalized to an average value of WST1 absorbance for cells heated at 37 C, as evidenced by the uniform shade in the 37 C row along the bottom of the figure (n 5 3). Note that the time scale is not linear. Journal of Biomechanical Engineering conditions were selected to more comprehensively study cell viability by the flow cytometry. Apoptosis and necrosis as determined by annexin-V FITC and PI staining, respectively, were used to more precisely define the thermal dose threshold of viability (Fig. 2) for a 10 min heating period in 2D cultures. The threshold between viability and apoptosis appears to occur between 48 C and 52 C, and increasing the thermal dose from 52 C to 60 C for 10 min results in an increasing fraction of cells undergoing necrosis as denoted by the percentage of cells which are annexin/PIþ or annexinþ/PIþ. Lower temperatures in combination with longer heating durations were tested to characterize the effect of more mild but prolonged thermal protocols. Figure 3 shows the results of heating at 44 C for 10, 30, 60, or 120 min. All protocols lasting less than 120 min resulted in minimal cell death by either apoptosis or necrosis. Heating for 120 min caused a more selective shift of the viable population into the apoptotic state. Data for thermal doses 1 C higher at 45 C for 30, 60, 120, or 180 min are shown in Fig. 4. The results demonstrate that a 1 C increase above the threshold temperature of 43 C was sufficient to cause cells to preferentially undergo necrotic cell death. Heating durations of 120 min or more induce a greater portion of cells to undergo necrosis. Based on these experiments, the two thermal doses of 44 C and 45 C for 120 min, which straddle the observed threshold between apoptosis and necrosis, were selected for a more refined analysis of heat-induced cell injury. Caspases are Involved in Thermally Induced Apoptosis. In order to quantify the involvement of caspases in apoptosis, as indicated by annexin V-FITC staining, PC3 cells grown in 2D culture were treated with pan-caspase inhibitor Z-VAD-FMK prior to heating at 45 C-120 min (Figs. 5(a)–5(c)). Analysis was by flow cytometry. In the 45 C-120 min group Z-VAD-FMKþ (Fig. 5(c)), a distinct apoptotic population (annexinþ/PI) is observed that does not appear in the corresponding 45 C-120 min, without ZVAD-FMK-group (Fig. 5(b)). Heating at 45 C for 180 min did not yield similar results, and no outstanding difference between ZVAD-FMK treated and untreated groups was seen. In an attempt to identify the apoptotic mechanism with an individual caspase, caspase 3 inhibitor Ac-DEVD-CHO was applied prior to heating at 45 C for 180 min and flow cytometry analysis. Figures 5(e) and 5(f) demonstrate no obvious difference between the heated groups that were and were not treated with Ac-DEVDCHO. This result was further confirmed by using the fluorescent caspase-3-specific substrate, Ac-DEVD-AMC, on cellular extracts from cells heated at various thermal doses. The results of these experiments in Fig. 6 demonstrate that none of the thermal doses used induced any measureable Ac-DEVD-AMC fluorescent signal over the broad range of hyperthermia time and temperature. In one case, heating at 40 C for 22 min yielded an elevated background level of fluorescence. However, no time-dependent increase in signal was detected (as observed in the positive control), dismissing the presence of any positive caspase-3 activity. The positive control demonstrated the predicted ramp up in capsase activity. A complementary experiment at 45 C for extended durations of heating up to 180 min also demonstrated the absence of caspase 3 activity (Fig. 7). Apoptosis and Necrosis are Mitigated and HSP70 is Enhanced in 3D Culture. To assess differences in cell viability between 2D and 3D cultures, two identical thermal doses of 44 C and 45 C for 120 min were applied to cells grown in 2D and 3D cultures. These doses define the threshold conditions for injury in 2D cultured cells. The cells were assayed for apoptosis and necrosis 24 h following hyperthermia. The results reported in Fig. 8 show a significantly greater percentage of cells undergoing apoptosis and necrosis in 2D culture than in 3D culture for cells heated at 45 C for 120 min (n ¼ 3, t-test, p < 0.05). There was no JULY 2014, Vol. 136 / 071006-3 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Fig. 2 Apoptosis and necrosis of PC3 cells heated at various temperatures for 10 min. (a) Unheated control, (b) 44 C, (c) 48 C, (d) 52 C, (e) 60 C. Cells were analyzed by flow cytometry using annexin-V FITC and PI staining 24 h after heat shock. statistically significant difference between the 2D and 3D data for heating at 44 C. HSP70 Expression. PC3-p4rep100 cells, which express EGFP under the control of the human HSP70 promoter, were heated at 44 C and 45 C for 10 min and assayed by flow cytometry 12 h later. The data for HSP70 expression in 2D and 3D cultures are reported in Fig. 9. These results show that 3D cultures heated at 45 C for 120 min, but not 44 C for 120 min, have a statistically higher level of HSP70 expression in comparison with 2D cultures (n ¼ 3, t-test p < 0.05). This differential is consistent with that for apoptosis and necrosis for the same hyperthermic conditions. Discussion In order to investigate the effect of a 3D culture environment on thermally induced cell death and HSP70 expression, the authors analyzed cellular heat shock responses across a broad 071006-4 / Vol. 136, JULY 2014 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Transactions of the ASME Fig. 3 Apoptosis and necrosis of PC3 cells heated at 44 C for various durations. (a) Unheated control, (b) 10 min, (c) 30 min, (d) 60 min, (e) 120 min. Cells were analyzed by flow cytometry using annexin-V FITC and PI staining 24 h after heat shock. range of temperatures and heating times using a high-throughput approach. The array of thermal doses used to generate the viability data in Fig. 1 demonstrates two important phenomena. First, a peak of metabolic activity (maximal WST-1 staining) exists in the landscape of thermal doses which we theorize corresponds to maximum cellular activity to repair thermal damage [16]. Second, there is a clear and relatively sharp threshold between viability and cell death. The region straddling this threshold between viability and cell death was chosen to further investigate apoptosis Journal of Biomechanical Engineering and necrosis in 2D and 3D cultures as it provides the greatest response contrast as indicated by cellular viability and HSP70 expression. Thus, the parameters identified in Fig. 1 were used to guide subsequent flow cytometry experiments. Analysis of cellular viability by flow cytometry required the reevaluation of heat shock responses across an array of temperature doses as demonstrated in Figures 2–4. These results illustrate how the temperature and time characteristics of an applied thermal dose dictate the pathways to cell survival or death. Previous JULY 2014, Vol. 136 / 071006-5 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Fig. 4 Flow cytometry scatter plots of PC3 cells heated at 45 C for various durations. (a) Unheated control, (b) 30 min, (c) 60 min, (d) 120 min, (e) 180 min. Cells were analyzed by flow cytometry using annexin-V FITC and PI staining 24 h after heat shock. work in our lab [31,32] and by others [33–35] has demonstrated a threshold of cell viability at a well-defined thermal dose. This type of constitutive data may be useful for treatment planning and real-time estimates of the efficacy of localized thermal therapies. Some types of thermal therapy for cancer may cause sites in the field of thermal stimulation to exceed 98 C and peripheral areas to reach 50 C via ablative methods, which temperatures far exceed threshold injury conditions [36]. Caspase inhibition experiments confirmed the involvement of caspases in thermally induced apoptosis of PC3s, although caspase3 is unlikely to play a direct role as evidenced by specific inhibition via Ac-DEVD-CHO. This finding is corroborated by other works that demonstrate the pan-caspase inhibitor Z-VAD-FMK affects thermal, but not radiation, induced apoptosis in a leukemia cell line, HL60 [37]. Others have demonstrated the selectivity of caspase 9 in thermally induced apoptosis of Jurkat cells [38]. 071006-6 / Vol. 136, JULY 2014 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Transactions of the ASME Fig. 5 Apoptosis and necrosis of PC3 cells heated in the presence of caspase inhibitors. (a)–(c) Pan-caspase inhibition (ZVAD-FMK) with thermal dose of 45 C for 120 min. (d)–(f) Caspase 3 inhibition (Ac-DEVD-CHO) with thermal dose of 45 C for 180 min. (a) Unheated control for Z-VAD-FMK, (b) heated without Z-VAD-FMK, (c) heated with Z-VAD-FMK, (d) unheated control for Ac-DEVD-CHO, (e) heated without Ac-DEVD-CHO, and (f) heated with Ac-DEVD-CHO. A delay in the progression to late apoptosis or necrosis is observed in the presence of inhibitor Z-VAD-FMK. No difference is detected in the presence of caspase 3 inhibitor. Cells were analyzed by flow cytometry using annexin-V FITC and PI staining 24 h after heat shock. The apoptotic population distribution that appears in Fig. 5(c) may be explained by an in vitro artifact referred to as late apoptosis [39], a process by which cells that have undergone apoptosis as a primary means of cell death progress further into necrotic cell death or secondary necrosis and become PI permeable. The process of secondary necrosis is not thought to be observed in vivo due to the presence of phagocytic cells of the reticuloendothelial Journal of Biomechanical Engineering system, i.e., tissue macrophages, which clear apoptotic and necrotic cells and debris before secondary necrosis can take place. In light of this theory of late apoptosis, it seems that inhibition of the caspases may delay the kinetics of this process, thus implicating their role in thermally induced apoptosis. If secondary necrosis is indeed occurring in these experiments, then the observation time points for apoptosis and necrosis experiments should be JULY 2014, Vol. 136 / 071006-7 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Fig. 6 Caspase 3 activity of PC3 cells heated at various temperatures and durations assessed by Ac-DEVD-AMC fluorometric assay. Cells heated for 3 or 5 min (blue markers) and 10 or 22 min (red markers) at 37 C (1), 40 C (䊊), 44 C (w), 50 C (䉫), 55 C (*), 56 C (䉮), 57 C (D), or caspase extract positive control (3). Cells were processed and analyzed at 6, 12, and 24 h after heat shock. Assay duration is approximately 3 h. Y axis units are arbitrary. No caspase 3 activity from PC3 cells was detected. Fig. 8 Apoptosis and necrosis of 2D and 3D cultured PC3 cells after heating. Cells were heated at the indicated temperatures for 120 min and observed 24 h after heat shock. Samples heated at 45 C demonstrate a significant difference (n 5 3, t-test p < 0.05) between 2D and 3D cultures. Populations have been normalized to respective 37 C control groups. Fig. 7 Caspase 3 activity as assessed by Ac-DEVD-AMC fluorometric assay in PC3 Cells. Cells were heated at 45 C at the indicated durations. Negative and positive controls were water and apoptotic Jurkat cell extract, respectively. Cells were processed and analyzed 24 h after heat shock. No significant caspase 3 activity was detected (n 5 3). carefully considered when utilizing the results for data-driven therapeutic systems [7,8]. One option would be to interpolate the kinetics of apoptosis and necrosis separately using the existing data. Alternatively, the percentages of apoptosis and necrosis can be summed to generate a predictive algorithm until further experimental improvements are made in differentiating between cell death kinetics. Having established thermal doses which preferentially lead to apoptosis or necrosis (120 min at 44 C or 45 C, respectively), experiments were repeated to investigate the effect that 3D culture had on the two modes of cell death. Relative apoptotic and necrotic events were significantly depressed in 3D culture compared to 2D culture at a thermal dose of 45 C for 120 min, which defined the threshold region of hyperthermia for induction of thermal injury, indicating a role for protective mechanisms specific to the 3D culture environment. It should be noted that the baseline level of cells which undergo apoptosis or necrosis in 3D cultures is higher than in 2D environments. In these studies, the results were normalized to untreated control to specifically determine the increase or decrease of cellular response, as shown in Fig. 8. The existence of elevated background levels of apoptotic and necrotic cells is consistent with other studies using different 3D matrices, 071006-8 / Vol. 136, JULY 2014 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Transactions of the ASME the details of the underlying mechanism of the observed results, which when clearly understood should inform the treatment planning and clinical management of patients who receive localized thermal therapies. Acknowledgement This research was sponsored by National Science Foundation Grants CNS 0540033, CBET 0828131, and CBET 096998, and the Robert and Prudie Leibrock Professorship in Engineering at the University of Texas at Austin. The authors also would like to acknowledge Andrew Mark in his contribution to the programming of the PID algorithm for the temperature control software of the heating apparatus. References Fig. 9 HSP70 induction in 2D and 3D cultures of PC3 cells at 44 C and 45 C for 120 min. The difference in HSP70 induction between the 2D and 3D culture was found to be statistically significant for heating at 45 C for 120 min (n 5 3, t-test p < 0.001). such as viscose-rayon/styrene butadiene copolymer or agar [19,20]. Upregulation of HSP70 was evaluated as the protective mechanism that reduces the incidence of apoptosis and necrosis in 3D culture. The data in Fig. 9 demonstrate a greater induction of HSP70 expression in 3D cultures at the same thermal dose (45 C for 120 min) for which there was reduced induction of apoptosis and necrosis in Fig. 8. The reason for increased HSP70 expression in 3D culture is not well understood. Khoei et al. have reported a similar observation [19] and attribute the decrease of apoptotic and necrotic events in DU145 spheroids to HSP70 expression. The role of HSP70 in modulating temperature-induced cell death is well-established, and its upregulated expression is likely to be a component of the mechanism by which apoptosis and necrosis are reduced in 3D culture. It is well-established that a high level of heat shock protein expression and HSP70, in particular, correlates with protection from hyperthermia [9,15,16,40]. However, a direct causal relationship between enhanced thermoprotection and elevated HSP70 expression in 3D culture has yet to be established. Other factors may play a role. Extracellular adhesion molecules or intercellular signaling pathways may plausibly play a role in regulating HSP70 expression in 3D cultures. No endogenous intracellular molecules, such as growth factors, are known to affect HSP70 regulatory pathways, although the inverse paradigm has been observed [41–43]. No published work was found to support or refute a direct interaction between cell adhesion molecules and HSP70, but evidence was found for a convergence between various HSPs and integrins upon the pathway of apoptosis or, more precisely, detachment induced apoptosis (anoikis) [44–54]. Conclusions Understanding the role of the extracellular environment and its influence on HSP70 expression will facilitate refinement of thermoablative therapy parameters leading to more effective treatments. The potential for advancing thermoablative therapy, as illustrated by this study, highlights the need to more fully elucidate the role of the extracellular environment in the cellular response to hyperthermia. It can be concluded from this study that the 3D environment of reconstituted basement membrane reduces the induced cell death by apoptosis or necrosis of prostate cancer cell line, PC3, to a thermal dose (45 C–120 min) that preferentially evokes necrosis 24 h postheat shock. HSP70 expression is not simply enhanced in 3D culture for all thermal doses, but rather it is enhanced in the higher thermal dose of 45 C–120 min. This finding may allude to a mechanism of HSP70 expression that is affected by both 3D environment and thermal dose. Future investigation will focus on Journal of Biomechanical Engineering [1] Kennedy, J. E., Ter Haar, G. R., and Cranston, D., 2003, “High Intensity Focused Ultrasound: Surgery of the Future?,” Br. J. Radiol., 76, pp. 590–599. [2] Lal, S., Clare, S. E., and Halas, N. J., 2008, “Nanoshell-Enabled Photothermal Cancer Therapy: Impending Clinical Impact,” Acc. Chem. Res., 41(12), pp. 1842–1851. [3] Goldberg, S. N., and Dupuy, D. E., 2001, “Image-Guided Radiofrequency Tumor Ablation: Challenges and Opportunities—Part I,” J. Vasc. Interv. Radiol., 12(9), pp. 1021–1032. [4] Dupuy, D. E., and Goldberg, S. N., 2001, “Image-Guided Radiofrequency Tumor Ablation: Challenges and Opportunities—Part II,” J. Vasc. Interv. Radiol., 12(10), pp. 1135–1148. [5] Brausi, M., Castagnetti, G., Gavioli, M., Peracchia, G., de Luca, G., and Olmi, R., 2004, “Radio Frequency (RF) Ablation of Renal Tumours Does Not Produce Complete Tumour Destruction: Results of a Phase II Study,” Eur. Urol. Suppl., 3(3), pp. 14–17. [6] Solbiati. L., Ierace, T., Goldberg, S. N., Sironi, S., Livraghi, T., Fiocca, R., Servadio, G., Rizzatto, G., Mueller, P. R., Del Maschio, A., and Gazelle, G. S., 1997, “Percutaneous US-Guided Radio-Frequency Tissue Ablation of Liver Metastases: Treatment and Follow-up in 16 Patients,” Radiology, 202, pp. 195–203. [7] Oden, J. T., Diller, K. R., Bajaj, C., Browne, J. C., Hazle, J. D., Babuska, I., Bass, J., Biduat, L., Demkowicz, L., Elliott, A., Feng, Y., Fuentes, D., Prudhomme, S., Rylander, M. N., Stafford, R. J., and Zhang, Y., 2007, “Dynamic Data-Driven Finite Element Models for Laser Treatment of Cancer,” Numer. Methods Partial Differ. Equation, 23(4), pp. 904–922. [8] Fuentes, D., Oden, J. T., Diller, K. R., Hazle, J. D., Elliott, A., Shetty, A., and Stafford, R. J., 2009, “Computational Modeling and Real-Time Control of Patient-Specific Laser Treatment of Cancer,” Ann. Biomed. Eng., 37, pp. 763–782. [9] Lindquist, S., and Craig, E. A., 1988, “The Heat-Shock Proteins,” Annu. Rev. Genet., 22, pp. 631–677. [10] Lindquist, S., 1986, “The Heat-Shock Response,” Annu. Rev. Biochem., 55, pp. 1151–1191. [11] Yeh, C., Hsu, S., Yang, C., Chien, C., and Wang, N., 2010, “Hypoxic Preconditioning Reinforces HIF-Alpha-Dependent HSP70 Signaling to Reduce Ischemic Renal Failure-Induced Renal Tubular Apoptosis and Autophagy.” Life Sci., 86(3–4), pp. 115–123. [12] Kurz, A. K., Schliess, F., and H€aussinger, D., 1998, “Osmotic Regulation of the Heat Shock Response in Primary Rat Hepatocytes,” Hepatology, 28(3), pp. 774–781. [13] Schett, G., Redlich, K., Xu, Q., Bizan, P., Gr€ oger, M., and Tohidast-Akrad, M., 1998, “Enhanced Expression of Heat Shock Protein 70 (Hsp70) and Heat Shock Factor 1 (HSF1) Activation in Rheumatoid Arthritis Synovial Tissue. Differential Regulation of Hsp70 Expression and HSF1 Activation in Synovial Fibroblasts by Proinflammatory Cytokines, Shear Stress, and Antiinflammatory Drugs,” J. Clin. Invest., 102(2), pp. 302–311. [14] Calini, V., Urani, C., and Camatini, M., 2003, “Overexpression of HSP70 is Induced by Ionizing Radiation in C3H 10T1/2 Cells and Protects From DNA Damage,” Toxicol. in Vitro, 17(5–6), pp. 561–566. [15] Kregel, K. C., 2002, “Heat Shock Proteins: Modifying Factors in Physiological Stress Responses and Acquired Thermotolerance,” J. Appl. Physiol., 92(5), pp. 2177–2186. [16] Diller, K. R., 2006, “Stress Protein Expression Kinetics,” Annu. Rev. Biomed. Eng., 8, pp. 403–424. [17] Calderwood, S. K., Khaleque, M. A., Sawyer, D. B., and Ciocca, D. R., 2006, “Heat Shock Proteins in Cancer: Chaperones of Tumorigenesis,” Trends Biochem. Sci., 31(3), pp. 164–172. [18] Khoei, S., Fazeli, G., Amerizadeh, A., Eslimi, D., and Goliaei, B., 2010, “Elimination of Enhanced Thermal Resistance of Spheroid Culture Model of Prostate Carcinoma Cell Line by Inhibitors of Hsp70 Induction,” Yakhteh Med. J., 12(1), pp. 105–112. Available at: http://celljournal.org/components4. php?rQV==wHQwAkO0JXY0N3XmxHQwYDQ6QWS05WZyFGcfZGfAhjN 1EDQ6QWStVGdp9lZ8BEMApDZJxWY0J3bQxWYuJXdvp2XmxHQyATN ApDZJ52bpR3Yh9lZ [19] Khoei, S., Goliaei, B., Neshasteh-Riz, A., and Deizadji, A., 2004, “The Role of Heat Shock Protein 70 in the Thermoresistance of Prostate Cancer Cell Line Spheroids,” FEBS Lett., 561(1–3), pp. 144–148. JULY 2014, Vol. 136 / 071006-9 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms [20] Sun, T., Jackson, S., Haycock, J. W., and Macneil, S., 2006, “Culture of Skin Cells in 3D Rather Than 2D Improves Their Ability to Survive Exposure to Cytotoxic Agents,” J. Biotech., 122(3), pp. 372–381. [21] Jain, R. K., 2005, “Normalization of Tumor Vasculature: An Emerging Concept in Antiangiogenic Therapy,” Science, 307, pp. 58–62. [22] Harris, A. L., 2002, “Hypoxia—A Key Regulatory Factor in Tumor Growth,” Nature, 2, pp. 38–47. [23] Santos, I., Haemmerich, D., Pinheiro, C., and Rocha, A., 2008, “Effect of Variable Heat Transfer Coefficient on Tissue Temperature Next to a Large Vessel During Radio Frequency Tumor Ablation,” Biomed. Eng. Online, 7(1), p. 21. [24] Gomer, C. J., Ryter, S. W., Ferrario, A., Rucker, N., Wong, S., and Fisher, A. M. R., 1996, “Photodynamic Therapy-Mediated Oxidative Stress can Induce Expression of Heat Shock Proteins,” Cancer Res., 56(10), pp. 2355–2360. Available at: http://cancerres.aacrjournals.org/content/56/10/2355.abstract [25] Luk, J. M., Lam, C.-T., Siu, A. F. M., Lam, B. Y., Ng, I. O. L., and Ju, M.-Y., 2006, “Proteomic Profiling of Hepatocellular Carcinoma in Chinese Cohort Reveals Heat-Shock Proteins (Hsp27, Hsp70, GRP78) Up-Regulation and Their Associated Prognostic Values,” Proteomics, 6(3), pp. 1049–1057. [26] Heacock, C. S., and Sutherland, R. M., 1990, “Enhanced Synthesis of Stress Proteins Caused by Hypoxia and Relation to Altered Cell Growth and Metabolism,” Br. J. Cancer, 62(2), pp. 217–225. [27] Li, G. C., and Shrieve, D. C., 1982, “Thermal Tolerance and Specific Protein Synthesis in Chinese Hamster Fibroblasts Exposed to Prolonged Hypoxia,” Exp. Cell Res., 142(2), pp. 464–468. [28] Khoei, S., Goliaei, B., and Neshasteh-Riz, A., 2004, “Differential ThermoResistance of Multicellular Tumor Spheroids,” Iran. J. Sci. Technol., 28, pp. 107–116. [29] He, X., and Bischof, J. C., 2005, “The Kinetics of Thermal Injury in Human Renal Carcinoma Cells,” Ann. Biomed. Eng., 33(4), pp. 502–510. [30] Connors, K. A., 1990, Chemical Kinetics: The Study of Reaction Rates in Solution, VCH Publishers, Inc., New York. [31] Rylander, M. N., Diller, K. R., Wang, S., and Aggarwal, S. J., 2005, “Correlation of HSP70 Expression and Cell Viability Following Thermal Stimulation of Bovine Aortic Endothelial Cells,” ASME J. Biomech. Eng., 127(5), pp. 751–757. [32] Wang, S., Xie, W., Rylander, M. N., Tucke, P. W., Aggarwal, S. J., and Diller, K. R., 2008, “HSP70 Kinetics Study by Continuous Observation of HSP-GFP Fusion Protein Expression on a Perfusion Heating Stage,” Biotechnol. Bioeng., 99, pp. 146–154. [33] Samali, A., Holmberg, C. I., Sistonen, L., and Orrenius, S., 1999, “Thermotolerance and Cell Death are Distinct Cellular Responses to Stress: Dependence on Heat Shock Proteins,” FEBS Lett., 461(3), pp. 306–310. [34] Huang, C.-T., Lu, Y.-H., and Jen, C.-P., 2010, “Investigation on Supraphysiological Thermal Injury in Two Well-Differentiated Human Hepatoma Cell Lines, Hepg2 and Hep3B,” J. Therm. Biol., 35(8), pp. 411–416. [35] Marylevitch, N. P., Schuschereba, S. T., Mata, J. R., Gilligan, G. R., Lawlor, D. F., and Goodwin, C. W., 1998, “Apoptosis and Accidental Cell Death in Cultured Human Keratinocytes After Thermal Injury,” Am. J. Pathol., 153(2), pp. 567–577. [36] Madersbacher, S., Pedevilla, M., Vingers, L., Susani, M., and Marberger, M., 1995, “Effect of High-Intensity Focused Ultrasound on Human Prostate Cancer in Vivo,” Cancer Res., 55(15), pp. 3346–3351. Available at: http://cancerres. aacrjournals.org/content/55/15/3346.abstract?sid=e8f2c7a4-bcb4-4695-b4087c40ee713951 [37] Nijhuis, E. H. A., Poot, A. A., Feijen, J., and Vermes, I., 2006, “Induction of Apoptosis by Heat and c-Radiation in a Human Lymphoid Cell Line; Role of [38] [39] [40] [41] [42] [43] [44] [45] [46] [47] [48] [49] [50] [51] [52] [53] [54] Mitochondrial Changes and Caspase Activation,” Int. J. Hyperthermia, 22(8), pp. 687–698. Shelton, S. N., Dillard, C. D., and Robertson, J. D., 2010, “Activation of Caspase-9, but not Caspase-2 or Caspase-8, is Essential for Heat-Induced Apoptosis in Jurkat Cells,” J. Biol. Chem., 285(52), pp. 40525–40533. Wilson, L., and Matsudaira, P. T., 1995, Cell Death, Vol. 46, Academic Press, New York. Ritossa, F., 1962, “A New Puffing Pattern Induced by Temperature Shock and DNP in Drosophila,” Cell Mol. Life Sci., 18(12), pp. 571–573. Todryk, S., Melcher, A. A., Hardwick, N., Linardakis, E., Batemen, A., and Colombo, M. P., 1999, “Heat Shock Protein 70 Induced During Tumor Cell Killing Induces Th1 Cytokines and Targets Immature Dendritic Cell Precursors to Enhance Antigen Uptake,” J. Immunol., 163(3), pp. 1398–1408. Available at: http://www.jimmunol.org/content/163/3/1398.abstract Yoo, J. C., and Mayman, M. J., 2006, “HSP70 Binds to SHP2 and Has Effects on the SHP2-Related EGFR/GAB1 Signaling Pathway,” Biochem. Biophys. Res. Commun., 351(4), pp. 979–985. Theriault, J. R., Mambula, S. S., Sawamura, T., Stevenson, M. A., and Calderwood, S. K., 2005, “Extracellular HSP70 Binding to Surface Receptors Present on Antigen Presenting Cells and Endothelial/Epithelial Cells,” FEBS Lett., 579(9), pp. 1951–1960. Beere, H. M., Wolf, B. B., Cain, K., Mosser, D. D., Mahboubi, A., and Kuwana, T., 2000, “Heat-Shock Protein 70 Inhibits Apoptosis by Preventing Recruitment of Procaspase-9 to the Apaf-1 Apoptosome,” Nature Cell Biol., 2(8), pp. 469–475. Ravagnan, L., Gurbuxani, S., Susin, S. A., Maisse, C., Daugas, E., and Zamzami, N., 2001, “Heat-Shock Protein 70 Antagonizes Apoptosis-Inducing Factor,” Nature Cell Biol., 3(9), pp. 839–843. Kim, Y.-M., de Vera, M. E., Watkins, S. C., and Billiar, T. R., 1997, “Nitric Oxide Protects Cultured Rat Hepatocytes From Tumor Necrosis Factor-aInduced Apoptosis by Inducing Heat Shock Protein 70 Expression,” J. Biol. Chem., 272(2), pp. 1402–1411. Li, C.-Y., Lee, J.-S., Ko, Y.-G., Kim, J.-I., and Seo, J.-S., 2000, “Heat Shock Protein 70 Inhibits Apoptosis Downstream of Cytochrome C Release and Upstream of Caspase-3 Activation,” J. Biol. Chem., 275(33), pp. 25665–25671. Komarova, E. Y., Afanasyeva, E. A., Bulatova, M. M., Cheetham, M. E., Margulis, B. A., and Guzhova, I. V., 2004, “Downstream Caspases are Novel Targets for the Antiapoptotic Activity of the Molecular Chaperone HSP70,” Cell Stress Chaperones, 9(3), pp. 265–271. Creagh, E. M., Carmody, R. J., and Cotter, T. G., 2000, “Heat Shock Protein 70 Inhibits Caspace-Dependent and -Independent Apoptosis in Jurkat T Cells,” Exp. Cell Res., 257(1), pp. 58–66. Bretland, A. J., Lawry, J., and Sharrard, R. M., 2001, “A Study of Death by Anoikis in Cultured Epithelial Cells,” Cell Prolif., 34(4), pp. 199–210. Frisch, S. M., and Screaton, R. A., 2001, “Anoikis Mechanisms,” Curr. Opin. Cell Biol., 13(5), pp. 555–562. Grossmann, J., 2002, “Molecular Mechanisms of ‘Detachment-Induced Apoptosis—Anoikis’,” Apoptosis, 7(3), pp. 247–260. Kamarajan, P., and Kapila, Y. L., 2007, “An Altered Fibronectin Matrix Induces Anoikis of Human Squamous Cell Carcinoma Cells by Suppressing Integrin Alpha V Levels and Phosphorylation of FAK and ERK,” Apoptosis, 12, pp. 2221–2231. Bunek, J., Kamarajan, P., and Kapila, Y. L., 2011, “Anoikis Mediators in Oral Squamous Cell Carcinoma,” Oral Dis., 17(4), pp. 355–361. 071006-10 / Vol. 136, JULY 2014 Downloaded From: http://biomechanical.asmedigitalcollection.asme.org/ on 05/20/2014 Terms of Use: http://asme.org/terms Transactions of the ASME