1 Abstract: The inner layer of the human uterus (the junctional zone
advertisement

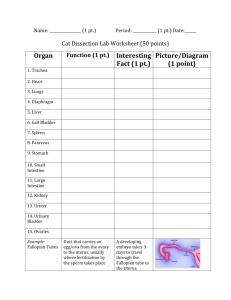
Abstract: The inner layer of the human uterus (the junctional zone, JZ) and Fallopian tube is of central importance for normal implantation, and for retrograde menstruation leading to diseases like endometriosis, but the factors involved in control of the complex motility pattern are poorly understood. Interstial Cajal-Like Cells (ICLCs)may play a central role, but no data are available on their distribution related to the mucosa and smooth muscle cells. The present study aims at describing the immunohistochemistry and location of these cells in the human Fallopian tube and uterus including the JZ. Introduction: The non-pregnant uterus has a complex motility pattern with peristalsis-like contractions of central importance for fertilization and implantation. In vivo imaging has demonstrated that peristalsis is confined to the endometrium and the subendometrial myometrium (1;2) which form the Junctional Zone (JZ) and represent the inner third of the uterine wall(3). Immunocytochemical studies have shown that the human JZ exhibits a cyclic pattern of oestrogen receptor (ER) and progesterone receptor (PR) expression that parallels that of the endometrium, whereas such changes are not observed in the outer layers of the myometrium (4) Both oestrogen and oxytocin may influence uterine peristalsis, and oestrogen up-regulates the oxytocin/oxytocinreceptor system (4). It is also likely that vasoactive substances such as thromboxane, other prostaglandins and β-adrenoceptors exhibit a cyclic expression since they are regulated by the ovarian sex hormones (5). Although these studies indicate a detailed endogenous control, no functional data are available to identify the actual mechanisms involved in human JZ motility. The length-tension relations are unknown, which precludes organ bath experiments on isolated muscle preparations. A recent study therefore defined these basic mechanical characteristics (6). The peristalsis-like motility suggests similarities between the uterine JZ and the gut. In the digestive system, Interstitial Cajal Cells (ICCs) serve as pacemakers of peristalsis and intermediaries between nerve endings and smooth muscle cells(7). Interstitial Cajal Like Cells (ICLCs, sometimes called “telocytes” (8)) have been identified in a number of organ systems outside the gut, including the uterus, and represent a specific cell type with a spindle-shaped body and several processes by which they establish contacts with other ICLCs, smooth muscle cells and nerve endings (9). So far, the peristaltic activity of the non-pregnant uterus is known to serve fundamental functions in the early process of reproduction, while hyper- and dysperistalsis of the JZ seems associated with the development of endometriosis, adenomyosis and dysmenorrhea(10;11). 1 In the bladder, Interstitial Cajal-like Cells (ICLCs) are found in the submucosa, and may serve as a functional link between the bladder mucosa and the smooth muscle (12). Demonstration of such contacts between the endometrium and the myometrial smooth muscle cells would imply a new paradigm in our understanding of uterine and tubal function and might imply new targets for pharmacological intervention for failed implantation, dysmenorrhea, and endometriosis. Several ICLC markers have been identified. Most ICLCs possess the C-kit receptor (7;8), which is a tyrosine kinase essential for normal cell function. Platelet Derived Growth Factor Receptor α (PDGFRα) is structurally similar to C-kit and both are currently accepted as ICLC markers. In addition, CD34 and small-conductance calcium-activated potassium channels (SK3) have been used to differentiate ICLCs from other cell types (13). CD34 is a cell-surface protein and functions as an adhesion glycoprotein. It is expressed on precursor hematopoietic cells and on ICC. It may also be expressed on fibroblasts and endothelial cells (8). Finally, SK3 are small-conductance Ca2+activated K+ channels. Immuno-electron microscopic analyses have indicated that SK3 channels are localized on processes of ICCs which are in close contact with nerves and smooth muscle cells (14). Immunohistochemical studies need supplementation with electron microscopy if detection of ICLCs is to be of “golden standard”(8;15). Such studies are also needed to evaluate functionally important contacts with structures like the endometrium and JZ smooth muscle. ICLCs have been detected in the human pregnant and non-pregnant myometrium (8;9;13) and the Fallopian tube (8), but so far, conflicting data have been presented (9). Most importantly, however, no data are available on the human JZ zone, which represents the area of functional interest due to the peristalsis-like motility of this tissue found in clinical studies (1;2). Moreover, no specific data on ICLCs in the circular and longitudinal layers of the ampullo-isthmic junction and the uterotubal junction of the human Fallopian tube are available, although these tissues show marked differences in functional properties(16-18). The aim of the present study is therefore to evaluate by immunohistochemistry the potential presence of ICLCs in the JZ compared to the outer layers of the human myometrium, together with the smooth muscle layers of the Fallopian tube. Moreover tissues will be stored for subsequent electron microscopy to evaluate potential ICLC contacts with the mucosal linings and the underlying smooth muscle layers Hypothesis ICLCs can be demonstrated in the submucosa of the endometrium, the JZ, and the intermediate and outer layers of the human uterus. 2 ICLCs can be demonstrated in the uterotubal junction and the ampullo-isthmic junction of the human Fallopian tube Tissues will be stored for subsequent electron microscopy in order to evaluate whether ICLCs exhibit cell projections in contact with smooth muscle cells of the JZ and outer layers of the myometrium ICLCs exhibit projections close to the endometrium Methods: A priori inclusion criteria are premenopausal women (age ≤ 51years) with no previous history of intrauterine surgery or treatment with GnRH analogues, undergoing hysterectomy for benign diseases or prophylactic hysterectomy with bilateral salpingoophorectomi. All women sign a form of informed consent prior to the hysterectomy. The study is approved by the Ethical Committee for Region Midt, Denmark (No. 2010.0094). Sample handling: The uterus is placed in 4 ˚C isotonic saline solution immediately after removal and sent to pathological examination. The pathologist divides the uterus in an anterior and posterior part, and cuts a specimen from a macroscopically normal area from the cervix, corpus, uterotubal junction and the ampullo-isthmic junction of the fallopian tube. The specimens are placed in 4 ˚C Krebs solution and transported to the laboratory. The pathologist determines whether the patient is in proliferative phase or secretory phase of the menstrual cycle. If the endometrium is atrophic, i.e. not under normal hormonal control, the corresponding result will be excluded from the study. Pre-analytic procedures are performed in the laboratory after collecting the tissue samples. Firstly, the tissue samples that have been approved by the pathologist need to be further dissected; samples from cervix, corpus, uterotubal junction and ampullo-isthmic junction are isolated (Figure 1). Sample dissection (Figure 1) will be standardized to ensure specific strips from the same uterine part in each sample. A standard procedure will likewise ensure separate specimens of the three myometrial layers and the three layers of the uterotubal junction and the two layers from the ampullo-isthmic junction. After dissection, the specimens are placed in fixative, and subsequently rinsed and stored prior to paraffin-embedding. After thin sectioning on a microtome and mounting on slides, the paraffin is removed and the tissue samples are subjected to heat-induced epitope retrieval (HIER), which is a pre-treatment procedure used to recover epitopes from the fixed tissue. HIER improves immunostaining of target proteins, in our case PDGFR, c-kit, CD34 and SK3. The primary antibody binds to the target proteins, while addition of the secondary fluorescent antibody is necessary for detection. Confocal microscopy of the antibody-specific immunofluorescence permits 3 analysis and interpretation of the results. These methods are well established in our laboratory, and have been used in previous studies on morphology of interstitial cells (15) Figur 1 - Dissection of the specimen. 1: Cervix. 2: Corpus. 3: Uterotubal junction. 4: Ampulloisthmic junction It has already been possible to run some pilot experiments of method and PDGFR expression in human myometrium. Figure 2 demonstrates that we can process fixation and creation of thinsection specimens, that our primary antibody PDGFR is specific for ICLCs, and that we have the capacity to make high quality images with our confocal microscope. Figure 2 - Control images compared with images of antiPDGFRα staining. Visualization of the primary antibody anti-PDGFR that binds to ICLCs in the human myometrium. 4 Perspectives: The immunohistochemical studies will be followed by electron microscopy to reveal the connections between ICLCs and the mucosa and smooth muscle cells, and functional studies including confocal imaging(15) to assess the physiological importance of ICLC function. Demonstration of ICLCs with potential connections to the mucosa and the smooth muscle layers of the uterus and the Fallopian tube implies new perspectives on the endogenous control of uterotubal motility, with possible targets for therapeutic intervention. Cooperation: Tissues are obtained at the Department of Obstetrics and Gynecology at Aarhus University Hospital, in a well-established cooperation. Excision of tissues is performed in cooperation with the Department of pathology at Aarhus University Hospital. Immunostaining of the tissue is performed in cooperation with the Institute of Biomedicine, University of Aarhus. Ethical aspects: The study has been approved by the Ethical Committee for Region Midt, Denmark (No 2010.0094). Applicant and supervisors: The study is run by Sergey Machado-Abakumov, BM, with supervision from Karl-Erik Andersson (main supervisor), Professor, Aarhus Institute of Advanced Studies (AIAS), Institute of Physiology and Department of Obstetrics and Gynecology, Aarhus University Further members of the research group: Donne Bødtker, ass professor, Department of Physiology, Aarhus University. Mathias Heide Gottschalck, MD Department of Obstetrics and Gynecology, Institute of Clinical Medicine, and Christian Aalkjær, professor, dr. med. Department of Physiology, Institute of Biomedicine. Axel Forman professor, Department of Obstetrics and Gynecology, Institute of Clinical Medicine. Time schedule: The project is planned to last twelve months and contains four phases: Sept Oct Nov Dec Jan Feb March April May June July Aug 1 2 3 4 1. Literature search, grant search, implementing sample collection, learning of procedures and statistical methods. 2. Experiments 3. Analysis 4. Article writing 5 Reference List (1) Kunz G, Beil D, Huppert P, Leyendecker G. Control and function of uterine peristalsis during the human luteal phase. Reprod Biomed Online 2006 Oct;13(4):528-40. (2) Nakai A, Togashi K, Yamaoka T, Fujiwara T, Ueda H, Koyama T, et al. Uterine peristalsis shown on cine MR imaging using ultrafast sequence. J Magn Reson Imaging 2003 Dec;18(6):726-33. (3) Brosens I, Derwig I, Brosens J, Fusi L, Benagiano G, Pijnenborg R. The enigmatic uterine junctional zone: the missing link between reproductive disorders and major obstetrical disorders? Hum Reprod 2010 Mar;25(3):569-74. (4) Noe M, Kunz G, Herbertz M, Mall G, Leyendecker G. The cyclic pattern of the immunocytochemical expression of oestrogen and progesterone receptors in human myometrial and endometrial layers: characterization of the endometrial-subendometrial unit. Hum Reprod 1999 Jan;14(1):190-7. (5) Mueller A, Maltaris T, Siemer J, Binder H, Hoffmann I, Beckmann MW, et al. Uterine contractility in response to different prostaglandins: results from extracorporeally perfused non-pregnant swine uteri. Hum Reprod 2006 Aug;21(8):2000-5. (6) Gottschalck MG, Staehr-Hansen E, Sundtoft I, Aalkjaer C, Dueholm M, Forman A. Specialized Mechanical Properties of the Junctional Zone in the Human Uterus. Hum.Reprod. Submitted. 2013. (7) Vannucchi MG. Receptors in interstitial cells of Cajal: identification and possible physiological roles. Microsc Res Tech 1999 Dec 1;47(5):325-35. (8) Popescu LM, Ciontea SM, Cretoiu D. Interstitial Cajal-like cells in human uterus and fallopian tube. Ann N Y Acad Sci 2007 Apr;1101:139-65. (9) Hutchings G, Williams O, Cretoiu D, Ciontea SM. Myometrial interstitial cells and the coordination of myometrial contractility. J Cell Mol Med 2009 Oct;13(10):4268-82. (10) Leyendecker G, Kunz G, Noe M, Herbertz M, Mall G. Endometriosis: a dysfunction and disease of the archimetra. Hum Reprod Update 1998 Sep;4(5):752-62. (11) Leyendecker G, Kunz G, Herbertz M, Beil D, Huppert P, Mall G, et al. Uterine peristaltic activity and the development of endometriosis. Ann N Y Acad Sci 2004 Dec;1034:338-55. (12) Soler R, Andersson KE, Chancellor MB, Chapple CR, de Groat WC, Drake MJ, et al. Future Direction in Pharmacotherapy for Non-neurogenic Male Lower Urinary Tract Symptoms. Eur Urol 2013 Oct;64(4):610-21. (13) Rosenbaum ST, Svalo J, Nielsen K, Larsen T, Jorgensen JC, Bouchelouche P. Immunolocalization and expression of small-conductance calcium-activated potassium channels in human myometrium. J Cell Mol Med 2012 Dec;16(12):3001-8. 6 (14) Fujita A, Takeuchi T, Saitoh N, Hanai J, Hata F. Expression of Ca(2+)-activated K(+) channels, SK3, in the interstitial cells of Cajal in the gastrointestinal tract. Am J Physiol Cell Physiol 2001 Nov;281(5):C1727-C1733. (15) Briggs BD, Rumessen J, Baandrup U, Skov MM, Telinius N, Pilegaard H, et al. Identification of interstitial Cajal-like cells in the human thoracic duct. Cells Tissues Organs 2013;197(2):145-58. (16) Lindblom B, Hamberger L, Ljung B. Contractile patterns of isolated oviductal smooth muscle under different hormonal conditions. Fertil Steril 1980 Mar;33(3):283-7. (17) Wilhelmsson L, Lindblom B, Wiqvist N. The human uterotubal junction: contractile patterns of different smooth muscle layers and the influence of prostaglandin E2, prostaglandin F2alpha, and prostaglandin I2 in vitro. Fertil Steril 1979 Sep;32(3):303-7. (18) Wilhelmsson L, Lindblom B. Adrenergic responses of the various smooth muscle layers at the human uterotubal junction. Fertil Steril 1980 Mar;33(3):280-2. 7