VIEW PDF - Glaucoma Today
advertisement

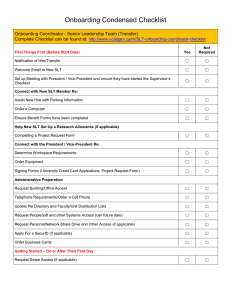
THERAPEUTICS UPDATE How SLT Works A technological hybrid for selective laser trabeculoplasty effectively treats glaucoma without damaging the trabecular meshwork. BY ROBERT J. NOECKER, MD, MBA M ark Latina, MD, of Reading, Massachusetts, developed selective laser trabeculoplasty (SLT) to achieve the benefits of argon laser trabeculoplasty (ALT) while causing fewer side effects. Whereas SLT does not significantly heat ocular tissue, ALT causes irreversible coagulative necrosis to the treated trabecular meshwork. If initial treatment of 180º ALT does not effectively lower the IOP, the surgeon should usually augment the procedure in the opposite 180º only, and total treatment is usually limited to 360º. With ALT, peripheral anterior synechiae often form postoperatively, which can increase IOP in the long term. Conversely, because SLT treats only pigmented cells, it does not cause structural damage to the trabecular meshwork, which can then be repopulated by endothelial cells. Theoretically, the number of treatments is not limited by structural damage, and therefore SLT is much safer and more repeatable than ALT. This article focuses on the mechanism and utility of SLT. THE LASER The Selecta II Glaucoma Laser System (Lumenis Inc., Santa Clara, CA) is a technological hybrid consisting of a double-frequency Nd:YAG laser, which works at a green wavelength (532 nm). Melanin absorbs this green light just as it does argon and other visible wavelengths of light. Rather than burn tissue to achieve the desired effect, the Selecta Duet laser (Lumenis Inc.) does not significantly heat the trabecular meshwork due to its brief pulses of energy (3 nanoseconds). The traditional Nd:YAG laser is ineffective for laser trabeculoplasty because its wavelength is not absorbed by pigmentcontaining structures. The exposure times of typical continuous-wave lasers are too long and cause thermal damage to ocular tissue. In ALT, the pulses of laser energy last longer than in SLT and cause burns that result in ongoing coagulative damage, sometimes for years. The Selecta Duet laser’s spot size is 400 µm in diameter, much larger than the typical spot size (10 µm) of an Nd:YAG laser focused on the posterior capsule or the 30 I GLAUCOMA TODAY I MARCH/APRIL 2005 A B Figure 1. There is no evidence of damage to the trabecular meshwork beams in a human eye treated with SLT. Viable endothelial cells are present in the treated region (A). Treatment of the same eye with ALT creates a large crater and coagulated trabecular meshwork beams. No viable cells are present in the treated region (B). iris. The larger spot size is less harmful to ocular tissue because the energy is not concentrated in a small area. The low fluency of energy safely and effectively diffuses over a larger area. Because the relative amount of energy placed in the eye per pulse per given area is at least 10,000 times lower with SLT than ALT, the treatment achieves the desired effect without focal damage. M E C H A N I S M O F AC T I O N In a process known as selective photothermolysis, SLT targets only pigmented trabecular cells and causes no structural or coagulative damage to the trabecular meshwork. For selective photothermolysis to occur, there must be a targeted intracellular chromophore (melanin) and no competing chromophores (such as blood) present. In other words, there must be pigment in a cell for it to be a target that will absorb the laser energy better than surrounding tissues. The laser’s brief pulse duration confines heat to the pigmented cells within the irradiated zone. For example, during SLT, the laser targets pigmented cells and does not damage the nonpigmented trabecular cells or collagen beams. In contrast, ALT destroys all cells (with and without pigment) in a culture model.1 ALT destroys a viable area of the trabecular meshwork, creates a crater in this tissue, and causes a THERAPEUTICS UPDATE depopulation of all the normal structures. A region treated with SLT, however, has a normal appearance and can be repopulated by trabecular cells (Figure 1). 0 -1 baseline 1 day 1 wk 2 wks 4wks 8 wks 14 wks 20 wks 26 wks -2 IOP (mmHg) -3 -4 LOW E R I N G T H E I O P -5 SLT has numerous biological effects. -6 For example, it causes a proliferation -7 of trabecular and endothelial cells, the release of cytokines, inflammation -8 (recruitment of macrophages), and -9 phagocytosis. The ultimate result is -10 Weeks increased aqueous outflow.2 Clinically, several distinct phases in Max Rx Group the photoactivation process occur Prior Failed Laser Trabeculoplasty after SLT. First, the laser targets and Combined destroys cells containing melanin. Figure 2. This graph shows typical IOP curves after treatment with SLT in the US Treatment generates small bubbles, clinical trial. Following an initial large drop in IOP on day 1, IOP plateaus for severwhich may float into the anterior chamber. These “champagne” bubbles al weeks after initial therapy. The effect lasted until the 6-month point of this trial. signal to me that I am near the energy (Data adapted from Latina MA, Sibayan SA, Shin DH, et al. Q-switched 532-nm Nd:YAG laser trabeculoplasty [selective laser trabeculoplasty]: a multicenter, pilot, threshold of treatment effect. Hours clinical study. Ophthalmology. 1998;105:2082-2090.) or days after SLT, an intermediate cellular response is noticeable. Biologically, the activity of the trabecular meshwork’s cells and F I R S T- L I N E T R E ATM E N T macrophages increases. Nuclear translocation of tranWhereas surgeons typically perform ALT after medical scription factors and an induction of vasoactive agents therapy has failed and prior to surgical intervention, SLT (eg, a release of cytokines) occur, and the recruitment may be appropriate as primary therapy for some patients of macrophages begins. The IOP decreases as the repair with open-angle glaucoma. The 13-site SLT/MED study process begins. will compare SLT with stepped medications as the initial In the long term (months or years), the number of monotherapy for the treatment of glaucoma. Three hunmacrophages present in the trabecular meshwork indred patients have been randomized to receive either creases and thus improves the eye’s outflow facility.3 medication or SLT as initial intervention. My co-investigaCytokines play many roles. They act as growth factors tors and I will follow these individuals for 12 months to for human trabecular meshwork cells, which repopulate see which treatment arm is more effective in terms of the treated areas. These cells can act at the level of slowing glaucomatous progression. ❏ Schlemm’s canal to increase transendothelial fluid flow. Robert J. Noecker, MD, MBA, is Director of They are also involved in the expression of certain metthe Glaucoma Service and Associate alloproteinases and stimulate the remodeling of the Professor/Vice Chair of the Department of extracellular matrix of the trabecular meshwork’s tisOphthalmology at the University of Pittsburgh. sues. The latter action promotes aqueous outflow. He is on the speaker’s bureau for Lumenis, Inc. It is not uncommon for the IOP to drop precipitously Dr. Noecker may be reached at (412) 647-2152; the day after SLT. A slight increase in pressure may occur noeckerrj@upmc.edu. during the intermediate phase when cellular infiltration begins. For instance, a patient may have a higher IOP 10 to 1. Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of 14 days after SLT. In the long term, IOP tends to level out, pulsed and CW laser interactions. Exp Eye Res. 1995;60:359-371. and the IOP gradually drops as the remodeling process 2. Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-switched 532-nm continues (Figure 2). Clinicians may wish to observe paNd:YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter, pilot, clinical tients whose initial postoperative IOPs are not sufficiently study. Ophthalmology. 1998;105:2082-2090. low, because SLT’s maximal effect may not occur for sever- 3. Latina MA, Gulati V. Selective laser trabeculoplasty: stimulating the meshwork to mend its ways. Int Ophthalmol Clin. 2004;44:93-103. al months. MARCH/APRIL 2005 I GLAUCOMA TODAY I 31